Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Goce Spasovski | -- | 2005 | 2024-02-29 11:18:42 | | | |
| 2 | Mona Zou | Meta information modification | 2005 | 2024-03-01 10:06:37 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Spasovski, G. Etiology of Hyponatremia. Encyclopedia. Available online: https://encyclopedia.pub/entry/55734 (accessed on 07 February 2026).
Spasovski G. Etiology of Hyponatremia. Encyclopedia. Available at: https://encyclopedia.pub/entry/55734. Accessed February 07, 2026.
Spasovski, Goce. "Etiology of Hyponatremia" Encyclopedia, https://encyclopedia.pub/entry/55734 (accessed February 07, 2026).
Spasovski, G. (2024, February 29). Etiology of Hyponatremia. In Encyclopedia. https://encyclopedia.pub/entry/55734
Spasovski, Goce. "Etiology of Hyponatremia." Encyclopedia. Web. 29 February, 2024.
Copy Citation
A perturbation in the water balance rather than any change in salt content is the main cause of hyponatremia, the most frequent electrolyte abnormality, defined as a serum sodium concentration <135 mEq/L. Hyponatremia may be divided between mild (Na > 120 mEq/L) or severe (Na < 120 mEq/L) hyponatremia, and is most frequently observed in elderly ICU hospitalized patients. Based on tonicity, hyponatremia may be hypotonic (a decreased concentration of the solute), isotonic, and hypertonic (falsely low sodium). According to the volume of extracellular fluid (ECF), hyponatremia is further divided among hypovolemic, euvolemic, or hypervolemic hyponatremia. Finally, hyponatremia may develop rapidly as acute (<48 h), usually with severe symptoms, or slowly as chronic hyponatremia, usually being asymptomatic or with mild symptoms. Acute severe hyponatremia presents with severe CNS problems, increased hospitalization rates, and mortality. The treatment with 3% sodium chloride and a 100 mL IV bolus based on severity and persistence of symptoms needs careful monitoring. A non-severe hyponatremia may be treated with oral urea. In asymptomatic mild hyponatremia, an adequate solute intake with an initial fluid restriction of 500 mL/d adjusted according to the serum sodium levels is preferred. Vaptans could be considered in patients with high ADH activity regardless of whether they are euvolemic or hypervolemic. In general, the treatment of hyponatremia should be based on the underlying cause, the duration and degree of hyponatremia, the observed symptoms, and volume status of patient.
hyponatremia
tonicity
volemia
acute
chronic
1. Introduction
Water and salt metabolism are crucial for the vast majority of dysnatremias, including hyponatremia, that arise from a primary imbalance in electrolyte-free water intake and loss, and, less frequently, from changes in the salt content of the body. Thus, a perturbation in the water balance rather than any change in salt content is the main problem.
Hyponatremia is the most frequent electrolyte abnormality and is defined as a serum sodium concentration of less than 135 mEq/L [1]. A disproportion between total body water (TBW) and a sodium content [2] below 120 mEq/L is considered as severe hyponatremia [3]. The highest prevalence may be found among elderly ICU hospitalized patients (20–35%) with an increased mortality risk due to multiple comorbidities and medications [4], and in around 10% of marathon runners [3][5].
The causes of hyponatremia can be divided based on tonicity as hypotonic (a decreased concentration of the solute), isotonic, or hypertonic (falsely low sodium) [6]; and according to the volume of the extracellular fluid (ECF) as hypovolemic, euvolemic, or hypervolemic hyponatremia [7]. In addition, hyponatremia may develop rapidly as acute (<48 h), usually with severe symptoms, or slowly as chronic hyponatremia, usually asymptomatic or with mild symptoms.
2. Hypertonic Hyponatremia
An increased serum tonicity (>290 mOsm/kg) in hypertonic hyponatremia may be caused by hyperglycemia and the use of mannitol. In the case of hyperglycemia, a conversion factor for the serum sodium correction [plasma sodium (PNa) increased by 1.6 mEq/L (1.6 mmol/L) for every 100 mg/dL (5.6 mmol/L) of plasma glucose elevation over 100 mg/dL (5.6 mmol/L) level] should be used [8].
3. Isotonic Hyponatremia
This type of hyponatremia (275–290 mOsm/kg) is also known as pseudo-hyponatremia and is associated with hypertriglyceridemia and hyperproteinemia. It could create a laboratory misinterpretation since plasma consists of 93% of water and 7% of lipids and proteins, while the sodium distribution belongs to the aqueous fraction. The measurement of PNa with an indirect ion-selective electrode (ISE) always requires a dilutional step. The increased levels of plasma triglycerides and/or proteins are associated with an increased volume of the nonaqueous fraction that displaces the water fraction and thus the whole plasma contains less water and sodium per unit volume, respectively. Hence, the PNa+ measurement may cause a dilutional error with a falsely low plasma sodium. To avoid such an error, PNa should be measured by direct ISE, i.e., with a blood gas analyzer. Additionally, an isotonic hyponatremia may be also found when irrigant solutions, like mannitol, sorbitol, or glycine, are used in urology (a transurethral resection of the prostate), gastroenterology (colonoscopy), and some gynecological procedures [9].
4. Hypotonic Hyponatremia
As explained in the physiology introduction, a normal plasma sodium (135–145 mmol/L) and plasma osmolality/tonicity (275–290 mOsm/kg) is maintained by an interplay between thirst and ADH secretion, balancing the water intake with urinary water excretion.
Hypotonic hyponatremia or true hyponatremia (serum osmolality <275 mOsm/kg) is the most common type of hyponatremia and may be found in cases of: (a) a free-water excess caused by either the intake of a large volume exceeding the kidney diluting capacity or in cases of reduced kidney water excretion with an inappropriately high non-osmotically stimulated ADH level. The latter can be caused by a decreased effective arterial blood volume (because of diarrhea, vomiting, heart failure with low cardiac output, or vasodilation in sepsis or cirrhosis), a syndrome of an inappropriate antidiuresis hormone (SIADH) with autonomous ADH secretion (a brain or lung disorder, certain classes of drugs, and other conditions like nausea and pain), and a decreased cortisol release and a lack of the inhibitory effect on ADH secretion [10]; (b) a reduced glomerular filtration rate (GFR) and thus the kidneys’ ultrafiltration capacity (acute/chronic and end-stage kidney disease); (c) a decreased solute daily consumption (<600 mOsm) and, hence, a reduced solute excretion and urine volume (beer potomania or an excessive tea consumption without a sufficient nutritional osmolar intake). The beer potomania is considered as an uncommon etiology of hyponatremia, with variable urinary osmolality < or >100 mOsm/kg if the urine volume is also small. Hence, it should be recommended to measure the urine osmolality via daily urine collection, rather than solely through spot urine. The mechanism of water retention by the kidney in the presence of a broad range of urine osmolality seems to involve a dynamic course of vasopressin secretion during the development of hyponatremia, though the status of the vasopressin release is rarely investigated. Thus, detailed fluid balance studies and sequential observations of changes in urine and plasma osmolality would advance the understanding of its pathophysiology [11].
Based on the Edelman equation, a decreased ratio between the sum of the total body exchangeable sodium (NaE) and potassium (KE) and the total body water (TBW) points out an ensuing hypotonic hyponatremia. In this regard, there are various clinical scenarios leading to hypotonic hyponatremia: (1) in primary polydipsia, there are normal levels of NaE and KE with an increased TBW; (2) cirrhosis and heart failure are represented by an increased NaE and KE with a proportionally higher increase in TBW; (3) a hypovolemic situation with a proportionally greater decrease in NaE + KE compared to the decrease in TBW; and (4) SIADH being represented by a decreased NaE and KE in the presence of an increased TBW.
An important concept based on this equation is thus that hypotonic hyponatremia is always caused by an electrolyte-free water (EFW) excess, i.e., TBW is proportionally higher than the sum of the NaE and KE.
A clinical history and physical examination provide essential information for the diagnosis of hypotonic hyponatremia and should allow the classification of patients with hypovolemic, euvolemic, or hypervolemic hyponatremia. It should be noted in Figure 1 that the assessment of the urinary sodium excretion is important to differentiate the hypo- and hypervolemic forms associated with hyponatremia, while, to diagnose the different causes of euvolemic hyponatremia, measuring the urinary osmolality should be helpful.
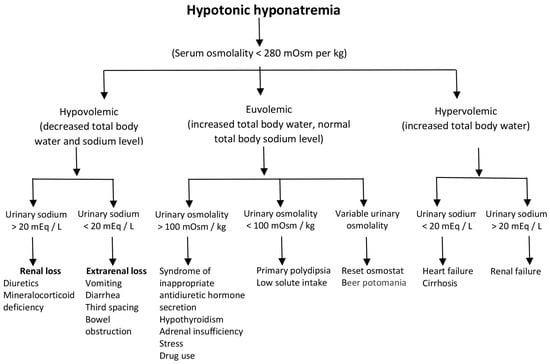
Figure 1. Summary of the clinical approach to hypotonic hyponatremia.
Hyperglycemia and other causes of non-hypotonic hyponatremia must be excluded to confirm hypotonic hyponatremia. Initial laboratory tests and imaging studies combined with a history and physical examination are usually sufficient to arrive at the cause of hyponatremia. However, it is often very difficult to assess the volume status in patients with hyponatremia [12], except in cases with an apparent volume depletion with hemodynamic instability or an apparent volume excess with a significant edema/pleural effusion. Since most hypotonic hyponatremic patients present with appetite loss/nausea, many young physicians assume that the patients are hypovolemic. Nevertheless, most frequently, after ADH suppression, a significantly large hypotonic urine output ensues (which is retained in the intracellular space). Hence, the limitation of an extracellular volume assessment in hyponatremia should be always considered.
An extensive list of causes of hypotonic hyponatremia can be consulted in the review by Adrogue et al. [13].
5. Hypovolemic Hypotonic Hyponatremia
The most frequent category, hypotonic hypovolemic hyponatremia (a greater decrease in TBW relative to the total body sodium and potassium decrease), may be caused by the use of diuretics with volume depletion and a stimulated antidiuretic hormone (ADH) release [6], fluid loss (vomiting, diarrhea, or sweating) [2], the loss of fluids in the third space most frequently associated with hypoalbuminemia, a cerebral salt-wasting (CSW) condition (increased brain natriuretic peptide), a combined glucocorticoid and mineralocorticoid deficiency [6], and an exercise-associated hyponatremia (EAH) [14]. A clinically important, although relatively rare, cause of hyponatremia is treatment with diuretics, known as thiazide-induced hyponatremia (TIH). Besides the increased sodium excretion, there is a complex mechanism of thiazide-induced hyponatremia interfering with the diluting mechanisms of the urine through their action on the cortical-diluting nephron segments (see the physiology introduction), via stimulation of a non-osmotic antidiuretic hormone release, and through their induction of a chronic potassium depletion [15]. Here, the hypokalemia shifts the sodium intracellularly and enhances vasopressin release, worsening hyponatremia. The role of the hypokalemia-induced hyponatremia is important for understanding the adequate treatment of diuretic-induced hyponatremia (see the discussion below on the therapy of hyponatremia). Hypertensive old women that have a low body mass and are hypokalemic are especially susceptible to thiazide-induced hyponatremia, particularly when they have a pre-existing defect in their renal capacity to excrete free water. However, they rarely develop severe hyponatremia and the TIH resolves itself two weeks after drug withdrawal [16].
6. Euvolemic Hyponatremia
It is considered as a stable total body sodium with increased TBW in the presence of excessive (nausea, severe pain), or inappropriate, ADH secretion, known as SIADH [17]. It may be divided into cases with diluted urine (adrenal insufficiency, hypothyroidism, and an excessive intake of water; polydipsia or beer potomania) or concentrated urine—true SIADH [18]. SIADH has been characterized by inappropriate ADH secretion regardless of an increased plasma volume, reducing urine output and leading to hyponatremia [19]. The diagnosis is based on the exclusion of other causes since any unique test or sign is unavailable [20]. It may be caused by any central nervous system (CNS) disorder, ectopic ADH production (small cell carcinoma of the lung), pneumonia or tuberculosis, and in patients on various postoperative anti-pain medications. The treatment of the underlying causes of SIADH [13], together with a reduction in fluid intake and the use of vasopressin 2 receptor inhibitors, may be helpful for the treatment of hyponatremia [21].
Euvolemic hyponatremia may also be caused by various drugs (antidepressants, opioids and antipsychotics [22], thiazides, some anti-cancer drugs, or non-steroidal anti-inflammatory drugs) [23], recreational drugs (ecstasy), excessive fluid use during transurethral resection (TUR) syndrome, colonoscopy or cardiac catheterization intervention [9], and CSW [24].
Ecstasy-associated hyponatremia is complicated and, due to a large water intake, often secondary to ecstasy-mediated hyperthermia with a loss of water and electrolytes, and non-osmotic ADH-secretion mediated by ecstasy and its metabolites. Women are over-represented (85%) in the population with this complication [25].
Hyponatremia associated with disorders in cerebral pathology, such as contusions, intracranial hemorrhages, CNS tumors, meningitis, and encephalitis, is most commonly due to SIADH or CSW, especially in those with a subarachnoid hemorrhage [26]. CSW may be caused by either a decreased sympathetic nervous system function or the secretion of a circulating factor that decreases renal sodium reabsorption. It is characterized by low serum sodium with low plasma osmolality and high urine osmolality (>100 mOsm/L (mmol/L) and frequently >300). Urine sodium is usually >40 mmol/L and serum uric acid is low. CSW may be improved with isotonic saline administration, unlike SIADH, which is not.
7. Hypervolemic Hyponatremia
This type of hyponatremia (a greater increase in TBW compared to the increase in total body sodium) can develop in the presence of acute/chronic renal failure or nephrotic syndrome, or by extrarenal causes such as congestive heart failure, liver cirrhosis, or an excessive fluid intake [27]. In this category, there is a decreased effective circulating volume stimulating a non-osmotically induced antidiuretic hormone (ADH) release, resulting in water retention and generalized edema.
References
- Overgaard-Steensen, C. Initial approach to the hyponatremic patient. Acta Anaesthesiol. Scand. 2011, 55, 139–148.
- Lee, J.J.; Kilonzo, K.; Nistico, A.; Yeates, K. Management of hyponatremia. CMAJ Can. Med. Assoc. J. 2014, 186, E281–E286.
- Henry, D.A. In the Clinic: Hyponatremia. Ann. Intern. Med. 2015, 163, ITC1–ITC19.
- Burst, V. Etiology and Epidemiology of Hyponatremia. Front. Horm. Res. 2019, 52, 24–35.
- Filippatos, T.D.; Liamis, G.; Christopoulou, F.; Elisaf, M.S. Ten common pitfalls in the evaluation of patients with hyponatremia. Eur. J. Intern. Med. 2016, 29, 22–25.
- Dineen, R.; Thompson, C.J.; Sherlock, M. Hyponatraemia—Presentations and management. Clin. Med. 2017, 17, 263–269.
- Hoorn, E.J.; Zietse, R. Diagnosis and Treatment of Hyponatremia: Compilation of the Guidelines. J. Am. Soc. Nephrol. 2017, 28, 1340–1349.
- Ing, T.S.; Ganta, K.; Bhave, G.; Lew, S.Q.; Agaba, E.I.; Argyropoulos, C.; Tzamaloukas, A.H. The corrected serum sodium concentration in hyperglycemic crises: Computation and clinical applications. Front. Med. 2020, 7, 477.
- Darwish, O.M.; Lutnick, E.; Dalimov, Z.; Waisanen, K.M.; Wang, D.; Houjaij, A.; Jung, I.; Nader, N.D. Neuraxial vs. General Anesthesia: 30-Day Mortality Outcomes Following Transurethral Resection of Prostate. Urology 2021, 157, 274–279.
- Peri, A.; Grohé, C.; Berardi, R.; Runkle, I. SIADH: Differential diagnosis and clinical management. Endocrine 2017, 55, 311–319.
- Joshi, R.; Chou, S.Y. Beer Potomania: A View on the Dynamic Process of Developing Hyponatremia. Cureus 2018, 10, e3024.
- Hoorn, E.J.; Halperin, M.L.; Zietse, R. Diagnostic approach to a patient with hyponatraemia: Traditional versus physiology-based options. Q. J. Med. 2005, 98, 529–540.
- Adrogué, H.J.; Tucker, B.M.; Madias, N.E. Diagnosis and Management of Hyponatremia: A Review. JAMA 2022, 328, 280–291.
- Bennett, B.L.; Hew-Butler, T.; Hoffman, M.D.; Rogers, I.R.; Rosner, M.H. Wilderness Medical Society practice guidelines for treatment of exercise-associated hyponatremia. Wilderness Environ. Med. 2013, 24, 228–240.
- Spital, A. Diuretic-Induced Hyponatremia. Am. J. Nephrol. 1999, 19, 447–452.
- Kim, G.H.J. Pathophysiology of Drug-Induced Hyponatremia. Clin. Med. 2022, 11, 5810.
- Verbalis, J.G.; Goldsmith, S.R.; Greenberg, A.; Korzelius, C.; Schrier, R.W.; Sterns, R.H.; Thompson, C.J. Diagnosis, evaluation, and treatment of hyponatremia: Expert panel recommendations. Am. J. Med. 2013, 126 (Suppl. S1), S1–S42.
- Reddy, P. Clinical Approach to Euvolemic Hyponatremia. Cureus 2023, 15, e35574.
- Martin, J.; Burnier, M.; Lu, H. Approach to the syndrome of inappropriate antidiuretic hormone secretion (SIADH). Rev. Med. Suisse 2018, 14, 2116–2120.
- De Las Peñas, R.; Ponce, S.; Henao, F.; Camps Herrero, C.; Carcereny, E.; Escobar Álvarez, Y.; Rodríguez, C.A.; Virizuela, J.A.; López López, R. R SIADH-related hyponatremia in hospital day care units: Clinical experience and management with tolvaptan. Support. Care Cancer. 2016, 24, 499–507.
- Shepshelovich, D.; Schechter, A.; Calvarysky, B.; Diker-Cohen, T.; Rozen-Zvi, B.; Gafter-Gvili, A. Medication-induced SIADH: Distribution and characterization according to medication class. Br. J. Clin. Pharmacol. 2017, 83, 1801–1807.
- Sahoo, S.; Grover, S. Hyponatremia and psychotropics. J. Geriatr. Ment. Health. 2016, 3, 108–122.
- Braun, M.M.; Barstow, C.H.; Pyzocha, N.J. Diagnosis and management of sodium disorders: Hyponatremia and hypernatremia. Am. Fam. Physician 2015, 91, 299–307.
- Verbalis, J.G. The Curious Story of Cerebral Salt Wasting: Fact or Fiction? Clin. J. Am. Soc. Nephrol. 2020, 15, 1666–1668.
- Elkattawy, S.; Mowafy, A.; Younes, I.; Tucktuck, M.; Agresti, J. Methylenedioxymethamphetamine (MDMA)-Induced Hyponatremia: Case Report and Literature Review. Cureus 2021, 13, e15223.
- Sterns, R.H.; Rondon-Berrios, H. Cerebral Salt Wasting Is a Real Cause of Hyponatremia: CON. Kidney360 2023, 4, e441–e444.
- Spasovski, G.; Vanholder, R.; Allolio, B.; Annane, D.; Ball, S.; Bichet, D.; Decaux, G.; Fenske, W.; Hoorn, E.J.; Ichai, C.; et al. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Nephrol. Dial. Transplant. 2014, 170, G1–G47.
More
Information
Subjects:
Urology & Nephrology
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
729
Revisions:
2 times
(View History)
Update Date:
01 Mar 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




