Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Miguel A Montoro | -- | 5762 | 2024-01-22 08:25:15 | | | |
| 2 | Catherine Yang | -36 word(s) | 5726 | 2024-01-22 08:34:41 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Utrilla Fornals, A.; Costas-Batlle, C.; Medlin, S.; Menjón-Lajusticia, E.; Cisneros-González, J.; Saura-Carmona, P.; Montoro-Huguet, M.A. Short Bowel Syndrome (SBS). Encyclopedia. Available online: https://encyclopedia.pub/entry/54169 (accessed on 07 February 2026).
Utrilla Fornals A, Costas-Batlle C, Medlin S, Menjón-Lajusticia E, Cisneros-González J, Saura-Carmona P, et al. Short Bowel Syndrome (SBS). Encyclopedia. Available at: https://encyclopedia.pub/entry/54169. Accessed February 07, 2026.
Utrilla Fornals, Alejandra, Cristian Costas-Batlle, Sophie Medlin, Elisa Menjón-Lajusticia, Julia Cisneros-González, Patricia Saura-Carmona, Miguel A. Montoro-Huguet. "Short Bowel Syndrome (SBS)" Encyclopedia, https://encyclopedia.pub/entry/54169 (accessed February 07, 2026).
Utrilla Fornals, A., Costas-Batlle, C., Medlin, S., Menjón-Lajusticia, E., Cisneros-González, J., Saura-Carmona, P., & Montoro-Huguet, M.A. (2024, January 22). Short Bowel Syndrome (SBS). In Encyclopedia. https://encyclopedia.pub/entry/54169
Utrilla Fornals, Alejandra, et al. "Short Bowel Syndrome (SBS)." Encyclopedia. Web. 22 January, 2024.
Copy Citation
Short bowel syndrome (SBS) is a malabsorptive condition that is most often caused by a massive resection of the small intestine. Its prevalence is 3–4 per million and occurs in about 15% of adult patients undergoing an intestinal resection, either massive (3/4) or from multiple sequential resections (1/4). SBS and intestinal failure (IF) are not necessarily synonymous. Intestinal failure describes the state when an individual’s gastrointestinal function is inadequate to maintain his or her nutrient and hydration status without intravenous or enteral supplementation.
malnutrition
metabolism
micronutrients
nutritional deficiencies
dietitian
1. Clinical Presentation
1.1. Global Outlook
The clinical presentation of SBS comprises a range of intestinal and extraintestinal manifestations (see related complications). It may be categorized into three symptom patterns: First, those that depend on the impairment of absorption and/or stimulation of water and electrolyte secretion. Diarrhea, dehydration, and undernutrition are the most prominent symptoms in this group, and their severity mainly depends on the factors listed above (Figure 1) and especially on the location and extent of the removed intestinal segment. Thus, some functions of the ileum (e.g., bile salt and vitamin B12 absorption) are specific to this anatomical segment and cannot be supplied by the jejunum [1][2][3][4][5]. In addition, the ileum typically reabsorbs a large portion of the fluid secreted by the jejunum. Therefore, patients who lose a significant portion of the ileum have a limited capacity to absorb fluids and electrolytes and have difficulties tolerating high-osmolarity liquids [6]. On the other hand, losing the ileocecal valve increases the risk of SIBO and enteropathy, resulting in multiple intestinal symptoms that depend on dysbiosis, like bloating, diarrhea, and abdominal discomfort [7][8] (Figure 2).
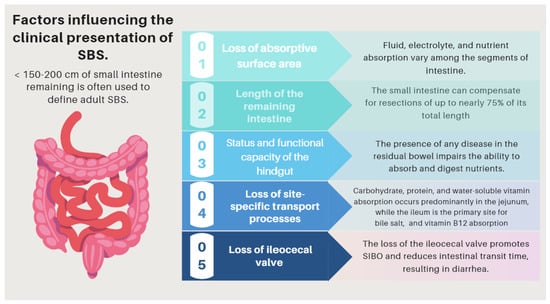
Figure 1. Factors influencing the pathophysiology of SBS. SBS: short bowel syndrome.
Second, those reflecting specific metabolic disturbances or inherent to the specific nutritional support these patients receive and manifested by extraintestinal symptoms and signs (e.g., refeeding syndrome, D-lactic acidosis, IF-associated liver dysfunction, biliary gallstones, or nephrolithiasis [10][11][12][13][14][15][16][17] (Table 1).
Third, those dependent on the insertion of central catheters (e.g., sepsis or central line thrombosis) which are necessary for PN support (Table 1).
Table 1. A list of nutritional and metabolic consequences that are related to the pathophysiology of SBS.
| Complications Related to SBS | Pathogenesis |
|---|---|
| (I) Complications related to SBS pathophysiology and its underlying pathology | The pattern of nutrient absorption native to the parts of the gastrointestinal tract is shown in Figure 1. |
| Peptic ulcer | Hypergastrinemia resulting from a failure of enterogastrone release (e.g., VIP, GIP, neurotensin, peptide YY, and GLP-1). Treatment with antisecretory drugs could also aggravate SIBO due to hipoclorhydria [16]. |
| Electrolyte disturbances: hypocalcemia, hypokalemia, and hypomagnesemia |
Occur especially when large-volume diarrhea is present. (e.g., associated with an end jejunostomy). |
| D-lactic acidosis (D-LA) | The SBS microbiota, since it is rich in Lactobacillus, leads to the accumulation of fecal lactate. Lactate does not accumulate in healthy human feces because it is absorbed by intestinal cells, but in some SBS patients, the high amount of lactate found in feces indicates that production exceeds absorption capacities by the host. Excess lactate released into the colon is fermented by bacteria and converted into D-lactate, which has neuro-toxic effects [10][11][12]. |
| Cholelithiasis | In the presence of an ileum resection, it breaks the enterohepatic circle of bile salts, causing a reduced biliary excretion and a marked decrease of the bile salt pool in the duodenal lumen. Consequently, cholesterol is oversaturated, favoring the formation of biliary stones [13][14]. |
| Nephrolithiasis | As a result of steatorrhea, increased free fatty acids are available to bind to calcium, resulting in an increased concentration of non-bound oxalate, which is easily absorbed across the colonic mucosa, where it is moving to the kidneys. Nephrolithiasis is more common among patients with an intact colon. The risk of nephrolithiasis is enhanced by volume depletion, metabolic acidosis, and hypomagnesemia, resulting in decreased renal perfusion, urine output, pH, and citrate excretion [15][16]. |
| Metabolic osteopathy | Metabolic changes that occur in SBS result in the depletion of calcium, magnesium, and vitamin D, which results in the demineralization of bone. The release of pro-inflammatory cytokines, steroid use, PN, chronic metabolic acidosis, and renal insufficiency may contribute to the development of metabolic osteopathy [17]. |
| (II) Complications related with nutritional therapy | Pathogenesis |
| Thrombus-associated venous occlusion | Central venous catheter (CVC)-related thrombosis (CRT) is a severe complication of parenteral nutrition (HPN), which increases its associated morbidity (due to pulmonary embolism) and mortality rates of this population [18][19]. |
| Catheter-associated central line bloodstream infections | Primary and intravascular catheter-associated bloodstream infections represent an important clinical entity in the intensive care unit (ICU) and has a poor effect on outcomes. Over-abundant levels of Proteobacteria have been found in the feces of patients with SBS presenting with Ca-CLBI [20][21][22][23]. |
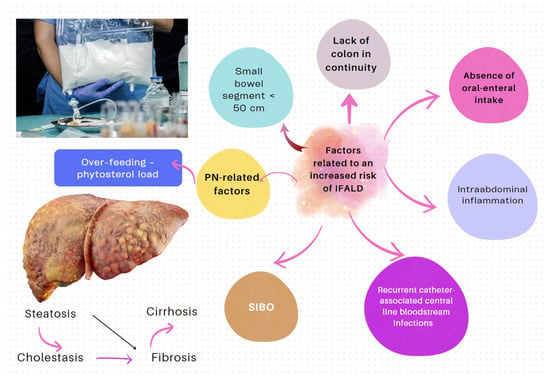
| IF-associated liver disease (IFALD) | IFALD is a possible complication in patients with IF who need intravenous support for survival due to severe intestinal dysfunction. An elevation of aminotransferases or cholestasis enzymes in this setting should raise clinical suspicion of this entity, which may progress from hepatic steatosis to cirrhosis. Some factors that increase the risk of this condition are shown in Figure 6. Liver cholestasis can be a life-threatening complication during HPN and may lead to a combined liver–intestinal transplantation (Figure 6) [22][24][25][26]. |
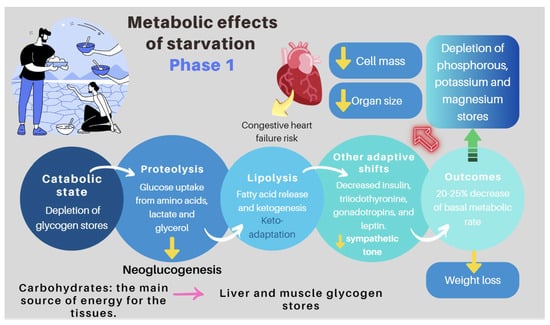
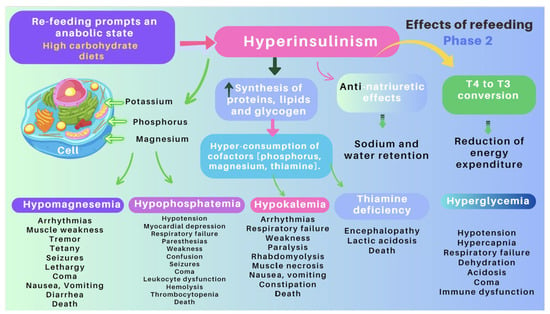
| Re-feeding syndrome (RFS) | The switch from a catabolic state to an anabolic state in malnourished patients undergoing refeeding (orally, enterally, or parenteral) may be the cause of all these clinical manifestations, which, in some cases, can lead to death. RS include a complex and extensive list of changes, such as hypophosphatemia, hypomagnesemia, hypokalemia, hyponatremia, hypocalcemia, hyperglycemia, and vitamin deficiency (especially thiamine deficiency), all of which are accompanied by clinical signs and symptoms, reflecting organ dysfunction (cardiovascular, renal, respiratory, and neurological manifestations, among others). Figure 7 and Figure 8 summarize the relationship between the pathophysiology of RS and its clinical presentation [27][28][29][30][31][32][33][34]. |
1.2. D-lactic Acidosis
D-lactic acidosis is an unusual complication that mainly occurs in patients with malabsorption due to SBS or after a bariatric surgery. Colonic bacteria may degrade a surplus of fermentable carbohydrates to form D (−) lactate, which is absorbed but not easily metabolized and leads to severe encephalopathy of metabolic origin. D-lactic acidosis only occurs in patients with SBS and colon continuity and requires the following conditions: (1) colonic bacterial flora of a type that produces d-lactic acid; (2) ingestion of significant amounts of carbohydrates; (3) diminished colonic motility, allowing time for nutrients in the colon to undergo bacterial fermentation; and (4) impaired D-lactate metabolism [10][11][12]. Clinical manifestations of this condition include episodes of encephalopathy and metabolic acidosis. Its diagnosis should be considered in the presence of metabolic acidosis and neurological symptoms that cannot be attributed to other causes. Serum levels of more than 3 mmol/L of D-lactate are required to verify the diagnosis. Its treatments include the correction of metabolic acidosis by intravenous bicarbonate, restriction of carbohydrates or fasting, and antibiotics to eliminate intestinal bacteria that produce D-lactic acid [10][11][12].
1.3. Refeeding Syndrome (RS)
RS is a rare, but severe, and potentially fatal complication related to the re-feeding of individuals who have fasted or consumed very few calories over a long period of time (83–87). Its clinical features comprise fluid-balance abnormalities, abnormal glucose metabolism, hypophosphatemia, hypomagnesemia, and hypokalemia. In addition, thiamine deficiencies can occur. The switch from a catabolic state to an anabolic state may be the cause of the clinical manifestations of RFS and justifies all the clinical features of this often severe and devastating clinical condition (Figure 3 and Figure 4) [32][33].
2. Basic Principles of Nutritional Management
The treatment of patients with IF is complex and requires a comprehensive approach that frequently necessitates the long-term, if not life-long, use of PN. The appropriate management of this disorder requires an interdisciplinary approach to facilitate intestinal rehabilitation in combination with the treatment of the sequelae of IF [16]. Recently, guidelines and recommendations have been developed by the American Gastroenterological Association (AGA) [35], ASPEN [29][34], and ESPEN [36]. Although an extensive review is beyond the scope of this manuscript, it is essential to highlight some basic concepts:
-
Nutritional interventions to treat SBS include enteral and PN, intestinal rehabilitation techniques to increase the absorptive ability of the residual bowel, and surgical reconstruction designed to enhance the surface area for absorption [37][38][39]. Therefore, managing these patients requires a comprehensive and interdisciplinary approach in centers with proven experience in treating such challenging scenarios [38][39][40][41][42]. This issue is essential, as has been demonstrated by Geransar P et al., who reported a low level of awareness of chronic IF among non-specialist healthcare professionals [40]. Figure 5 highlights the components of a multidisciplinary team caring for these patients in a highly specialized center [38][41], and Figure 6 outlines the fundamental steps to be followed in the assessment and treatment of these patients [42].
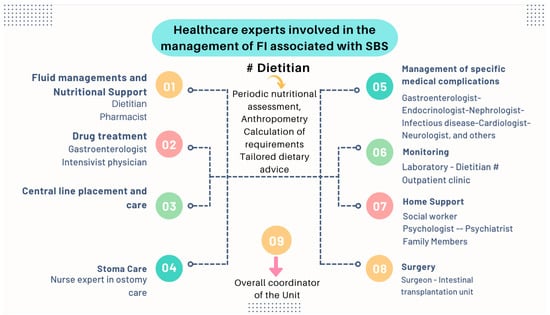
Figure 5. The management of patients with chronic IF requires an interdisciplinary approach through management by intestinal rehabilitation centers as the standard of care. This figure shows the team members involved in the overall care of these patients [38].
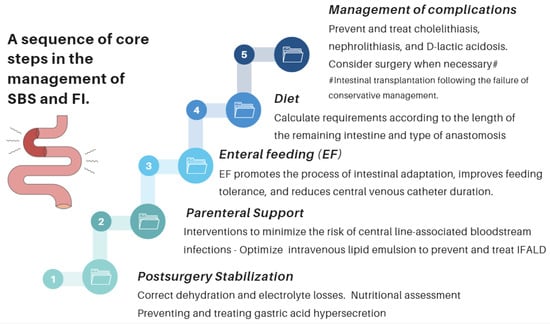
Figure 6. Essential strategic issues for the management of SBS and IF.
-
The role of an experienced dietitian is also fundamental in the initial assessment and monitoring of the nutritional status of patients with SBS. Concerning this point, the dietitian should obtain information regarding multiple details related to the type of surgery performed, the patient’s baseline post-operative conditions (renal function, water–electrolyte, and acid–base balance), their degree of malnutrition, and the type of nutritional support received (enteral or parenteral), including access routes, as well as their associated complications (Figure 6 and Figure 7).
-
Almost all patients with SBS need PN during the early period after a resection. PN should be initiated and adjusted to meet the patient’s fluid, electrolyte, energy, protein, and micronutrient needs. The literature provides excellent reviews of PN performance in this setting [43][44][45][46]. Although few patients with severe SBS can discontinue PN before hospital discharge, more than 50% of adults will be able to wean completely from PN within five years of their diagnosis. PN volume can be decreased when the patient begins to tolerate oral nutrition. This is possible if the volume or flow of feces from the rectum or through the ostomy is adequately reduced and the patient begins to gain weight. Enteral nutrition (EN) provides clear benefits, prevents villous atrophy, helps preserve the intestinal epithelial barrier, enhances the local immunity needed to avoid SIBO, and promotes the mechanisms of bowel adaptation, enhancing weaning from parenteral nutrition. The introduction of EN should always be prudent and judicious [45][46]. One approach is to start EN by providing 5% of the total calories and increasing this ratio every 3–7 days and assess tolerance. Patients who require long-term PN cannot be kept in hospital indefinitely, and thus transition to home PN when they are clinically stable. To maximize patient mobility and convenience at home, PN infusion time is minimized, and the solution is infused overnight. PN infusion time can typically be reduced (cycled) to 10–15 h, depending on patient tolerance [41][42]. Notably, the SBS patient receiving home PN is still at risk of micronutrient deficiencies, as well as liver and bone complications, and requires regular monitoring and supplementation with PN (Table 2).
-
Many patients with less severe forms of SBS may be fed orally early. The dietary and nutritional management of these patients necessitate to understand the physiology and to consider the individual anatomy and adaptation phase. During the hypersecretory phase, fluid losses are usually the largest. Dehydration and saline depletion can occur during any phase, especially in patients without a colon, and particularly in case of an end jejunostomy [43].
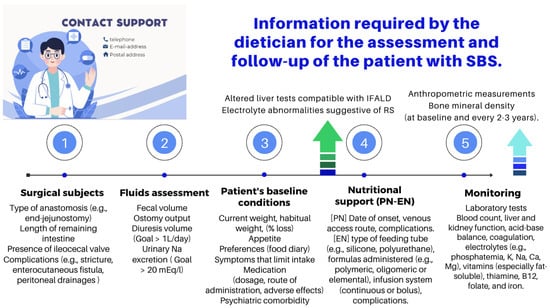
Table 2. Nutritional recommendations for the “end jejunostomy” (ASPEN).
| Requirement | Comment | |
|---|---|---|
| Energy | 35–45 kcal/kg/day. In some cases, increasing the energy intake up to 60 kcal/kg/day may be necessary. |
Patients with SBS develop compensatory hyperphagia, and it is advisable to take 5–6 meals spaced out during the day. |
| Carbohydrates | 20–40% of the daily energy target. | In the absence of a colon, it is not possible to rescue energy inherent in the production of short-chain fatty acids from the bacterial fermentation of sugars. |
| Protein | 1.5–2.0 g/kg/day or 20–30% of the daily energy target. | It is preferable to choose lean proteins of high biological value. |
| Fat | 40–60% of the daily energy target. | Choose essential fatty acids as the main component of fat intake. Consider MCTs in cases of malabsorption. |
| Fluids | Reduce oral hypotonic fluids to 500 mL/day #. Separating solids and liquids (i.e., do not drink anything for half an hour before or after a meal). |
Add sodium chloride to any liquid feeds to make the sodium concentration near 100 mmol/L while keeping osmolality near 300 mOsmol/kg *. |
| Oxalate | The restriction is not necessary. | Calcium oxalate stones only occur in patients with a preserved colon. |
* Administer glucose/saline solution in small sips (sodium concentration of at least 90 mmol/L). Most stomal/fistula leakages (except from the colon) have a sodium concentration of least 90 mmol/L. In cases of severe dehydration, administration of intravenous saline while the patient does not take anything by mouth for 24–48 h will stop thirst and therefore the desire to drink. # Osmolarity of drinks: hypertonic > 300 mOsmol kg−1; isotonic: 275–300 mOsmol kg−1; and hypotonic: <275 mOsmol kg−1.
3. Recommendations of Scientific Societies
ASPEN has issued specific dietary advice and recommendations for the above phenotypes (ASPEN, www.nutritioncare.org). The researchers outline some key messages about these recommendations:
-
Type 1: end jejunostomy. This is the most unfavorable phenotype, as malabsorption is more severe, and it presents with a high ostomy output. Patients without a colon and <100 cm of the jejunum have a higher risk of requiring long-term PN. Indeed, dehydration, hydroelectolytic abnormalities, acidosis, and renal failure are more likely in these patients [47]. Sodium absorption in the jejunum is dependent on water fluxes and is coupled to the absorption of glucose. For this reason, hydration with hypotonic solutions (e.g., water, tea, or coffee) should be discouraged, as they only exacerbate fluid losses through the stoma. Hypertonic drinks (e.g., fruit juices) should also not be recommended as they cause osmotic diarrhea. Some measures that may be useful for these patients are lowering the intake of sugars, decreasing the size of intakes, and take the oral rehydration solutions (ORSs) whose composition is best suited to promote the entry of sodium and water into the enterocytes [48][49]. Regarding calorie and macronutrient requirements, the recommendations are as follow (Table 2):
-
Type 2: jejunocolic. It retains a portion of the jejunum anastomosed to a portion of the colon. In these patients, the clinical picture is dominated by diarrhea due to severe malabsorption, vitamin–mineral deficiencies, and subsequent malnutrition. Patients with jejunocolic anastomosis and <50 cm of the jejunum also have a higher risk of requiring long-term PN. The nutritional recommendations for those who recover intestinal autonomy are as follows (Table 3):
-
Type 3: jejunoileocolic. These patients retain their entire colon and ileocecal valve along with a portion of their terminal ileum and jejunum. This is indeed the most advantageous phenotype, and these patients often do not require additional nutritional support because the ileum has a greater ability to adapt. This subgroup does not usually develop malnutrition, electrolyte disorders, or dehydration [47].
Table 3. Nutritional recommendations for the jejunocolic anastomosis (ASPEN).
| Requirement | Comment | |
|---|---|---|
| Energy | 35–45 kcal/kg/day. In some cases, increasing the energy intake up to 60 kcal/kg/day may be necessary. |
Patients with SBS develop compensatory hyperphagia, and it is advisable to take 5–6 meals spaced out during the day. |
| Carbohydrates | 50–60% of the daily energy target. | The colon provides energy (up to 1000 kcal/day) in SBS by releasing the SCFAs resulting from the fermentation of carbohydrates. In addition, it provides nutrition to the colonocytes. |
| Protein | 1.5–2.0 g/kg/day or 20–30% of the daily energy target. | It is preferable to choose lean proteins of high biological value. |
| Fluids | Isotonic/hypotonic #. | In SBS, the colon plays a vital role in fluid and electrolyte reabsorption, given the additional fluid that enters the colon with a capacity to absorb up to 6 L daily. |
| Fat | 20–30% of daily energy target. | In jejunum–colon patients, unabsorbed long-chain fatty acids in the colon are likely to reduce the transit time and reduce their water and sodium absorption, making their diarrhea worsen. Consider MCTs only in the case of severe malabsorption. MCT does not contain essential fatty acids. |
| Oxalate | The diet should be low in oxalate. | Nephrolithiasis only occurs in patients with a preserved large bowel. |
# Osmolarity of drinks: hypertonic > 300 mOsmol kg−1; isotonic: 275–300 mOsmol kg−1; and hypotonic: <275 mOsmol kg−1.
4. Common Recommendations for All Three Phenotypes
The intestinal mucosa usually absorbs lactose unless it is affected by lesions (e.g., Crohn’s disease), leading to villous atrophy and a secondary lactase deficiency. Therefore, lactose restriction is not justified, as it is a natural protein, calcium, and vitamin D source. With respect to the amount of fiber, 10–15 g/day is recommended (depending on individual tolerance). Patients with a fecal fluid excretion level >3 L/24 h may require 5–10 g of soluble fiber per day.
5. Vitamin and Mineral Replacement
As water-soluble vitamins are absorbed in the proximal small bowel, deficiencies in SBS patients are uncommon, except in very extensive resections. Nevertheless, fat-soluble vitamin deficits are relatively frequent, and large doses may be required to maintain normal serum levels [9][47]. Consequently, in all patients with SBS, serum vitamin and trace element concentrations should be measured at baseline and monitored on a regular basis (Table 4) [9][47][50][51][52][53][54][55][56].
| Type of Micronutrient and Average Nutritional Intake Ranges | Clinical Signs Reflecting a Deficiency | Measurement | Typical Supplementation in SBS * |
|---|---|---|---|
| Water-soluble vitamins | Doses (all values per day) | ||
| Vitamin B1—thiamine (DRI: 1.1–1.2 mg/day) |
Mental changes (apathy, decrease in short-term memory, confusion, and irritability), cognitive deficits, congestive heart failure, and metabolic lactic acidosis | Whole-blood ThDP or RBCs | Oral: 1–2 capsules daily (multivitamin: B1, B2, B3 B5, B6, and B7) |
| HPN and long-term PN: 2.5 mg/day | |||
| Vitamin B2—riboflavin (DRI: 1.3 mg/day—males. 1.1 mg/day—females) |
Seborrheic dermatitis of the face, trunk, and scrotum, oral buccal lesions, ocular manifestations, marrow aplasia, and normochromic, normocytic anemia | Glutathione reductase activity in red blood cells | Oral: 1–2 capsules daily (multivitamin: B1, B2, B3 B5, B6, and B7) |
| HPN and long-term PN: 3.6 mg/day | |||
| Vitamin B3—niacin (DRI: 16 mg/day—adolescents and adult males > 14 years. 14 mg/day—females > 14 years) |
Dementia, dermatitis, and diarrhea | Blood or tissue NAD | Oral: 1–2 capsules daily (multivitamin: B1, B2, B3 B5, B6, and B7) |
| HPN and long-term PN: 40 mg/day | |||
| Vitamin B5—pantothenic acid (DRI: 5 mg/day for 14 to over 70 years) |
Fall in the diastolic and lability of systolic blood pressure, with postural hypotension, vertigo, and tachycardia. Gastrointestinal and neurological symptoms | Blood pantothenic acid | Oral: 1–2 capsules daily (multivitamin: B1, B2, B3 B5, B6, and B7) |
| HPN and long-term PN: 10 mg/day | |||
| Vitamin B6—pyridoxine (DRI: 1.3–1.7 mg/day for 14 to over 70 years) |
Microcytic anemia, seborrheic dermatitis with cheilosis and glossitis, angular stomatitis, epileptiform convulsions, confusion, and/or depression | PLP levels. Red cell PLP in serious patients or in the presence of inflammation | Oral: 1–2 capsules daily (multivitamin: B1, B2, B3 B5, B6, and B7) |
| HPN and long-term PN: 4 mg/day | |||
| Vitamin B7—biotin (DRI: 40 μg/day) |
Ataxia, dermatitis, and alopecia | Direct measure of urine and blood biotin that must be completed with the determination of biotin activity | Oral: 1–2 capsules daily (multivitamin: B1, B2, B3 B5, B6, and B7) |
| HPN and long-term PN: 60 μg/day | |||
| Vitamin B9—folic acid (DRI: 330 μg/day DFE) |
Glossitis, megaloblastic anemia, pancytopenia, oral ulcers, angular stomatitis, and neuropsychiatric manifestations | Folate level in the plasma or serum—short-term status. In RBCs—long-term status | Oral: 1 mg daily |
| HPN and long-term PN: 400 μg/day | |||
| Vitamin B12—cobalamin (DRI: 2.4 μg/day) |
Hematological, neurological, neuropsychiatric, and cognitive symptoms | Combination of at least two bio- markers (e.g., holo-TC and MMA), with serum cobalamin as a replacement for holo-TC when the measurement of this latter is unavailable | Oral: 1–2 capsules daily (multivitamin: B1, B2, B3 B5, B6, and B7) |
| HPN and long-term PN: 5 μg/day | |||
| Vitamin C—ascorbic acid (DRI: 90–100 mg/day) |
Lassitude; shortness of breath; anemia; poor wound healing; myalgia and bone pain; loose teeth; spongy and purplish gums that are prone to bleeding; bulging eyes; scaly, dry, and brownish skin; dry hair that breaks; edema; petechiae; and easy bruising | Total plasma vitamin C (sum of AA and DHAA) or AA. | Oral: 200–500 mg daily ǂ |
| HPN and long-term PN: 100–200 mg/day | |||
| Fat-soluble vitamins | Doses (all values per day) | ||
| Vitamin A (DRI: 700–900 µg/day) |
Night blindness, Bitot spots, foamy appearance on the conjunctiva, xerophthalmia, increased susceptibility to infections, and impairment of the intestinal immune and barrier function | Serum retinol | Oral: 5000–50,000 IU daily # |
| HPN and long-term PN: 800–1100 µg/day | |||
| Vitamin D (DRI: 15–20 µg/day) |
Osteomalacia and nutritional rickets; increased susceptibility to infections | Serum 25-hydroxyvitamin D (25(OH)D) |
<12 ng/mL: oral: 50,000 IU# once weekly (or calcitriol 0.25–2 mg daily), followed by maintenance:
|
| HPN and long-term PN: 200 IU/5 µg/day | |||
| Vitamin E (DRI: 15 mg/day) |
Neurological symptoms (balance and coordination disorders and peripheral neuropathy) and muscle weakness | Serum alpha-tocopherol | Oral: 400 IU up to 3 times daily |
| HPN and long-term PN: 9–10 mg/day | |||
| Vitamin K (DRI: 90–120 µg/day) |
Prolongation of prothrombin time with impaired clotting or bleeding, poor bone development, osteoporosis, and increased cardiovascular disease | Combination of biomarkers and dietary intake | Oral: 2.5 to 10 mg twice weekly to daily, or 10-mg single dose #; can be repeated 48–72 h later |
| HPN & long-term PN: 150 µg/day, usually provided by lipid emulsions | |||
| Trace mineral | Doses (all values per day) | ||
| Iron (DRI: 8 mg/day. 18 mg/day for female 19–50 years old) |
Microcytic anemia | Serum ferritin, sideremia, and transferrin saturation (%) | Oral: 100–200 mg once daily or every other day # ǂ |
| HPN and long-term PN: 1.1 mg/day | |||
| Copper (DRI: 1.1–2 mg/day) |
Microcytic anemia, neutropenia, osteoporosis, hair depigmentation, cardiac arrhythmias, delayed wound healing, and myeloneuropathy | Serum copper | Oral: 2 mg of elemental copper daily ǂ Higher doses may be needed |
| HPN and long-term PN: 0.3–0.5 mg/day- | |||
| Chromium (DRI: 20–35 µg/day) |
Hyperglycemia, insulin resistance, elevated plasma fatty acids, weight loss, and peripheral neuropathy | Serum chromium | Oral: 100–200 mg up to 3 times daily |
| HPN and long-term PN: 10–15 µg/day | |||
| Zinc (DRI: 8–11 mg/day) |
Impairment of immune defense, reduced growth rate, alopecia, skin rash of the face, groins, hands, and feet, delayed sexual development and bone maturation, impaired wound healing, diarrhea, and blunting of taste and smell | Serum zinc | Oral: 50 mg elemental zinc (once or twice daily) Dietary sources such as oysters and mussels can also be considered |
| HPN and long-term PN: 3–5 mg/day | |||
| Selenium (DRI: 55 µg/day) |
Cardiomyopathy, skeletal muscle myopathy, and skin and nail impact | Serum selenium | Oral: 100–200 mg daily |
| HPN and long-term PN: 60–100 µg/day |
* The doses shown in the table allow for the daily requirements to be covered. A dose adjustment would be necessary for severe deficiencies of any micronutrient that has been referred to (see Refs. [54][55][56]). # IM: administration also available; ǂ IV: administration also available HPN: home parenteral nutrition; IM: intramuscular; IV: intravenous; DRI: dietary reference intake; AI: adequate intake; DFE: dietary folate equivalent; ThDP: thiamine diphosphate; RBCs: red blood cells; NAD: nicotinamide adenine dinucleotide; PLP: plasma pyridoxal phosphate; holo-TC: holo-transcobalamin; MMA: methylmalonic acid; AA: ascorbic acid; and DHAA: dehydroascorbic acid.
6. Pharmacological Treatment
Regarding the most prescribed pharmacological treatments for SBS, anti-secretory medications (e.g., proton-pump inhibitors or histamine H2 receptor antagonists) can reduce gastric acid secretion after a massive bowel resection in order to decrease fluid and electrolyte losses. They are generally used for periods of up to 6 months [57][58]. Antimotility medications, such as loperamide (2–8 mg, 30–60 min before meals and bedtime) and occasionally codeine phosphate (30–60 mg), are usually used to enlarge the intestinal transit time and therefore prevent the loss of large volumes of fecal fluid. Treatment should be initiated with a single first-line medication at the low end of its dosing range. Dosage and/or dosing frequency can then be slowly escalated (every 3–5 days) to achieve maximal effects while minimizing adverse events. Codeine phosphate is a potent anti-diarrheal agent, but it should be used cautiously due to its CNS-acting effects and addictive properties [47][59].
Antimicrobial agents, such as rifaximin (550 mg, three times a day), metronidazole (250–500 mg, three times a day), or doxycycline (100 mg, twice a day), administered periodically may be helpful in neutralizing the effects of SIBO, a condition associated with various gastrointestinal symptoms, as well as nutrient deficiencies, and weight loss [60][61]. It has recently been shown that the bioavailability of oral antibiotics was higher than expected in patients who have suffered a loss of their anatomical surface area for absorption [62].
Other emerging therapies may include probiotics, diet manipulation, and prokinetic agents. Bile acid sequestrants (e.g., cholestyramine or colesevelam) can be used in patients with bile acid diarrhea due to limited ileal disease or resection. However, they can worsen steatorrhea in SBS, and should be discouraged in patients with ileal resections >100 cm [59][63][64][65][66][67][68]. The role of the pancreatic enzyme replacement treatment in this scenario has not been sufficiently elucidated [58][69]. Ursodeoxycholic acid (UDCA) treatment decreases the hepatic synthesis of triglycerides and cholesterol. Recent studies have reported that UDCA (20 mg/kg/day) could prevent the onset of IFALD by decreasing hepatic lipogenesis [70].
Somatostatin and octreotide reduce salivary, gastric, and pancreaticobiliary secretions, slow small bowel transit, and may delay gastric emptying; for these reasons, they reduce the intestinal output from a jejunostomy in both net ‘secretors’ and ‘absorbers’. Studies involving adults have shown octreotide to reduce ileostomy diarrhea and large- volume jejunostomy outputs (2 L/d) [71][72]. Some problems associated with the long-term use of octreotide are: (1) A lower number of amino acids for splanchnic protein synthesis. This may interfere with the physiological process of adaptation to an intestinal resection [71][72]; (2) a reduction in pancreaticobiliary secretion, worsening fat absorption [73][74][75]; however, it is usually unchanged [76][77][78]; (3) a higher risk of cholelithiasis [71][72][79][80][81]. The effectiveness of other long-acting somatostatin analogues, such as lanreotide, has not been sufficiently tested in this setting [82].
Teduglutide reduces gastric emptying and secretion and may promote the growth of the mucosa [83][84][85][86][87][88][89][90]. Studies over the last five years have shown that teduglutide, in addition to reducing the volume and calories administered through parenteral support, also reduces infusion days, sleep disturbances, stable oral intake alternatives, and improved stool characteristics [91][92][93][94][95]. Growth hormone (GH) activates the proliferation of intestinal stem cells (ISCs), enhances the formation of crypt organoids, and drives the differentiation of ISCs into Paneth cells and enterocytes. Glutamine (GLN), on the other hand, also enhances the proliferation of ISCs [96]. It has been hypothesized that the administration of growth factors and/or nutrients could enhance further compensation of the remnant intestine and thereby improve absorption. Specifically, animal studies have shown that there is enhanced cellularity with the administration of GH or GLN or a fiber-containing diet. A retrospective evaluation of 17 studies carried out in humans with SBS showed an improvement in protein absorption by 39% and a 33% decrease in stool output with the GH + GLN + DIET (high-carbohydrate, low-fat diet). In the long-term study, 40% of the group remained off PN, and an additional 40% had reduced their PN requirements [97]. More recent studies have suggested that the benefits of administering recombinant human GH alone, or together with GLN with or without a low-fat diet containing a high level of carbohydrates (fiber), are, if any, marginal, and there are concerns about their potential long-term risks [98].
7. Management of Other Specific Conditions
The clinical management of the patients with IF and SBS includes preventing and treating a range of complications related to the pathophysiology of the small and large intestines (e.g., nephrolithiasis [15][16][17], cholelithiasis [13][14], and metabolic bone diseases [17]) or to the artificial nutritional support systems (IAFLD and catheter-related bloodstream infections). Figure 8 outlines the critical points in the management of these conditions [26][99][100].
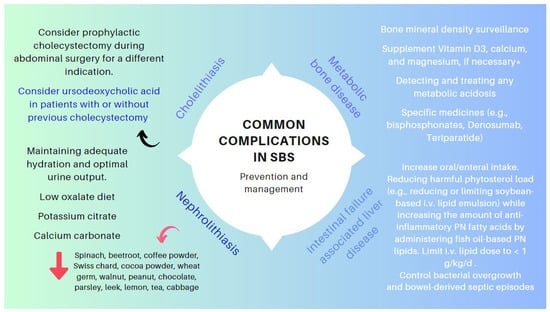
Figure 8. Key points in the management of specific complications associated with SBS. * SBS leads to gastrointestinal losses of magnesium. Hypomagnesaemia (mainly if Mg < 1.5 mg/dL) often leads to genuine hypocalcemia by blocking parathormone secretion and promoting parathormone resistance. Hence, the importance of correcting hypomagnesemia so as not to aggravate metabolic osteopat.
8. Surgical Management
Conservative management remains the first-line approach for patients with SBS. Nevertheless, various nontransplantation surgical procedures have a role in improving intestinal function in SBS and have shown their effectiveness in properly selected patients. These surgeries focus on slowing down intestinal transit, to increase contact time between nutrients and the mucosa, to correct remnant bowel dilation and stasis, to improve intestinal motility, and to increase mucosal surface area. The type of procedure is selected depending on the age, length, and functionality of the remnant bowel, the existence of intestinal dilation, the presence of SIBO, and the presence or absence of PN-related complications. The most common procedures include:
- (1)
-
Preserving the existing intestine: It is common that after the initial resection, some patients need to be re-operated for various reasons (e.g., stenosis and perforations). In these scenarios, avoiding a resection and preserving the existing length of the intestinal remnant (e.g., serosal patching for certain strictures and chronic perforations) are essential. When carrying out a resection becomes unavoidable, an end-to-end anastomosis is preferred to prevent blind loops and, thus, optimize the functionality of the hindgut [101].
- (2)
-
Restoration of intestinal continuity, elimination of a stoma with the aim of improving the patient’s quality of life and avoiding some of the complications associated with central venous catheters [47].
- (3)
-
Tapering surgery when the remaining small bowel remains excessively dilated [102]. Intestinal tapering may be necessary in this context as a dilated intestine increases the risk of mucosal injury, bloodstream infections, and liver disease in patients with SBS [103]. Several techniques have been described to taper the dilated small bowel, including longitudinal intestinal lengthening and tapering, serial transverse enteroplasty, and spiral intestinal lengthening and tailoring [102][104].
- (4)
-
Correction of stenoses, if possible, with stricturoplasties and with remodeling or intestinal plication if needed [105].
- (5)
-
Serosal patching for chronic fistulae to prevent avoidable intestinal excisions [106].
- (6)
-
Autologous gastrointestinal reconstruction operation: The aim of this procedure is to either enhance the mucosal surface area for absorption (e.g., lengthening procedures) or to slow intestinal transit to facilitate the assimilation of the nutrients or counterbalance stasis that cause gastrointestinal symptoms due to SIBO (e.g., reversing the segments of the intestine) [107][108], creating intestinal valves, or interposing a colonic segment in the mall intestinal remnant in either an isoperistaltic or antiperistaltic fashion [109][110][111][112]. These procedures should only be used in carefully selected patients and in centers with proven experience [113][114][115].
New surgical methods are currently under development, including spring-mediated distraction enterogenesis (implantation of self-expanding springs through an endoscopic intervention) [116] and a set of techniques focused on regenerative medicine, opening up the possibility of repairing and replacing intestinal tissue on demand. The latter include a variety of tissue-engineered small intestines (TESIs). TESI approaches range from small intestinal submucosa grafts to intestinal tissue repurposing with either stem cells or organoid units, the latter of which appears extraordinarily promising [113][117][118][119][120].
9. Intestinal Transplantation (ITx)
ITx can be lifesaving and can improve the quality of life for patients with irreversible IF. The long-term results of ITx are not as good as other types of visceral transplants (e.g., liver, heart, or kidney). The intestine is a complex organ to transplant due to its immunogenicity, large population of donor immune cells present within the graft, and its nonsterile contents. Rejection causes barrier failure and bacterial translocation, so sepsis may occur when increased immunosuppression is required [121]. Thus, unlike renal failure, ITx cannot yet be recommended as an alternative therapy for patients stably maintained on intravenous nutrition. Unfortunately, the outcomes following ITx are not optimal, with 10−20% of patients continuing to be dependent on, at least, partial PN and survival at ten years post-transplant of only 40% with a lower graft survival rate [122][123][124].
Scientific societies have formulated guidelines and recommendations focused on the need to balance the advantages and disadvantages of ITx [36][121][123][125][126][127][128]. Following this postulate, ESPEN published, in 2016 [122] and 2021 [36], specific recommendations regarding the indications for ITx in patients with SBS, which have ultimately been updated in 2023 [128]. Patients with SBS–IF with high morbidity or a low acceptance of PN should be considered for early listing for ITx on a case-by-case basis [122][123][124][125][126][127][128]. So, threatening complications warranting the consideration of intestinal Tx include IAFLD, recurrent sepsis, and threatened loss of central venous access. Table 5 shows the revised criteria for placement on a waitlist for ITx, presuming that a multidisciplinary team will have assessed patients, explored rehabilitation options, and a state of permanent or life-limiting intestinal failure exists [24][36][126][127][128][129][130].
Table 5. Clinical conditions that should be considered for the indication of ITx in patients with SBS and IF (adapted from references [36][127][128]).
| Clinical Condition | Criteria | Comments |
|---|---|---|
| IAFLD | Forthcoming (total bilirubin above 3–6 mg/dL (54–108 μmol/L), progressive thrombocytopenia, and progressive splenomegaly) or overt liver failure (portal hypertension, hepatosplenomegaly, hepatic fibrosis, or cirrhosis because of IFALD). |
Liver biopsy is the gold standard test to identify the stage of liver disease, the timing of transplantation, and the type of transplant required (isolated ITx or combined liver–ITx) It has been suggested that patients with METAVIR stage II fibrosis (perisinusoidal and portal/periportal fibrosis) should be considered for an isolated ITx, whereas those with stage III (bringing fibrosis) or IV (cirrhosis) should be considered for LITx. |
| Esophageal varices, ascites, and impaired synthetic function are not always present. | ||
| Central venous catheter-related thrombosis (CRVT) | Thrombosis of two or more central veins (loss of right and left internal jugular vein, right and left subclavian vein, or right and left femoral vein). |
CRVT is a severe complication that is responsible for the loss of central venous accesses in patients on HPN and may be an indication for ITx if it affects two or more of the central venous vessels. For adults, this criterion is on a case-by-case basis. |
| Catheter-related bloodstream infection (CRBSI). | Frequent central line sepsis: two or more episodes per year of systemic sepsis secondary to line infections requiring hospitalization; a single episode of line-related fungemia; septic shock and/or acute respiratory distress syndrome. |
Children: two admissions to an intensive care unit because of cardiorespiratory failure (mechanical ventilation or inotrope infusion) due to sepsis. For adults, this criterion is on a case-by-case basis, because recurrent episodes of CRBSI have been demonstrated to not be associated with an increased risk of death. |
| Other indications | Refractory electrolyte changes and frequent episodes of dehydration. High risk of death attributable to underlying diseases, such as congenital mucosal disorders, ultra-short bowel syndrome (gastrostomy; duodenostomy; residual small bowel <10 cm in infants and <20 cm in adults), and invasive intra-abdominal desmoid tumors; patients with high morbidity (frequent hospitalization, narcotic dependency, and inability to function (i.e., pseudo-obstruction; high output stoma)) or a low acceptance of long-term PN, especially in young patients. |
|
IAFLD: intestinal failure-associated liver disease (previously referred to as parenteral nutrition-associated liver disease, or PNALD). ITx: intestinal transplant. LITx: combined intestinal and liver transplantation. HPN: home parenteral nutrition. CRBSI: catheter-related bloodstream infection.
References
- Kumar, A.; Al-Hassi, H.O.; Jain, M.; Phipps, O.; Ford, C.; Gama, R.; Steed, H.; Butterworth, J.; McLaughlin, J.; Galbraith, N.; et al. A single faecal bile acid stool test demonstrates potential efficacy in replacing SeHCAT testing for bile acid diarrhoea in selected patients. Sci. Rep. 2022, 12, 8313.
- Arasaradnam, R.P.; Steven Brown, S.; Forbes, A.; Fox, M.R.; Hungin, P.; Kelman, L.; Major, G.; O’Connor, M.; Dave SSanders, D.S.; Sinha, R.; et al. Guidelines for the investigation of chronic diarrhoea in adults: British Society of Gastroenterology, 3rd edition. Gut 2018, 67, 1380–1399.
- Calzadilla, N.; Comiskey, S.M.; Dudeja, P.K.; Saksena, S.; Gill, R.K.; Alrefai, W.A. Bile acids as inflammatory mediators and modulators of intestinal permeability. Front. Immunol. 2022, 13, 1021924.
- Kumar, A.; Galbraith, N.; Al-Hassi, H.O.; Jain, M.; Phipps, O.; Butterworth, J.; Steed, H.; McLaughlin, J.; Brookes, M.J. The impact of treatment with bile acid sequestrants on quality of life in patients with bile acid diarrhoea. BMC Gastroenterol. 2022, 22, 325.
- Germani, P.; Zucca, A.; Giudici, F.; Terranova, S.; Troian, M.; Samardzic, N.; Greco, M.; Janez, J.; Gasparini, C.; Cagnazzo, E.; et al. Ileocecal valve syndrome and vitamin B12 deficiency after surgery: A multicentric prospective study. Updates Surg. 2021, 73, 569–580.
- Fordtran, J.S.; Rector, F.C., Jr.; Ewton, M.F.; Soter, N.; Kinney, J. Permeability characteristics of the human small intestine. J. Clin. Investig. 1965, 44, 1935–1944.
- Ziegler, T.R.; Cole, C.R. Small bowel bacterial overgrowth in adults: A potential contributor to intestinal failure. Curr. Gastroenterol. Rep. 2007, 9, 463–467.
- Sorathia, S.J.; Chippa, V.; Rivas, J.M. Small Intestinal Bacterial Overgrowth. In StatPearls ; StatPearls Publishing: Treasure Island, FL, USA, 2023.
- Bischoff, S.C.; Bager, P.; Escher, J.; Forbes, A.; Hébuterne, X.; Hvas, C.L.; Joly, F.; Klek, S.; Krznaric, Z.; Ockenga, J. ESPEN guideline on Clinical Nutrition in inflammatory bowel disease. Clin. Nutr. 2023, 42, 352–379.
- Jain, A.; Jhinger, K.; Bellas, J. Recurrent Encephalopathy and Severe Anion Gap Metabolic Acidosis in a Patient with Short Bowel: It Is D-Lactic Acidosis. Case Rep. Gastroenterol. 2021, 15, 92–96.
- Uribarri, J.; Oh, M.S.; Carroll, H.J. D-lactic acidosis. A review of clinical presentation, biochemical features, and pathophysiologic mechanisms. Medicine 1998, 77, 73–82.
- Bianchetti, D.G.A.M.; Amelio, G.S.; Lava, S.A.G.; Bianchetti, M.G.; Simonetti, G.D.; Agostoni, C.; Fossali, E.F.; Milani, G.P. D-lactic acidosis in humans: Systematic literature review. Pediatr. Nephrol. 2018, 33, 673–681.
- Gao, X.; Zhang, L.; Wang, S.; Xiao, Y.; Song, D.; Zhou, D.; Wang, X. Prevalence, Risk Factors, and Complications of Cholelithiasis in Adults with Short Bowel Syndrome: A Longitudinal Cohort Study. Front. Nutr. 2021, 8, 762240.
- Thompson, J.S.; Rochling, F.A.; Lyden, E.; Merani, S.; Vargas, L.M.; Grant, W.J.; Langnas, A.N.; Mercer, D.F. Cholecystectomy prior to short bowel syndrome does not alter nutritional prognosis. Am. J. Surg. 2022, 224, 1285–1288.
- Yang, J.; Sun, H.; Wan Mamtawla, G.; Gao, X.; Zhang, L.; Li, Y.; Wang, X.; Li, J. Risk Factors for Nephrolithiasis in Adults with Short Bowel Syndrome. Ann. Nutr. Metab. 2019, 75, 47–54.
- Salazar, J.A.; Carey, A.N.; Duggan, C.P. Nutritional, and medical approaches to intestinal failure. Curr. Opin. Clin. Nutr. Metab. Care 2023, 26, 201–209.
- Johnson, E.; Vu, L.; Matarese, L.E. Bacteria, Bones, and Stones: Managing Complications of Short Bowel Syndrome. Nutr. Clin. Pract. 2018, 33, 454–466.
- Malec, L.M.; Cooper, J.; Rudolph, J.; Michaels, M.G.; Ragni, M.V. Prophylactic rtPA in the Prevention of Line-associated Thrombosis and Infection in Short Bowel Syndrome. J. Pediatr. Gastroenterol. Nutr. 2018, 66, 972–975.
- Mundi, M.S.; Mohamed Elfadil, O.; Hurt, R.T.; Bonnes, S.; Salonen, B.R. Management of long-term home parenteral nutrition: Historical perspective, common complications, and patient education and training. JPEN J. Parenter. Enter. Nutr. 2023, 47 (Suppl. S1), S24–S34.
- Stewart, A.G.; Laupland, K.B.; Tabah, A. Central line associated and primary bloodstream infections. Curr. Opin. Crit. Care 2023, 29, 423–429.
- Alanazi, F.K.; Lapkin, S.; Molloy, L.; Sim, J. Healthcare-associated infections in adult intensive care units: A multisource study examining nurses’ safety attitudes, quality of care, missed care, and nurse staffing. Intensive Crit. Care Nurs. 2023, 78, 103480.
- Wang, P.; Wang, Y.; Lu, L.; Yan, W.; Tao, Y.; Zhou, K.; Jia, J.; Cai, W. Alterations in intestinal microbiota relate to intestinal failure-associated liver disease and central line infections. J. Pediatr. Surg. 2017, 52, 1318–1326.
- Gotchac, J.; Poullenot, F.; Guimber, D.; Ecochard-Dugelay, E.; Schneider, S.; Peretti, N.; Billiauws, L.; Borderon, C.; Breton, A.; Chaillou Legault, E.; et al. Management of Central Venous Catheters in Children and Adults on Home Parenteral Nutrition: A French Survey of Current Practice. Nutrients 2022, 14, 2532.
- Rosen, H.; Sebesta, C.G.; Sebesta, C. Management of Low Anterior Resection Syndrome (LARS) following Resection for Rectal Cancer. Cancers 2023, 15, 778.
- Cavicchi, M.; Beau, P.; Crenn, P.; Degott, C.; Messing, B. Prevalence of liver disease and contributing factors in patients receiving home parenteral nutrition for permanent intestinal failure. Ann. Intern. Med. 2000, 132, 525–532.
- Mutanen, A.; Lohi, J.; Merras-Salmio, L.; Koivusalo, A.; Pakarinen, M.P. Prediction, identification, and progression of histopathological liver disease activity in children with intestinal failure. J. Hepatol. 2021, 74, 593–602.
- Ponzo, V.; Pellegrini, M.; Cioffi, I.; Scaglione, L.; Bo, S. The Refeeding Syndrome: A neglected but potentially serious condition for inpatients. A narrative review. Intern. Emerg. Med. 2021, 16, 49–60.
- Marinella, M.A. The refeeding syndrome and hypophosphatemia. Nutr. Rev. 2003, 61, 320–323.
- Da Silva, J.S.V.; Seres, D.S.; Sabino, K.; Adams, S.C.; Berdahl, G.J.; Citty, S.W.; Cober, M.P.; Evans, D.C.; Greaves, J.R.; Gura, K.M.; et al. ASPEN Consensus Recommendations for Refeeding Syndrome. Nutr. Clin. Pract. 2020, 35, 178–195.
- Araujo-Castro, M.; Vázquez-Martínez, C. The refeeding syndrome. Importance of phosphorus. Med. Clin. 2018, 150, 472–478.
- Crook, M.A.; Hally, V.; Panteli, J.V. The importance of the refeeding syndrome. Nutrition 2001, 17, 632–637.
- Pacei, F.; Tesone, A.; Laudi, N.; Laudi, E.; Cretti, A.; Pnini, S.; Varesco, F.; Colombo, C. The Relevance of Thiamine Evaluation in a Practical Setting. Nutrients 2020, 12, 2810.
- Dos Santos, V.M.; Dos Santos, L.A.M.; Sugai, T.A.M. Refeeding syndrome: A challenging entity. An. Sist. Sanit. Navar. 2022, 45, e0995.
- Wales, P.W.; Allen, N.; Worthington, P.; George, D.; Compher, C.; American Society for Parenteral and Enteral Nutrition; Teitelbaum, D. A.S.P.E.N. Clinical Guidelines: Support of Pediatric Patients With Intestinal Failure at Risk of Parenteral Nutrition–Associated Liver Disease. JPEN J. Parenter. Enter. Nutr. 2014, 38, 538–557.
- Iyer, K.; DiBaise, J.K.; Rubio-Tapia, A. AGA clinical practice update on management of short bowel syndrome: Expert review. Clin. Gastroenterol. Hepatol. 2022, 20, 2185–2194.
- Cuerda, C.; Pironi, L.; Arends, J.; Bozzetti, F.; Gillanders, L.; Jeppesen, P.B.; Joly, F.; Kelly, D.; Lal, S.; Staun, M.; et al. ESPEN practical guideline: Clinical nutrition in chronic intestinal failure. Clin. Nutr. 2021, 40, 5196–5220.
- Matarese, L.E.; Harvin, G. Nutritional Care for Patients with Intestinal Failure. Gastroenterol. Clin. N. Am. 2021, 50, 201–216.
- Matarese, L.E.; Jeppesen, P.B.; O’Keefe, S.J. Short bowel syndrome in adults: The need for an interdisciplinary approach and coordinated care. JPEN J. Parenter. Enter. Nutr. 2014, 38 (Suppl. S1), 60S–64S.
- Wall, E.; Catron, H.; Delgado, A.; Greif, S.; Herlitz, J.; Moccia, L.; Lozano, E.; Mercer, D.; Vanuytsel, T.; Berner-Hansen, M.; et al. A multidisciplinary team evaluation of management guidelines for adult short bowel syndrome. Clin. Nutr. ESPEN 2023, 54, 41–44.
- Geransar, P.; Lal, S.; Jeppesen, P.B.; Pironi, L.; Rzepa, E.; Schneider, S.M. Survey of healthcare professionals’ experiences of care delivery in patients with chronic intestinal failure: ATLAS of Variance. Clin. Nutr. ESPEN 2023, 54, 157–165.
- Belcher, E.; Mercer, D.; Raphael, B.P.; Salinas, G.D.; Stacy, S.; Tappenden, K.A. Management of short-bowel syndrome: A survey of unmet educational needs among healthcare providers. JPEN J. Parenter. Enter. Nutr. 2022, 46, 1839–1846.
- Premkumar, M.H.; Soraisham, A.; Bagga, N.; Adriana Massieu, L.; Maheshwari, A. Nutritional Management of Short Bowel Syndrome. Clin. Perinatol. 2022, 49, 557–572.
- Bielawska, B.; Allard, J.P. Parenteral nutrition and intestinal failure. Nutrients 2017, 9, 466.
- Bering, J.; DiBaise, J.K. Home Parenteral and Enteral Nutrition. Nutrients 2022, 14, 2558.
- Doley, J. Enteral Nutrition Overview. Nutrients 2022, 14, 2180.
- Avitzur, Y.; Courtney-Martin, G. Enteral approaches in malabsorption. Best Pract. Res. Clin. Gastroenterol. 2016, 30, 295–307.
- Bering, J.; DiBaise, J.K. Short bowel syndrome in adults. Am. J. Gastroenterol. 2022, 117, 876–883.
- Bonnes, S.L.; Salonen, B.R.; Hurt, R.T.; McMahon, M.T.; Mundi, M.S. Parenteral and Enteral Nutrition-from Hospital to Home: Will It Be Covered? Nutr. Clin. Pract. 2017, 32, 730–738.
- Griffin, G.E.; Fagan, G.E.; Hodgson, H.J.; Chadwick, V.S. Enteral therapy in the management of massive gut resection complicated by chronic fluid and electrolyte depletion. Dig. Dis. Sci. 1982, 27, 902–908.
- Gustafsson, U.O.; Ljungqvist, O. Perioperative nutritional management in digestive tract surgery. Curr. Opin. Clin. Nutr. Metab. Care 2011, 14, 504–509.
- Berger, M.M.; Shenkin, A.; Schweinlin, A.; Amrein, K.; Augsburger, M.; Biesalski, H.K.; Bischoff, S.C.; Casaer, M.P.; Gundogan, K.; Lepp, H.L.; et al. ESPEN micronutrient guideline. Clin. Nutr. 2022, 41, 1357.e424.
- Btaiche, I.F.; Carver, P.L.; Welch, K.B. Dosing and monitoring of trace elements in long-term home parenteral nutrition patients. JPEN J. Parenter. Enter. Nutr. 2011, 35, 736–747.
- Jin, J.; Mulesa, L.; Carrilero Rouillet, M. Trace Elements in Parenteral Nutrition: Considerations for the Prescribing Clinician. Nutrients 2017, 9, 440.
- McKeever, L. Vitamin and Trace Elements. In The ASPEN Adult Nutrition Support Core Curriculum, 3rd ed.; Mueller, C.M., Ed.; ASPEN: Silver Spring, MD, USA, 2017; pp. 139–184.
- Konrad, D.; Mitchell, R.; Hendrickson, E. Home nutrition support. In The ASPEN Adult Nutrition Support Core Curriculum, 3rd ed.; Mueller, C.M., Ed.; ASPEN: Silver Spring, MD, USA, 2017; pp. 765–784.
- Charney, P.; Malone, A. Biochemical Test, Medical Data, and Procedures. In Pocket Guide to Nutrition Assessment, 4th ed.; Charney, P., Malone, A., Eds.; Academy of Nutrition and Dietetics: Chicago, IL, USA, 2022; pp. 111–201.
- Williams, N.S.; Evans, P.; King, R.F. Gastric acid secretion and gastrin production in the short bowel syndrome. Gut 1985, 26, 914–919.
- Thompson, J.S.; Langnas, A.N. Surgical approaches to improving intestinal function in the short bowel syndrome. Arch. Surg. 1999, 134, 706–711.
- Kumpf, V.J. Pharmacologic management of diarrhea in patients with short bowel syndrome. JPEN J. Parenter. Enter. Nutr. 2014, 38 (Suppl. S1), 38S–44S.
- Zafar, H.; Jimenez, B.; Schneider, A. Small intestinal bacterial overgrowth: Current update. Curr. Opin. Gastroenterol. 2023, 39, 522–528.
- Larsen, H.M.; Krogh, K.; Borre, M.; Gregersen, T.; Mejlby Hansen, M.; Arveschoug, A.K.; Christensen, P.; Drewes, A.M.; Emmertsen, K.J.; Laurberg, S.; et al. Chronic loose stools following right-sided hemicolectomy for colon cancer and the association with bile acid malabsorption and small intestinal bacterial overgrowth. Color. Dis. 2023, 25, 600–607.
- Korzilius, J.W.; Gompelman, M.; Wezendonk, G.T.J.; Jager, N.G.L.; Rovers, C.P.; Brüggemann, R.J.M.; Wanten, G.J.A. Oral antimicrobial agents in patients with short bowel syndrome: Worth a try! J. Antimicrob. Chemother. 2023, 78, 2008–2014.
- Hofmann, A.F. The syndrome of ileal disease and the broken enterohepatic circulation: Cholerheic enteropathy. Gastroenterology 1967, 52, 752–757.
- Hoffmann, A.F.; Poley, J.R. Cholestyramine treatment of diarrhea associated with ileal resection. N. Engl. J. Med. 1969, 281, 397–402.
- Hofmann, A.F.; Poley, J.R. Role of bile acid malabsorption in pathogenesis of diarrhea and steatorrhea in patients with ileal resection. I. Response to cholestyramine or replacement of dietary long chain triglyceride by medium chain triglyceride. Gastroenterology 1972, 62, 918–934.
- Scaldaferri, F.; Pizzoferrato, M.; Ponziani, F.R.; Gasbarrini, G.; Gasbarrini, A. Use and indications of cholestyramine and bile acid sequestrants. Intern. Emerg. Med. 2013, 8, 205–210.
- Poley, J.R.; Hofmann, A.F. Role of fat maldigestion in pathogenesis of steatorrhea in ileal resection. Fat digestion after two sequential test meals with and without cholestyramine. Gastroenterology 1976, 71, 38–44.
- DiBaise, J.K. Does my patient have bile acid malabsorption? Pract. Gastroenterol. 2020, 44, 10–24.
- Sainath, N.N.; Bales, C.; Brownell, J.N. Octavia Pickett-Blakely, Aisha Sattar, Virginia A Stallings. Impact of Pancreatic Enzymes on Enteral Fat and Nitrogen Absorption in Short Bowel Syndrome. J. Pediatr. Gastroenterol. Nutr. 2022, 75, 36–41.
- Mouillot, T.; Beylot, M.; Drai, J.; Hillon, P.; Gelas, P.; Lauverjat, M.; Brondel, L.; Chambrier, C. Effect of bile acid supplementation on endogenous lipid synthesis in patients with short bowel syndrome: A pilot study. Clin. Nutr. 2020, 39, 928–934.
- O’Keefe, S.J.; Haymond, M.W.; Bennet, W.M.; Oswald, B.; Nelson, D.K.; Shorter, R.G. Long-acting somatostatin analogue therapy and protein metabolism in patients with jejunostomies. Gastroenterology 1994, 107, 379–388.
- Nightingale, J.M.D. How to manage a high-output stoma. Frontline Gastroenterol. 2021, 13, 140–151.
- Kusuhara, K.; Kusunoki, M.; Okamoto, T.; Sakanoue, Y.; Utsunomiya, J. Reduction of the effluent volume in high- output ileostomy patients by a somatostatin analogue, SMS 201-995. Int. J. Color. Dis. 1992, 7, 202–205.
- Shaffer, J.L.; O’Hanrahan, T.; Rowntree, S. Does somatostatin analogue (201-995) reduce high output stoma effluent? A controlled trial. Gut 1988, 29, A1432–A1433.
- Nightingale, J.M.; Walker, E.R.; Burnham, W.R.; Farthing, M.J.; Lennard-Jones, J.E. Octreotide (a somatostatin analogue) improves the quality of life in some patients with a short intestine. Aliment. Pharmacol. Ther. 1989, 3, 67–73.
- Ladefoged, K.; Christensen, K.C.; Hegnhoj, J.; Jarnum, S. Effect of a long-acting somatostatin analogue SMS 201-995 on jejunostomy effluents in patients with severe short bowel syndrome. Gut 1989, 30, 943–949.
- Lémann, M.; de Montigny, S.; Mahé, S. Effect of octreotide on water and electrolytes losses, nutrient absorption, and transit in short bowel syndrome. Eur. J. Gastroenterol. Hepatol. 1993, 5, 817–822.
- O’Keefe, S.J.; Peterson, M.E.; Fleming, C.R. Octreotide as an adjunct to home parenteral nutrition in the management of permanent end-jejunostomy syndrome. JPEN J. Parenter. Enter. Nutr. 1994, 18, 26–34.
- Nightingale, J.M.; Lennard-Jones, J.E.; Gertner, D.J.; Wood, S.R.; Bartram, C.I. Colonic preservation reduces need for parenteral therapy, increases incidence of renal stones, but does not change high prevalence of gall stones in patients with a short bowel. Gut 1992, 33, 1493–1497.
- Dowling, R.H.; Hussaini, S.H.; Murphy, G.M.; Wass, J.A. Gallstones during octreotide therapy. Digestion 1993, 54, 107–120.
- Nehra, V.; Camilleri, M.; Burton, D.; Oenning, L.; Kelly, D.G. An open trial of octreotide long-acting release in the management of short bowel syndrome. Am. J. Gastroenterol. 2001, 96, 1494–1498.
- Mesli, Y.; Holterbach, L.; Delhorme, J.B.; Lakkis, Z.; Ortega-Deballon, P.; Deguelte, S.; Rohr, S.; Brigand, C.; Meyer, N.; Romain, B. Is lanreotide useful in high output stoma? comparison between lanreotide to conventional antidiarrheal treatment alone. J. Investig. Surg. 2020, 4, 1312–1316.
- Jeppesen, P.B.; Pertkiewicz, M.; Messing, B.; Iyer, K.; Seidner, D.L.; O’keefe, S.J.D.; Forbes, A.; Bo Joelsson, H.H. Teduglutide reduces need for parenteral support among patients with short bowel syndrome with intestinal failure. Gastroenterology 2012, 143, 1473–1481.
- Jeppesen, P.B.; Pertkiewicz, M.; Forbes, A.; Pironi, L.; Gabe, S.M.; Joly, F.; Messing, B.; Loth, S.; Youssef, N.N.; Heinze, H.; et al. Quality of life in patients with short bowel syndrome treated with the new glucagon-like peptide-2 analogue teduglutide—Analyses from a randomised, placebo-controlled study. Clin. Nutr. 2013, 32, 713–721.
- Jeppesen, P.B.; Gilroy, R.; Pertkiewicz, M.; Allard, J.P.; Messing, B.; O’Keefe, S.J. Randomised placebo-controlled trial of teduglutide in reducing parenteral nutrition and/or intravenous fluid requirements in patients with short bowel syndrome. Gut 2011, 60, 902–914.
- Jeppesen, P.B.; Gabe, S.M.; Seidner, D.L.; Lee, H.M.; Olivier, C. Factors Associated with Response to Teduglutide in Patients with Short-Bowel Syndrome and Intestinal Failure. Gastroenterology 2018, 154, 874–885.
- Jeppesen, P.B. Pharmacologic options for intestinal rehabilitation in patients with short bowel syndrome. JPEN J. Parenter. Enter. Nutr. 2014, 38 (Suppl. S1), 45S–52S.
- Nørholk, L.M.; Holst, J.J.; Jeppesen, P.B. Treatment of adult short bowel syndrome patients with teduglutide. Expert Opin. Pharmacother. 2012, 13, 235–243.
- Valiente, P.A.; Nim, S.; Kim, J.; Kim, P.M. Computational Design of Potent and Selective d-Peptide Agonists of the Glucagon-like Peptide-2 Receptor. J. Med. Chem. 2023, 66, 10342–10353.
- de Dreuille, B.; Nuzzo, A.; Bataille, J.; Mailhat, C.; Billiauws, L.; Le Gall, M.; Joly, F. Post-Marketing Use of Teduglutide in a Large Cohort of Adults with Short Bowel Syndrome-Associated Chronic Intestinal Failure: Evolution and Outcomes. Nutrients 2023, 15, 2448.
- Greif, S.; Maasberg, S.; Wehkamp, J.; Fusco, S.; Zopf, Y.; Herrmann, H.J.; Lamprecht, G.; Jacob, T.; Schiefke, I.; von Websky, M.W.; et al. Long-term results of teduglutide treatment for chronic intestinal failure—Insights from a national, multi-centric patient home-care service program. Clin. Nutr. ESPEN 2022, 51, 222–230.
- Blüthner, E.; Pape, U.F.; Tacke, F.; Greif, S. Quality of Life in Teduglutide-Treated Patients with Short Bowel Syndrome Intestinal Failure-A Nested Matched Pair Real-World Study. Nutrients 2023, 15, 1949.
- Joly, F.; Seguy, D.; Nuzzo, A.; Chambrier, C.; Beau, P.; Poullenot, F.; Thibault, R.; Armengol Debeir, L.; Layec, S.; Boehm, V.; et al. Six-month outcomes of teduglutide treatment in adult patients with short bowel syndrome with chronic intestinal failure: A real-world French observational cohort study. Clin. Nutr. 2020, 39, 2856–2862.
- Pironi, L. Translation of Evidence into Practice with Teduglutide in the Management of Adults with Intestinal Failure due to Short-Bowel Syndrome: A Review of Recent Literature. JPEN J. Parenter. Enter. Nutr. 2020, 44, 968–978.
- Kochar, B.; Herfarth, H.H. Teduglutide for the treatment of short bowel syndrome—A safety evaluation. Expert Opin. Drug Saf. 2018, 17, 733–739.
- Chen, Y.; Tsai, Y.H.; Tseng, B.J.; Tseng, S.H. Influence of Growth Hormone and Glutamine on Intestinal Stem Cells: A Narrative Review. Nutrients 2019, 11, 1941.
- Byrne, T.A.; Wilmore, D.W.; Iyer, K.; DiBaise, J.K.; Clancy, K.; Robinson, M.K.; Chang, P.; Gertner, J.M.; Lautz, D. Growth hormone, glutamine, and an optimal diet reduces parenteral nutrition in patients with short bowel syndrome: A prospective, randomized, placebo-controlled, double-blind clinical trial. Ann. Surg. 2005, 242, 655–661.
- Ling, L.; Irving, M. The effectiveness of growth hormone, glutamine and a low-fat diet containing high carbohydrate on the enhancement of the function of remnant intestine among patients with short bowel syndrome: A review of published trials. Clin. Nutr. 2001, 20, 199–204.
- Lauriti, G.; Zani, A.; Aufieri, R.; Cananzi, M.; Chiesa, P.L.; Eaton, S.; Pierro, A. Incidence, prevention, and treatment of parenteral nutrition-associated cholestasis and intestinal failure-associated liver disease in infants and children: A systematic review. JPEN J. Parenter. Enter. 2014, 38, 70–85.
- Bond, A.; Huijbers, A.; Pironi, L.; Schneider, S.M.; Wanten, G.; Lal, S. Review article: Diagnosis and management of intestinal failure-associated liver disease in adults. Aliment. Pharmacol. Ther. 2019, 50, 640–653.
- Seetharam, P.; Rodrigues, G. Short Bowel Syndrome. Saudi J. Gastroenterol. 2011, 17, 229–235.
- Cruz, R.J., Jr. Modified Antimesenteric Tapering Enteroplasty: An Alternative Technique for the Treatment of Dysfunctional Anastomosis in Patients with Short Bowel. Dis. Colon Rectum 2021, 64, e520–e525.
- Hukkinen, M.; Mutanen, A.; Pakarinen, M.P. Small bowel dilation in children with short bowel syndrome is associated with mucosal damage, bowel-derived bloodstream infections, and hepatic injury. Surgery 2017, 162, 670–679.
- Wendel, D.; Javid, P.J. Medical and Surgical Aspects of Intestinal Failure in the Child. Surg. Clin. N. Am. 2022, 102, 861–872.
- Bueno, J. Surgical strategies in short bowel syndrome. Nutr. Hosp. 2007, 22 (Suppl. S2), 103–112.
- Carey, J.N.; Sheckter, C.C.; Watt, A.J.; Lee, G.K. Intra-abdominal pedicled rectus abdominis muscle flap for treatment of high-output enterocutaneous fistulae: Case reports and review of literature. J. Plast. Reconstr. Aesthet. Surg. 2013, 66, 1145–1148.
- Beyer-Berjot, L.; Joly, F.; Maggiori, L.; Corcos, O.; Bouhnik, Y.; Bretagnol, F.; Panis, Y. Segmental reversal of the small bowel can end permanent parenteral nutrition dependency: An experience of 38 adults with short bowel syndrome. Ann. Surg. 2012, 256, 739–744.
- Panis, Y.; Messing, B.; Rivet, P.; Coffin, B.; Hautefeuille, P.; Matuchansky, C.; Rambaud, J.C.; Valleur, P. Segment reversal of the small bowel as an alternative to intestinal transplantation in patients with short bowel syndrome. Ann. Surg. 1997, 225, 401–407.
- Lauro, A.; Cirocchi, R.; Cautero, N.; Dazzi, A.; Pironi, D.; Di Matteo, F.M.; Santoro, A.; Pironi, L.; Pinna, A.D. Reconnection surgery in adult post-operative short bowel syndrome <100 cm: Is colonic continuity sufficient to achieve enteral autonomy without autologous gastrointestinal reconstruction? Report from a single center and systematic review of literature. G. Chir. 2017, 38, 163–175.
- Rege, A.S.; Sudan, D.L. Autologous gastrointestinal reconstruction: Review of the optimal nontransplant surgical options for adults and children with short bowel syndrome. Nutr. Clin. Pract. 2013, 28, 65–74.
- Boroni, G.; Parolini, F.; Stern, M.V.; Moglia, C.; Alberti, D. Autologous Intestinal Reconstruction Surgery in Short Bowel Syndrome: Which, When, and Why. Front. Nutr. 2022, 9, 861093.
- Thompson, J.S. Surgical approach to the short bowel syndrome: Procedures to slow intestinal transit. Eur. J. Pediatr. Surg. 1999, 9, 263–266.
- Muff, J.L.; Sokolovski, F.; Walsh-Korb, Z.; Choudhury, R.A.; Dunn, J.C.Y.; Holland-Cunz, S.G.; Vuille-Dit-Bille, R.N. Surgical Treatment of Short Bowel Syndrome-The Past, the Present and the Future, a Descriptive Review of the Literature. Children 2022, 9, 1024.
- Aubert, M.; Mege, D.; Billiauws, L.; Joly, F.; Panis, Y. State-of-the-art colorectal disease: Conservative surgical management of intestinal failure in adults. Int. J. Color. Dis. 2021, 36, 1597–1607.
- Horslen, S.P.; Smith, J.M.; Ahn, Y.; Skeans, M.A.; Cafarella, M.; Noreen, S.M.; Snyder, J.J.; Israni, A.K. OPTN/SRTR 2019 annual data report: Intestine. Am. J. Transpl. 2021, 21 (Suppl. S2), 316–355.
- Huynh, N.; Dubrovsky, G.; Rouch, J.D.; Scott, A.; Chiang, E.; Nguyen, T.; Wu, B.M.; Shekherdimian, S.; Krummel, T.M.; Dunn, J.C.Y. Three-Dimensionally Printed Surface Features to Anchor Endoluminal Spring for Distraction Enterogenesis. PLoS ONE 2018, 13, e0200529.
- Sugimoto, S.; Kobayashi, E.; Fujii, M.; Ohta, Y.; Arai, K.; Matano, M.; Ishikawa, K.; Miyamoto, K.; Toshimitsu, K.; Takahashi, S.; et al. An Organoid-Based Organ-Repurposing Approach to Treat Short Bowel Syndrome. Nature 2021, 592, 99–104.
- Huang, J.; Xu, Z.; Ren, J. Intestinalization Small of Colon Using Ileum Organoids. Trends Cell Biol. 2021, 31, 517–519.
- Sugimoto, S.; Kobayashi, E.; Kanai, T.; Sato, T. In Vivo Intestinal Research Using Organoid Transplantation. Keio J. Med. 2022, 71, 73–81.
- Kobayashi, E.A. New stage of experimental surgery for organoid based intestinal regeneration—A review of or-ganoid research and recent advance. Magy. Seb. 2022, 75, 261–264.
- Nightingale, J.; Woodward, J.M. Small Bowel and Nutrition Committee of the British Society of Gastroenterology Guidelines for management of patients with a short bowel. Gut 2006, 55 (Suppl. S4), iv1–iv12.
- Khalaf, R.T.; Sokol, R.J. New Insights into Intestinal Failure-Associated Liver Disease in Children. Hepatology 2020, 71, 1486–1498.
- Lacaille, F.; Gupte, G.; Colomb, V.; D’Antiga, L.; Hartman, C.; Hojsak, I.; Kolacek, S.; Puntis, J.; Shamir, R. Intestinal failure associated liver disease: A position paper of the ESPGHAN Working Group of Intestinal Failure and Intestinal Transplantation. J. Pediatr. Gastroenterol. Nutr. 2015, 60, 272–283.
- Secor, J.D.; Yu, L.; Tsikis, S.; Fligor, S.; Puder, M.; Gura, K.M. Current strategies for managing intestinal failure-associated liver disease. Expert Opin. Drug Saf. 2021, 20, 307–320.
- Buchman, A.L.; Scolapio, J.; Fryer, J. AGA technical review on short bowel syndrome and intestinal transplantation. Gastroenterology 2003, 124, 1111–1134.
- Kaufman, S.S.; Atkinson, J.B.; Bianchi, A.; Goulet, O.J.; Grant, D.; Langnas, A.N.; McDiarmid, S.V.; Mittal, N.; Reyes, J.; Tzakis, A.G. American Society of Transplantation. Indications for pediatric intestinal transplantation: A position paper of the American Society of Transplantation. Pediatr. Transpl. 2001, 5, 80–87.
- Pironi, L.; Arends, J.; Bozzetti, F.; Cuerda, C.; Gillanders, L.; Jeppesen, P.B.; Joly, F.; Kelly, D.; Lal, S.; Staun, M.; et al. Home Artificial Nutrition & Chronic Intestinal Failure Special Interest Group of ESPEN. ESPEN guidelines on chronic intestinal failure in adults. Clin. Nutr. 2016, 35, 247–307.
- Pironi, L.; Cuerda, C.; Jeppesen, P.B.; Joly, F.; Jonkers, C.; Krznarić, Ž.; Lal, S.; Lamprecht, G.; Lichota, M.M.; Mundi, M.S.; et al. ESPEN guideline on chronic intestinal failure in adults—Update 2023. Clin. Nutr. 2023, 42, 1940–2021.
- Lal, S.; Pironi, L.; Wanten, G.; Arends, J.; Bozzetti, F.; Cuerda, C.; Joly, F.; Kelly, D.; Staun, M.; Szczepanek, K.; et al. Clinical approach to the management of Intestinal Failure Associated Liver Disease (IFALD) in adults: A position paper from the Home Artificial Nutrition and Chronic Intestinal Failure Special Interest Group of ESPEN. Clin. Nut 2018, 37 Pt A, 1794–1797.
- Bettag, J.; Po, L.; Cunningham, C.; Tallam, R.; Kurashima, K.; Nagarapu, A.; Hutchinson, C.; Morfin, S.; Nazzal, M.; Lin, C.; et al. Novel Therapeutic Approaches for Mitigating Complications in Short Bowel Syndrome. Nutrients 2022, 14, 4660.
More
Information
Subjects:
Nutrition & Dietetics
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.4K
Entry Collection:
Gastrointestinal Disease
Revisions:
2 times
(View History)
Update Date:
22 Jan 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No