Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Raffaella Gozzelino | -- | 3708 | 2024-05-06 23:02:25 | | | |
| 2 | Jason Zhu | Meta information modification | 3708 | 2024-05-07 07:35:09 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Pêgo, A.C.; Lima, I.S.; Gozzelino, R. COVID-19 Pandemic in Africa. Encyclopedia. Available online: https://encyclopedia.pub/entry/56619 (accessed on 28 February 2026).
Pêgo AC, Lima IS, Gozzelino R. COVID-19 Pandemic in Africa. Encyclopedia. Available at: https://encyclopedia.pub/entry/56619. Accessed February 28, 2026.
Pêgo, Ana Catarina, Illyane Sofia Lima, Raffaella Gozzelino. "COVID-19 Pandemic in Africa" Encyclopedia, https://encyclopedia.pub/entry/56619 (accessed February 28, 2026).
Pêgo, A.C., Lima, I.S., & Gozzelino, R. (2024, May 06). COVID-19 Pandemic in Africa. In Encyclopedia. https://encyclopedia.pub/entry/56619
Pêgo, Ana Catarina, et al. "COVID-19 Pandemic in Africa." Encyclopedia. Web. 06 May, 2024.
Copy Citation
On 30 January 2020, WHO declared COVID-19 a public health emergency of global concern. COVID-19 became pandemic on 11 March 2020, and spread unprecedently. No country was prepared to face its impact. Major fears started to be expressed for Africa, where dramatic consequences were expected, due to the weakness of health systems. The limited resources, in terms of qualified physicians, medical equipment and hospital infrastructures marked an undeniable inequality and highlighted the need to empower local capacity, raising the level of preparedness of African nations against infection outbreaks.
SARS-CoV-2
COVID-19
infections
Africa
1. COVID-19 in Africa
Africa is the second most populated continent, with around 1.3 billion people (17% of the world population) [1]. It comprises 54 independent nations, many of which are referred to as fragile states [2][3]. Original predictions indicated that Africa would be disproportionately affected by COVID-19 [4], also in view of the difficulty of implementing effective measures of social distancing [5]. The first case of COVID-19 was reported in Egypt on 14 February 2020 [6]. Then, imported cases started to be detected in other African nations, as most Europeans were trying to escape the dramatic reality they were experiencing [7]. African governments were highly sensitized to seeing countries with large economies being defeated by the virus and started to close borders and isolate nations from foreign entry [7]. Although in Africa local transmission increased slowly [7], the limited financial and qualified human resources to overcome the deadly disease forced this continent to preventively lock down [5][8]. The youthfulness of the African population is the most plausible explanation for reduced severity of COVID-19 in this continent. The average age is 19.7 years, and 60% of the population is younger than 25. Severe symptoms predominantly affected the elderly population [9], who suffered from sub-chronic impairments of the immune system. In Africa, immunity is linked to multiple pathogen exposures [10], which shape the immune response. This continuous activation is capable of reprogramming immune cells [11] and providing them with the ability to respond differently to microbes [12]. This is an advantage which allows individuals to better cope with infection, including during childhood. In the context of COVID-19, this notion was demonstrated by comparing the immunity elicited upon infection in Belgian, Canadian, Ecuadorian, and South African cohorts, the latter showing a reduced functional response of immune cells. Lifestyle trends, scarce consumption of processed food, climate, and environmental aspects are other factors that might have contributed to mitigating the dramatic effects caused by the pandemic [13]. This notion was supported by evidence showing that environmental parameters were able to contradict initial predictions and reduce virus lifespan [14][15]. While the low temperatures and humidity of the northern globe hemisphere facilitated the virus’ survival [16], the warm African climate was shown to reduce the risk of COVID-19 infection [17]. The effect of sunshine UV rays acted synergistically, on one hand compromising viral stability and diminishing disease transmission, and on the other causing a beneficial effect on the host. Individuals presenting an increased level of vitamin D were able to elicit a more efficient activation of an immune response against the virus [18]. It is also worth mentioning that the windy weather in some countries was also considered an advantage. It negatively affected viral spreading [19] and contributed to dispersing viral pathogens, lowering disease transmission. Hence, the growth curve for COVID-19 in Africa was inversely correlated to average temperature and wind speed [20].
However, a shift from this initial positive scenario occurred when multiple SARS-CoV-2 variants started to appear. By the end of 2020, most African countries underwent a second wave of infection, with a 30% growth in weekly incidence and daily average of new cases, in relation to the peak of the first COVID-19 wave [21]. Controversial suggestions were publicly advanced, with people proposing on international television channels to let the continent reaching heard immunity, a possibility that was finally not considered. Whether this was due to a global voice raised against those statements or to the fear of a potential “boomerang effect” is still not clear. Indeed, the many efforts made to contain the COVID-19 pandemic could have been jeopardized with a reestablished mobility between continents. The concern that implemented measures might have been of no use is possibly the reason for which “common sense” prevailed.
In March 2023, nearly 180,000 fatalities were reported in Africa vs. almost 8 million deaths registered worldwide. According to the WHO, South Africa and Morocco were the most affected [3][22]. In this regard, it should be highlighted that over 50% of African citizens reside in rural areas, with limited interaction with travelers or urban communities that could potentially carry the virus [23]. When compared to other continents, the rate of foreign travel to Africa is relatively low. South Africa and Morocco have the highest rates, ranking, respectively, 22nd and 28th worldwide. This may explain why these countries showed the highest number of cumulative COVID-19 cases in Africa [24].
Concerns regarding a possible discrepancy between predicted and confirmed cases stood out. The reduced morbidity and mortality registered in the African continent was inconsistent with the results obtained from seroprevalence tests [25]. Antibodies were detected in 10–30% of the African population. However, this percentage also raised numerous discussions, as positivity relied on the testing capacity of the country where the assay was performed [8]. No nations had the financial resources to purchase tests for all suspected cases. So, while there were countries who received more assistance than others from state cooperation and international donations, the percentage of conducted tests was not comparable to the developed world. While South Africa conducted a total of 54,224 tests per million people, Egypt and Nigeria carried out 1317 and 1504 tests, respectively. In the UK, the number of conducted tests was 266,500 per million people, and in the US it was 195,072 during the same period [26].
However, despite the overall lower number of individuals that were reported to have developed severe symptoms [4], COVID-19 in Africa is still a threat. The precarious situation, characterized by a variety of infectious diseases, malnutrition, and limited access to healthcare, has worsened since the pandemic occurred [27][28]. In addition, the inequality of vaccine distribution as well as of population adhesion to vaccination programs hindered African response to COVID-19 [29].
2. Genetic Variants of SARS-CoV-2 Reported in Africa
Virus variants emerged since the outbreak and mostly affected the spike protein, which became the target of vaccine and monoclonal antibody production (Figure 1) [30][31]. The first variant was known as D614G. It appeared in April 2020, replacing the original SARS-CoV-2 by June 2020 [30][32]. A few months later, another variant was reported in the UK and was named Alpha (B.1.1.7) [32]. Many additional mutations occurred since then, showing distinct effects, in terms of infection spread and symptom severity, related to the affected region. In the spike protein, mutations like N501Y increased virus transmissibility [30]. Similar effects were also identified in variants affecting the non-spike and nucleocapsid regions, resulting in different sub-lineages [32]. South Africa was the incubator of the Beta variant (B.1.351) [32], a highly transmissible strain, sharing D614G and N501Y mutations with the Alpha variant. Unexpectedly, B.1.351 was less effectively neutralized by conventional therapies [30]. While the country was severely affected, Brazil reported a new variant, the Gamma (P.1) variant [33], causing an infection rate of approximately 75%. Mutations in the spike protein region [30][32] and in the amino-terminal domain [32] characterized P.1. This variant was not reported in Africa, raising concerns regarding how much sequencing the continent could afford. Nevertheless, the Delta variant (B.1.617.2) started to spread. From India, it reached Africa, where it significantly increased the morbidity and mortality rate of many fragile nations [3][34]. The same occurred with the Kappa (B.1.617.1) variant, although its transmissibility and number of sub-lineages were lower [32]. Despite all these mutations, the variant that prevailed in Africa was Omicron (B.1.1.529) [3][34][35][36]. The many genetic changes affecting Omicron [37] increased its infectivity [38], but reduced the risk of the virus causing severe clinical outcomes. Hence, this variant became less lethal [39]. Since then, different mutations were identified in Omicron and many sub-variants were reported [40][41][42]. Some emerged as lineage combinations, and their evolution is still closely followed.
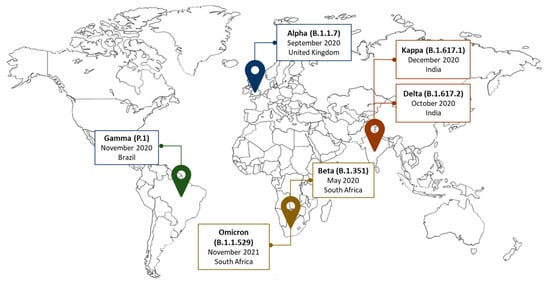
Figure 1. Variants of concern. RNA viruses, such as SARS-CoV-2, constantly evolve. Some mutations can provide the virus with a selective advantage, like increased transmissibility.
3. The Transmissibility of SARS-CoV-2 and the Difficulty of Applying Standardized Protection Measures in Africa
The fear of unprecedented mortality in Africa due to the COVID-19 pandemic grew exponentially when it was realized that the best healthcare provided in the developed world was not sufficient to stop the lethality of SARS-CoV-2. The virus was shown to replicate from 5 to 11 days [43][44]. Then, common symptoms, like fever, fatigue, and dry cough, began to appear [45]. Malaise and myalgias were also reported [46], as well as headache, abdominal pain, diarrhea, nausea, and vomiting [47]. While anosmia and ageusia were considered early markers of COVID-19 [46], shortness of breath was suggestive of a worsening disease stage [47]. Hence, protection measures to mitigate the infection started to be standardized. However, soon after their implementation, it became clear that they were designed for different realities than that in Africa. The virus was transmitted through close contact with infected individuals and the inhalation of viral-containing particles in the form of microscopic aerosols [48][49][50][51][52][53][54][55]. Thus, how could distance be maintained among people that mostly live of the informal sector or running small restoration businesses? How could home confinement be followed by people belonging to economically devasted communities, in which street selling remains the only source of sustenance? The difficulty of adopting standardized norms also referred to preventive measures of hygiene. Besides alcohol shortages, inequalities were highlighted even upon recommendations of simple actions, such as hand washing. In Africa, only one third of the population has regular access to clean water [56]. So, not stressing measures that required financial support to be implemented, many took for granted the privileges of living in developed countries. When scientific evidence found active viruses in biological samples, like urine [57][58] and feces [57][59][60][61], even after patient recovery [59][62], many concerns were raised in the continent, as most African citizens do not have access to private and clean sanitary facilities. Hence, viral infectivity was also expected to significantly grow because of open drains and squat toilets, lacking flushing water systems [63]. Accordingly, an enhanced number of cases started to be reported in countries where open defecation was a common practice. The lack of proper infrastructures for human waste management was seen as an additional risk for viral spreading [64]. This emphasized that despite the effort made to educate society on how to avoid infection, the applicability of many measures caused a double-edge feeling. The rules globally adopted contradicted many socioeconomic and cultural aspects associated with an increased risk of viral transmission, such as breastfeeding, which was referred as one of the routes for SARS-CoV-2 transmission [65]. In Africa, approximately 40% of infants are exclusively breastfed [66][67], a percentage below the WHO’s Global Nutrition Target of a 50% prevalence to be reached in 2025 [68]. The hypothesis that those women could have turned into disease incubators stood out. Concerns were also expressed in the case of intrauterine spreading [69], as the impact of COVID-19 became more evident in reproductive healthcare. In over 115 evaluated countries, including almost 50 African nations, maternal and child mortality rates increased monthly by 38.4% and 44%, respectively [70]. Nowadays, since COVID-19 does not pose a deadly threat to the world anymore, efforts should be made to evaluate Africa’s response to viral infectivity, teaching lessons for future outbreaks and promoting policies to leverage healthcare.
4. The Comorbidities Underlying COVID-19 Severity in Africa
Among the comorbidities enhancing the severity of COVID-19, non-communicable diseases were recognized worldwide as a prevalent risk factor for poor clinical outcomes. Their incidence in Africa is a major concern [34][71]. Non-communicable diseases are expected to be the primary cause of mortality in African nations by 2030 [72]. The Democratic Republic of the Congo, Nigeria, Ethiopia, and South Africa present the highest rates, considered as a potential explanation for the increased number of reported severe COVID-19 cases. According to the Global Burden of Disease studies, the incidence of non-communicable diseases in Africa has also been linked to the growing adoption of the Western lifestyle [73][74][75].
Among those pathologies, diabetes mellitus stood out [76]. In Africa, the number of diabetic individuals is 24 million and is projected to increase by 129% in 2045, reaching 55 million people [77]. Diabetic patients were more likely to manifest severe COVID-19 symptoms. Their compromised immune system, hypercoagulable pro-thrombotic state, endothelial dysfunction, and vascular inflammation [78] led to diabetes mellitus being a major contributor to COVID-19-induced complications and mortality [79][80][81][82]. According to WHO, during pandemic times, the fatality rate of diabetic patients was 10.2%, as assessed in 13 sub-Saharan countries. Conversely, in non-pandemic times, it was 2.5% [83].
Another risk factor for the appearance of severe COVID-19 symptoms was cardiovascular diseases [84]. Their prevalence varies from 0.1% in Sudan, where coronary events prevail, to 20% in Mozambique, where individuals mainly develop endomyocardial fibrosis [72]. Childhood rheumatic heart disease is also widespread in sub-Saharan Africa [85], ranging from 0.2% to 3% [86][87][88][89][90]. In terms of long-term sequelae, the occurrence of thrombosis and cardiorenal syndrome, upon COVID-19 infection, prevailed [91]. However, cardiovascular pathologies are also triggered by other highly prevalent infections, among which are HIV and tuberculosis [92], alerting of the difficulty in discriminating cardiovascular impairments caused by SARS-CoV-2 or other pathogens. In Africa, almost 50% of the individuals that suffer from tuberculosis show symptoms of pericarditis [72]. Its severity was significantly worsened by COVID-19 when individuals also carried HIV [93]. Similar results were even obtained in relation to the number of casualties [94]. Inflammation, elicited by SARS-CoV-2, exacerbated heart and blood vessel damage, as evidenced by the tropism of the virus for these cells [95][96]. Also, fibrosis-altered lung function and chronic obstructive pulmonary disease were reported as long-term COVID-19-induced sequelae in patients with tuberculosis [91][97][98]. Coinfections are prevalent in Africa. In the presence of different pathogens, the response to COVID-19 was impaired [34], as revealed in a study including 17,871 participants infected with SARS-CoV-2 [99].
Another concern drawing attention to severe COVID-19 symptomatology was obesity. According to WHO, 20% of adults and 10% of children and teenagers in South Africa, Nigeria, Mozambique, Uganda, Tanzania, Zambia, Zimbabwe, Kenya, Malawi, and Ethiopia, were expected to be classified as obese by December 2023 [100]. Although a causal relationship between obesity and COVID-19 was not fully established, evidence suggested they are strictly related. Hospitalized COVID-19 patients manifesting adult respiratory distress syndrome were often obese [101][102][103][104] and presented associated comorbidities [105]. However, differences in obesity epidemiology might have impacted the severity of COVID-19, especially when referring to urban regions. Most African people living in rural areas suffer from malnutrition, which is known to impair immune response and increase symptom severity [106]. In Angola, Liberia, Tanzania, Burkina Faso, Chad, Mali, Niger, Sudan, as well as in the Northern African region and Yemen, malnutrition and iron deficiency prevail, presumably justifying the high mortality caused by COVID-19 [107].
The prevalence of diseases related to disruption of iron metabolism also highlighted the possibility that deficiency of this metal might have played an important role in the fight against COVID-19 in Africa. Iron is a vital element, ensuring the development and survival of many organisms [108]. Viruses also need iron to proliferate, as it is required for the synthesis of their genetic material and energy production. Despite the lack of studies evaluating the correlation between iron levels and COVID-19 severity in Africa, numerous investigations were conducted in developed countries. In human volunteers, the exposure to norovirus was associated with the induction of hypoferremia, caused by an increased hepcidin, the hormone regulating iron absorption and circulating levels [109]. Dysregulation of iron homeostasis in COVID-19 patients was observed since the beginning of the outbreak [110]. The analyses of 99 patients, hospitalized in Wuhan Jinyintan Hospital with COVID-19-induced pneumonia, showed tissue iron overload and increased serum ferritin, the neutralizing protein storing iron within its subunits [111]. A higher production of pro-inflammatory cytokines directly linked to iron levels, like IL-1, IL-6, INF-γ, and TNF, was associated with a poor prognosis [112][113]. The cross-talk between inflammation and iron metabolism led researchers to investigate if hepcidin levels could predict the fatal outcome of COVID-19 infection [114]. Patients with hepcidin levels below 394 ng/mL were found to be more likely to survive. Higher levels of hepcidin were shown to increase inflammatory markers, like CRP and ferritin, as assessed in a descriptive study conducted with 5700 COVID-19 patients [103]. Hypoferremia was manifested in almost all ICU-admitted COVID-19 patients [115] and was associated with expression of organ damage markers, like aspartate aminotransferase-AST and lactic acid dehydrogenase-LDH [116][117]. Severe COVID-19 was also linked to low levels of hemoglobin, possibly as a consequence of the lower iron levels available for its synthesis. This negatively impacted erythrocyte production, as confirmed by the decrease in erythropoietin [118]. Its release also depends on the ability to sense hypoxia [117][119], and patients suffering from severe hypoxemia were found with lower levels of serum iron [120]. Given that the activation of immune cells relies on iron [119], low levels of this metal justified the impaired T cell response reported in COVID-19 patients [120][121].
5. Vaccine Inequity Distribution in Africa
Contrarily to the multiple vaccination rounds that developed countries benefited from, most African nations did not reach complete vaccination coverage (Figure 2) [122]. Several aspects contributed to the vaccine distribution inequity, including the poor social services taking care of vaccine storage, the conflicts and wars occurring in different countries, the internal migration issues and environmental degradation that hindered vaccine transportation, and a weak governance, violating human rights [3]. Many African countries also lacked the logistics necessary to receive and administer vaccines against SARS-CoV-2, some of which required low-temperature storage and efficient energy and power to maintain freezer functioning. The level of medical preparedness was a challenge. Contrarily to developed countries, the number of health care professionals able to plan, supervise, and follow vaccination procedures was low [3]. This hindered training new nurses and physicians, as the scarce qualified personnel were occupied with saving lives. Insufficient investment, even related to basic equipment and hospital beds, increased the vulnerability of Africa to COVID-19. However, the assumption that most SARS-CoV-2 infections in Africa were asymptomatic or associated with mild clinical symptoms contributed to the decision to regard the continent as a non-priority [122]. The disparity in vaccine distribution, as shown in the figure below, reflected the economic power of many countries and should have raised ethical concerns.
In Africa, vaccination programs began on 1 March 2021. The COVAX Facility, co-led by the Coalition for Epidemic Preparedness Innovations (CEPI), Gavi, the Vaccine Alliance, and WHO, secured around 2 billion doses. Vaccines were distributed by the end of the year [123][124], through the cooperation of the Africa Centers for Disease Control and Prevention, the African Union, and the WHO Regional Office for Africa. One of the biggest successes of this partnership was the acquisition of 400 million doses of the Johnson & Johnson single-dose vaccine before the end of 2022 [122]. The AstraZeneca vaccine was approved on 15 February 2021 [125] and had great repercussions in the continent due to its cost-effectiveness, ease of storage, and transportation [3]. It is therefore fair to highlight that it contributed to increasing the vaccination rate in Africa. The International Rescue Committee (IRC) estimated that the extra doses in the US, UK, and EU could have vaccinated individuals over 16 years old in the 20 countries most at risk of humanitarian disaster [126]. However, the multiple waves of COVID-19 reduced donations and caused vaccine shortage. On 19 March 2023, the African continent registered over 55 COVID-19 vaccine doses administered per 100 people, which was significantly lower when compared to the global average of over 167 doses per 100 people [127]. According to WHO, more than 1 billion doses have been administered in Africa, with 61% of them coming from COVAX, 27% from bilateral agreements, and 11% from the African Union’s African Vaccine Acquisition Trust (AVAT). The COVID-19 vaccines used in Africa include Janssen (35%), Pfizer/BioNTech (19%), AstraZeneca (15%), Sinopharm (13%), Sinovac (7%), Moderna (5%), and others (7%) [128]. So far, the African continent has achieved 36.7% coverage of COVID-19 vaccination among its population, which is significantly lower than the global coverage of 69.7% [127][128]. Sierra Leone and Botswana showed the highest level of immunization, reaching 96%, followed by Tunisia (94%) and Eswatini (93%). Conversely, Burundi, Namibia, and the Republic of Congo presented the lowest vaccination coverage, with 4%, 25%, and 26%, respectively. Eritrea is yet to start its COVID-19 vaccination campaign [128], as vaccine hesitancy in sub-Saharan Africa slowed the inoculation rate of COVID-19 vaccines. Some countries refused to participate in the COVAX free vaccine program or delayed vaccination programs due to anti-vaccine sentiments and religious beliefs [129]. Some donated vaccines with a short shelf life rapidly expired [130][131]. Yet, Africa is still vulnerable to new and more transmissible variants of SARS-CoV-2 that may require country-specific solutions [13][126]. The need for African countries to invest in medical science, so as to reduce scientific dependence and assistance from developed nations [3], led several agreements to share vaccine technology, as proposed by Moderna, WHO, BioNTech, and Afrigen Biologics and Vaccines in South Africa [132][133]. The manufacturing capacity was already assessed in Tunisia, Senegal, Egypt, Ethiopia, and South Africa. However, commercial capabilities require further development, given the need to reinforce business planning and market potential, since products produced in many African countries are not accepted in developed regions, as experienced by Rwanda. Whether lucrative markets and parallel importation may be the cause of competing conflicts, to overcome healthcare inequality, multilateral collaborations are required. Sustainable and innovative solutions are needed to overcome disease outbreaks [122], which include empowering the continent to accelerate vaccine manufacturing. Speeding up and encouraging local production, vaccines can be supplied in a timely manner, contributing to removing some of the inequities in the provision of essential health products [134]. In view of the creation of new expertise, this action will foster global collaborative research, which might also aid the discovery of therapeutic treatments better adjusted to the genetics of African individuals, while investigating the consequences of COVID-19 on diseases that are prevalent in the continent. Many pathologies were neglected during the pandemic and now are reemerging, such as measles in the Democratic Republic of Congo [135]. The decreased number of awareness campaigns [136] led to the false perception that the morbidity and mortality of certain pathologies were reduced, as was the case for HIV, cardiovascular diseases, and cervical cancers in Northern Ethiopia [137]. Blood bank services and malaria testing also decreased in Rwanda by almost 200%. Conversely, neonatal death dramatically increased in South Africa, as most personnel were occupied in saving the population from COVID-19 [138].
Finally, it is also worth mentioning that the impact of COVID-19 in Africa extended beyond public health, affecting social and economic aspects. Increased anxiety, social isolation, and stress characterized the pandemic period [3], potentially contributing to enhance domestic violence. Tunisia (43%), Somalia (50%), and South Africa (69%) registered the highest increases [139][140]. A higher risk of child labor and exploitation was also detected [141], possibly considered as a way for families to overcome the economic pressure imposed by the lockdown. These aspects contributed to a rise in the incidence of mental and psychosocial disorders [3], enhancing the vulnerability of this continent.
References
- United Nations World Population Prospects 2019: Highlights. Available online: https://population.un.org/wpp/Publications/Files/wpp2019_10KeyFindings.pdf (accessed on 9 April 2023).
- The Fund for Peace Global Data. Available online: https://fragilestatesindex.org/global-data/ (accessed on 19 March 2023).
- Bwire, G.; Ario, A.R.; Eyu, P.; Ocom, F.; Wamala, J.F.; Kusi, K.A.; Ndeketa, L.; Jambo, K.C.; Wanyenze, R.K.; Talisuna, A.O. The COVID-19 Pandemic in the African Continent. BMC Med. 2022, 20, 167.
- Udoakang, A.; Oboh, M.; Henry-Ajala, A.; Anyigba, C.; Omoleke, S.; Amambua-Ngwa, A.; Paemka, L.; Awandare, G.; Quashie, P. Low COVID-19 Impact in Africa: The Multifactorial Nexus. Open Res. Afr. 2021, 4, 47.
- Cilliers, J.; Kwasi, S.; Yeboua, K.; Oosthuizen, M.; Alexander, K.; Pooe, T.; Moyer, J. Impact of COVID-19 in Africa: A Scenario Analysis to 2030. SSRN Electron. J. 2020.
- Dong, E.; Du, H.; Gardner, L. An Interactive Web-Based Dashboard to Track COVID-19 in Real Time. Lancet Infect. Dis. 2020, 20, 533–534.
- El-Sadr, W.M.; Justman, J. Africa in the Path of COVID-19. N. Engl. J. Med. 2020, 383, e11.
- Mutombo, P.N.; Fallah, M.P.; Munodawafa, D.; Kabel, A.; Houeto, D.; Goronga, T.; Mweemba, O.; Balance, G.; Onya, H.; Kamba, R.S.; et al. COVID-19 Vaccine Hesitancy in Africa: A Call to Action. Lancet Glob. Health 2022, 10, e320–e321.
- Hussein, M.I.H.; Albashir, A.A.D.; Elawad, O.A.M.A.; Homeida, A. Malaria and COVID-19: Unmasking Their Ties. Malar. J. 2020, 19, 457.
- Yazdanbakhsh, M.; Kremsner, P.G.; Van Ree, R. Immunology: Allergy, Parasites, and the Hygiene Hypothesis. Science 2002, 296, 490–494.
- Arts, R.J.W.; Moorlag, S.J.C.F.M.; Novakovic, B.; Li, Y.; Wang, S.Y.; Oosting, M.; Kumar, V.; Xavier, R.J.; Wijmenga, C.; Joosten, L.A.B.; et al. BCG Vaccination Protects against Experimental Viral Infection in Humans through the Induction of Cytokines Associated with Trained Immunity. Cell Host Microbe 2018, 23, 89–100.e5.
- Rolot, M.; Dougall, A.M.; Chetty, A.; Javaux, J.; Chen, T.; Xiao, X.; Machiels, B.; Selkirk, M.E.; Maizels, R.M.; Hokke, C.; et al. Helminth-Induced IL-4 Expands Bystander Memory CD8+ T Cells for Early Control of Viral Infection. Nat. Commun. 2018, 9, 4516.
- Boum, Y.; Bebell, L.M.; Bisseck, A.-C.Z.-K. Africa Needs Local Solutions to Face the COVID-19 Pandemic. Lancet 2021, 397, 1238–1240.
- Nguimkeu, P.; Tadadjeu, S. Why Is the Number of COVID-19 Cases Lower than Expected in Sub-Saharan Africa? A Cross-Sectional Analysis of the Role of Demographic and Geographic Factors. World Dev. 2021, 138, 105251.
- Mwiinde, A.M.; Siankwilimba, E.; Sakala, M.; Banda, F.; Michelo, C. Climatic and Environmental Factors Influencing COVID-19 Transmission—An African Perspective. Trop. Med. Infect. Dis. 2022, 7, 433.
- Chan, K.H.; Peiris, J.S.M.; Lam, S.Y.; Poon, L.L.M.; Yuen, K.Y.; Seto, W.H. The Effects of Temperature and Relative Humidity on the Viability of the SARS Coronavirus. Adv. Virol. 2011, 2011, 734690.
- Sharif, N.; Sarkar, M.K.; Ahmed, S.N.; Ferdous, R.N.; Nobel, N.U.; Parvez, A.K.; Talukder, A.A.; Dey, S.K. Environmental Correlation and Epidemiologic Analysis of COVID-19 Pandemic in Ten Regions in Five Continents. Heliyon 2021, 7, e06576.
- Whittemore, P.B. COVID-19 Fatalities, Latitude, Sunlight, and Vitamin D. Am. J. Infect. Control 2020, 48, 1042–1044.
- Shao, L.; Ge, S.; Jones, T.; Santosh, M.; Silva, L.F.O.; Cao, Y.; Oliveira, M.L.S.; Zhang, M.; BéruBé, K. The Role of Airborne Particles and Environmental Considerations in the Transmission of SARS-CoV-2. Geosci. Front. 2021, 12, 101189.
- Adekunle, I.A.; Tella, S.A.; Oyesiku, K.O.; Oseni, I.O. Spatio-Temporal Analysis of Meteorological Factors in Abating the Spread of COVID-19 in Africa. Heliyon 2020, 6, e04749.
- Salyer, S.J.; Maeda, J.; Sembuche, S.; Kebede, Y.; Tshangela, A.; Moussif, M.; Ihekweazu, C.; Mayet, N.; Abate, E.; Ouma, A.O.; et al. The First and Second Waves of the COVID-19 Pandemic in Africa: A Cross-Sectional Study. Lancet 2021, 397, 1265–1275.
- World Health Organization (WHO). WHO Coronavirus (COVID-19) Dashboard. Available online: https://covid19.who.int/ (accessed on 3 November 2021).
- Diop, B.Z.; Ngom, M.; Pougué Biyong, C.; Pougué Biyong, J.N. The Relatively Young and Rural Population May Limit the Spread and Severity of COVID-19 in Africa: A Modelling Study. BMJ Glob. Health 2020, 5, e002699.
- World Data International Tourism: The Most Popular Countries. Available online: https://www.worlddata.info/tourism.php (accessed on 9 April 2023).
- Bradshaw, D.; Dorrington, R.; Moultrie, T.; Groenewald, P.; Moultrie, H. Underestimated COVID-19 Mortality in WHO African Region. Lancet Glob. Health 2022, 10, e1559.
- Chitungo, I.; Dzobo, M.; Hlongwa, M.; Dzinamarira, T. COVID-19: Unpacking the Low Number of Cases in Africa. Public Health Pract. 2020, 1, 100038.
- Lucero-Prisno, D.E.; Adebisi, Y.A.; Lin, X. Current Efforts and Challenges Facing Responses to 2019-NCoV in Africa. Glob. Health Res. Policy 2020, 5, 21.
- Jensen, N.; Kelly, A.H.; Avendano, M. The COVID-19 Pandemic Underscores the Need for an Equity-Focused Global Health Agenda. Humanit. Soc. Sci. Commun. 2021, 8, 15.
- Smolen, K.K.; Cai, B.; Gelinas, L.; Edgardo, S.; Iii, F.; Larsen, M.; Speert, D.P.; Cooper, P.J.; Esser, M.; Marchant, A.; et al. Single-Cell Analysis of Innate Cytokine Responses to Pattern Recognition Receptor Stimulation in Children across Four Continents. J. Immunol. 2014, 193, 3003–3012.
- Mascola, J.R.; Graham, B.S.; Fauci, A.S. SARS-CoV-2 Viral Variants—Tackling a Moving Target. JAMA 2021, 325, 1261–1262.
- Prévost, J.; Finzi, A. The Great Escape? SARS-CoV-2 Variants Evading Neutralizing Responses. Cell Host Microbe 2021, 29, 322–324.
- Tao, K.; Tzou, P.L.; Nouhin, J.; Gupta, R.K.; de Oliveira, T.; Kosakovsky Pond, S.L.; Fera, D.; Shafer, R.W. The Biological and Clinical Significance of Emerging SARS-CoV-2 Variants. Nat. Rev. Genet. 2021, 22, 757–773.
- World Health Organization (WHO) Tracking SARS-CoV-2 Variants. Available online: https://www.who.int/activities/tracking-SARS-CoV-2-variants (accessed on 24 January 2024).
- Tessema, S.K.; Nkengasong, J.N. Understanding COVID-19 in Africa. Nat. Rev. Immunol. 2021, 21, 469–470.
- Viana, R.; Moyo, S.; Amoako, D.G.; Tegally, H.; Scheepers, C.; Althaus, C.L.; Anyaneji, U.J.; Bester, P.A.; Boni, M.F.; Chand, M.; et al. Rapid Epidemic Expansion of the SARS-CoV-2 Omicron Variant in Southern Africa. Nature 2022, 603, 679–686.
- Gao, S.-J.; Guo, H.; Luo, G. Omicron Variant (B.1.1.529) of SARS-CoV-2, a Global Urgent Public Health Alert! J. Med. Virol. 2022, 94, 1255–1256.
- Chang, D.; Chang, X.; He, Y.; Tan, K.J.K. The Determinants of COVID-19 Morbidity and Mortality across Countries. Sci. Rep. 2022, 12, 5888.
- Ma, Q.; Liu, J.; Liu, Q.; Kang, L.; Liu, R.; Jing, W.; Wu, Y.; Liu, M. Global Percentage of Asymptomatic SARS-CoV-2 Infections Among the Tested Population and Individuals with Confirmed COVID-19 Diagnosis: A Systematic Review and Meta-Analysis. JAMA Netw. Open 2021, 4, e2137257.
- Christie, B. COVID-19: Early Studies Give Hope Omicron Is Milder than Other Variants. BMJ 2021, 375, n3144.
- World Health Organization (WHO). TAG-VE Statement on the Meeting of 3 January on the COVID-19 Situation in China. Available online: https://www.who.int/news/item/04-01-2023-tag-ve-statement-on-the-3rd-january-meeting-on-the-covid-19-situation-in-china (accessed on 9 April 2023).
- Cao, Y.; Jian, F.; Wang, J.; Yu, Y.; Song, W.; Yisimayi, A.; Wang, J.; An, R.; Chen, X.; Zhang, N.; et al. Imprinted SARS-CoV-2 Humoral Immunity Induces Convergent Omicron RBD Evolution. Nature 2023, 614, 521–529.
- Sun, Y.; Wang, M.; Lin, W.; Dong, W.; Xu, J. Evolutionary Analysis of Omicron Variant BF.7 and BA.5.2 Pandemic in China. J. Biosaf. Biosecur. 2023, 5, 14–20.
- Bai, Y.; Yao, L.; Wei, T.; Tian, F.; Jin, D.-Y.; Chen, L.; Wang, M. Presumed Asymptomatic Carrier Transmission of COVID-19. JAMA 2020, 323, 1406–1407.
- Lauer, S.A.; Grantz, K.H.; Bi, Q.; Jones, F.K.; Zheng, Q.; Meredith, H.R.; Azman, A.S.; Reich, N.G.; Lessler, J. The Incubation Period of Coronavirus Disease 2019 (COVID-19) From Publicly Reported Confirmed Cases: Estimation and Application. Ann. Intern. Med. 2020, 172, 577–582.
- Azkur, A.K.; Akdis, M.; Azkur, D.; Sokolowska, M.; van de Veen, W.; Brüggen, M.-C.; O’Mahony, L.; Gao, Y.; Nadeau, K.; Akdis, C.A. Immune Response to SARS-CoV-2 and Mechanisms of Immunopathological Changes in COVID-19. Allergy 2020, 75, 1564–1581.
- Gandhi, R.T.; Lynch, J.B.; del Rio, C. Mild or Moderate COVID-19. N. Engl. J. Med. 2020, 383, 1757–1766.
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA-J. Am. Med. Assoc. 2020, 323, 1061–1069.
- Liu, J.; Liao, X.; Qian, S.; Yuan, J.; Wang, F.; Liu, Y.; Wang, Z.; Wang, F.-S.; Liu, L.; Zhang, Z. Community Transmission of Severe Acute Respiratory Syndrome Coronavirus 2, Shenzhen, China, 2020. Emerg. Infect. Dis. 2020, 26, 1320–1323.
- Chan, J.F.-W.; Yuan, S.; Kok, K.-H.; To, K.K.-W.; Chu, H.; Yang, J.; Xing, F.; Liu, J.; Yip, C.C.-Y.; Poon, R.W.-S.; et al. A Familial Cluster of Pneumonia Associated with the 2019 Novel Coronavirus Indicating Person-to-Person Transmission: A Study of a Family Cluster. Lancet 2020, 395, 514–523.
- Burke, R.M.; Midgley, C.M.; Dratch, A.; Fenstersheib, M.; Haupt, T.; Holshue, M.; Ghinai, I.; Jarashow, M.C.; Lo, J.; McPherson, T.D.; et al. Active Monitoring of Persons Exposed to Patients with Confirmed COVID-19-United States, January-February 2020. MMWR Morb. Mortal. Wkly. Rep. 2020, 69, 245–246.
- van Doremalen, N.; Bushmaker, T.; Morris, D.H.; Holbrook, M.G.; Gamble, A.; Williamson, B.N.; Tamin, A.; Harcourt, J.L.; Thornburg, N.J.; Gerber, S.I.; et al. Aerosol and Surface Stability of SARS-CoV-2 as Compared with SARS-CoV-1. N. Engl. J. Med. 2020, 382, 1564–1567.
- Van Damme, W.; Dahake, R.; van de Pas, R.; Vanham, G.; Assefa, Y. COVID-19: Does the Infectious Inoculum Dose-Response Relationship Contribute to Understanding Heterogeneity in Disease Severity and Transmission Dynamics? Med. Hypotheses 2021, 146, 110431.
- Gralton, J.; Tovey, E.R.; McLaws, M.-L.; Rawlinson, W.D. Respiratory Virus RNA Is Detectable in Airborne and Droplet Particles. J. Med. Virol. 2013, 85, 2151–2159.
- Somsen, G.A.; van Rijn, C.; Kooij, S.; Bem, R.A.; Bonn, D. Small Droplet Aerosols in Poorly Ventilated Spaces and SARS-CoV-2 Transmission. Lancet Respir. Med. 2020, 8, 658–659.
- Stadnytskyi, V.; Bax, C.E.; Bax, A.; Anfinrud, P. The Airborne Lifetime of Small Speech Droplets and Their Potential Importance in SARS-CoV-2 Transmission. Proc. Natl. Acad. Sci. USA 2020, 117, 11875.
- UNICEF. Water Security for All; UNICEF: New York, NY, USA, 2021.
- Guan, W.; Ni, Z.; Hu, Y.; Liang, W.; Ou, C.; He, J.; Liu, L.; Shan, H.; Lei, C.; Hui, D.S.C.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720.
- Peng, L.; Liu, J.; Xu, W.; Luo, Q.; Chen, D.; Lei, Z.; Huang, Z.; Li, X.; Deng, K.; Lin, B.; et al. SARS-CoV-2 Can Be Detected in Urine, Blood, Anal Swabs, and Oropharyngeal Swabs Specimens. J. Med. Virol. 2020, 92, 1676–1680.
- Wu, Y.; Guo, C.; Tang, L.; Hong, Z.; Zhou, J.; Dong, X.; Yin, H.; Xiao, Q.; Tang, Y.; Qu, X.; et al. Prolonged Presence of SARS-CoV-2 Viral RNA in Faecal Samples. Lancet Gastroenterol. Hepatol. 2020, 5, 434–435.
- Wang, W.; Xu, Y.; Gao, R.; Lu, R.; Han, K.; Wu, G.; Tan, W. Detection of SARS-CoV-2 in Different Types of Clinical Specimens. JAMA 2020, 323, 1843–1844.
- Xiao, F.; Tang, M.; Zheng, X.; Liu, Y.; Li, X.; Shan, H. Evidence for Gastrointestinal Infection of SARS-CoV-2. Gastroenterology 2020, 158, 1831–1833.e3.
- Zheng, S.; Fan, J.; Yu, F.; Feng, B.; Lou, B.; Zou, Q.; Xie, G.; Lin, S.; Wang, R.; Yang, X.; et al. Viral Load Dynamics and Disease Severity in Patients Infected with SARS-CoV-2 in Zhejiang Province, China, January-March 2020: Retrospective Cohort Study. BMJ 2020, 369, m1443.
- UNICEF; World Health Organization (WHO). Progress on Drinking Water, Sanitation and Hygiene 2000–2017; UNICEF: New York, NY, USA, 2019.
- Sun, S.; Han, J. Open Defecation and Squat Toilets, an Overlooked Risk of Fecal Transmission of COVID-19 and Other Pathogens in Developing Communities. Environ. Chem. Lett. 2021, 19, 787–795.
- World Health Organization. Breastfeeding and COVID-19: WHO Scientific Brief; World Health Organization: Geneva, Switzerland, 2020; pp. 1–3.
- Bhattacharjee, N.V.; Schaeffer, L.E.; Marczak, L.B.; Ross, J.M.; Swartz, S.J.; Albright, J.; Gardner, W.M.; Shields, C.; Sligar, A.; Schipp, M.F.; et al. Mapping Exclusive Breastfeeding in Africa between 2000 and 2017. Nat. Med. 2019, 25, 1205–1212.
- Bhattacharjee, N.V.; Schaeffer, L.E.; Hay, S.I.; Lu, D.; Schipp, M.F.; Lazzar-Atwood, A.; Donkers, K.M.; Abady, G.G.; Abd-Allah, F.; Abdelalim, A.; et al. Mapping Inequalities in Exclusive Breastfeeding in Low- and Middle-Income Countries, 2000–2018. Nat. Hum. Behav. 2021, 5, 1027–1045.
- World Health Organization (WHO); UNICEF. Global Nutrition Targets 2025: Breastfeeding Policy Brief; World Health Organization: Geneva, Switzerland, 2014.
- Dong, L.; Tian, J.; He, S.; Zhu, C.; Wang, J.; Liu, C.; Yang, J. Possible Vertical Transmission of SARS-CoV-2 From an Infected Mother to Her Newborn. JAMA 2020, 323, 1846–1848.
- Alabi, Q.K.; Oyedeji, A.S.; Kayode, O.O.; Kajewole-Alabi, D.I. Impact of COVID-19 Pandemic on Mother and Child Health in Sub-Saharan Africa—A Review. Pediatr. Res. 2023, 94, 1278–1283.
- Lawal, Y. Africa’s Low COVID-19 Mortality Rate: A Paradox? Int. J. Infect. Dis. 2021, 102, 118–122.
- Dalal, S.; Beunza, J.J.; Volmink, J.; Adebamowo, C.; Bajunirwe, F.; Njelekela, M.; Mozaffarian, D.; Fawzi, W.; Willett, W.; Adami, H.-O.; et al. Non-Communicable Diseases in Sub-Saharan Africa: What We Know Now. Int. J. Epidemiol. 2011, 40, 885–901.
- World Health Organization (WHO). Deaths from Noncommunicable Diseases on the Rise in Africa. Available online: https://www.afro.who.int/news/deaths-noncommunicable-diseases-rise-africa (accessed on 9 April 2023).
- Ajaero, C.K.; De Wet-Billings, N.; Atama, C.; Agwu, P.; Eze, E.J. The Prevalence and Contextual Correlates of Non-Communicable Diseases among Inter-Provincial Migrants and Non-Migrants in South Africa. BMC Public Health 2021, 21, 999.
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global Burden of 369 Diseases and Injuries in 204 Countries and Territories, 1990-2019: A Systematic Analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396, 1204–1222.
- Cole, J.B.; Florez, J.C. Genetics of Diabetes Mellitus and Diabetes Complications. Nat. Rev. Nephrol. 2020, 16, 377–390.
- World Health Organization (WHO). African Region Tops World in Undiagnosed Diabetes: WHO Analysis. Available online: https://www.afro.who.int/news/african-region-tops-world-undiagnosed-diabetes-who-analysis (accessed on 28 March 2023).
- Anjorin, A.A.; Abioye, A.I.; Asowata, O.E.; Soipe, A.; Kazeem, M.I.; Adesanya, I.O.; Raji, M.A.; Adesanya, M.; Oke, F.A.; Lawal, F.J.; et al. Comorbidities and the COVID-19 Pandemic Dynamics in Africa. Trop. Med. Int. Health 2021, 26, 2–13.
- Schoen, K.; Horvat, N.; Guerreiro, N.F.C.; de Castro, I.; de Giassi, K.S. Spectrum of Clinical and Radiographic Findings in Patients with Diagnosis of H1N1 and Correlation with Clinical Severity. BMC Infect. Dis. 2019, 19, 964.
- Banik, G.R.; Alqahtani, A.S.; Booy, R.; Rashid, H. Risk Factors for Severity and Mortality in Patients with MERS-CoV: Analysis of Publicly Available Data from Saudi Arabia. Virol. Sin. 2016, 31, 81–84.
- Yang, J.K.; Feng, Y.; Yuan, M.Y.; Yuan, S.Y.; Fu, H.J.; Wu, B.Y.; Sun, G.Z.; Yang, G.R.; Zhang, X.L.; Wang, L.; et al. Plasma Glucose Levels and Diabetes Are Independent Predictors for Mortality and Morbidity in Patients with SARS. Diabet. Med. 2006, 23, 623–628.
- Hussain, A.; Bhowmik, B.; do Vale Moreira, N.C. COVID-19 and Diabetes: Knowledge in Progress. Diabetes Res. Clin. Pract. 2020, 162, 108142.
- Burki, T. COVID-19 and Diabetes in Africa: A Lethal Combination. Lancet Diabetes Endocrinol. 2022, 10, 23.
- Kerolos, M.M.; Ruge, M.; Gill, A.; Planek, M.I.; Volgman, A.S.; Du-Fay-De-Lavallaz, J.M.; Gomez, J.M.D.; Suboc, T.M.; Williams, K.A.; Abusin, S. Clinical Outcomes of COVID-19 Infection in Patients with Pre-Existing Cardiovascular Disease. Am. Heart J. Plus Cardiol. Res. Pract. 2022, 20, 100189.
- Nkomo, V.T. Epidemiology and Prevention of Valvular Heart Diseases and Infective Endocarditis in Africa. Heart 2007, 93, 1510.
- Anabwani, G.M.; Amoa, A.B.; Muita, A.K. Epidemiology of Rheumatic Heart Disease among Primary School Children in Western Kenya. Int. J. Cardiol. 1989, 23, 249–252.
- McLaren, M.J.; Hawkins, D.M.; Koornhof, H.J.; Bloom, K.R.; Bramwell-Jones, D.M.; Cohen, E.; Gale, G.E.; Kanarek, K.; Lachman, A.S.; Lakier, J.B.; et al. Epidemiology of Rheumatic Heart Disease in Black Shcoolchildren of Soweto, Johannesburg. Br. Med. J. 1975, 3, 474.
- Marijon, E.; Ou, P.; Celermajer, D.S.; Ferreira, B.; Mocumbi, A.O.; Jani, D.; Paquet, C.; Jacob, S.; Sidi, D.; Jouven, X. Prevalence of Rheumatic Heart Disease Detected by Echocardiographic Screening. N. Engl. J. Med. 2007, 357, 470–476.
- Ibrahim-Khalil, S.; Elhag, M.; Ali, E.; Mahgoub, F.; Hakiem, S.; Omer, N.; Shafie, S.; Mahgoub, E. An Epidemiological Survey of Rheumatic Fever and Rheumatic Heart Disease in Sahafa Town, Sudan. J. Epidemiol. Community Health 1992, 46, 477.
- Oli, K.; Tekle-Haimanot, R.; Forsgren, L.; Ekstedt, J. Rheumatic Heart Disease Prevalence among Schoolchildren of an Ethiopian Rural Town. Cardiology 1992, 80, 152–155.
- Nyasulu, P.S.; Tamuzi, J.L.; Erasmus, R.T. Burden, Causation, and Particularities of Long-COVID in African Populations: A Rapid Systematic Review. medRxiv 2023.
- Margolin, E.; Burgers, W.A.; Sturrock, E.D.; Mendelson, M.; Chapman, R.; Douglass, N.; Williamson, A.-L.; Rybicki, E.P. Prospects for SARS-CoV-2 Diagnostics, Therapeutics and Vaccines in Africa. Nat. Rev. Microbiol. 2020, 18, 690–704.
- Western Cape Department of Health in Collaboration with the National Institute for Communicable; Diseases, S.A. Risk Factors for Coronavirus Disease 2019 (COVID-19) Death in a Population Cohort Study from the Western Cape Province, South Africa. Clin. Infect. Dis. 2021, 73, e2005.
- Motta, I.; Centis, R.; D’Ambrosio, L.; García-García, J.-M.; Goletti, D.; Gualano, G.; Lipani, F.; Palmieri, F.; Sánchez-Montalvá, A.; Pontali, E.; et al. Tuberculosis, COVID-19 and Migrants: Preliminary Analysis of Deaths Occurring in 69 Patients from Two Cohorts. Pulmonology 2020, 26, 233–240.
- Nägele, F.; Graber, M.; Hirsch, J.; Pölzl, L.; Sahanic, S.; Fiegl, M.; Hau, D.; Engler, C.; Lechner, S.; Stalder, A.K.; et al. Correlation between Structural Heart Disease and Cardiac SARS-CoV-2 Manifestations. Commun. Med. 2022, 2, 142.
- Tomasoni, D.; Italia, L.; Adamo, M.; Inciardi, R.M.; Lombardi, C.M.; Solomon, S.D.; Metra, M. COVID-19 and Heart Failure: From Infection to Inflammation and Angiotensin II Stimulation. Searching for Evidence from a New Disease. Eur. J. Heart Fail. 2020, 22, 957–966.
- Omoush, S.A.; Alzyoud, J.A.M. The Prevalence and Impact of Coinfection and Superinfection on the Severity and Outcome of COVID-19 Infection: An Updated Literature Review. Pathogens 2022, 11, 445.
- Blanco, J.-R.; Cobos-Ceballos, M.-J.; Navarro, F.; Sanjoaquin, I.; Arnaiz de las Revillas, F.; Bernal, E.; Buzon-Martin, L.; Viribay, M.; Romero, L.; Espejo-Perez, S.; et al. Pulmonary Long-Term Consequences of COVID-19 Infections after Hospital Discharge. Clin. Microbiol. Infect. 2021, 27, 892–896.
- Raisi-Estabragh, Z.; Cooper, J.; Salih, A.; Raman, B.; Lee, A.M.; Neubauer, S.; Harvey, N.C.; Petersen, S.E. Cardiovascular Disease and Mortality Sequelae of COVID-19 in the UK Biobank. Heart 2023, 109, 119.
- World Health Organization (WHO). Obesity Rising in Africa, WHO Analysis Finds. Available online: https://www.afro.who.int/news/obesity-rising-africa-who-analysis-finds (accessed on 12 March 2023).
- Arentz, M.; Yim, E.; Klaff, L.; Lokhandwala, S.; Riedo, F.X.; Chong, M.; Lee, M. Characteristics and Outcomes of 21 Critically Ill Patients With COVID-19 in Washington State. JAMA 2020, 323, 1612–1614.
- Bhatraju, P.K.; Ghassemieh, B.J.; Nichols, M.; Kim, R.; Jerome, K.R.; Nalla, A.K.; Greninger, A.L.; Pipavath, S.; Wurfel, M.M.; Evans, L.; et al. COVID-19 in Critically Ill Patients in the Seattle Region—Case Series. N. Engl. J. Med. 2020, 382, 2012–2022.
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; Cohen, S.L.; et al. Presenting Characteristics, Comorbidities, and Outcomes Among 5700 Patients Hospitalized With COVID-19 in the New York City Area. JAMA 2020, 323, 2052–2059.
- Nakeshbandi, M.; Maini, R.; Daniel, P.; Rosengarten, S.; Parmar, P.; Wilson, C.; Kim, J.M.; Oommen, A.; Mecklenburg, M.; Salvani, J.; et al. The Impact of Obesity on COVID-19 Complications: A Retrospective Cohort Study. Int. J. Obes. 2020, 44, 1832–1837.
- Nagy, É.; Cseh, V.; Barcs, I.; Ludwig, E. The Impact of Comorbidities and Obesity on the Severity and Outcome of COVID-19 in Hospitalized Patients—A Retrospective Study in a Hungarian Hospital. Int. J. Environ. Res. Public Health 2023, 20, 1372.
- Katona, P.; Katona-Apte, J. The Interaction between Nutrition and Infection. Clin. Infect. Dis. 2008, 46, 1582–1588.
- Mertens, E.; Peñalvo, J.L. The Burden of Malnutrition and Fatal COVID-19: A Global Burden of Disease Analysis. Front. Nutr. 2021, 7, 351.
- Menshawey, R.; Menshawey, E.; Alserr, A.H.K.; Abdelmassih, A.F. Low Iron Mitigates Viral Survival: Insights from Evolution, Genetics, and Pandemics—A Review of Current Hypothesis. Egypt. J. Med. Hum. Genet. 2020, 21, 75.
- Williams, A.M.; Ladva, C.N.; Leon, J.S.; Lopman, B.A.; Tangpricha, V.; Whitehead, R.D.; Armitage, A.E.; Wray, K.; Morovat, A.; Pasricha, S.R.; et al. Changes in Micronutrient and Inflammation Serum Biomarker Concentrations after a Norovirus Human Challenge. Am. J. Clin. Nutr. 2019, 110, 1456–1464.
- Cavezzi, A.; Troiani, E.; Corrao, S. COVID-19: Hemoglobin, Iron, and Hypoxia beyond Inflammation. A Narrative Review. Clin. Pract. 2020, 10, 1271.
- Chen, N.; Zhou, M.; Dong, X.; Qu, J.; Gong, F.; Han, Y.; Qiu, Y.; Wang, J.; Liu, Y.; Wei, Y.; et al. Epidemiological and Clinical Characteristics of 99 Cases of 2019 Novel Coronavirus Pneumonia in Wuhan, China: A Descriptive Study. Lancet 2020, 395, 507–513.
- Chen, X.; Zhao, B.; Qu, Y.; Chen, Y.; Xiong, J.; Feng, Y.; Men, D.; Huang, Q.; Liu, Y.; Yang, B.; et al. Detectable Serum Severe Acute Respiratory Syndrome Coronavirus 2 Viral Load (RNAemia) Is Closely Correlated with Drastically Elevated Interleukin 6 Level in Critically Ill Patients with Coronavirus Disease 2019. Clin. Infect. Dis. 2020, 71, 1937–1942.
- Liu, B.; Li, M.; Zhou, Z.; Guan, X.; Xiang, Y. Can We Use Interleukin-6 (IL-6) Blockade for Coronavirus Disease 2019 (COVID-19)-Induced Cytokine Release Syndrome (CRS)? J. Autoimmun. 2020, 111, 102452.
- Martins, A.C.; Almeida, J.I.; Lima, I.S.; Kapitão, A.S.; Gozzelino, R. Iron Metabolism and the Inflammatory Response. IUBMB Life 2017, 69, 442–450.
- Alipour, R.; Hashemi, S.H.; Mikaeili, F. Serum Iron Level in Patients with COVID-19: A Case Report Study. Int. J. Res. Med. Sci. 2020, 8, 2658.
- Nai, A.; Lorè, N.I.; Pagani, A.; De Lorenzo, R.; Di Modica, S.; Saliu, F.; Cirillo, D.M.; Rovere-Querini, P.; Manfredi, A.A.; Silvestri, L. Hepcidin Levels Predict COVID-19 Severity and Mortality in a Cohort of Hospitalized Italian Patients. Am. J. Hematol. 2021, 96, E32–E35.
- Ganz, T. Anemia of Inflammation. N. Engl. J. Med. 2019, 381, 1148–1157.
- Yağcı, S.; Serin, E.; Acicbe, Ö.; Zeren, M.İ.; Odabaşı, M.S. The Relationship between Serum Erythropoietin, Hepcidin, and Haptoglobin Levels with Disease Severity and Other Biochemical Values in Patients with COVID-19. Int. J. Lab. Hematol. 2021, 43, 142–151.
- Litton, E.; Lim, J. Iron Metabolism: An Emerging Therapeutic Target in Critical Illness. Crit. Care 2019, 2019, 573–584.
- Shah, A.; Frost, J.N.; Aaron, L.; Donovan, K.; Drakesmith, H.; McKechnie, S.R.; Stanworth, S.J. Systemic Hypoferremia and Severity of Hypoxemic Respiratory Failure in COVID-19. Crit. Care 2020, 24, 320.
- Bu, X.; Yao, Y.; Li, X. Immune Checkpoint Blockade in Breast Cancer Therapy. In Advances in Experimental Medicine and Biology; Springer: Berlin/Heidelberg, Germany, 2017.
- The Lancet. COVID-19 in Africa: A Lesson in Solidarity. Lancet 2021, 398, 185.
- Herzog, L.M.; Norheim, O.F.; Emanuel, E.J.; McCoy, M.S. Covax Must Go beyond Proportional Allocation of COVID Vaccines to Ensure Fair and Equitable Access. BMJ 2021, 372, m4853.
- World Health Organization (WHO). Fair Allocation Mechanism for COVID-19 Vaccines through the COVAX Facility. Available online: https://www.who.int/publications/m/item/fair-allocation-mechanism-for-covid-19-vaccines-through-the-covax-facility (accessed on 9 April 2023).
- World Health Organization (WHO). WHO Lists Two Additional COVID-19 Vaccines for Emergency Use and COVAX Roll-Out. Available online: https://www.who.int/news/item/15-02-2021-who-lists-two-additional-covid-19-vaccines-for-emergency-use-and-covax-roll-out (accessed on 1 February 2023).
- Mwai, P. COVID-19 Africa: Who Is Getting the Vaccine? Available online: https://www.bbc.com/news/56100076 (accessed on 2 April 2021).
- Our World in Data Coronavirus (COVID-19) Vaccinations. Available online: https://ourworldindata.org/covid-vaccinations#what-share-of-the-population-has-received-at-least-one-dose-of-vaccine (accessed on 19 March 2023).
- World Health Organization (WHO). Africa COVID-19 Vaccination Dashboard. Available online: https://app.powerbi.com/view?r=eyJrIjoiOTI0ZDlhZWEtMjUxMC00ZDhhLWFjOTYtYjZlMGYzOWI4NGIwIiwidCI6ImY2MTBjMGI3LWJkMjQtNGIzOS04MTBiLTNkYzI4MGFmYjU5MCIsImMiOjh9 (accessed on 9 April 2023).
- Kabakama, S.; Konje, E.T.; Dinga, J.N.; Kishamawe, C.; Morhason-Bello, I.; Hayombe, P.; Adeyemi, O.; Chimuka, E.; Lumu, I.; Amuasi, J.; et al. Commentary on COVID-19 Vaccine Hesitancy in Sub-Saharan Africa. Trop. Med. Infect. Dis. 2022, 7, 130.
- World Health Organization (WHO). Joint Statement on Dose Donations of COVID-19 Vaccines to African Countries. Available online: https://www.who.int/news/item/29-11-2021-joint-statement-on-dose-donations-of-covid-19-vaccines-to-african-countries (accessed on 9 April 2023).
- World Health Organization (WHO). Strategy to Achieve Global COVID-19 Vaccination by Mid-2022. Available online: https://www.who.int/publications/m/item/strategy-to-achieve-global-covid-19-vaccination-by-mid-2022 (accessed on 1 February 2023).
- Nature. Africa Is Bringing Vaccine Manufacturing Home. Nature 2022, 602, 184.
- Paton, J. BioNTech to Send COVID Vaccine Production Units to Africa. Available online: https://www.bloomberg.com/news/articles/2022-02-16/biontech-to-send-covid-vaccine-production-units-to-africa#xj4y7vzkg (accessed on 12 March 2023).
- Wellcome. Scaling Up African Vaccine Manufacturing Capacity. Available online: https://cms.wellcome.org/sites/default/files/2023-01/Wellcome-Biovac-BCG-Scaling-up-African-vaccine-manufacturing-capacity-report-2023_0.pdf (accessed on 24 January 2024).
- World Health Organization (WHO). Africa Continued Delivery of Immunization Services in the Context of COVID-19 Pandemic. Available online: https://www.afro.who.int/news/continued-delivery-immunization-services-context-covid-19-pandemic (accessed on 28 March 2023).
- Hakizimana, D.; Ntizimira, C.; Mbituyumuremyi, A.; Hakizimana, E.; Mahmoud, H.; Birindabagabo, P.; Musanabaganwa, C.; Gashumba, D. The Impact of COVID-19 on Malaria Services in Three High Endemic Districts in Rwanda: A Mixed-Method Study. Malar. J. 2022, 21, 48.
- Desta, A.A.; Woldearegay, T.W.; Gebremeskel, E.; Alemayehu, M.; Getachew, T.; Gebregzabiher, G.; Ghebremedhin, K.D.; Zgita, D.N.; Aregawi, A.B.; Redae, G. Impacts of COVID-19 on Essential Health Services in Tigray, Northern Ethiopia: A Pre-Post Study. PLoS ONE 2021, 16, e0256330.
- Jensen, C.; McKerrow, N.H. Child Health Services during a COVID-19 Outbreak in KwaZulu-Natal Province, South Africa. S. Afr. Med. J. 2020, 111, 114.
- Harvey, R. The Ignored Pandemic: The Dual Crises of Gender-Based Violence and COVID-19; Oxfam: Oxford, UK, 2021.
- Mednick, S. COVID-19 Brings Abuse and Other Fears to Displaced Women in South Sudan. Available online: https://www.thenewhumanitarian.org/feature/2020/05/06/coronavirus-south-sudan-women-abuse-gender-violence (accessed on 24 January 2024).
- International Labour Organization. COVID-19 Impact on Child Labour and Forced Labour: The Response of the IPEC+ Flagship Programme; International Labour Organization: Geneva, Switzerland, 2020.
More
Information
Subjects:
Health Care Sciences & Services
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.5K
Entry Collection:
COVID-19
Revisions:
2 times
(View History)
Update Date:
07 May 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





