You're using an outdated browser. Please upgrade to a modern browser for the best experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Francesco Nappi | -- | 2806 | 2022-10-23 17:55:33 | | | |
| 2 | Sirius Huang | Meta information modification | 2806 | 2022-10-25 02:32:35 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Nappi, F.; Giacinto, O.; Lusini, M.; Garo, M.; Caponio, C.; Nenna, A.; Nappi, P.; Rousseau, J.; Spadaccio, C.; Chello, M. Patients with Bicuspid Aortopathy and Aortic Dilatation. Encyclopedia. Available online: https://encyclopedia.pub/entry/30745 (accessed on 28 December 2025).
Nappi F, Giacinto O, Lusini M, Garo M, Caponio C, Nenna A, et al. Patients with Bicuspid Aortopathy and Aortic Dilatation. Encyclopedia. Available at: https://encyclopedia.pub/entry/30745. Accessed December 28, 2025.
Nappi, Francesco, Omar Giacinto, Mario Lusini, Marialuisa Garo, Claudio Caponio, Antonio Nenna, Pierluigi Nappi, Juliette Rousseau, Cristiano Spadaccio, Massimo Chello. "Patients with Bicuspid Aortopathy and Aortic Dilatation" Encyclopedia, https://encyclopedia.pub/entry/30745 (accessed December 28, 2025).
Nappi, F., Giacinto, O., Lusini, M., Garo, M., Caponio, C., Nenna, A., Nappi, P., Rousseau, J., Spadaccio, C., & Chello, M. (2022, October 23). Patients with Bicuspid Aortopathy and Aortic Dilatation. In Encyclopedia. https://encyclopedia.pub/entry/30745
Nappi, Francesco, et al. "Patients with Bicuspid Aortopathy and Aortic Dilatation." Encyclopedia. Web. 23 October, 2022.
Copy Citation
Bicuspid aortic valve (BAV) is the most frequent congenital cardiac disease. Alteration of ascending aorta diameter is a consequence of shear stress alterations due to haemodynamic abnormalities developed from inadequate valve cusp coaptation.
bicuspid aortic valve
aortopathy
classification
1. Introduction
Bicuspid aortic valve (BAV) is the most frequent congenital cardiac pathology; has a prevalence of 1–2% [1], a high incidence of adverse outcomes, especially aortic stenosis (AS) and aortic regurgitation (MR) [2]; and is at least three times more common in males than females [3].
Bicuspid aortopathy, reported in 50% of BAV patients, consists of the aorta enlargement starting from the aortic root and involving the aortic arch and depends on blood flux turbulences characterized by power vectors directed against the aortic toot and the convexity of the vessel [4][5][6][7]. Recently, micro-RNA (miRNA) has been studied regarding post-transcriptional regulation of genes in aortopathy manifestation. [8][9].
2. Genetics and Molecular Biology
Estimating mutation genes and their inheritance patterns is challenging [7] because locus 9q34.3 alteration causes mutations in regulators NOTCH1 with secondary pathological aortic valve development [10][11]; gene damages on 18q, 5q, and 13q induces BAV [12]; and finally, damages to the smooth muscle alfa actine (ACTA 2) gene produce BAV and aortic aneurysms [13].
There is a tight linkage between BAV expression and other congenital pathologies such as the coarctation of the aorta. Concerning BAV phenotype, Shone’s syndrome with a left-sided lesion that can cause inflow and outflow obstruction, Turner’s syndrome with aortic coarctation, and William’s syndrome involving supravalvular stenosis may be observed. Moreover, ventricular septal defect, atrial septal defect, patent ductus arteriosus, and coronary vessels, which may mainly involve single coronary and reversal coronary dominance, have been reported [14][15][16].
Micro-RNAs (MiRNAs) need to be considered in biochemical and molecular changes in BAV and aorthopathy (Table 1). MiRNAs are small, single-stranded, noncoding RNA molecules that determine the post-transcriptional regulation of gene expression. The effects of miRNAs are the result of base pairing with complementary sequences within mRNA molecules that are silenced by cleavage of the mRNA strand, destabilization of the mRNA by shortening its tail, and less efficient translation into proteins by ribosomes [17]. MiRNA expression profiling studies show that the expression levels of certain miRNAs change in diseased human hearts, suggesting their involvement in cardiomyopathies. MiR-712 is a potential predictor of atherosclerosis, has blood flow-dependent expression, and miR-712 is also upregulated in endothelial cells exposed to naturally occurring d-flow in the greater curvature of the aortic arch [18]. Several studies have investigated the cooperation of miRNA, metalloproteinases (MMP), and tissue inhibitor of matrix metalloproteinases (TIMP) in aorthopathy secondary to morphological alteration of the aortic valve. miRNAs related to dilation of the thoracic aorta (TA) are upregulated in transcriptional and epigenetic ways: different levels of MMP-2, MMP-9, TIMP-1, and TIMP-9 were observed [19]. A high level of MMP-2 and increased levels of miR-17 and miRNAs with the same genetic features as miR-17 were found in a comparative study involving patients with mild and severe aorta dilation, with a decreased level of TIMP -1, TIMP-2, and TIMP-3, thus hypothesizing a continuous development of TA influenced by BAV [20]. A recent study showed a relationship between miR-133a and TIMP-1 and TIMP-2 without reporting a statistically significant association between miR-143 and MMP-2 [21].
Table 1. Gene expression involved in valve and aortic diseases. ACTA 2: alfa actine 2, AXIN: gene encodes a cytoplasmic protein that contains a regulation of G-protein signaling (RGS) domain and a disheveled and axin (DIX) domain, BAV: bicuspid aortic valve, ENG: Endoglin, FBN1: fibrillin 1, GATA (sequence for transcription factors for zinc proteins’ binding DNA sequence), NOS3: nitric oxide synthase 3, NOTCH1 (gene encoding transmembrane proteins), PDIA2: protein disulfide isomerase family A member 2, PECAM-1: platelet endothelial cell adhesion molecule-1, TGF: transforming growth factor, TIMP: tissue inhibitor of matrix metalloproteinases.
| Gene Expression | Pathology |
|---|---|
| miR-146-5p | BAV, aortic aneuurysm (convex region) |
| miR-21-5p | BAV, aortic aneuurysm (convex region) |
| miR-17 | Aoritc anurysm |
| miR 21 | Aortic aneurysm |
| miR-34 a | Aortic aneurysm |
| miR-122 | BAV |
| miR 130 a | BAV |
| miR-133a | TIMP1,TIMP2, aortic aneurysm |
| mi-R 143 | Aortic aneurysm |
| mi-R 145 | Aortic aneurysm |
| miR 146-5p | Aortic aneurysm |
| miR-200 | Endothelial-mesenchimal/epithelial mesenchimal |
| miR-423-5p | BAV, aortic aneurysm |
| miR-424-3p downregulation | Cell proliferation, apoptosis, endothelial cells alterations, aortic anuerysm |
| miR-486 | BAV |
| miR-494 | PECAM |
| miR-712 | Atherosclerosis, aortic aneurysm |
| miR-718 | Aortic aneurysm |
| ACTA2 | BAV. Aortic aneurysm |
| AXIN1-PDIA2 | BAV |
| ENG | BAV |
| FBN 1 | BAV |
| GATA4/GATA5/GATA6 | BAV |
| NOS3 | BAV |
| NOTCH1 (9q34.3) | BAV, outflow tract malformation |
| TGFb1/TGFb2 | Sporadic BAV, Loeys-Dietz syndrome |
| 18q | BAV |
| 5q | BAV |
| 13q | BAV |
Plasma exosomal miR-423-5p regulates TGF-β signaling by targeting “similar mothers against decapentaplegic Drosophila gene” 2 (SMAD2), exerting functions in the initiation and development of BAV disease and its complication, bicuspid aortopathy [22][23]. Circulating miRNAs may reflect remodeling processes in the proximal aorta in patients with bicuspid aortopathy, and a recent study found a significant association between miRNA expression in peripheral blood and aortic tissue, as levels of miR-21, miR-133a, miR-143, and miR-145 were associated with dilated aorta [24].
Since abnormalities in vascular smooth muscle cells (VSMCs) may influence the development of TA dilation, primarily when contractile function converts to secretory function, this molecular situation causes cell apoptosis, in which the role of miRNA regulation may play a crucial role. Specifically, the convex part of ascending thoracic aorta (ATA) in BAV has increased miR-146-5p and miR-21-5p and reduced miR-133a-3p levels [25]; miR-424-3p and miR-3688-3p are downregulated in Hippo, ErbB, and TGF-beta signalling pathways, an epiphenomenon of cell proliferation and apoptosis [26]; and, finally, endothelial cells may have alterations due to abnormal flux patterns and genetic factors. This last alteration results in a less resistant vessel wall and can start a process of aortic dilation. Moreover, miR-494 is associated with platelet endothelial cell adhesion molecule (PECAM) and microparticles derived from endothelial cells [26], and the decreased expression of the miR-200 group can determine the involvement of the miR-200 family in endothelial–mesenchymal/epithelial–mesenchymal transition (EndMT/EMT) [27].
Observing the role of miRNAs as aortopathy biomarker of aortic dilation and increasing aortic dilation, it has been observed that miR-133a has a special linkage with the aneurysms’ incidence [28]; miR-122, miR-130a, and miR-486 are expressed in BAV; and miR-718 is used to predict aneurysms [29] similar to miR-34a [30].
Fibrillin 1 (FBN1) mutations have been found in BAV and aortic dilation. This gene encodes a glycoprotein of extracellular matrix (ECM), which manteins elastic fibers, and is also involved in the linkage of epithelial cells to interstitial matrix. A downregualtion of this gene has been associated with BAV [31]. GATA (sequence for transcription factors for zinc proteins’ binding DNA sequence) variations are involved in BAV: a missense p. Arg202Gln in GATA5 and three synonymous variants—p. Cys274 and p. His302 in GATA4, and p. Asn458 in GATA6 [32]. Alterations in nitric oxide synthase 3 (NOS3) are also associated with BAV. A single nucleotide polymorphism (SNP) is present in aneurysmal and non-aneurysmal BAV [33]. A haplotype within the AXIN-1-protein disulfide isomerase family A member 2 (AXIN1-PDIA2) locus and in the Endoglin (ENG) gene has been found to be linked to BAV [34]. Cilia and excyst have a main role in regulate mitogen-activated protein kinase (MAPK) signaling. An alteration of this mechanism is the cause of an activation of MAPK and the formation of BAV and calcified aortic stenosis [35].
3. Classification and Nomenclature
Since 1970, several classifications of BAV, derived from pathology, US scan, CT scan, and MR patterns (Table 2), have been proposed [36]. Recently, an international consensus statement developed a classification based on the progression of cusps fusion and geometry of commissurae [37], with particular attention to surgical indications and techniques.
Table 2. BAV classifications (adapted from Michelena HI et al./European Journal of cardio-thoracic surgery). Abbreviations; BAV, bicuspid aortic valve; BAVCon, bicuspid aortic valve consortium; LN, left non-coronary fusion; RL, right–left fusion; RN, right non-coronary fusion.
| Author | Nomenclature |
|---|---|
| Roberts [36] 1970 | Anterior–posterior cusps Right–left cusps Presence of raphe |
| Brandenburg et al. [38] 1983 | Clock-face nomenclature: Commissures at 4–10 o’clock with raphe at 2 o’clock (R-L) Commissures at 1–6 o’clock with raphe at 10 o’clock (RN) Commissures at 3–9 o’clock without raphe (L-N) |
| Angelini et al. [39] 1989 | Anterior–posterior cusps Right–left cusps Presence of raphe |
| Sabet et al. [40] 1999 | RL RN LN Presence of raphe |
| Sievers and Schmidtke [41] 2007 | Type 0 (no raphe): anteroposterior or lateral cusps (true BAV) Type 1 (1 raphe): R-L, RN, L-N Type 2 (2 raphes): L-R, RN |
| Schaefer et al. [42] 2008 | Type 1: RL Type 2: RN Type 3: LN Presence of raphe Aorta: Type N: normal shape Type E: sinus effacement Type A: ascending aorta dilatation |
| Kang et al. [43] 2013 | Anteroposterior orientation: type 1: R-L with raphe type; 2: R-L without raphe Right–left orientation: Type 3: RN with raphe Type 4: L-N with raphe Type 5: symmetrical cusps with 1 coronary artery originating from each cusp Aorta: Type 0: normal Type 1: dilated root Type 2: dilated ascending aorta Type 3: diffuse involvement of the ascending aorta and arch |
| Michelena et al. [44] 2014 | BAVCon nomenclature: Type 1: R-L Type 2: RN Type 3: L-N Presence of raphe |
| Jilaihawi et al. [45] 2016 | Tricommissural: functional or acquired bicuspidity of a trileaflet valve Bicommissural with raphe Bicommissural without raphe |
| Sun et al. [46] 2017 | Dichotomous nomenclature: R-L Mixed: (RN or L-N) |
| Murphy et al. [47] 2017 | Clock-face nomenclature: Type 0: partial fusion/eccentric leaflet? Type 1: RN, RL, LN partial fusion/eccentric leaflet? Type 2: RL and RN, RL and LN, RN and LN partial fusion/eccentric leaflet? |
From this consensus statement, three BAV patterns related to the fusion of cusps and the number of sinuses may be observed. Every pattern should be considered like a schematic-based US short-axis scan at the base of the heart; the ideal circumference of the aortic valve is subdivided into parts like the face of a clock, in which the points over the watch are the coordinates of the anatomical features of the BAV.
In normal cardiogenesis, endothelium-derived nitric oxide syntethase (eNOS) expression is related to endocardial cells and is dependent upon the shear stress [48][49]. Nitric oxide is the promotor of podokinesis. In this way, cardiac jelly is populated by endocardil cells to make endocardil cushions [50]. In a study on mice, eNOS deficency may cause an alteration of cell migration with impairment in the development of valvular cushions, and an alteration of the function of cardiac neural crest cells has a role in this pathogenetic pattern [7][51].
The first pattern related to embryological events is defined as the fused bicuspid aortic valve (Figure 1) and diagnosed in 90–95% of cases [44] and presents three subtypes defined according to the cusps involved.
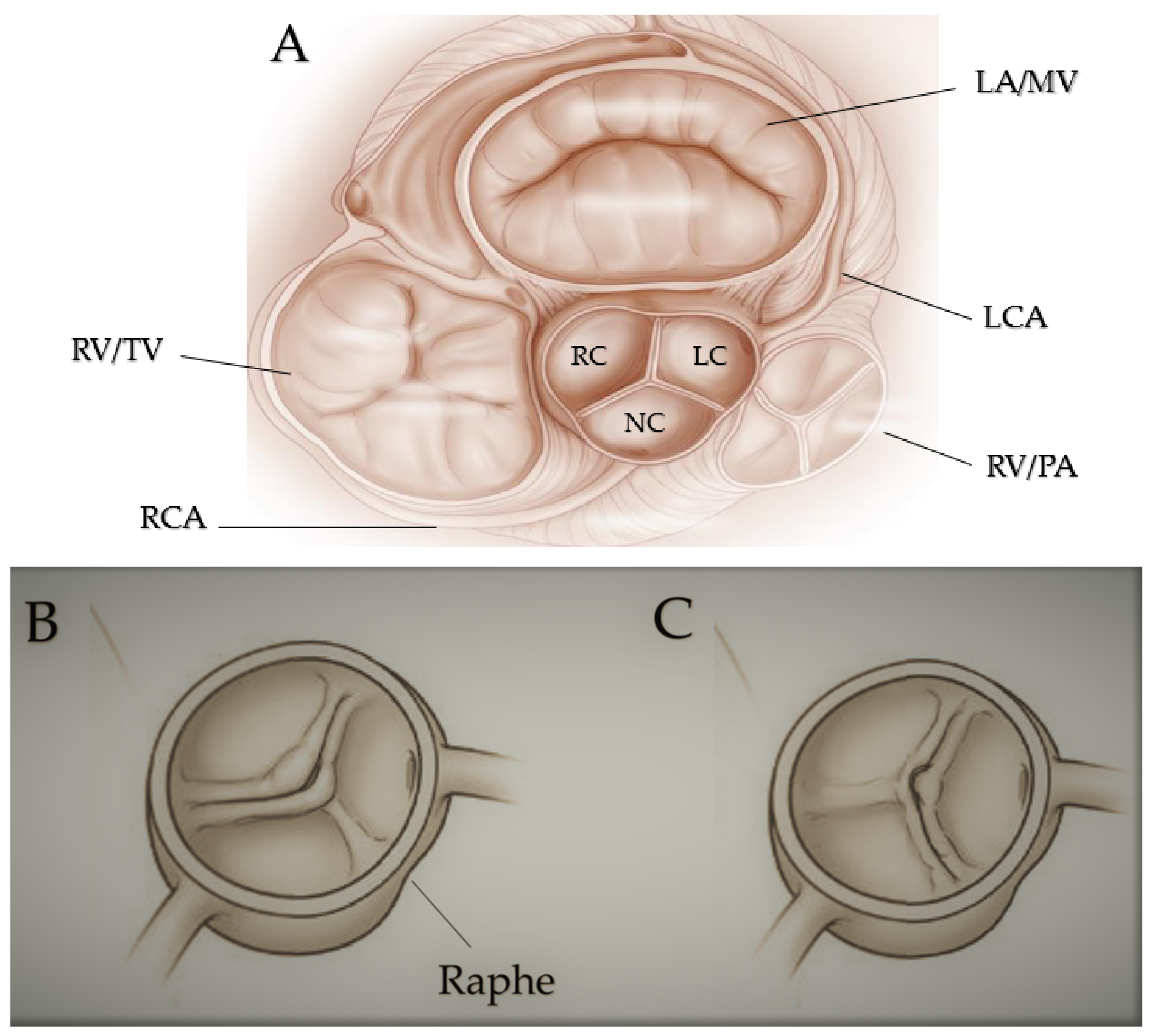
Figure 1. Fused bicuspid aortic valve. (A) Represents short-axis normal tricuspidal aortic pattern with anatomical proximities. Cusps’ fusion patterns seen in short heart axis: right-left coronary fusion (B), right-non coronary fusion (C). All BAVs have three sinuses. Raphe structure is between the fused cusps. Non-fused cusp is prominent in respect to the fused ones. The commissure angle of the non-fused cusp has a degree < 180°. Abbreviations: LA, left atrium; LC, left cusp; LCA, left coronary artery; MV, mitral valve; NC, non-coronary cusp; PA, pulmonary artery; RA, right atrium; RC, right cusp; RCA, right coronary artery; RV, right ventricule; TV, tricuspidalic valve. Licenses Centre Cardiologique du Nord; order date 8 September 2022; order number 5384080341542; publication NEJM; Title: Mitral valve Repair for Mitral valve prolapse.
In normal conditions, valve cushions are modelled by an excavation process resulting in fusion of the cusps in case of process alteration [51][52][53][54][55]. It is possible to distinguish three sinuses and the fusion of two of the three cusps. In contrast, the non-fused cusp commissure has an angle of different degrees and generally is more prominent than the fused cusps, as occurs for its sinus compared to the other two sinuses. A fibrous raphe, a predictor of further development of AS [56] between the two fused cusps, has been frequently observed [40][57]. The right–left cusp fusion, observed in 70–80% of patients [58] and often associated with AS and aortic regurgitation (AR) [44], is derived from a mild alteration in the outflow tract septation during embryogenesis and is linked to the formation of aneurysms in every section of the aorta (aortic root, ascending aorta, aortic arch) and frequently characterized by root dilation. An association has also been observed between right–left cusp fusion and aortic coarctation. The right–left cusp fusion is common in genetic syndromes, such as Turner’s one and Shone’s complex and people with Down syndrome [59]. In 20–30% of BAV cases, a proper non-coronary cusp fusion is present, more common among the Asian population [60] and frequently associated with AS in adults [56].
Moreover, it may be observed combined with an alteration of the process involved in the formation of the endocardial cushion, an independent predictor of AR [61]. In children, this phenotype may induce a more rapid development of AS and AR [62][63]. Left non-coronary cusp fusion is only present in 3–6% of patients [37].
The second type of BAV is referred to as the two sinuses BAV type (Figure 2).
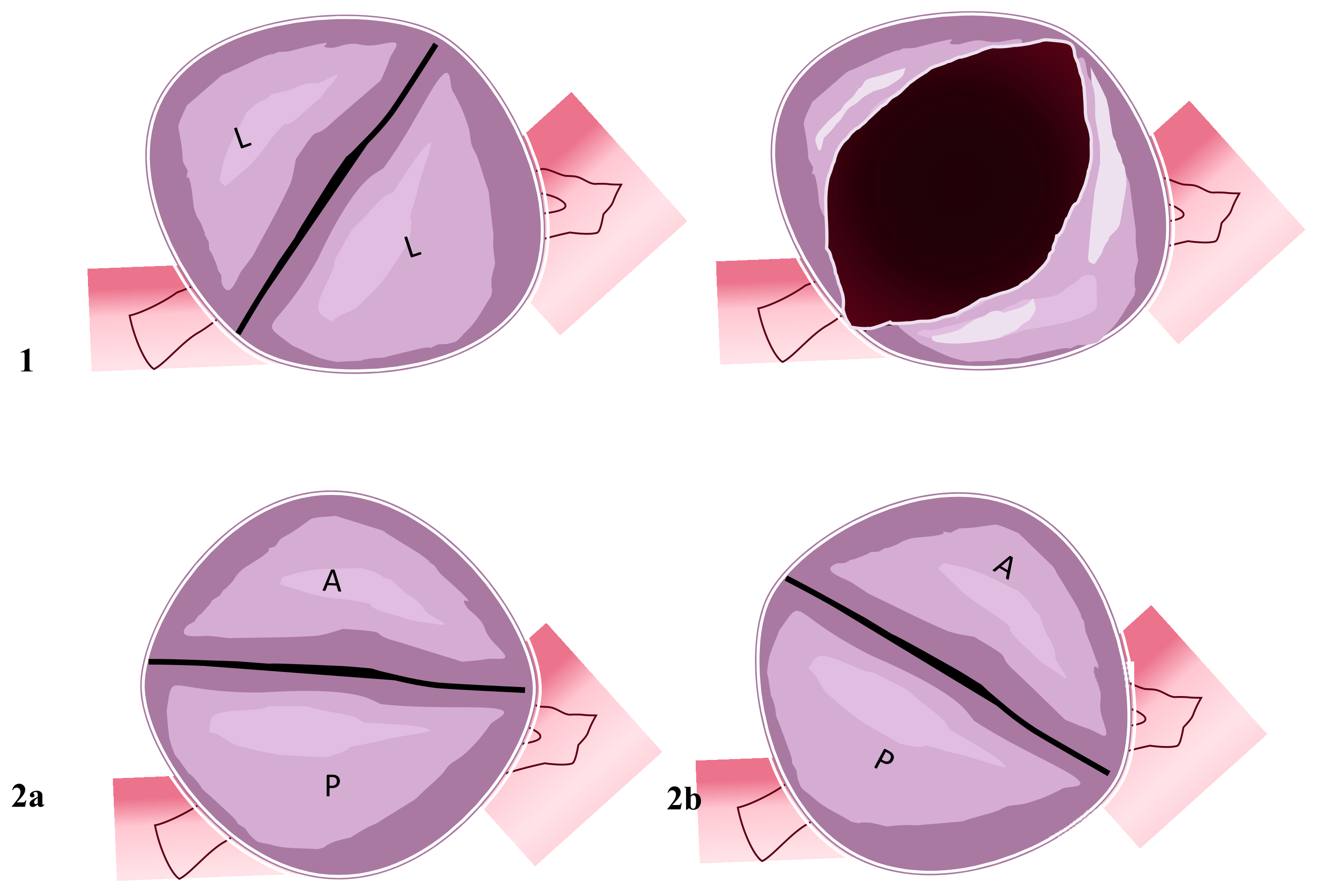
Figure 2. Two-sinus bicuspid aortic valve. Figure represents two cusps’ non-fusion patterns seen in the short heart axis. Aortic valves have two sinuses with two leaflets non-derived from fusion mechanisms. (1) Coronary arteries originate from the two sinuses with two lateral leaflets. The opened valve in systole phase has the oval-ball image. (2a) In this position, coronary arteries originate from the anterior sinus (right coronary artery) and posterior sinus (common left stem). (2b) Right coronary artery and common left stem both originate from anterior sinus. Abbreviations; A, anterior; L, lateral P, posterior.
Its incidence ranges between 5 and 7% of cases [40][44][64]. In this pattern, it is possible to identify two cusps corresponding to homologous sinuses, not depending upon fusion but upon the abnormal embryological constitution. Typically, the cusps are the same in size, a raphe is not present, and the aortic orifice is divided into two portions: laterolateral (Figure 2(1)) and anteroposterior (Figure 2(2a,2b)). In the laterolateral pattern, coronary setup is from each sinus; in the anteroposterior type, coronaries may originate from each sinus or the anterior one. Embryological alteration involved in the laterolateral pattern is secondary to abnormal endocardial cushion formation and positioning. The aetiology of the anteroposterior model is due to abnormal outflow tract septation. The same mechanism in the fused aortic bicuspid valve type is present in this second morphological pattern, but the two-sinus valve may constitute a more severe embryological development alteration [37].
The third BAV type is a partial fusion bicuspid aortic valve (Figure 3), with an unknown prevalence [65].
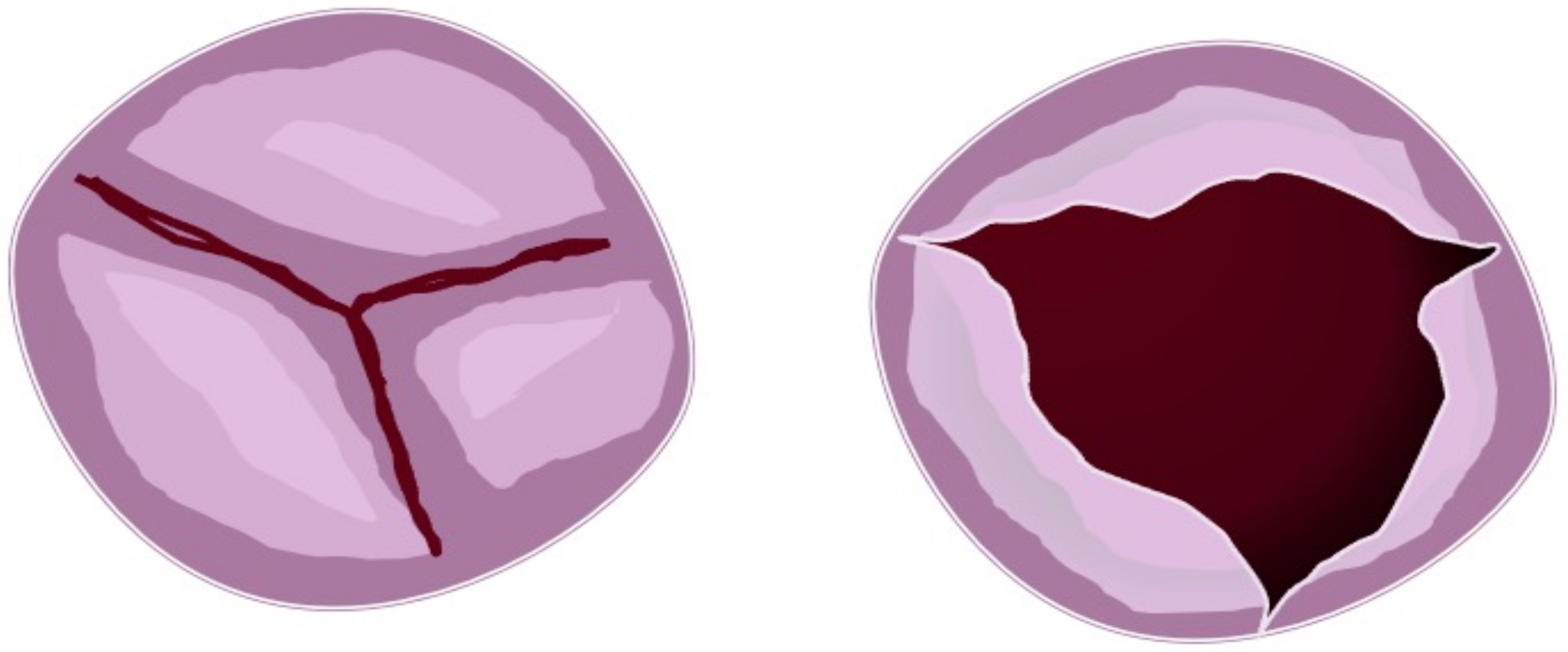
Figure 3. Partial fusion aortic valve. Figure represents three cusps with partial leaflets fusion seen in the short heart axis (left). In this case, the opened (right) aortic valve is similar to the normal valve but with a more narrow area.
Morphological features are similar to a tricuspid valve with symmetry of the cusps, and the aortic orifice area is less comprehensive than the normal surface. A raphe is localized at the base of each commissure, causing a fixed portion of the cusp to the artic wall. For this reason, this phenotype is also called form fruste aortic valve [66][67][68]. An alteration of normal embryological processes may be identified. Therefore, it is assumed that a mild defect in outflow tract septation and remodelling of aortic valve cushions are present.
The above classifications (Table 2) have implications for daily clinical practice. Siever’s classification is still the most important for diagnosis and surgical indication. The classifications with the determination of the leaflets and the fusion patterns of the commissures are crucial for the development of aortic dilatation [69]. Even aortic valve morphology, flow changes, and prognostic evaluation are well determined by models derived from fusion pattern classification.
4. BAV Geometry Types and Surgical Implications
In every subtype of the previous classification, we can identify the BAV geometrical pattern by evaluating the position of commissures related to the aortic orifice, their angle in the coaptation zone, the presence of raphe, and the morphology and the area of the cusps. In the fused BAV type, it is relevant to establish the relationships between the fused cusps and non-fused cusp and the angle of the commissures of the non-fused cusps (Figure 4).
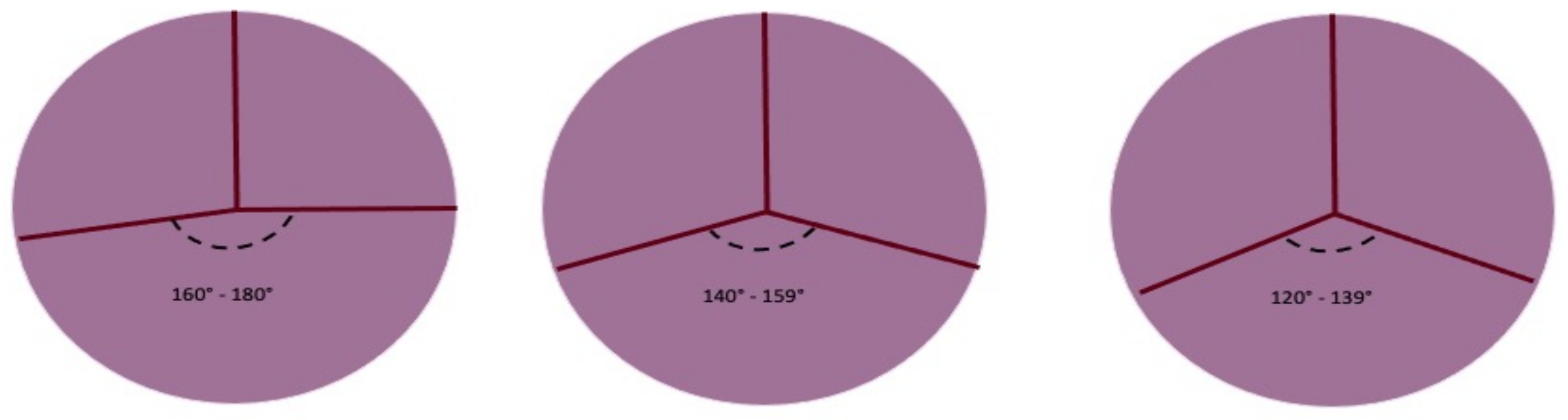
Figure 4. Symmetry of fused bicuspid aortic valve (adapted from Michelena HI et al./European Journal of cardio-thoracic surgery). Figure represents the angles determined by aortic valve leaflets fusion patterns. The length of raphe causes the retraction of fused leaflets and the non-physiological coaptation of the non-fused leaflet with fused leaflets. The geometry of the three patterns can be summarized as symmetrical, asymmetrical, and very asymmetrical The degree of the angle is important for surgical technique.
When the two fused cusps are retracted over the raphe, AR may develop. Therefore, the coaptation line and angle must be described mainly for surgical indications and practice. The coaptation angle may vary from 180° to less than 150°; to ensure a higher probability of valve repair, the ideal angle should range between 180° and 160°. When the angle approximates 140°, valve sparing and repairing is more complex [70]. Pre-cardiopulmonary bypass transoesophageal echocardiography establishes the coaptation model and commissural angle.
The two-cusp fusion model, more frequent in AS, has the two cusps/two sinuses feature, and the commissural angle is nearly close to 180° [37]. In partial fusion, the commissural angle resembles the one present in the normal aortic valve.
Surgical valve-preserving techniques are indicated by the commissural geometry of the aortic valve, as mentioned by a recent paper that also considers the relationship of the aortic root from the virtual basal ring (VBR) to the sinitubular junction [71].
References
- Ward, C. Clinical significance of the bicuspid aortic valve. Heart 2000, 83, 81–85.
- Tzemos, N.; Therrien, J.; Yip, J.; Thanassoulis, G.; Tremblay, S.; Jamorski, M.T.; Webb, G.D.; Siu, S.C. Outcomes in adults with bicuspid aortic valves. JAMA 2008, 300, 1317–1325.
- Tutar, E.; Ekici, F.; Atalay, S.; Nacar, N. The prevalence of bicuspid aortic valve in newborns by echocardiographic screening. Am. Heart J. 2005, 150, 513–515.
- Carro, A.; Teixido-Tura, G.; Evangelista, A. Aortic Dilatation in Bicuspid Aortic Valve Disease. Rev. Esp. Cardiol. 2012, 65, 977–981.
- Fedak, P.; Verma, S.; David, T.E.; Leask, R.; Weisel, R.D.; Butany, J. Clinical and Pathophysiological Implications of a Bicuspid Aortic Valve. Circulation 2002, 106, 900–904.
- Girdauskas, E.; Borger, M.; Secknus, M.-A.; Girdauskas, G.; Kuntze, T. Is aortopathy in bicuspid aortic valve disease a congenital defect or a result of abnormal hemodynamics? A critical reappraisal of a one-sided argument. Eur. J. Cardio-Thorac. Surg. 2011, 39, 809–814.
- Siu, S.C.; Silversides, C.K. Bicuspid aortic valve disease. J. Am. Coll. Cardiol. 2010, 55, 2789–2800.
- Jia, H.; Kang, L.; Ma, Z.; Lu, S.; Huang, B.; Wang, C.; Zou, Y.; Sun, Y. MicroRNAs involve in bicuspid aortic aneurysm: Pathogenesis and biomarkers. J. Cardiothorac. Surg. 2021, 16, 230.
- Nappi, F.; Iervolino, A.; Singh, S.S.A.; Chello, M. MicroRNAs in Valvular Heart Diseases: Biological Regulators, Prognostic Markers and Therapeutical Targets. Int. J. Mol. Sci. 2021, 22, 12132.
- Garg, V.; Muth, A.N.; Ransom, J.F.; Schluterman, M.K.; Barnes, R.; King, I.N.; Grossfeld, P.D.; Srivastava, D. Mutations in NOTCH1 cause aortic valve disease. Nature 2005, 437, 270–274.
- Mohamed, S.A.; Aherrahrou, Z.; Liptau, H.; Erasmi, A.W.; Hagemann, C.; Wrobel, S.; Borzym, K.; Schunkert, H.; Sievers, H.H.; Erdmann, J. Novel missense mutations (p. T596M and p. P1797H) in NOTCH1 in patients with bicuspid aortic valve. Biochem. Biophys. Res. Commun. 2006, 345, 1460–1465.
- Martin, L.; Ramachandran, V.; Cripe, L.H.; Hinton, R.B.; Andelfinger, G.; Tabangin, M.; Shooner, K.; Keddache, M.; Benson, D.W. Evidence in favor of linkage to human chromosomal regions 18q, 5q and 13q for bicuspid aortic valve and associated cardiovascular malformations. Hum. Genet. 2007, 121, 275–284.
- Guo, D.-C.; Pannu, H.; Tran-Fadulu, V.; Papke, C.L.; Yu, R.K.; Avidan, N.; Bourgeois, S.; Estrera, A.L.; Safi, H.J.; Sparks, E.; et al. Mutations in smooth muscle α-actin (ACTA2) lead to thoracic aortic aneurysms and dissections. Nat. Genet. 2007, 39, 1488–1493.
- Higgins, C.B.; Wexler, L. Reversal of dominance of the coronary arterial system in isolated aortic stenosis and bicuspid aortic valve. Circulation 1975, 52, 292–296.
- Hutchins, G.M.; Nazarian, I.H.; Bulkley, B.H. Association of left dominant coronary arterial system with congenital bicuspid aortic valve. Am. J. Cardiol. 1978, 42, 57–59.
- Rashid, A.; Saucedo, J.F.; Hennebry, T.A. Association of Single Coronary Artery and Congenital Bicuspid Aortic Valve with Review of Literature. J. Interv. Cardiol. 2005, 18, 389–391.
- Bartel, D.P. MicroRNAs: Target Recognition and Regulatory Functions. Cell 2009, 136, 215–233.
- Insull, W., Jr. The Pathology of Atherosclerosis: Plaque Development and Plaque Responses to Medical Treatment. Am. J. Med. 2009, 122, S3–S14.
- LeMaire, S.A.; Wang, X.; Wilks, J.A.; Carter, S.A.; Wen, S.; Won, T.; Leonardelli, D.; Anand, G.; Conklin, L.D.; Wang, X.L.; et al. Matrix metalloproteinases in ascending aortic aneurysms: Bicuspid versus trileaflet aortic valves1. J. Surg. Res. 2005, 123, 40–48.
- Wu, J.; Song, H.-F.; Li, S.-H.; Guo, J.; Tsang, K.; Tumiati, L.; Butany, J.; Yau, T.M.; Ouzounian, M.; Fu, S.; et al. Progressive Aortic Dilation Is Regulated by miR-17–Associated miRNAs. J. Am. Coll. Cardiol. 2016, 67, 2965–2977.
- Naito, S.; Petersen, J.; Sequeira-Gross, T.; Neumann, N.; Escobar, J.D.; Zeller, T.; Reichenspurner, H.; Girdauskas, E. Bicuspid aortopathy—Molecular involvement of microRNAs and MMP-TIMP. Biomarkers 2020, 25, 711–718.
- Zhang, H.; Liu, D.; Zhu, S.; Wang, F.; Sun, X.; Yang, S.; Wang, C. Plasma Exosomal Mir-423-5p Is Involved in the Occurrence and Development of Bicuspid Aortopathy via TGF-beta/SMAD2 Pathway. Front. Physiol. 2021, 12, 759035.
- Zheng, R.; Zhu, P.; Gu, J.; Ni, B.; Sun, H.; He, K.; Bian, J.; Shao, Y.; Du, J. Transcription factor Sp2 promotes TGFB-mediated interstitial cell osteogenic differentiation in bicuspid aortic valves through a SMAD-dependent pathway. Exp. Cell Res. 2022, 411, 112972.
- Naito, S.; Sequeira-Gross, T.; Petersen, J.; Detlef, I.; Sachse, M.; Zeller, T.; Reichenspurner, H.; Girdauskas, E. Circulating microRNAs in the prediction of BAV aortopathy: Do the expression patterns correlate between blood and aortic tissue? Rev. Cardiovasc. Med. 2022, 23, 47.
- Albinsson, S.; Della Corte, A.; Alajbegovic, A.; Krawczyk, K.K.; Bancone, C.; Galderisi, U.; Cipollaro, M.; De Feo, M.; Forte, A. Patients with bicuspid and tricuspid aortic valve exhibit distinct regional microrna signatures in mildly dilated ascending aorta. Heart Vessel. 2017, 32, 750–767.
- Borghini, A.; Foffa, I.; Pulignani, S.; Vecoli, C.; Ait-Ali, L.; Andreassi, M.G. miRNome Profiling in Bicuspid Aortic Valve-Associated Aortopathy by Next-Generation Sequencing. Int. J. Mol. Sci. 2017, 18, 2498.
- Martínez-Micaelo, N.; Beltrán-Debón, R.; Aragonès, G.; Faiges, M.; Alegret, J.M. MicroRNAs Clustered within the 14q32 Locus Are Associated with Endothelial Damage and Microparticle Secretion in Bicuspid Aortic Valve Disease. Front. Physiol. 2017, 8, 648.
- Maleki, S.; Cottrill, K.A.; Poujade, F.-A.; Bhattachariya, A.; Bergman, O.; Gådin, J.R.; Simon, N.; Lundströmer, K.; Franco-Cereceda, A.; Björck, H.M.; et al. The mir-200 family regulates key pathogenic events in ascending aortas of individuals with bicuspid aortic valves. J. Intern. Med. 2019, 285, 102–114.
- Martínez-Micaelo, N.; Beltrán-Debón, R.; Baiges, I.; Faiges, M.; Alegret, J.M. Specific circulating microRNA signature of bicuspid aortic valve disease. J. Transl. Med. 2017, 15, 76.
- Gallo, A.; Agnese, V.; Coronnello, C.; Raffa, G.M.; Bellavia, D.; Conaldi, P.G.; Pilato, M.; Pasta, S. On the prospect of serum exosomal miRNA profiling and protein biomarkers for the diagnosis of ascending aortic dilatation in patients with bicuspid and tricuspid aortic valve. Int. J. Cardiol. 2018, 273, 230–236.
- Giusti, B.; Sticchi, E.; De Cario, R.; Magi, A.; Nistri, S.; Pepe, G. Genetic Bases of Bicuspid Aortic Valve: The Contribution of Traditional and High-Throughput Sequencing Approaches on Research and Diagnosis. Front. Physiol. 2017, 8, 612.
- Alonso-Montes, C.; Martín, M.; Martínez-Arias, L.; Coto, E.; Naves-Díaz, M.; Morís, C.; Cannata-Andía, J.B.; Rodríguez, I. Variants in cardiac GATA genes associated with bicuspid aortic valve. Eur. J. Clin. Investig. 2018, 48, e13027.
- Hill, J.C.; Billaud, M.; Richards, T.D.; Kotlarczyk, M.P.; Shiva, S.; Phillippi, J.A.; Gleason, T.G. Layer-specific Nos3 expression and genotypic distribution in bicuspid aortic valve aortopathy. Eur. J. Cardio-Thorac. Surg. 2022, ezac237.
- Wooten, E.C.; Iyer, L.K.; Montefusco, M.C.; Hedgepeth, A.K.; Payne, D.D.; Kapur, N.K.; Housman, D.E.; Mendelsohn, M.E.; Huggins, G.S. Application of gene network analysis techniques identifies AXIN1/PDIA2 and endoglin haplotypes associated with bicuspid aortic valve. PLoS ONE 2010, 5, e8830.
- Fulmer, D.; Toomer, K.; Guo, L.; Moore, K.; Glover, J.; Moore, R.; Stairley, R.; Lobo, G.; Zuo, X.; Dang, Y.; et al. Defects in the Exocyst-Cilia Machinery Cause Bicuspid Aortic Valve Disease and Aortic Stenosis. Circulation 2019, 140, 1331–1341.
- Roberts, W.C. The congenitally bicuspid aortic valve. A study of 85 autopsy cases. Am. J. Cardiol. 1970, 26, 72–83.
- Michelena, H.I.; Della Corte, A.; Evangelista, A.; Maleszewski, J.J.; Edwards, W.D.; Roman, M.J.; Devereux, R.B.; Fernández, B.; Asch, F.M.; Barker, A.J.; et al. International consensus statement on nomenclature and classification of the congenital bicuspid aortic valve and its aortopathy, for clinical, surgical, interventional and research purposes. Eur. J. Cardiothorac. Surg. 2021, 60, 448–476.
- Brandenburg, R.O.; Tajik, A.J.; Edwards, W.D.; Reeder, G.S.; Shub, C.; Seward, J.B. Accuracy of 2-dimensional echocardiographic diagnosis of congenitally bicuspid aortic valve: Echocardiographic-anatomic correlation in 115 patients. Am. J. Cardiol. 1983, 51, 1469–1473.
- Angelini, A.; Ho, S.Y.; Anderson, R.H.; Devine, W.A.; Zuberbuhler, J.R.; Becker, A.E.; Davies, M.J. The morphology of the normal aortic valve as compared with the aortic valve having two leaflets. J. Thorac. Cardiovasc. Surg. 1989, 98, 362–367.
- Sabet, H.Y.; Edwards, W.D.; Tazelaar, H.D.; Daly, R.C. Congenitally Bicuspid Aortic Valves: A Surgical Pathology Study of 542 Cases (1991 Through 1996) and a Literature Review of 2,715 Additional Cases. Mayo Clin. Proc. 1999, 74, 14–26.
- Sievers, H.-H.; Schmidtke, C. A classification system for the bicuspid aortic valve from 304 surgical specimens. J. Thorac. Cardiovasc. Surg. 2007, 133, 1226–1233.
- Schaefer, B.M.; Lewin, M.B.; Stout, K.K.; Gill, E.; Prueitt, A.; Byers, P.H.; Otto, C.M. The bicuspid aortic valve: An integrated phenotypic classification of leaflet morphology and aortic root shape. Heart 2008, 94, 1634–1638.
- Kang, J.-W.; Song, H.G.; Yang, D.H.; Baek, S.; Kim, D.-H.; Song, J.-M.; Kang, D.-H.; Lim, T.-H.; Song, J.-K. Association Between Bicuspid Aortic Valve Phenotype and Patterns of Valvular Dysfunction and Bicuspid Aortopathy: Comprehensive Evaluation Using MDCT and Echocardiography. JACC Cardiovasc. Imaging 2013, 6, 150–161.
- Michelena, H.I.; Prakash, S.K.; Della Corte, A.; Bissell, M.M.; Anavekar, N.; Mathieu, P.; Bossé, Y.; Limongelli, G.; Bossone, E.; Benson, D.W.; et al. Bicuspid aortic valve: Identifying knowledge gaps and rising to the challenge from the International Bicuspid Aortic Valve Consortium (BAVCon). Circulation 2014, 129, 2691–2704.
- Jilaihawi, H.; Chen, M.; Webb, J.; Himbert, D.; Ruiz, C.E.; Rodés-Cabau, J.; Pache, G.; Colombo, A.; Nickenig, G.; Lee, M.; et al. A Bicuspid Aortic Valve Imaging Classification for the TAVR Era. JACC Cardiovasc. Imaging 2016, 9, 1145–1158.
- Sun, B.J.; Lee, S.; Jang, J.Y.; Kwon, O.; Bae, J.S.; Lee, J.H.; Kim, D.-H.; Jung, S.-H.; Song, J.-M.; Kang, D.-H.; et al. Performance of a Simplified Dichotomous Phenotypic Classification of Bicuspid Aortic Valve to Predict Type of Valvulopathy and Combined Aortopathy. J. Am. Soc. Echocardiogr. 2017, 30, 1152–1161.
- Murphy, I.G.; Collins, J.; Powell, A.; Markl, M.; McCarthy, P.; Malaisrie, S.C.; Carr, J.C.; Barker, A.J. Comprehensive 4-stage categorization of bicuspid aortic valve leaflet morphology by cardiac MRI in 386 patients. Int. J. Cardiovasc. Imaging 2017, 33, 1213–1221.
- Bernard, C.; Morgant, M.C.; Guillier, D.; Cheynel, N.; Bouchot, O. Point on the Aortic Bicuspid Valve. Life 2022, 12, 518.
- Groenendijk, B.C.; Hierck, B.P.; Gittenberger-De Groot, A.C.; Poelmann, R.E. Development-related changes in the expression of shear stress responsive genes KLF-2, ET-1, and NOS-3 in the developing cardiovascular system of chicken embryos. Dev. Dyn. 2004, 230, 57–68.
- Noiri, E.; Lee, E.; Testa, J.; Quigley, J.; Colflesh, D.; Keese, C.R.; Giaever, I.; Goligorsky, M.S. Podokinesis in endothelial cell migration: Role of nitric oxide. Am. J. Physiol. Physiol. 1998, 274, C236–C244.
- Fernández, B.; Durán, A.C.; Fernández-Gallego, T.; Fernández, M.C.; Such, M.; Arqué, J.M.; Sans-Coma, V. Bicuspid Aortic Valves with Different Spatial Orientations of the Leaflets Are Distinct Etiological Entities. J. Am. Coll. Cardiol. 2009, 54, 2312–2318.
- Fernández, B.; Soto-Navarrete, M.T.; López-García, A.; López-Unzu, M.; Durán, A.C.; Fernández, M.C. Bicuspid Aortic Valve in 2 Model Species and Review of the Literature. Veter. Pathol. 2020, 57, 321–331.
- Phillips, H.M.; Mahendran, P.; Singh, E.; Anderson, R.H.; Chaudhry, B.; Henderson, D.J. Neural crest cells are required for correct positioning of the developing outflow cushions and pattern the arterial valve leaflets. Cardiovasc. Res. 2013, 99, 452–460.
- Sans-Coma, V.; Fernández, B.; Durán, A.C.; Thiene, G.; Arqué, J.M.; Muñoz-Chápuli, R.; Cardo, M. Fusion of valve cushions as a key factor in the formation of congenital bicuspid aortic valves in Syrian hamsters. Anat. Rec. 1996, 244, 490–498.
- Soto-Navarrete, M.T.; López-Unzu, M.; Durán, A.C.; Fernández, B. Embryonic development of bicuspid aortic valves. Prog. Cardiovasc. Dis. 2020, 63, 407–418.
- Evangelista, A.; Gallego, P.; Calvo-Iglesias, F.; Bermejo, J.; Robledo-Carmona, J.; Sánchez, V.; Saura, D.; Arnold, R.; Carro, A.; Maldonado, G.; et al. Anatomical and clinical predictors of valve dysfunction and aortic dilation in bicuspid aortic valve disease. Heart 2018, 104, 566–573.
- Kong, W.K.F.; Delgado, V.; Poh, K.K.; Regeer, M.V.; Ng, A.C.; McCormack, L.; Yeo, T.C.; Shanks, M.; Parent, S.; Enache, R.; et al. Prognostic Implications of Raphe in Bicuspid Aortic Valve Anatomy. JAMA Cardiol. 2017, 2, 285–292.
- Kong, W.K.F.; Regeer, M.V.; Poh, K.K.; Yip, J.W.; van Rosendael, P.; Yeo, T.C.; Tay, E.; Kamperidis, V.; Van Der Velde, E.T.; Mertens, B.; et al. Inter-ethnic differences in valve morphology, valvular dysfunction, and aortopathy between Asian and European patients with bicuspid aortic valve. Eur. Heart J. 2018, 39, 1308–1313.
- Niaz, T.; Poterucha, J.T.; Olson, T.M.; Johnson, J.N.; Craviari, C.; Nienaber, T.; Palfreeman, J.; Cetta, F.; Hagler, D.J. Characteristic Morphologies of the Bicuspid Aortic Valve in Patients with Genetic Syndromes. J. Am. Soc. Echocardiogr. 2018, 31, 194–200.
- Sun, B.J.; Jin, X.; Song, J.-K.; Lee, S.; Lee, J.H.; Park, J.-B.; Lee, S.-P.; Kim, D.-H.; Park, S.-J.; Kim, Y.-J.; et al. Clinical Characteristics of Korean Patients with Bicuspid Aortic Valve Who Underwent Aortic Valve Surgery. Korean Circ. J. 2018, 48, 48–58.
- Yang, L.T.; Pellikka, P.A.; Enriquez-Sarano, M.; Maalouf, J.F.; Scott, C.G.; Michelena, H.I. Stage B Aortic Regurgitation in Bicuspid Aortic Valve: New Observations on Progression Rate and Predictors. JACC Cardiovasc. Imaging 2020, 13, 1442–1445.
- Fernandes, S.M.; Khairy, P.; Sanders, S.P.; Colan, S.D. Bicuspid Aortic Valve Morphology and Interventions in the Young. J. Am. Coll. Cardiol. 2007, 49, 2211–2214.
- Fernandes, S.M.; Sanders, S.P.; Khairy, P.; Jenkins, K.J.; Gauvreau, K.; Lang, P.; Simonds, H.; Colan, S.D. Morphology of bicuspid aortic valve in children and adolescents. J. Am. Coll. Cardiol. 2004, 44, 1648–1651.
- Michelena, H.I.; Della Corte, A.; Evangelista, A.; Maleszewski, J.J.; Enriquez-Sarano, M.; Bax, J.J.; Otto, C.M.; Schäfers, H.-J. Speaking a common language: Introduction to a standard terminology for the bicuspid aortic valve and its aortopathy. Prog. Cardiovasc. Dis. 2020, 63, 419–424.
- Sperling, J.S.; Lubat, E. Forme fruste or ‘Incomplete’ bicuspid aortic valves with very small raphes: The prevalence of bicuspid valve and its significance may be underestimated. Int. J. Cardiol. 2015, 184, 1–5.
- American College of Cardiology Foundation Appropriate Use Criteria Task Force; American Society of Echocardiography; American Heart Association; American Society of Nuclear Cardiology; Heart Failure Society of America; Heart Rhythm Society; Society for Cardiovascular Angiography and Interventions; Society of Critical Care Medicine; Society of Cardiovascular Computed Tomography; Society for Cardiovascular Magnetic Resonance; et al. ACCF/ASE/AHA/ASNC/HFSA/HRS/SCAI/SCCM/SCCT/SCMR 2011 Appropriate Use Criteria for Echocardiography. A Report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, American Society of Echocardiography, American Heart Association, American Society of Nuclear Cardiology, Heart Failure Society of America, Heart Rhythm Society, Society for Cardiovascular Angiography and Interventions, Society of Critical Care Medicine, Society of Cardiovascular Computed Tomography, Society for Cardiovascular Magnetic Resonance American College of Chest Physicians. J. Am. Soc. Echocardiogr. 2011, 24, 229–267.
- Guala, A.; Rodriguez-Palomares, J.; Galian-Gay, L.; Teixido-Tura, G.; Johnson, K.M.; Wieben, O.; Avilés, A.S.; Evangelista, A. Partial Aortic Valve Leaflet Fusion Is Related to Deleterious Alteration of Proximal Aorta Hemodynamics. Circulation 2019, 139, 2707–2709.
- Michelena, H.I.; Yang, L.-T.; Enriquez-Sarano, M.; Pochettino, A. The elusive ‘forme fruste’ bicuspid aortic valve: 3D transoesophageal echocardiography to the rescue. Eur. Heart J. Cardiovasc. Imaging 2020, 21, 1169.
- Borger, M.A.; Fedak, P.W.; Stephens, E.H.; Gleason, T.G.; Girdauskas, E.; Ikonomidis, J.S.; Khoynezhad, A.; Siu, S.C.; Verma, S.; Hope, M.D.; et al. The American Association for Thoracic Surgery consensus guidelines on bicuspid aortic valve–related aortopathy: Full online-only version. J. Thorac. Cardiovasc. Surg. 2018, 156, e41–e74.
- Aicher, D.; Kunihara, T.; Issa, O.A.; Brittner, B.; Gräber, S.; Schäfers, H.-J. Valve Configuration Determines Long-Term Results After Repair of the Bicuspid Aortic Valve. Circulation 2011, 123, 178–185.
- Jahanyar, J.; de Kerchove, L.; El Khoury, G. Bicuspid aortic valve repair: The 180 degrees -Reimplantation technique. Ann. Cardiothorac. Surg. 2022, 11, 473–481.
More
Information
Subjects:
Cardiac & Cardiovascular Systems
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.1K
Entry Collection:
Hypertension and Cardiovascular Diseases
Revisions:
2 times
(View History)
Update Date:
25 Oct 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




