Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Sotirios Sotiriou | + 714 word(s) | 714 | 2021-08-20 04:28:16 | | | |
| 2 | Camila Xu | + 191 word(s) | 905 | 2021-09-02 05:44:00 | | | | |
| 3 | Camila Xu | + 191 word(s) | 905 | 2021-09-02 05:44:39 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Sotiriou, S. β-Thalassemia Heterozygotes. Encyclopedia. Available online: https://encyclopedia.pub/entry/13763 (accessed on 07 February 2026).
Sotiriou S. β-Thalassemia Heterozygotes. Encyclopedia. Available at: https://encyclopedia.pub/entry/13763. Accessed February 07, 2026.
Sotiriou, Sotirios. "β-Thalassemia Heterozygotes" Encyclopedia, https://encyclopedia.pub/entry/13763 (accessed February 07, 2026).
Sotiriou, S. (2021, August 31). β-Thalassemia Heterozygotes. In Encyclopedia. https://encyclopedia.pub/entry/13763
Sotiriou, Sotirios. "β-Thalassemia Heterozygotes." Encyclopedia. Web. 31 August, 2021.
Copy Citation
β-Thalassemia is the most prevalent single gene blood disorder, while the assessment of its susceptibility to coronavirus disease 2019 (COVID-19) warrants it a pressing biomedical priority.
β-thalassemia
risk
coronavirus
1. Introduction
Identifying medical conditions with a high or potentially deadly impact on the disease caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), is a critical initial step towards containment of associated morbidity and mortality risks. Given that viral stress from SARS-CoV-2 elicits anabolic responses supported by increasing blood pressure to meet enhanced oxygen needs of vital organs and organ systems, hypoxemia is rendered a high-risk medical condition [1][2]. As the most common blood disorder affecting approximately one third of the global population, anemia presents a low tolerance to hypoxemia and may have either acquired polysystemic or inherited poly- or monogenic background [3]. Monogenic anemia—which is caused by abnormal hemoglobin—is a rather prevalent medical disorder with 270 million carriers worldwide [4][5][6]. β-Thalassemia is the most common inherited single gene disorder in the world. Approximately one-third of all hemoglobinopathies and/or nearly 1.5% of the global population carry the β-thalassemia trait [7]. In this context, β-thalassemia heterozygosity is a strong candidate condition for assessing an individual’s susceptibility to COVID-19.
2. Associations
Association of β-thalassemia heterozygosity with severe and critical COVID-19 symptoms.
Considering the clinical spectrum of COVID-19 as a primary outcome, patients were categorized into three groups (asymptomatic and mild/ moderate/ severe and critical). No difference in chest X ray or CT scan was observed among study participants. In univariate analysis, sex (p = 0.047), age (p < 0.001), atrial fibrillation (p = 0.022), coronary disease (p = 0.041), hyperlipidemia (p = 0.014), hypertension (p < 0.001), and being heterozygous for thalassemia (p = 0.004) were associated with severe COVID-19 symptoms (Table 1). In multivariate analysis, male sex (p = 0.023), increased age (p < 0.001), and being heterozygous for thalassemia (p = 0.002) were identified as independent risk factors for severe and critical clinical COVID-19 symptoms. Specifically, males had a 1.81 times (95% CI, 1.09 to 3.01) increased possibility for severe or critical clinical symptoms; increased age was associated with increased odds of severe and clinical symptoms with OR = 1.06 (95% CI, 1.04 to 1.08). A finding of great interest is that patients who were heterozygous for thalassemia were 2.89 times (95% CI, 1.49 to 5.62) more likely to have severe and critical clinical symptoms of COVID-19 (Figure 1).
Table 1. Characteristics and COVID-19 clinical spectrum.
| Severity | Univariate | Multivariate Ordinal Logistic Regression (Severe and Critical vs. Others) | ||||
|---|---|---|---|---|---|---|
| Mild (%) | Moderate (%) | Severe and Critical (%) | p-Value | p-Value | aOR with 95% CI | |
| Sex (M/F) | 34/34 | 67/46 | 52/22 | 0.047 * | 0.023 | 1.81 (1.09–3.01) |
| Age (median, IQR) | 51.5 (34) | 64.0 (17) | 70.5 (15) | <0.001 ± | <0.001 | 1.06 (1.04–1.08) |
| Atrial Fibrillation | 17 (25.0) | 32 (28.3) | 33 (44.6) | 0.022 * | 0.787 | 0.92 (0.49–1.71) |
| Respiratory Disease | 5 (7.4) | 13 (11.5) | 14 (18.9) | 0.104 * | 0.325 | 1.47 (0.68–3.15) |
| Coronary Disease | 7 (10.3) | 23 (20.4) | 20 (27.0) | 0.041 * | 0.955 | 1.02 (0.50–2.09) |
| Diabetes | 10 (14.7) | 25 (22.1) | 18 (24.3) | 0.331 * | 0.619 | 0.85 (0.45–1.60) |
| Neoplasia | 7 (10.3) | 11 (9.7) | 11 (14.9) | 0.529 * | 0.209 | 0.61 (0.28–1.32) |
| Hyperlipidemia | 21(30.9) | 60 (53.1) | 32 (43.2) | 0.014 * | 0.138 | 0.65 (0.37–1.15) |
| Hypertension | 24 (35.3) | 62 (54.9) | 56 (75.7) | <0.001 * | 0.104 | 1.67 (0.90–3.08) |
| β-Thalassemia Heterozygotes | 5 (7.4) | 19 (16.8) | 21 (28.4) | 0.004 * | 0.002 | 2.89 (1.49–5.62) |
* Chi-square test, ± Mann–Whitney test; Bold is for the statistically significant results (p-value < 0.05).
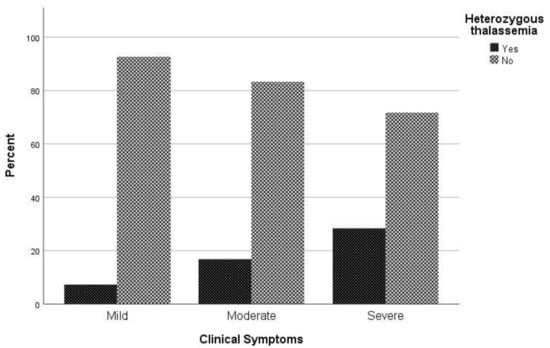
Figure 1. Proportion of β-thalassemia heterozygotes relative to non-carriers regarding clinical symptoms to COVID-19.
2.1. Association of β-Thalassemia Heterozygotes with Mortality Due to COVID-19
Regarding mortality associated with COVID-19 infection, in univariate analysis sex (p = 0.022), age (p < 0.001), atrial fibrillation (p = 0.002), respiratory disease (p = 0.027), coronary disease (p = 0.027), hypertension (p < 0.001), and being heterozygous for thalassemia (p = 0.005) were associated with mortality (Table 2). In logistic regression analysis, male patients had a 2.09 times (95% CI, 1.05 to 4.18) greater possibility of dying and patients with increased age were 1.06 times (95% CI, 1.03 to 1.09) more likely to die. It is worth noting that hyperlipidemia plays a beneficial role in COVID-19 mortality, as the odds ratio of mortality in patients with hyperlipidemia is 0.65 (95% CI 0.37–1.15). It should be highlighted that patient who are heterozygous for thalassemia have a 2.79 times (95% CI, 1.28 to 6.09) greater possibility of dying than other patients (Figure 2).
Table 2. Characteristics and mortality due to COVID-19.
| Mortality | Univariate | MultivariateBinary Logistic Regression | |||||
|---|---|---|---|---|---|---|---|
| Yes (%) | No (%) | p-Value | OR with 95% CI | RR with 95% CI | p-Value | aOR with 95% CI | |
| Sex (M/F) | 50/20 | 103/82 | 0.022 * | 1.99 (1.10–3.61) | 1.67 (1.06–2.64) | 0.036 | 2.09 (1.05–4.18) |
| Age (median, IQR) | 72.5 (15) | 61.0 (24) | <0.001 ± | - | - | <0.001 | 1.06 (1.03–1.09) |
| Atrial Fibrillation | 33 (47.1) | 49 (26.5) | 0.002 * | 2.48 (1.40–4.39) | 1.88 (1.28–2.78) | 0.201 | 1.64 (0.77–3.48) |
| Respiratory Disease | 14 (20.0) | 18 (9.7) | 0.027 * | 2.32 (1.08–4.97) | 1.74 (1.11–2.74) | 0.297 | 1.61 (0.66–3.95) |
| Coronary Disease | 20 (28.6) | 30 (16.2) | 0.027 * | 2.07 (1.08–3.96) | 1.64 (1.08–2.49) | 0.808 | 0.90 (0.39–2.09) |
| Diabetes | 18 (25.7) | 35 (18.9) | 0.233 * | 1.48 (0.77–2.84) | 1.32 (0.85-2.05) | 0.758 | 0.87 (0.41–1.91) |
| Neoplasia | 10 (14.3) | 19 (10.3) | 0.367 * | 1.46 (0.64-3.31) | 1.30 (0.75–2.24) | 0.395 | 0.67 (0.26–1.70) |
| Hyperlipidemia | 30 (42.9) | 83 (44.9) | 0.773 * | 0.92 (0.53–1.61) | 0.94 (0.63–1.41) | 0.008 | 0.38 (0.19–0.78) |
| Hypertension | 52 (74.3) | 90 (48.6) | <0.001 * | 3.05 (1.66–6.60) | 2.30 (1.43–3.70) | 0.198 | 1.67 (0.77–3.62) |
| β-Thalassemia Heterozygotes | 20 (28.6) | 25 (13.5) | 0.005 * | 2.56 (1.31–4.99) | 1.87 (1.24–2.80) | 0.010 | 2.79 (1.28–6.09) |
* Chi-square test, ± Mann–Whitney test; Bold is for the statistically significant results (p-value < 0.05).
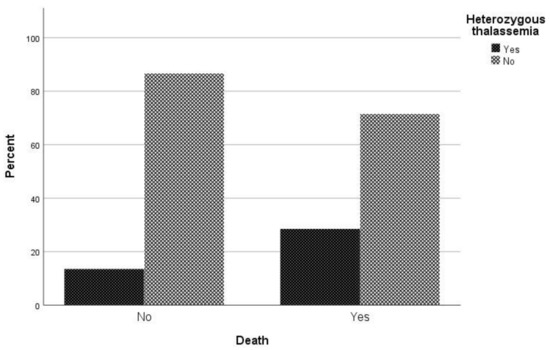
Figure 2. Proportion of β-thalassemia heterozygotes relative to non-carriers regarding mortality due to COVID-19.
2.2. Admission of COVID-19 Infected β-Thalassemia Heterozygotes to the ICU
Regarding the requirement for ICU care, it was found through univariate analysis that age (p = 0.03), respiratory disease (p = 0.043), coronary disease (p = 0.029) and hypertension (p < 0.001) were associated with ICU admission (Table 3). Through logistic regression analysis, patients with hypertension had 5.12 times (95% CI, 2.04 to 12.87) greater risk of requiring ICU care than patients without hypertension. On the contrary, hyperlipidemia was identified as a protective factor against ICU admission, with OR = 0.44 (95% CI, 0.21 to 0.94). Furthermore, in relation to the requirement for ICU care, being heterozygous for thalassemia had no effect on the possibility of admission to the ICU (p = 0.505).
Table 3. Characteristics and ICU admission due to COVID-19.
| ICU | Univariate | MultivariateBinary Logistic Regression | |||||
|---|---|---|---|---|---|---|---|
| Yes (%) | No (%) | p-Value | OR with 95% CI | RR with 95% CI | p-Value | aOR with 95% CI | |
| Sex (M/F) | 36/17 | 117/85 | 0.186 * | 1.54 (0.81–2.92) | 1.41 (0.84–2.37) | 0.305 | 1.45 (0.72–2.93) |
| Age (median, IQR) | 66.2 (17) | 60.4 (24) | 0.030 ± | - | - | 0.649 | 1.01 (0.98–1.04) |
| Atrial Fibrillation | 21 (36.9) | 61 (30.2) | 0.191* | 1.52 (0.81–2.84) | 1.39 (0.85–2.25) | 0.966 | 0.98 (0.43–2.23) |
| Respiratory Disease | 11 (20.8) | 21 (10.4) | 0.043 * | 2.26 (1.01–5.04) | 1.83 (1.05–3.17) | 0.205 | 1.80 (0.73–4.46) |
| Coronary Disease | 16 (30.2) | 34 (16.8) | 0.029 * | 2.14 (1.07–4.27) | 1.77 (1.08–2.92) | 0.393 | 1.48 (0.61–3.59) |
| Diabetes | 10 (18.9) | 43 (21.3) | 0.699 * | 0.86 (0.40–1.85) | 0.87 (0.48–1.64) | 0.098 | 0.49 (0.21–1.14) |
| Neoplasia | 4 (7.5) | 25 (12.4) | 0.466 † | 0.58 (0.19–1.74) | 0.64 (0.25–1.63) | 0.102 | 0.37 (0.11–1.22) |
| Hyperlipidemia | 22 (41.5) | 91 (45.0) | 0.644 * | 0.87 (0.47–1.60) | 0.89 (0.55–1.45) | 0.033 | 0.44 (0.21–0.94) |
| Hypertension | 42 (79.2) | 100 (49.5) | <0.001 * | 3.90 (1.90–7.99) | 3.04 (1.64–5.63) | 0.001 | 5.12 (2.04–12.87) |
| β-Thalassemia Heterozygotes | 11 (20.8) | 34 (16.8) | 0.505 * | 1.29 (0.61–2.77) | 1.22 (0.68–2.18) | 0.508 | 1.33 (0.57–3.06) |
* Chi-square test, ± Mann–Whitney test, † Fisher’s exact test; Bold is for the statistically significant results (p-value < 0.05).
2.3. Length of Hospitalization until Death
When comparing the median length of hospitalization (days) between patients being heterozygous for thalassemia and non-carriers, a statistically significant difference was observed (p = 0.046) (Figure 3). More specifically, the median duration of hospitalization among carriers and non-carriers was 12 and 17.5 days, respectively.
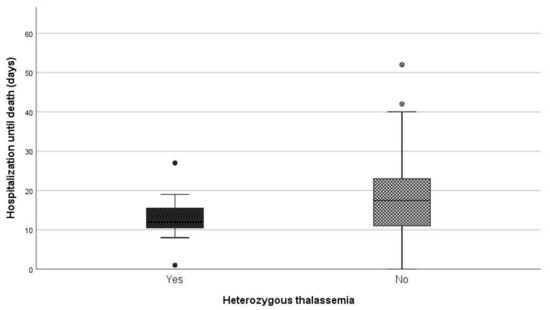
Figure 3. Days of hospitalization until death between carries and non-carriers.
2.4. Length of Hospitalization among Patients Who Survived
Regarding days of hospitalization among patients that survived COVID-19, the median duration was eight days for patients that were heterozygous for thalassemia and six days for non-carriers (p = 0.014) (Figure 4).
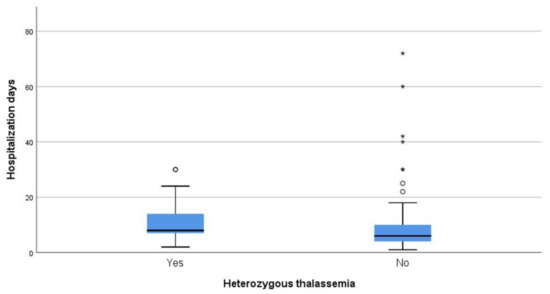
Figure 4. Days of hospitalization between carries and non-carriers that survived.
References
- Gheblawi, M.; Wang, K.; Viveiros, A.; Nguyen, Q.; Zhong, J.-C.; Turner, A.J.; Raizada, M.K.; Grant, M.B.; Oudit, G.Y. Angiotensin-Converting Enzyme 2: SARS-CoV-2 Receptor and Regulator of the Renin-Angiotensin System. Circ. Res. 2020, 126, 1456–1474.
- Rahman, A.; Tabassum, T.; Araf, Y.; Al Nahid, A.; Ullah, A.; Hosen, M.J. Silent hypoxia in COVID-19: Pathomechanism and possible management strategy. Mol. Biol. Rep. 2021, 48, 3863–3869.
- Lopez, A.; Cacoub, P.; Macdougall, I.C.; Peyrin-Biroulet, L. Iron deficiency anaemia. Lancet 2015, 387, 907–916.
- Samara, M.; Chiotoglou, I.; Kalamaras, A.; Likousi, S.; Chassanidis, C.; Vagena, A.; Vagenas, C.; Eftichiadis, E.; Vamvakopoulos, N.; Patrinos, G.P.; et al. Large-scale population genetic analysis for hemoglobinopathies reveals different mutation spectra in Central Greece compared to the rest of the country. Am. J. Hematol. 2007, 82, 634–636.
- De Sanctis, V. β-thalassemia distribution in the old world: A historical standpoint of an ancient disease. Mediterr. J. Hematol. Infect. Dis. 2016, 9, e2017018.
- Williams, T.N.; Weatherall, D.J. World Distribution, Population Genetics, and Health Burden of the Hemoglobinopathies. Cold Spring Harb. Perspect. Med. 2012, 2, a011692.
- Whetheral, D.J. The thalassemias. In Williams Hematology, 5th ed.; Beutler, E., Lichtman, M.A., Coller, B.S., Kipps, T.J., Eds.; McGraw-Hill: New York, NY, USA, 1995.
More
Information
Subjects:
Obstetrics & Gynaecology
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.3K
Entry Collection:
COVID-19
Revisions:
3 times
(View History)
Update Date:
02 Sep 2021
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




