Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Ronald B. Brown | -- | 1686 | 2024-03-13 14:02:34 | | | |
| 2 | Peter Tang | Meta information modification | 1686 | 2024-03-14 03:38:11 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Brown, R.B. SIDS, Pulmonary Edema, and Sodium Toxicity. Encyclopedia. Available online: https://encyclopedia.pub/entry/56217 (accessed on 08 February 2026).
Brown RB. SIDS, Pulmonary Edema, and Sodium Toxicity. Encyclopedia. Available at: https://encyclopedia.pub/entry/56217. Accessed February 08, 2026.
Brown, Ronald B.. "SIDS, Pulmonary Edema, and Sodium Toxicity" Encyclopedia, https://encyclopedia.pub/entry/56217 (accessed February 08, 2026).
Brown, R.B. (2024, March 13). SIDS, Pulmonary Edema, and Sodium Toxicity. In Encyclopedia. https://encyclopedia.pub/entry/56217
Brown, Ronald B.. "SIDS, Pulmonary Edema, and Sodium Toxicity." Encyclopedia. Web. 13 March, 2024.
Copy Citation
Sudden Infant Death Syndrome (SIDS) occurs unexpectedly in an otherwise healthy infant with no identifiable cause of death following a thorough investigation. A general hypervolemic state has been identified in SIDS, and fluid in the lungs suggests the involvement of pulmonary edema and hypoxia as the cause of death.
sudden infant death syndrome
SIDS
pulmonary edema
hypoxia
sodium chloride
hypervolemia
fever
alveolar epithelium
microvascular endothelium
1. Introduction
Sudden infant death syndrome (SIDS) is currently defined by the World Health Organization (WHO) as “the abrupt and unexplained death of an apparently healthy infant under one year of age, remaining unexplained after a thorough case investigation, including performance of a complete autopsy, examination of the death scene, and review of the clinical history” [1]. Accidental suffocation/asphyxia and deaths due to uncertain circumstances are listed separately from SIDS, under sudden unexpected infant death (SUID) [2]. This diagnostic shift reassigns asphyxia or undetermined causes to the sleep environment, which “serves to underestimate the actual mortality of what was once considered SIDS” [3].
Autopsy findings of SIDS cases include increased brain weight, possibly caused by cerebral edema “secondary to hypoxia/anoxia or toxic/metabolic factors” [4]. However, further postmortem examinations suggest that environmental toxins, including lead, mercury, and arsenic, are not a cause of SIDS [5]. On the other hand, sodium toxicity, the toxic effect from acute salt poisoning [6] or from prolonged intake of excessive dietary sodium [7], is an unexamined toxic factor potentially involved in SIDS.
Excessive dietary salt intake (sodium chloride) is strongly associated with hypervolemia, fluid overload [8], and blood–brain barrier dysregulation [9]. Of relevance, “abnormalities of regulation of the blood brain barrier with disturbances in water homeostasis” could contribute to increased brain weight in SIDS, although possible causes remain controversial [10]. Other organs with increased weight in SIDS include the thymus, liver, and lungs [4].
2. Alveolar Epithelial Permeability
Noncardiogenic pulmonary edema is unrelated to the increased vascular hydrostatic pressure in cardiogenic pulmonary edema usually seen in heart failure. In noncardiogenic pulmonary edema, disruption of the microvascular endothelial barrier increases permeability to fluid, which then fills the interstitium. Disruption of the alveolar epithelial barrier additionally increases permeability to interstitial fluid that floods the alveolus [11]; see Figure 1. This influx of edematous fluid may contain red blood cells [12].
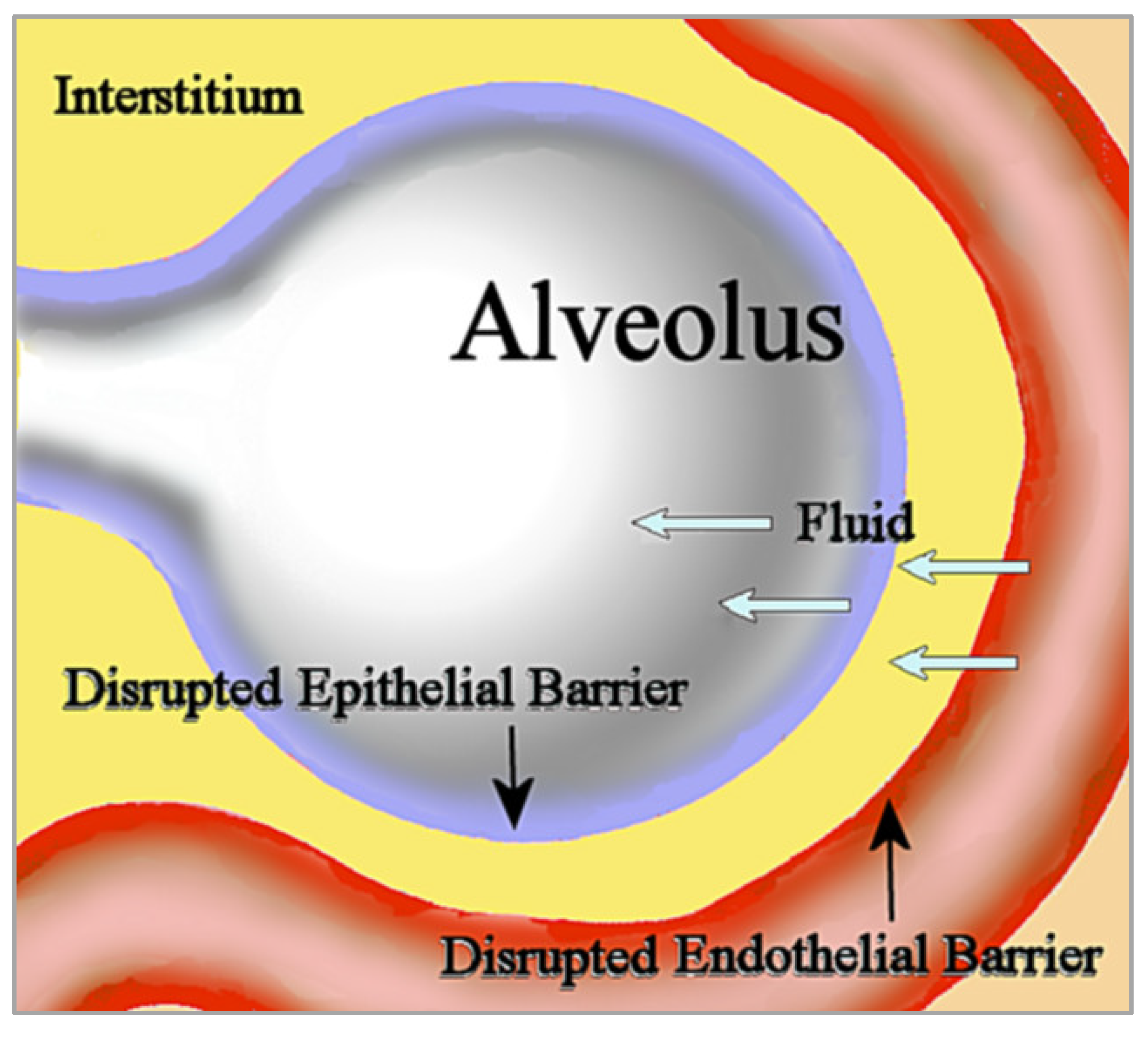
Figure 1. In noncardiogenic pulmonary edema, fluid flows into the interstitium through the disrupted microvascular endothelial barrier, then subsequently flows into the alveolus through the disrupted epithelial barrier.
Importantly, “resolution of alveolar oedema depends on the active removal of salt and water from the distal air spaces of the lung across the distal lung epithelial barrier” [13]. Salt water aspiration is a well-known cause of acute salt water-induced lung injury, and produces severe pulmonary edema, hypoxia, inflammation, apoptosis, and oxidative stress [14][15]. Of relevance, rapid administration of intravenous 0.9% saline (sodium chloride) can cause lung injury and interstitial permeability pulmonary edema in healthy volunteers [16], and acute and chronic salt load from intravenous hypertonic saline infusions in healthy participants in a randomized intervention increased microvascular permeability, with “direct effects on the endothelial surface layer” [17].
Figure 2 shows a directed acyclic graph in which the association of sodium toxicity with SIDS is mediated by microvascular endothelial barrier disruption, alveolar epithelial barrier disruption, pulmonary edema, and hypoxia.

Figure 2. The association of sodium toxicity with sudden infant death syndrome (dotted arrow) is mediated (straight arrows) by disruptions of the microvascular endothelial and alveolar epithelial barriers in the lungs, leading to pulmonary edema and hypoxia (straight arrows).
3. Sodium Channelopathies and SIDS
Impaired contraction of skeletal respiratory muscles, thought to contribute to respiratory failure in SIDS, is caused by variants in the voltage-gated sodium channel NaV1.4, which is encoded by the SCN4A gene. A case-control study found that variants of SCN4A caused dysfunctional sodium channels in SIDS cases but not in controls [18].
Disturbances in sodium and water homeostasis commonly occur in severely ill neurology patients, and “have a profound effect on the brain” [19]. This effect suggests a potential link between dysfunctional sodium channelopathies in the brain and brainstem alterations thought to affect respiration in SIDS, such as reduced levels of serotonin 5-HT neurotransmitter [20], although more research is needed in this area. Similar to sodium channelopathies in SIDS that affect respiratory muscles and arrhythmias, future studies should investigate whether brainstem alternations in SIDS are a side effect of sodium toxicity rather than the key pathophysiological mechanism leading to respiratory failure.
4. Hyperthermia and Fever
Hyperthermia and fever are pathological factors associated with SIDS; the bodies of deceased children with SIDS are often found hot and sweaty, suggesting that environmental conditions that cause hyperthermia, such as overclothing and heavy bedding, may be causative factors in SIDS [21]. However, heat stress is not a direct or significant cause of SIDS [22]. Importantly, whereas hyperthermia related to heat stress is an unregulated rise of core body temperature due to environmental conditions, fever is a regulated increase in internal temperature due to resetting by the hypothalamus, and is often seen in infections [21]. Additionally, “many SIDS infants have a history of viral illness preceding death” [23], and the number of cases of SIDS reported to have had weekly or more frequent “drenching’” sweats was much higher than control cases [24], likely related to fever in respiratory infections [23].
5. Intrathoracic Petechial Hemorrhages
Among the distinctive features of SIDS, small blood vessel haemorrhages appear on the surface of the heart, lungs, and thymus, called intrathoracic petechiae; “the almost universal finding of intrathoracic petechiae in SIDS stands out as a poorly investigated phenomenon” [25]. Early investigators suggested petechiae in SIDS were caused by respiratory obstruction, although similar petechiae in infants were not found in cases of suffocation or asphyxia [26]. While subpleural and subpericardial hemorrhages are a sign of terminal respiratory obstruction, petechiae in SIDS may be related to other factors. Furthermore, salt induces endothelial cell secretion of the Willebrand factor, which causes hypercoagulability in blood clotting [27], and damage to the endothelial glycocalyx from excessive sodium impairs inhibition of platelet aggregation and adhesion, which “is thought to contribute to thrombosis formation” [28]. These mechanisms imply that intrathoracic petechial hemorrhages in SIDS may be associated with blood clotting in small vessels of the heart, lungs, and thymus from exposure to high salt concentrations. More research is needed in this area.
6. Sodium and Near-Miss SIDS
In near-miss SIDS, subsequently categorized as ALTE (apparent life-threatening event) and more recently as BRUE (brief resolved unexplained event) [29], infants rescued from hypoxia where found to have “metabolic acidosis, cardiovascular instability, acute renal failure, ischaemic colitis, or acute neurological dysfunction” [30]. Each of these conditions in near-miss SIDS cases is potentially linked with dysregulated sodium. For example, metabolic acidosis found in rat models of salt-sensitive hypertension was associated with a high-salt diet [31]. Colitis in experiments with mice was exacerbated by a high-salt diet, which was suggested as being caused by inflammatory changes in the gut microbiota [32]. Furthermore, acute kidney injury is exacerbated by excessive salt intake [33], unstable cardiac status is associated with extreme hypernatremia [34], and neurological injury is caused by salt toxicity from rapid ingestion of massive amounts of sodium chloride [35]. These findings provide further support for the involvement of sodium toxicity in SIDS.
7. Diet, Sodium, and SIDS
Breastfed infants have lower risk of SIDS compared to non-breastfed infants [36]. Of significance, human breast milk is much lower in sodium compared to cow milk [37], at 15 mg and 43 mg/100 g, respectively [38]. “Infants’ systems cannot handle the high levels of protein, sodium, and potassium of unmodified cow milk”, while infant formula based on modified cow milk “attempts to mimic the nutritional composition of breast milk” [39]. However, according to the World Health Organization, “formula milk marketing, not the product itself, disrupts informed decision-making and undermines breastfeeding and child health” [40]. By comparison, breastfed milk precludes infants’ exposure to sodium salts used in food processing [37][41], which potentially reduces risk of sodium toxicity in breastfed infants compared to formula-fed infants.
As more foods and beverages are gradually introduced into the young child’s diet, intake levels of sodium, calories, and sugar “escalate upward from recommendations in toddlers, becoming even more pronounced among young children” [42]. Note that sodium chloride contains 40% sodium by weight. The World Health Organization recently established new benchmarks to reduce global mean sodium intake by 30%, “with the aim of achieving a target of less than 5 g of salt (i.e., <2 g of sodium) per day by 2025” [43].
Importantly:
“Infants are less efficient than adults at excreting excess sodium, and the sodium intakes of infants should therefore be moderated. By about four months, healthy infants can begin to excrete an excessive sodium load”[44]
Consequently, increased incidence of SIDS, which peaks between 2–4 months from birth [45], occurs during a developmental period when infants are most vulnerable to harm from excessive sodium intake.
In addition to high sodium levels, cow milk is much higher in phosphorus than breast milk, and excessive dietary phosphate has been linked to degeneration of dopaminergic neurons [46]. Coincidently, a recent study found degeneration of dopaminergic neurons in the majority of 36 SIDS cases, compared to no effect in control infants [47], a finding that is concordant with harm in SIDS from cow milk consumption. Infants’ exposure to excessive minerals in cow milk and other solid foods with potential risk associated with sodium toxicity and SIDS can be reduced by recommendation of exclusive breastfeeding during the first six months after birth, as advised by the American Academy of Pediatrics [48] and the World Health Organization [49].
8. Seasonality and Socioeconomic Status in SIDS
Other dietary factors related to SIDS are associated with seasonality and socioeconomic status. Increased seasonal incidence of SIDS is associated with winter, which is concurrent with increased respiratory infections during colder months [50]. However, seasonal SIDS incidence is also concurrent with cold-weather changes in diet. For example, mice increase sodium intake with exposure to cold temperatures [51], and higher estimated salt intake is associated with daytime cold exposure in elderly humans [52]. Studies should investigate infants’ increased sodium intake in winter and potential associations with increased SIDS incidence.
SIDS is more prevalent in populations with lower socioeconomic status (SES), according to an analysis of education, employment, and income factors [53]. Coincidently, dietary sodium intake is higher in children from populations with lower SES as well [54][55], leading to the inference that sodium toxicity is a potential mediating factor that may increase risk of SIDS in populations with lower SES.
References
- WHO. International Classification of Diseases for Mortality and Morbidity Statistics, 11th ed.; WHO: Geneva, Switzerland, 2018.
- Kim, H.; Pearson-Shaver, A.L. Sudden Infant Death Syndrome. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 2022.
- Goldstein, R.D.; Blair, P.S.; Sens, M.A.; Shapiro-Mendoza, C.K.; Krous, H.F.; Rognum, T.O.; Moon, R.Y. Inconsistent classification of unexplained sudden deaths in infants and children hinders surveillance, prevention and research: Recommendations from The 3rd International Congress on Sudden Infant and Child Death. Forensic Sci. Med. Pathol. 2019, 15, 622–628.
- Goldwater, P.N. Sudden infant death syndrome: A critical review of approaches to research. Arch. Dis. Child. 2003, 88, 1095–1100.
- Althoff, H.; Wehr, K.; Michels, S.; Prajsnar, D. Toxic environmental factors in sudden infant death (SIDS). Z. Rechtsmed. 1987, 98, 103–110.
- Mehlenbacher, G.; Garbach, D.; Eggleston, W.; Gorodetsky, R.; Nacca, N. Death from salt and baking soda ingestion. Toxicol. Commun. 2020, 4, 15–17.
- Soloway, R.A.G. Sodium: Too Much of a Good Thing. The Dangers of Sodium Poisoning. Available online: https://www.poison.org/articles/sodium-too-much-of-a-good-thing (accessed on 7 June 2022).
- Borrelli, S.; Provenzano, M.; Gagliardi, I.; Michael, A.; Liberti, M.E.; De Nicola, L.; Conte, G.; Garofalo, C.; Andreucci, M. Sodium Intake and Chronic Kidney Disease. Int. J. Mol. Sci. 2020, 21, 4744.
- Zhang, T.; Fang, S.; Wan, C.; Kong, Q.; Wang, G.; Wang, S.; Zhang, H.; Zou, H.; Sun, B.; Sun, W.; et al. Excess salt exacerbates blood-brain barrier disruption via a p38/MAPK/SGK1-dependent pathway in permanent cerebral ischemia. Sci. Rep. 2015, 5, 16548.
- Elliott, J.A.; Vink, R.; Jensen, L.; Byard, R.W. Brain weight-body weight ratio in sudden infant death syndrome revisited. Med. Sci. Law 2012, 52, 207–209.
- Ware, L.B.; Matthay, M.A. Clinical practice. Acute pulmonary edema. N. Engl. J. Med. 2005, 353, 2788–2796.
- Matthay, M.A.; Zemans, R.L.; Zimmerman, G.A.; Arabi, Y.M.; Beitler, J.R.; Mercat, A.; Herridge, M.; Randolph, A.G.; Calfee, C.S. Acute respiratory distress syndrome. Nat. Rev. Dis. Primers 2019, 5, 18.
- Sartori, C.; Matthay, M.A. Alveolar epithelial fluid transport in acute lung injury: New insights. Eur. Respir. J. 2002, 20, 1299–1313.
- Schober, P.; Seidel, D.; Kalb, R.; Obal, D.; Pakulla, M.A.; Loer, S.A. Partial liquid ventilation in acute salt water-induced lung injury. Eur. J. Anaesthesiol. 2005, 22, 536–540.
- Jin, F.; Li, C. Seawater-drowning-induced acute lung injury: From molecular mechanisms to potential treatments. Exp. Ther. Med. 2017, 13, 2591–2598.
- Li, H.; Bersten, A.; Wiersema, U.; Schembri, D.; Cavallaro, E.; Dixon, D.L.; Bihari, S. Bolus intravenous 0.9% saline leads to interstitial permeability pulmonary edema in healthy volunteers. Eur. J. Appl. Physiol. 2021, 121, 3409–3419.
- Rorije, N.M.G.; Olde Engberink, R.H.G.; Chahid, Y.; van Vlies, N.; van Straalen, J.P.; van den Born, B.-J.H.; Verberne, H.J.; Vogt, L. Microvascular Permeability after an Acute and Chronic Salt Load in Healthy Subjects: A Randomized Open-label Crossover Intervention Study. Anesthesiology 2018, 128, 352–360.
- Männikkö, R.; Wong, L.; Tester, D.J.; Thor, M.G.; Sud, R.; Kullmann, D.M.; Sweeney, M.G.; Leu, C.; Sisodiya, S.M.; FitzPatrick, D.R.; et al. Dysfunction of NaV1.4, a skeletal muscle voltage-gated sodium channel, in sudden infant death syndrome: A case-control study. Lancet 2018, 391, 1483–1492.
- Tisdall, M.; Crocker, M.; Watkiss, J.; Smith, M. Disturbances of sodium in critically ill adult neurologic patients: A clinical review. J. Neurosurg. Anesth. 2006, 18, 57–63.
- Brummelte, S.; Mc Glanaghy, E.; Bonnin, A.; Oberlander, T.F. Developmental changes in serotonin signaling: Implications for early brain function, behavior and adaptation. Neuroscience 2017, 342, 212–231.
- Bach, V.; Libert, J.P. Hyperthermia and Heat Stress as Risk Factors for Sudden Infant Death Syndrome: A Narrative Review. Front. Pediatr. 2022, 10, 816136.
- Scheers-Masters, J.R.; Schootman, M.; Thach, B.T. Heat stress and sudden infant death syndrome incidence: A United States population epidemiologic study. Pediatrics 2004, 113, e586–e592.
- Blood-Siegfried, J. The role of infection and inflammation in sudden infant death syndrome. Immunopharmacol. Immunotoxicol. 2009, 31, 516–523.
- Taylor, B.J.; Williams, S.M.; Mitchell, E.A.; Ford, R.P. Symptoms, sweating and reactivity of infants who die of SIDS compared with community controls. New Zealand National Cot Death Study Group. J. Paediatr. Child Health 1996, 32, 316–322.
- Goldwater, P.N. The Science (or Nonscience) of Research Into Sudden Infant Death Syndrome (SIDS). Front. Pediatr. 2022, 10, 865051.
- Beckwith, J.B. Intrathoracic petechial hemorrhages: A clue to the mechanism of death in sudden infant death syndrome? Ann. N. Y. Acad. Sci. 1988, 533, 37–47.
- Dmitrieva, N.I.; Burg, M.B. Secretion of von Willebrand factor by endothelial cells links sodium to hypercoagulability and thrombosis. Proc. Natl. Acad. Sci. USA 2014, 111, 6485–6490.
- Fraser, D.D.; Patterson, E.K.; Slessarev, M.; Gill, S.E.; Martin, C.; Daley, M.; Miller, M.R.; Patel, M.A.; Dos Santos, C.C.; Bosma, K.J.; et al. Endothelial Injury and Glycocalyx Degradation in Critically Ill Coronavirus Disease 2019 Patients: Implications for Microvascular Platelet Aggregation. Crit. Care Explor. 2020, 2, e0194.
- Behnam-Terneus, M.; Clemente, M. SIDS, BRUE, and Safe Sleep Guidelines. Pediatr. Rev. 2019, 40, 443–455.
- Constantinou, J.E.; Gillis, J.; Ouvrier, R.A.; Rahilly, P.M. Hypoxic-ischaemic encephalopathy after near miss sudden infant death syndrome. Arch. Dis. Child. 1989, 64, 703–708.
- Sharma, A.M.; Kribben, A.; Schattenfroh, S.; Cetto, C.; Distler, A. Salt sensitivity in humans is associated with abnormal acid-base regulation. Hypertension 1990, 16, 407–413.
- Miranda, P.M.; De Palma, G.; Serkis, V.; Lu, J.; Louis-Auguste, M.P.; McCarville, J.L.; Verdu, E.F.; Collins, S.M.; Bercik, P. High salt diet exacerbates colitis in mice by decreasing Lactobacillus levels and butyrate production. Microbiome 2018, 6, 57.
- Wang, C.T.; Tezuka, T.; Takeda, N.; Araki, K.; Arai, S.; Miyazaki, T. High salt exacerbates acute kidney injury by disturbing the activation of CD5L/apoptosis inhibitor of macrophage (AIM) protein. PLoS ONE 2021, 16, e0260449.
- Arambewela, M.H.; Somasundaram, N.P.; Garusinghe, C. Extreme hypernatremia as a probable cause of fatal arrhythmia: A case report. J. Med. Case Rep. 2016, 10, 272.
- Metheny, N.A.; Krieger, M.M. Salt Toxicity: A Systematic Review and Case Reports. J. Emerg. Nurs. 2020, 46, 428–439.
- Landa-Rivera, J.L.; Pérez-Pérez, J.; González-Núñez, M.D.P.; Gil-Miralles, R.A.; Jover-Escolano, Y.; Fernández-Pan Astacio, V. Population-Based Survey Showing That Breastfed Babies Have a Lower Frequency of Risk Factors for Sudden Infant Death Syndrome Than Nonbreastfed Babies. Breastfeed. Med. 2022, 17, 182–188.
- Camara, A.O.d.; Rodrigues, L.G.; Ferreira, T.d.S.; Moraes, O.M.G.d. Sodium found in processed cow milk and estimated intake by infants. J. Pediatr. 2021, 97, 665–669.
- Pietrzak-Fiećko, R.; Kamelska-Sadowska, A.M. The Comparison of Nutritional Value of Human Milk with Other Mammals’ Milk. Nutrients 2020, 12, 1404.
- Martin, C.R.; Ling, P.R.; Blackburn, G.L. Review of Infant Feeding: Key Features of Breast Milk and Infant Formula. Nutrients 2016, 8, 279.
- WHO. How the Marketing of Formula Milk Influences Our Decisions on Infant Feeding; World Health Organization and the United Nations Children’s Fund (UNICEF): Geneva, Switzerland, 2022.
- Doko Jelinić, J.; Nola, I.A.; Andabaka, D. Food processing industry—The salt shock to the consumers. Acta Med. Croat. 2010, 64, 97–103.
- Dwyer, J.T. The Feeding Infants and Toddlers Study (FITS) 2016: Moving Forward. J. Nutr. 2018, 148, 1575S–1580S.
- WHO. WHO Global Sodium Benchmarks for Different Food Categories; World Health Organization: Geneva, Switzerland, 2021.
- Michaelsen, K.F.; Weaver, L.; Branca, F.; Robertson, A.; World Health Organization. Feeding and Nutrition of Infants and Young Children: Guidelines for the WHO European Region, with Emphasis on the Former Soviet Countries; World Health Organization, Regional Office for Europe: Copenhagen, Denmark, 2003.
- Duncan, J.R.; Byard, R.W. Sudden Infant Death Syndrome: An Overview; University of Adelaide Press: Adelaide, Australia, 2018.
- Brown, R.B. Parkinson’s Disease Etiology: Insights and Associations with Phosphate Toxicity. Int. J. Mol. Sci. 2022, 23, 8060.
- Lavezzi, A.M. Altered Development of Mesencephalic Dopaminergic Neurons in SIDS: New Insights into Understanding Sudden Infant Death Pathogenesis. Biomedicines 2021, 9, 1534.
- Meek, J.Y.; Noble, L.; Breastfeeding, S.O. Policy Statement: Breastfeeding and the Use of Human Milk. Pediatrics 2022, 150, e2022057988.
- WHO. Global Strategy for Infant and Young Child Feeding; World Health Organization: Geneva, Switzerland, 2003.
- Guntheroth, W.G.; Lohmann, R.; Spiers, P.S. A seasonal association between SIDS deaths and kindergarten absences. Public Health Rep. 1992, 107, 319–323.
- Dejima, Y.; Fukuda, S.; Ichijoh, Y.; Takasaka, K.; Ohtsuka, R. Cold-Induced Salt Intake in Mice and Catecholamine, Renin and Thermogenesis Mechanisms. Appetite 1996, 26, 203–220.
- Saeki, K.; Obayashi, K.; Tone, N.; Kurumatani, N. Daytime cold exposure and salt intake based on nocturnal urinary sodium excretion: A cross-sectional analysis of the HEIJO-KYO study. Physiol. Behav. 2015, 152, 300–306.
- Radojevic, N.; Konatar, J.; Vukcevic, B.; Jovovic, A.; Begic, S.; Savic, S.; Subramanian, S.V.; Miranovic, V. The socio-economic status of families experiencing the sudden unexpected death of an infant–Is it possibly related to a higher rate of non-natural deaths among them. J. Forensic Leg. Med. 2021, 80, 102168.
- Grimes, C.A.; Campbell, K.J.; Riddell, L.J.; Nowson, C.A. Is socioeconomic status associated with dietary sodium intake in Australian children? A cross-sectional study. BMJ Open 2013, 3, e002106.
- Cheng, Y.L.; Hu, H.; Song, J.; MacGregor, G.A.; He, F.J. Socioeconomic status and dietary sodium intake in children from 2008 to 2019 in the UK. J. Hypertens. 2022, 40, 1499–1503.
More
Information
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.1K
Revisions:
2 times
(View History)
Update Date:
14 Mar 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




