
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Tsvetelina Velikova | + 2909 word(s) | 2909 | 2020-12-25 04:05:59 | | | |
| 2 | Conner Chen | -35 word(s) | 2874 | 2021-01-12 04:16:23 | | |
Video Upload Options
Inflammatory bowel diseases (IBDs) are chronic inflammatory disorders of the gastrointestinal tract whose etiology is unknown. Pathogenesis of IBD is attributed to the complex interaction of genetic susceptibility, environmental factors (such as smoking, diet, and infections), and the gut microbiota. This results in an uncontrolled immune response leading to mucosal damage. IBDs are characterized by a relapsing and remitting course and require lifelong treatment. Therapy aims to induce remission, maintain remission, and avoid disease progression.
Fecal markers are a heterogeneous group of biological substances formed by the inflamed intestinal mucosa or pass through it and enter the intestinal lumen and feces, where they can be measured. The advantage of fecal markers of inflammation over blood markers is that they provide information about the inflammatory process’s location, particularly the location along the gastrointestinal tract. Still, they also are not specific to IBD.
1. Fecal Alpha-1 Antitrypsin
Alpha-1 antitrypsin (AAT) is a serum protease inhibitor that constrains and modifies the effect of 90% of serum proteolytic enzymes—trypsin, neutrophil elastase, pancreatic elastase, serine protease, collagenase, kallikrein, and factor-8. Unlike other major serum proteins, it is highly resistant to intestinal protein degradation and is excreted intact in the feces [1]. In the presence of intestinal inflammation, due to increased permeability and impaired mucosal integrity, AAT excretion in the feces increases [2]. Elevated fecal AAT levels are found in protein-losing enteropathies, celiac disease, giardiasis, IBD, malignancies, etc. Various studies have been performed in patients with IBD to assess the relationship between fecal AAT concentration and disease activity. However, the results are contradictory [3][4][5][6].
2. Fecal Lactoferrin
Lactoferrin is an 80 kDa iron-binding protein. It is secreted by specific epithelial cells and can be found in various bodily fluids, including serum, tears, synovial fluid, and breast milk [7][8]. Besides, lactoferrin is the major protein in the secondary granules of polymorphonuclear granulocytes. It has both proinflammatory and anti-inflammatory properties [9]. In the presence of intestinal inflammation, polymorphonuclear cells infiltrate into the intestinal mucosa and subsequently enter the intestinal lumen, which results in a rise of the concentration of lactoferrin in the feces [10].
Fecal lactoferrin (FL) is stable for up to 5 days at room temperature. Its presence can be determined by qualitative and quantitative tests [11][12]. FL testing is used both in the diagnosis and in the follow-up of patients with IBD [11][13]. Its limitations as a marker in IBD are related to its non-specificity—elevated levels of FL are also found in various intestinal infections, during the administration of non-steroidal anti-inflammatory drugs (NSAIDs), in malignant intestinal diseases, etc.; to the fact that, in addition to neutrophils, it is secreted by other cells; and to the evidence of its lower accuracy as a laboratory indicator compared to fecal calprotectin (FC), a fecal marker that is most widely studied and used in clinical practice [14][15][16].
3. Fecal Calprotectin
Calprotectin is a small calcium and zinc-binding protein with a molecular weight of 36 kDa [17]. It was discovered in 1980 by Magne Fagerhol et al. and was initially named the L1 protein or leukocyte-derived L1 protein [18]. The name calprotectin was proposed after it was found to have antimicrobial (protective) properties and given its ability to bind calcium [19]. Calprotectin is a heterocomplex consisting of one light (8 kDa) and two heavy chains (14 kDa each), which are non-covalently linked [20]. It belongs to the group of S100 proteins [21]. S100 are low molecular weight proteins that bind calcium and participate in many intracellular and extracellular processes, including enzyme activation, cell growth, differentiation, inflammatory responses, etc. [22]. The genes encoding calprotectin and other S100 proteins are located in the long arm of chromosome 1q12–q21 [21].
Calprotectin is found predominantly in neutrophils, monocytes, and macrophages [23][24][25]. It makes up 5% of the total amount of protein and approximately 60% of the cytosolic proteins in neutrophils. In monocytes, it is approximately 1.6% of the total amount of protein [18][20]. Calprotectin features antimicrobial and antifungal activity [19][26]. Additionally, it inhibits cell growth and induces cell death in specific cell types such as fibroblasts, some tumor cells, and others [27][28][29]. Thus, as a result of its biological functions, it participates actively in regulating the inflammatory process. Upon stimulation, neutrophils and monocytes secrete calprotectin extracellularly [66]. Its extracellular release is also observed in cell destruction or cell death [30]. Typically, calprotectin can be found in plasma, synovial fluid, cerebrospinal fluid, saliva, urine, and feces [31][32]. An elevated level of calprotectin has been observed with increased accumulation of inflammatory cells in the course of an infection, some other inflammatory process, or malignancies [31].
In intestinal inflammation, the concentration of calprotectin in the feces is proportional to the degree of neutrophil infiltration into the intestinal wall, and the number of neutrophils in the intestinal lumen [33]. Elevated levels of FC are found in IBD, polyps, intestinal malignancies, intestinal infections, and others [32][33][34]. The use of NSAIDs and proton pump inhibitors and bleeding outside the gastrointestinal tract also elevates FC levels. Its concentration is physiologically higher in early childhood [34]. FC is homogeneously distributed in feces and is stable for up to 1 week at room temperature [32]. Significant differences in its concentration may be observed if measured sequentially on different days [35].
In recent years, FC has been widely studied as a marker in IBD. Its importance for diagnosing IBD, its role in monitoring patients with IBD to assess the disease activity and the response to therapy, and its ability to predict clinical recurrence or mucosal healing have been studied. The results generally show that FC helps to diagnose patients with IBD and facilitate patient follow-up by providing information on disease activity, the presence or absence of response to treatment, remission achieved, or recurrence risk [36]. The specific sensitivity and specificity of this indicator and the different correlation indices vary widely between the studies and depend on the studied population and the cut-off values used [36][37].
4. M2-Pyruvate Kinase
It was shown that fecal M2-PK concentrations are elevated in colorectal carcinoma and intestinal inflammation [38], indicating increased cell turnover. Moreover, it is believed that intestinal epithelial cells may be resistant to apoptosis by upregulation of M2-PK via the Bcl-xl pathway in CD [39].
Czub et al. tested fecal M2-PK levels in 107 Polish children with IBD (75 with UC, 32 with CD, and 35 healthy controls) [40]. M2-PK levels in stool samples were higher in children with IBD and were associated with the pediatric Crohn’s disease activity index (PCDAI). While mean M2-PK levels were higher in those with active disease, 47% of children with IBD deemed to be in remission still had elevated M2-PK levels. Another study, conducted by Day et al. (2012), also demonstrated higher fecal M2-PK in CD children but without an established association with PCDAI scores or serum inflammatory markers, such as fecal S100A12 [41]. Interestingly, children with ileocolonic disease appeared to have higher concentrations of M2-PK than those with isolated colonic or ileal disease.
Enhanced fecal M2-PK levels have also been seen in children with active UC [42]. Furthermore, M2-PK was superior to other markers (calprotectin, S100A12, and lactoferrin). In a 2014 study by Czub et al., when using Truelove–Witts score for UC patients and PCDAI for CD patients, M2-PK concentration was identified as inferior to calprotectin, especially in children in IBD remission. However, on the contrary, are the findings made by Roszak et al. [43] who suggest that M2-PK is a more sensitive marker to assess disease activity in pediatric UC or CD than calprotectin and lactoferrin. More studies are needed to explain this difference in this field.
5. Osteoprotegerin
Osteoprotegerin (OPG) belongs to the TNF superfamily and represents a cytokine receptor. A broad variety of cell types, distinct from those that produce calprotectin and lactoferrin, produce OPG—osteoblasts, B lymphocytes, dendritic cells, stromal bone marrow cells, epithelial cells, and monocytes/macrophages [39]. It is thought that OPG promotes bone formation, contrary to inflammatory cytokines such as IL-1, TNFα, etc. This is especially important for pediatric IBD, where the increased risk of fracture associated with the disease is described. Nevertheless, the role of OPG produced in the intestinal mucosa on bone loss in the IBD remains unresolved. Besides its bone turnover role, OPG exerts functions in IBD pathogenesis related to local and systemic inflammation [39].
A limited number of studies have shown that OPG is a useful biomarker of inflammation in pediatric IBD. Nahidi et al. [44] measured OPG in children with CD. Serum, stool, and biopsy samples showed dramatically rise in the OPG levels. Moreover, the remission after induction therapy dropped the serum and fecal levels substantially. Those children with isolated colonic CD had higher levels than those with ileocolonic form. However, serum and fecal of OPG did not correlate with the PCDAI scores, but with CRP and fecal S100A12 before and not after treatment.
Regarding pediatric UC, Sylvester et al. [45] assessed fecal OPG as a predictive marker for children’s treatment response. They demonstrated that patients with failed first-line corticosteroid therapy or who required infliximab or colectomy had elevated fecal OPG. Thus, OPG was superior to lactoferrin or S100A12 in predicting the treatment response. This gives us hope that it can be used for follow up and monitoring pediatric IBD patients. An important note is that OPG is more easily degraded at room temperature in the stool, and special preservation and storage conditions should be applied.
6. High Mobility Group Box Protein 1
High mobility group box protein 1 (HMGB1) is released by the immune cells during inflammation. Vitali et al. (2011) demonstrated that HMGB1 was significantly elevated in fecal and biopsy samples of children with IBD compared to healthy controls [46]. Furthermore, fecal HMGB1 correlated with FC, even though the cell sources for the two proteins are different. HMGB1 also correlates with mucosal changes in children with remission and active disease (moderate correlation with simple endoscopic score for Crohn’s disease (SES-CD) and endoscopic Mayo subscore. However, HMGB1 levels and activity indices (Crohn’s disease activity index (CDAI) and a partial UC Mayo score) did not correlate.
Accordingly, it is suggested that fecal HMGB1 as a marker of subclinical gut inflammation and a novel biomarker of mucosal healing [47], taking into account that it can be elevated in enteric infection as well [48]. It was also sown in animal models that HMGB1 could be treated with dipotassium glycyrrhizate or ethyl pyruvate, which should be further investigated in human IBD [39].
7. Chitinase 3-Like 1
Chitinase 3-like 1 (CHI3L1) expression in colonocytes and lamina propria macrophages is upregulated as a factor that facilitates bacterial penetration and adhesion to epithelial cells [39]. This protein was found elevated not only in adults with IBD but also in children. Aomatsu et al. [49] showed a marked increase of fecal CHI3L1 in children with IBD. Even a cut-off of 13.7 ng/g in fecal samples could differentiate between children’s IBD and controls with 84.7% sensitivity and 88.9% specificity. CHI3L1 levels were also shown to correlate with the scores for endoscopic severity of UC and CD, and with FC levels. The concentrations of the protein were dropped down in pediatric patients in remission.
Interestingly, CHI3L1 may be involved in neoplastic inflammation-related changes of the colonic epithelial cells in addition to his alleged role in IBD [50]. This, mainly, should be investigated further since the chronic inflammation accompanying IBD affects children early in their lives and may increase the cancerogenic susceptibility.
An overview of the fecal and serum biomarkers available for pediatric IBD is shown in Figure 1.
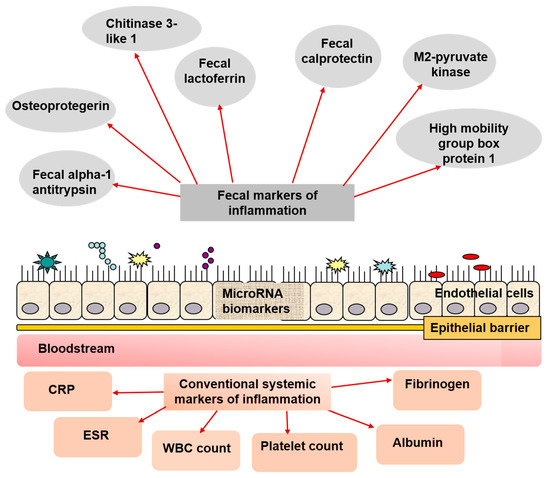
Figure 1. Biomarkers employed in pediatric IBD diagnosing, managing, and follow-up. Along with the conventional non-specific markers for inflammation, there are a great variety of fecal biomarkers that can be easily assessed in fecal samples, and in blood. A promising perspective is assessing microRNA in the mucosa, which alterations can be attributed to IBD, including in the pediatric practice.
It is worth mentioning that the most recent guidelines of ESPGHAN, NASPGHAN, and ECCO recommend the routine use of laboratory parameters not only for the diagnosis [51][52] but also for the management of pediatric IBD [53][54][55].
Blood tests (CBC, albumin, CRP, ESR, etc.) should be performed regularly by pediatric patients with UC depending on their symptoms and therapy and at least every three months while on immunosuppressive medications and at least every 6–12 months otherwise. Measurement of FC is advisable to verify mucosal healing in the patients in clinical remission, as a significant endoscopic activity may be present in 20% of children with PUCAI < 10. In addition, values of FC > 250 mg/g accurately predict mucosal inflammation and may select those patients who require endoscopic assessment and therapy escalation [53][54].
Regarding pediatric CD, repeat FC measurements in patients in clinical remission make it possible to identify a disease flare early, as FC increase precedes the disease relapse by 2–3 months. The combination of FC and CRP is superior in detecting endoscopic disease activity than FC alone. On the other side, the constellation of clinical remission, FC < 250 µg/g and CRP < 5 mg/L is the best non-invasive test for mucosal healing and can be used for treatment target [55].
The available information regarding the performance of all the discussed systemic and fecal markers for detecting intestinal inflammation and disease activity is presented in Table 1, when applicable.
Table 1. Laboratory markers for the pediatric inflammatory bowel disease (IBD) population. Not all proposed biomarkers have validated data on the cut-off, sensitivity, and specificity for detecting intestinal inflammation and disease activity in the pediatric population.
| Marker | Cut Off Value | Sensitivity | Specificity | Citation |
|---|---|---|---|---|
| C-reactive protein | 5 mg/L | 51–73% | 80–93% | Waugh et al., 2013 [56] |
| Erythrocyte sedimentation ratio | N/A | 58–73% | 80–88% | DeRidder et al., 2010 [57] |
| Fibrinogen | N/A | N/A | N/A | - |
| Albumin | N/A | 31–66% | 86–98% | Bossuyt et al., 2006 [58] |
| White blood cells | N/A | N/A | N/A | - |
| Platelet count | N/A | 36–73% | 81–93% | Van Rheenen et al., 2010 [59] |
| Fecal alpha-1 antitrypsin | N/A | N/A | N/A | - |
| Fecal lactoferrin | 13 μg/g | 80.7% | 92.7% | Borkowska et al., 2015 [60] |
| Fecal calprotectin | 50–275 μg/g | 94.4–100% | 71.9–100% | Sipponen et al., 2010 [61] |
| M2-pyruvate kinase | 4–5 U/g | 94.1–97.1% | 94.3–100% | Chung-Faye et al., 2007 [38] |
| Osteoprotegerin * | 50 pmol/L | 71% | 69% | Sylvester et al., 2011 [45] |
| High mobility group box protein 1 | N/A | N/A | N/A | - |
| Chitinase 3-like 1 | 13.7 ng/g | 81.6–84.7% | 90–100% | Aomatsu et al., 2011 [49] |
| microRNAs | N/A | N/A | N/A | - |
8. Novel Promising Biomarkers in Pediatric Inflammatory Bowel Disease
In addition to the well-established biomarkers for pediatric IBD management, some promising markers are likely to represent different cell origins and aspects of the IBD immunopathogenesis. Currently, no single novel marker appears as a highly specific, sensitive, diagnostic, and prognostic IBD predictor [39]. However, novel biomarkers must be tested comprehensively to ascertain their role in diagnosing, follow-up, and predicting disease behavior in children.
9. miRNAs in Pediatric IBD
The role of miRNAs is crucial to the development and homeostasis of the intestines. Many studies have shown that mature miRNAs are involved in forming proper intestinal structure and function [62][63]. Moreover, without specific miRNAs, the mouse’s intestinal epithelia lack proper barrier integrity goblet cells and simultaneously induce inflammation, which reminisces of IBD. Studies have shown so far that in various pathologies, including IBD, colorectal carcinoma [64], etc., miRNA expression is disrupted.
In adults with UC and CD, alterations in intestinal microRNAs have been identified. In children with IBD, however, the data on microRNA expression associated with colitis is still insufficient. In line with this, identifying molecular disorders can also lead to better management and care of pediatric IBDs. Moreover, since children frequently have a more severe phenotype, pediatric IBD pathogenesis can be molecularly distinct from adult IBD.
Zahm et al. (2014) researched specific rectal and serum microRNAs in pediatric IBD [65]. The results showed that the most abundant miRNAs were miR-21, miR-142-3p, comprising more than 20% of the overall miRNA of the rectal mucosal biopsies. Four miRNAs (miR-192, miR-194, miR-200b, and miR-375) were downregulated, and four (miR-21, miR-142-3p and miR-146a, and let-7i) were considerably increased in pediatric UC. In L2 CD patients, in comparison to controls, only miR-375 and miR-21 have been substantially modified [65]. Furthermore, in UC patients receiving 6-mercaptopurine or methotrexate immunomodulators, significant correlations were found between rectal miRNAs and the treatment. In contrast with UC patients lacking immunomodulators, these were seen to have substantially elevated miR-375 and miR-192. There was no correlation between miRNAs levels and the time needed for establishing the diagnosis of IBD [65].
It remains a struggle to distinguish UC from L2 CD in the pediatric population. Even after endoscopy, the diagnosis could not be straightforward. Compared CD to UC, the rectal miR-24 was the only microRNA altered between IBD subtypes, increased almost one and a half times in UC. On this basis, rectal miR-24 could correctly identify 84.2% of patients, with a sensitivity of 83.3% and specificity of 85.7%. The other investigated miRNAs, such as MiR-192, miR-142-3p, and miR-21, correctly distinct 78.72%, 72.34%, and 72.34% of patients, respectively. However, serum and rectal miRNAs did not show a correlation in this study. Further studies are required to confirm miRNA tissue biomarkers of IBD, L2 CD against UC in infants [65].
Previously, Zahm et al. (2011) reported rectal miRNAs consistent with colitis in children with IBD and controls. In children with IBD, miR-192 or miR-21 have been identified as elevated in pediatric CD [66]. On this basis, they suggested that circulating miRNAs are potential biomarkers of pediatric CD. Furthermore, the findings and preliminary research exploring miRNA shifts in adult IBD are broadly overlapping. Additionally, miRNAs are likely to contribute through targeted disease-related mRNAs to the pathogenesis of IBD.
References
- Sharp, H.L. The current status of alpha-1-antityrpsin, a protease inhibitor, in gastrointestinal disease. Gastroenterology 1976, 70, 611–621.
- Kosek, M.; Haque, R.; Lima, A. Fecal markers of intestinal inflammation and permeability associated with the subsequent acquisition of linear growth deficits in infants. Am. J. Trop. Med. Hyg. 2013, 88, 390–396.
- Fischbach, W.; Becker, W.; Mössner, J.; Koch, W.; Reiners, C. Faecal alpha-1-antitrypsin and excretion of 111indium granulocytes in assessment of disease activity in chronic inflammatory bowel diseases. Gut 1987, 28, 386–393.
- Grill, B.B.; Hillemeier, A.C.; Gryboski, J.D. Fecal alpha 1-antitrypsin clearance in patients with inflammatory bowel disease. J. Pediatr. Gastroenterol. Nutr. 1984, 3, 56–61.
- Meyers, S.; Wolke, A.; Field, S.P.; Feuer, E.J.; Johnson, J.W.; Janowitz, H.D. Fecal alpha-1-antitrypsin measurement: An indicator of Crohn’s disease activity. Gastroenterology 1985, 89, 13–18.
- Thomas, D.W.; Sinatra, F.R.; Merritt, R.J. Fecal α-1-antitrypsin excretion in young people with Crohn’s disease. J. Pediatr. Gastroenterol. Nutr. 1983, 2, 491–496.
- Masson, P.L.; Heremans, J.F.; Dive, C. An iron-binding protein common to many external secretions. Clinica Chimica Acta 1966, 14, 735–729.
- Masson, P.L.; Heremans, J.F.; Schonne, E. Lactoferrin, an iron-binding protein in neutrophilic leukocytes. J. Exp. Med. 1969, 130, 643–658.
- Mason, D.Y.; Taylor, C.R. Distribution of transferrin, ferritin, and lactoferrin in human tissues. J. Clin. Pathol. 1978, 31, 316–327.
- Desai, D.; Faubion, W.A.; Sandborn, W.J. Review article: Biological activity markers in inflammatory bowel disease. Aliment. Pharmacol. Ther. 2007, 25, 247–255.
- Sugi, K.; Saitoh, O.; Hirata, I.; Katsu, K. Fecal lactoferrin as a marker for disease activity in inflammatory bowel disease: Comparison with other neutrophil-derived proteins. Am. J. Gastroenterol. 1996, 91, 927–934.
- Uchida, K.; Matsuse, R.; Tomita, S.; Sugi, K.; Saitoh, O.; Ohshiba, S. Immunochemical detection of human lactoferrin in feces as a new marker for inflammatory gastrointestinal disorders and colon cancer. Clin. Biochem. 1994, 27, 259–264.
- Schoepfer, A.; Trummler, M.; Seeholzer, P.; Seibold-Schmid, B.; Seibold, F. Discriminating IBD from IBS: Comparison of the test performance of fecal markers, blood leukocytes, CRP, and IBD antibodies. Inflamm. Bowel Dis. 2008, 14, 32 39.
- Schroder, O.; Naumann, M.; Shastri, Y.; Povse, N.; Stein, J. Prospective evaluation of faecal neutrophil-derived proteins in identifying intestinal inflammation: Combination of parameters does not improve diagnostic accuracy of calprotectin. Aliment. Pharmacol. Ther. 2007, 26, 1035–1042.
- Silberer, H.; Kuppers, B.; Mickisch, O.; Baniewicz, W.; Drescher, M.; Traber, L.; Kempf, A.; Schmidt-Gayk, H. Fecal leukocyte proteins in inflammatory bowel disease and irritable bowel syndrome. Clin. Lab. 2005, 51, 117–126.
- Vrabie, R.; Kane, S. Noninvasive markers of disease activity in inflammatory bowel disease. Gastroenterol. Hepatol. 2014, 10, 576–584.
- Dale, I.; Fagerhol, M.K.; Naesgaard, I. Purification and partial characterization of a highly immunogenic human leukocyte protein, the L1 antigen. Eur. J. Biochem. 1983, 134, 1–6.
- Fagerhol, M.K.; Dale, I.; Andersson, T. Release and quantitation of a leucocyte derived protein (LI). Scand. J. Haematol. 1980, 24, 393–398.
- Steinbakk, M.; Naess-Andresen, C.F.; Lingaas, E.; Dale, I.; Brandtzaeg, P. Antimicrobial actions of calcium binding leucocyte L1 protein, calprotectin. Lancet 1990, 29, 336, 763–765.
- Fagerhol, M.K.; Andersson, K.B.; Naess-Andresen, C.F.; Brandtzaeg, P.; Dale, I.; Smith, V.L.; Dedman, J.R. Calprotectin (the L1 leukocyte protein). In Stimulus Response Coupling: The Role of Intracellular Calcium-Binding Proteins; Smith, V.L., Dedman, J.R., Eds.; CRC Press: Boca Raton, FL, USA, 1990; pp. 187–210.
- Dorin, J.R.; Emslie, E.; Van Heyningen, V. Related calcium-binding proteins map to the same subregion of chromosome 1q and to an extended region of synteny on mouse chromosome 3. Genomics 1990, 8, 420–426.
- Donato, R. Intracellular and extracellular roles of S100 proteins. Microsc. Res. Technique 2003, 60, 540–551.
- Dale, I.; Brandtzaeg, P.; Fagerhol, M.K.; Scott, H. Distribution of a new myelomonocytic antigen (L1) in human peripheral blood leukocytes. Immunofluorescence and immunoperoxidase staining features in comparison with lysozyme and lactoferrin. Am. J. Clin. Pathol. 1985, 84, 24–34.
- Rugtveit, J.; Brandtzaeg, P.; Halstensen, T.S.; Fausa, O.; Scott, H. Increased macrophage subset in inflammatory bowel disease: Apparent recruitment from peripheral blood monocytes. Gut 1994, 35, 669–674.
- Rugtveit, J.; Scott, H.; Halstensen, T.S.; Norstein, J.; Brandtzaeg, P. Expression of the L1 antigen (calprotectin) by tissue macrophages reflects recent recruitment from peripheral blood rather than upregulation of local synthesis: Implications for rejection diagnosis in formalin-fixed kidney specimens. J. Pathol. 1996, 180, 194–199.
- Nisapakultorn, K.; Ross, K.; Herzberg, M. calprotectin expression inhibits bacterial binding to mucosal epithelial cells. Infect. Immun. 2001, 69, 3692–3696.
- Ghavami, S.; Kerkhoff, C.; Los, M.; Hashemi, M.; Sorg, C.; Karami‐Tehrani, F. Mechanism of apoptosis induced by S100A8/A9 in colon cancer cell lines: The role of ROS and the effect of metal ions. J. Leukoc. Biol. 2004, 76, 169–175.
- Yui, S.; Mikami, M.; Tsurumaki, K.; Yamazaki, M. Growth-inhibitory and apoptosis-inducing activities of calprotectin derived from inflammatory exudate cells on normal fibroblasts: Regulation by metal ions. J. Leukoc. Biol. 1997, 61, 50–57.
- Yui, S.; Mikami, M.; Yamazaki, M. Induction of apoptotic cell death in mouse lymphoma and human leukemia cell lines by a calcium-binding protein complex, calprotectin, derived from inflammatory peritoneal exudate cells. J. Leukoc. Biol. 1995, 58, 650–658.
- Voganatsi, A.; Panyutich, A.; Miyasaki, K.T.; Murthy, R.K. Mechanism of extracellular release of human neutrophil calprotectin complex. J. Leukoc. Biol. 2001, 70, 130–134.
- Sander, J.; Fagerhol, M.K.; Bakken, J.S.; Dale, I. Plasma levels of the leucocyte L1 protein in febrile conditions: Relation to aetiology, number of leucocytes in blood, blood sedimentation reaction and C-reactive protein. Scand. J. Clin. Lab. Invest. 1984, 44, 357–362.
- Røseth, A.G.; Fagerhol, M.K.; Aadland, E.; Schjønsby, H. Assessment of the neutrophil dominating protein calprotectin in feces. A methodologic study. Scand. J. Gastroenterol. 1992, 27, 793–798.
- Røseth, A.G.; Schmidt, P.N.; Fagerhol, M.K. Correlation between faecal excretion of indium-111-labelled granulocytes and calprotectin, a granulocyte marker protein, in patients with inflammatory bowel disease. Scand. J. Gastroenterol. 1999, 34, 50–54.
- Røseth, A.G.; Kristinsson, J.; Fagerhol, M.K.; Schjønsby, H.; Aadland, E.; Nygaard, K.; Roald, B. Faecal calprotectin: A novel test for the diagnosis of colorectal cancer? Scand. J. Gastroenterol. 1993, 28, 1073–1076.
- Mulder, D.; Noble, A.; Justinic, C.J.; Duffin, J.M. A tale of two diseases: The history of inflammatory bowel disease. J. Crohn’s Colitis 2014, 8, 341–348.
- Kostakis, I.; Cholidou, K.; Vaiopoulos, A.; Vlachos, I.S.; Perrea, D.; Vaos, G. Fecal calprotectin in pediatric inflammatory bowel disease: A systematic review. Dig. Dis. Sci. 2013, 58, 309–319.
- D’Angelo, F.; Felley, C.; Frossard, J.L. Calprotectin in daily practice: Where do we stand in 2017? Digestion 2017, 95, 293–301.
- Chung-Faye, G.; Hayee, B.; Maestranzi, S.; Donaldson, N.; Forgacs, I.; Sherwood, R. Fecal M2-pyruvate kinase (M2-PK): A novel marker of intestinal inflammation. Inflamm. Bowel Dis. 2007, 13, 1374–1378.
- Duvoisin, G.; Lopez, R.N.; Day, A.S.; Lemberg, D.A.; Gearry, R.B.; Leach, S.T. Novel biomarkers and the future potential of biomarkers in inflammatory bowel disease. Mediat. Inflamm. 2017, 2017, 1936315, doi:10.1155/2017/1936315.
- Czub, E.; Herzig, K.H.; Szaflarska-Popawska, A.; Kiehne, K.; Socha, P.; Woś, H.; Kamińska, B.; Błaszczyński, M.; Cichy, W.; Bała, G.; et al. Fecal pyruvate kinase: A potential new marker for intestinal inflammation in children with inflammatory bowel disease. Scand. J. Gastroenterol. 2007, 42, 1147 1150.
- Day, A.S.; Judd, T.; Lemberg, D.A.; Leach, S.T. Fecal M2-PK in children with Crohn’s disease: A preliminary report. Dig. Dis. Sci. 2012, 57, 2166–2170.
- Czub, E.; Nowak, J.K.; Szaflarska-Poplawska, A.; Grzybowska-Chlebowczyk, U.; Landowski, P.; Moczko, J.; Adamczak, D.; Mankowski, P.; Banasiewicz, T.; Plawski, A.; et al. Comparison of fecal pyruvate kinase isoform M2 and calprotectin in assessment of pediatric inflammatory bowel disease severity and activity. Acta Biochimica Polonica 2014, 61, 99–102.
- Roszak, D.; Galecka, M.; Cichy, W.; Szachta, P. Determination of faecal inflammatory marker concentration as a non-invasive method of evaluation of pathological activity in children with inflammatory bowel diseases. Adv. Med Sci. 2015, 60, 246–252.
- Nahidi, L.; Leach, S.T.; Sidler, M.A.; Levin, A.; Lemberg, D.A.; Day, A.S. Osteoprotegerin in pediatric Crohn’s disease and the effects of exclusive enteral nutrition. Inflamm. Bowel Dis. 2011, 17, 516–523.
- Sylvester, F.A.; Turner, D.; Draghi, A.; Uuosoe, K.; McLernon, R.; Koproske, K.; Mack, D.R.; Crandall, W.V.; Hyams, J.S.; LeLeiko, N.S.; et al. Fecal osteoprotegerin may guide the introduction of second-line therapy in hospitalized children with ulcerative colitis. Inflamm. Bowel Dis 2011, 17, 1726–1730.
- Vitali, R.; Stronati, L.; Negroni, A.; Di Nardo, G.; Pierdomenico, M.; Del Giudice, E.; Rossi, P.; Cucchiara, S. Fecal HMGB1 is a novel marker of intestinal mucosal inflammation in pediatric inflammatory bowel disease. Am. J. Gastroenterol. 2011, 106, 2029–2040.
- Dong, W.G.; Liu, S.P.; Zhu, H.H.; Luo, H.S.; Yu, J.P. Abnormal function of platelets and role of Angelica sinensis in patients with ulcerative colitis. World J. Gastroenterol. 2004, 10, 606–609.
- Poullis, A.; Foster, R.; Mendall, M.A. Proton pump inhibitors are associated with elevation of faecal calprotectin and may affect specificity. Eur. J. Gastroenterol. Hepatol. 2003, 15, 573–574.
- Aomatsu, T.; Imaeda, H.; Matsumoto, K.; Kimura, E., Yoden, A.; Tamai, H.; Fujiyama, Y.; Mizoguchi, E.; Andoh, A. Faecal chitinase 3-like-1: A novel biomarker of disease activity in paediatric inflammatory bowel disease. Aliment. Pharmacol. Ther. 2011, 34, 941–948.
- Chen, C.C.; Pekow, J.; Llado, V.; Kanneganti, M.; Lau, C.W.; Mizoguchi, A.; Mino-Kenudson, M.; Bissonnette, M.; Mizoguchi, E. Chitinase 3-like-1 expression in colonic epithelial cells as a potentially novel marker for colitis-associated neoplasia. Am. J. Pathol. 2011, 179, 1494–1503.
- Escher, J.C.; Dias, J.A.; Bochenek, K.; Buderus, S.; De Mesquita, M.B.; Bujanover, Y.; Büller, H.A.; Chong, S.K.F.; Cucchiara, S.; Fell, J.M.; et al. IBD Working Group of the European Society for Paediatric Gastroenterology, Hepatology and Nutrition. Inflammatory bowel disease in children and adolescents: Recommendations for diagnosis—the Porto criteria. J. Pediatr. Gastroenterol. Nutr. 2005, 41, 1–7.
- Levine, A.; Koletzko, S.; Turner, D.; Escher, J.C.; Cucchiara, S.; De Ridder, L.; Kolho, K.L.; Veres, G.; Russell, R.K.; Paerregaard, A.; et al. ESPGHAN revised Porto criteria for the diagnosis of inflammatory bowel disease in children and adolescents. J. Pediatr. Gastroenterol. Nutr. 2014, 58, 795–806.
- Turner, D.; Ruemmele, F.M.; Orlanski-Meyer, E.; Griffiths, A.M.; De Carpi, J.M.; Bronsky, J.; Veres, G.; Aloi, M.; Strisciuglio, C.; Braegger, C.P.; et al. Management of paediatric ulcerative colitis, part 1: Ambulatory care-an evidence-based guideline from European Crohn’s and colitis organization and European society of paediatric gastroenterology, hepatology and nutrition. J. Pediatr. Gastroenterol. Nutr. 2018, 67, 257–291.
- Turner, D.; Ruemmele, F.M.; Orlanski-Meyer, E.; Griffiths, A.M.; de Carpi, J.M.; Bronsky, J.; Veres, G.; Aloi, M.; Strisciuglio, C.; Braegger, C.P.; et al. Management of paediatric ulcerative colitis, Part 2: Acute severe colitis-an evidence-based consensus guideline from the European Crohn’s and colitis organization and the European society of paediatric gastroenterology, hepatology and nutrition. J. Pediatr. Gastroenterol. Nutr. 2018, 67, 292–310.
- Van Rheenen, P.F.; Aloi, M.; Assa, A.; Bronsky, J.; Escher, J.C.; Fagerberg, U.L.; Gasparetto, M.; Gerasimidis, K.; Griffiths, A.; Henderson, P.; et al. The medical management of paediatric Crohn’s disease: An ECCO-ESPGHAN guideline update. J. Crohns Colitis 2020, 7, 1–24.
- Waugh, N.; Cummins, E.; Royle, P.; Kandala, N.B., Shyangdan, D.; Arasaradnam, R.; Clar, C.; Johnston, R. Faecal calprotectin testing for differentiating amongst inflammatory and non-inflammatory bowel diseases: Systematic review and economic evaluation. Health Technol. Assess. 2013, 17, 15–19.
- DeRidder, L.; Rings, E.H.; Escher, J.C. Guideline diagnosis and treatment of inflammatory bowel disease in children. Nederlands Tijdschrift Voor Geneeskunde 2009, 154, A1898.
- Bossuyt, P.M.; Irwig, L.; Craig, J.; Glasziou, P. Comparative accuracy: Assessing new tests against existing diagnostic pathways. BMJ 2006, 332, 1089.
- Van Rheenen, P.F.; Van de Vijver, E.; Fidler, V. Faecal calprotectin for screening of patients with suspected inflammatory bowel disease: Diagnostic meta-analysis. BMJ 2010, 341, 3369.
- Borkowska, A.; Liberek, A.; Łuczak, G.; Jankowska, A.; Plata-Nazar, K.; Korzon, M.; Kamińska, B. Fecal lactoferrin, a marker of intestinal inflammation in children with inflammatory bowel disease. Acta Biochimica Polonica 2015, 62, 541–545.
- Sipponen, T.; Kolho, K.L. Faecal calprotectin in children with clinically quiescent inflammatory bowel disease. Scand. J. Gastroenterol. 2010, 45, 872–877.
- McKenna, L.B.; Schug, J.; Vourekas, A.; McKenna, J.B.; Bramswig, N.C.; Friedman, J.R.; Kaestner, K.H. MicroRNAs control intestinal epithelial differentiation, architecture, and barrier function. Gastroenterology 2010, 139, 1654–1664.
- Biton, M.; Levin, A.; Slyper, M.; Alkalay, I.; Horwitz, E.; Mor, H.; Kredo-Russo, S.; Avnit-Sagi, T.; Cojocaru, G.; Zreik, F.; et al. Epithelial microRNAs regulate gut mucosal immunity via epithelium-T cell crosstalk. Nat. Immunol. 2011, 12, 239–246.
- Peruhova, M.; Peshevska-Sekulovska, M.; Krastev, B.; Panayotova, G.; Georgieva, V.; Konakchieva, R.; Nikolaev, G.; Velikova, T.V. What could microRNA expression tell us more about colorectal serrated pathway carcinogenesis? World J. Gastroenterol. 2020, 26, 6556–6571.
- Zahm, A.M.; Hand, N.J.; Tsoucas, D.M.; Le Guen, C.L.; Baldassano, R.N.; Friedman, J.R. Rectal microRNAs are perturbed in pediatric inflammatory bowel disease of the colon. J. Crohn’s Colitis 2014, 8, 1108–1117.
- Zahm, A.M.; Thayu, M.; Hand, N.J.; Horner, A.; Leonard, M.B.; Friedman, J.R. Circulating microRNA is a biomarker of pediatric Crohn disease. J. Pediatr. Gastroenterol. Nutr. 2011, 53, 26–33.




