
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Massimo Iacoviello | -- | 4573 | 2023-10-27 17:05:10 | | | |
| 2 | Lindsay Dong | Meta information modification | 4573 | 2023-10-30 01:48:11 | | |
Video Upload Options
The relevance of genetics in cardiovascular diseases has expanded, especially in the context of cardiomyopathies. Its relevance extends to the management of patients diagnosed with heart failure (HF), given its capacity to provide invaluable insights into the etiology of cardiomyopathies and identify individuals at a heightened risk of poor outcomes. Notably, the identification of an etiological genetic variant necessitates a comprehensive evaluation of the family lineage of the affected patients. In the future, these genetic variants hold potential as therapeutic targets with the capability to modify gene expression.
1. Introduction
2. Advancements and Applications of Genetics in Cardiovascular Disease
2.1. Assessment of Pathogenic Genetic Variants
-
TGP (targeted gene panel): this method examines genes linked to a specific phenotype. However, its scope is primarily confined to selected genes known for their variants, necessitating ongoing updates. The process entails designing a gene panel correlated with a distinct disease and conducting parallel sequencing. It is commonly employed as the primary diagnostic test for probands [12][20].
-
WES: this method is adept at diagnosing probands presenting with diverse disorders, including pediatric and syndromic cardiomyopathies. It encompasses all genes with the objective of sequencing the complete exome. Through an integrated process, data corresponding to the entire exome can be produced, eliminating the need for additional analyses when updated information becomes available [21][22].
-
Whole-genome sequencing (WGS): this technique sequences the complete genome, offering diagnostic insights for probands with varied disorders and detailed data on pharmacokinetic variants. While comprehensive, WGS comes with a greater expense and necessitates intricate data analysis. If panel sequencing yields negative results, both WES and WGS stand as viable subsequent diagnostic options [23].
2.1.1. Sequencing Modalities
-
Presequencing panels (targeted resequencing): this approach enables the simultaneous analysis of multiple patients by selectively enriching specific genomic regions prior to sequencing.
-
In silico panels (targeted data analysis): this method is applied after exome sequencing and focuses on genes directly associated with the disease under investigation, generally allowing for the analysis of a restricted number of samples in each run [25].
- -
-
Cost: The difference in cost is influenced by the reagents used. The use of TGP is more economical if the number of samples per run is optimized. In economic terms, WGS is the most expensive, and although WES is pricier than panels, it can be advantageous depending on the type of study to be performed [27].
- -
-
Purpose: Typically, NGS techniques are employed for diseases with high genetic heterogeneity or Mendelian-based genetic diseases (or those suspected to be genetic) where the causative genes remain unidentified. For diseases with established genetic etiology, either custom-designed panels, WES, or WGS can be utilized [26].
- -
-
Sensitivity: Sensitivity largely depends on the coverage of the sequences under investigation, that is, the number of reads for specific DNA sections and the overlap extent between these reads. A greater number of reads for a specific region translates to higher sensitivity for that DNA segment [26]. During panel analysis, a reduced genome proportion under investigation leads to enhanced coverage and sensitivity. Thus, if a disease is believed to result from a mosaic genomic alteration, NGS panel analysis offers higher sensitivity compared to WES.
- -
-
IFs and VUSs: The probability of identifying IFs and VUSs depends on the genome proportion both analyzed and queried. Analysis based on panels has a reduced association with IFs, since the investigated sequences are directly relevant to the clinical presentation of the proband. In general, a broader sequence analysis correlates with a higher number of IFs and VUSs.
- -
-
Data storage: The extent of the genome analyzed directly influences the volume of data generated. Consequently, suitable platforms for data storage are essential, particularly for analyses yielding substantial data, such as those conducted via WES and, more prominently, WGS [26].
2.1.2. Identification and Interpretation of Pathogenic Genetic Variants in Clinical Diagnostics
-
Their allele frequency within the general population;
2.2. Variants of Uncertain Significance (VUS)
CardioBoost uses a disease-specific variant classifier algorithm tailored to predict the pathogenicity of missense variants linked to inherited cardiomyopathies and arrhythmias. One of its distinct advantages is that, when focused on heart disease, this specific variant classifier surpasses the performance of leading whole-genome tools. This superiority underscores the significant potential for improved pathogenicity predictions through disease-specific approaches [35]. On the other hand, some tools harness detailed structural information about proteins, examining how mutations might affect protein folding and stability to make their pathogenicity predictions [34].
2.3. Classification, Implications, and Clinical Utility of Genetic Variants in Cardiovascular Disease
2.4. Diagnosis and Counseling
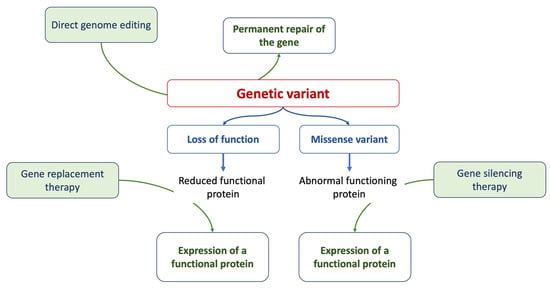
2.5. Gene Therapy
3. Genetics, Cardiomyopathies, and Heart Failure
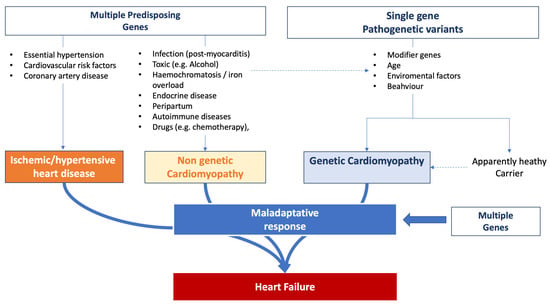
3.1. Genetic Factors Predisposing to Heart Failure
3.2. Genetics in Assessing the Risk of Heart Failure Progression
3.3. Arrhythmic Risk Stratification
3.4. Implications of Genetic Variants in Clinical Decisions
4. Heart Failure and Genetics
References
- Shah, R.A.; Asatryan, B.; Sharaf Dabbagh, G.; Aung, N.; Khanji, M.Y.; Lopes, L.R.; Van Duijvenboden, S.; Holmes, A.; Muser, D.; Landstrom, A.P.; et al. Genotype-first approach I. Frequency, penetrance, and variable expressivity of dilated cardiomyopathy-associated putative pathogenic gene variants in UK Biobank participants. Circulation 2022, 146, 110–124.
- De Marvao, A.; McGurk, K.A.; Zheng, S.L.; Thanaj, M.; Bai, W.; Duan, J.; Biffi, C.; Mazzarotto, F.; Statton, B.; Dawes, T.J.W.; et al. Phenotypic expression and outcomes in individuals with rare genetic variants of hypertrophic cardiomyopathy. J. Am. Coll. Cardiol. 2021, 78, 1097–1110.
- McGurk, K.A.; Zheng, S.L.; Henry, A.; Josephs, K.; Edwards, M.; De Marvao, A.; Whiffin, N.; Roberts, A.; Lumbers, T.R.; O’Regan, D.P.; et al. Correspondence on “ACMG SF v3.0 list for reporting of secondary findings in clinical exome and genome sequencing: A policy statement of the American College of Medical Genetics and Genomics (ACMG)” by Miller et al. Genet. Med. 2022, 24, 744–746.
- Wahbi, K.; Ben Yaou, R.; Gandjbakhch, E.; Anselme, F.; Gossios, T.; Lakdawala, N.K.; Stalens, C.; Sacher, F.; Babuty, D.; Trochu, J.N.; et al. Development and validation of a new risk prediction score for life-threatening ventricular tachyarrhythmias in laminopathies. Circulation 2019, 140, 293–302.
- Van Rijsingen, I.A.; Arbustini, E.; Elliott, P.M.; Mogensen, J.; Hermans-van Ast, J.F.; Van Der Kooi, A.J.; Van Tintelen, J.P.; Van den Berg, M.P.; Pilotto, A.; Pasotti, M.; et al. Risk factors for malignant ventricular arrhythmias in lamin A/C mutation carriers a European cohort study. J. Am. Coll. Cardiol. 2012, 59, 493–500.
- Bozkurt, B.; Coats, A.J.; Tsutsui, H.; Abdelhamid, M.; Adamopoulos, S.; Albert, N.; Anker, S.D.; Atherton, J.; Böhm, M.; Butler, J.; et al. Universal definition and classification of heart failure: A report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure. J. Card Fail. 2021, 27, 387–413.
- Conrad, D.F.; Keebler, J.E.; DePristo, M.A.; Lindsay, S.J.; Zhang, Y.; Casals, F.; Idaghdour, Y.; Hartl, C.L.; Torroja, C.; Garimella, K.V.; et al. Variation in genome-wide mutation rates within and between human families. Nat. Genet. 2011, 43, 712–714.
- 1000 Genomes Project Consortium; Abecasis, G.R.; Altshuler, D.; Auton, A.; Brooks, L.D.; Durbin, R.M.; Gibbs, R.A.; Hurles, M.E.; McVean, G. A map of human genome variation from population-scale sequencing. Nature 2010, 467, 1061–1073.
- Choi, M.; Scholl, U.I.; Ji, W.; Liu, T.; Tikhonova, I.R.; Zumbo, P.; Nayir, A.; Bakkaloğlu, A.; Ozen, S.; Sanjad, S.; et al. Genetic diagnosis by whole exome capture and massively parallel DNA sequencing. Proc. Natl. Acad. Sci. USA 2009, 106, 19096–19101.
- Claussnitzer, M.; Cho, J.H.; Collins, R.; Cox, N.J.; Dermitzakis, E.T.; Hurles, M.E.; Kathiresan, S.; Kenny, E.E.; Lindgren, C.M.; MacArthur, D.G.; et al. A brief history of human disease genetics. Nature 2020, 577, 179–189.
- Visser, M.; Dooijes, D.; van der Smagt, J.J.; van der Heijden, J.F.; Doevendans, P.A.; Loh, P.; Asselbergs, F.W.; Hassink, R.J. Next-generation sequencing of a large gene panel in patients initially diagnosed with idiopathic ventricular fibrillation. Heart Rhythm 2017, 14, 1035–1040.
- Chaisson, M.J.P.; Sanders, A.D.; Zhao, X.; Malhotra, A.; Porubsky, D.; Rausch, T.; Gardner, E.J.; Rodriguez, O.L.; Guo, L.; Collins, R.L.; et al. Multi-platform discovery of haplotype-resolved structural variation in human genomes. Nat. Commun. 2019, 10, 1784.
- Alkan, C.; Coe, B.P.; Eichler, E.E. Genome structural variation discovery and genotyping. Nat. Rev. Genet. 2011, 12, 363–376.
- Sanger, F.; Nicklen, S.; Coulson, A.R. DNA sequencing with chain-terminating inhibitors. Proc. Natl. Acad. Sci. USA 1977, 74, 5463–5467.
- Bagnall, R.D.; Weintraub, R.G.; Ingles, J.; Duflou, J.; Yeates, L.; Lam, L.; Davis, A.M.; Thompson, T.; Connell, V.; Wallace, J.; et al. A prospective study of sudden cardiac death among children and young adults. N. Engl. J. Med. 2016, 374, 2441–2452.
- Margulies, M.; Egholm, M.; Altman, W.E.; Attiya, S.; Bader, J.S.; Bemben, L.A.; Berka, J.; Braverman, M.S.; Chen, Y.J.; Chen, Z.; et al. Genome sequencing in microfabricated high-density picolitre reactors. Nature 2005, 437, 376–380.
- Bentley, D.R.; Balasubramanian, S.; Swerdlow, H.P.; Smith, G.P.; Milton, J.; Brown, C.G.; Hall, K.P.; Evers, D.J.; Barnes, C.L.; Bignell, H.R.; et al. Accurate whole human genome sequencing using reversible terminator chemistry. Nature 2008, 456, 53–59.
- Haas, J.; Frese, K.S.; Peil, B.; Kloos, W.; Keller, A.; Nietsch, R.; Feng, Z.; Müller, S.; Kayvanpour, E.; Vogel, B.; et al. Atlas of the clinical genetics of human dilated cardiomyopathy. Eur. Heart J. 2015, 36, 1123–1135.
- Michels, V.V.; Moll, P.P.; Miller, F.A.; Tajik, A.J.; Chu, J.S.; Driscoll, D.J.; Burnett, J.C.; Rodeheffer, R.J.; Chesebro, J.H.; Tazelaar, H.D. The frequency of familial dilated cardiomyopathy in a series of patients with idiopathic dilated cardiomyopathy. N. Engl. J. Med. 1992, 326, 77–82.
- Whiffin, N.; Karczewski, K.J.; Zhang, X.; Chothani, S.; Smith, M.J.; Evans, D.G.; Roberts, A.M.; Quaife, N.M.; Schafer, S.; Rackham, O.; et al. Characterizing the loss-of-function impact of 5’ untranslated region variants in 15,708 individuals. Nat. Commun. 2020, 11, 2523.
- Schwartz, P.J.; Crotti, L.; George, A.L., Jr. Modifier genes for sudden cardiac death. Eur. Heart J. 2018, 39, 3925–3931.
- Kalia, S.S.; Adelman, K.; Bale, S.J.; Chung, W.K.; Eng, C.; Evans, J.P.; Herman, G.E.; Hufnagel, S.B.; Klein, T.E.; Korf, B.R.; et al. Recommendations for reporting of secondary findings in clinical exome and genome sequencing, 2016 update (ACMG SF v2.0): A policy statement of the American College of Medical Genetics and Genomics. Genet. Med. 2017, 19, 249–255.
- Hanchard, N.A.; Umana, L.A.; D’Alessandro, L.; Azamian, M.; Poopola, M.; Morris, S.A.; Fernbach, S.; Lalani, S.R.; Towbin, J.A.; Zender, G.A.; et al. Assessment of large copy number variants in patients with apparently isolated congenital left-sided cardiac lesions reveals clinically relevant genomic events. Am. J. Med. Genet. A 2017, 173, 2176–2188.
- LaFramboise, T. Single nucleotide polymorphism arrays: A decade of biological, computational and technological advances. Nucleic Acids Res. 2009, 37, 4181–4193.
- Giudicessi, J.R.; Lieve, K.V.V.; Rohatgi, R.K.; Koca, F.; Tester, D.J.; van der Werf, C.; Martijn Bos, J.; Wilde, A.A.M.; Ackerman, M.J. Assessment and validation of a phenotype-enhanced variant classification framework to promote or demote RYR2 missense variants of uncertain significance. Circ. Genom. Precis. Med. 2019, 12, e002510.
- Biesecker, L.G.; Green, R.C. Diagnostic clinical genome and exome sequencing. N. Engl. J. Med. 2014, 370, 2418–2425.
- Seleman, M.; Hoyos-Bachiloglu, R.; Geha, R.S.; Chou, J. Uses of Next-Generation Sequencing Technologies for the Diagnosis of Primary Immunodeficiencies. Front. Immunol. 2017, 8, 847.
- Available online: https://www.ncbi.nlm.nih.gov/clinvar/ (accessed on 15 September 2023).
- Available online: https://www.omim.org (accessed on 15 September 2023).
- Available online: http://genetics.bwh.harvard.edu/pph2/ (accessed on 15 September 2023).
- Available online: https://www.mutationtaster.org (accessed on 15 September 2023).
- Available online: https://www.jcvi.org/research/provean (accessed on 15 September 2023).
- Richards, S.; Aziz, N.; Bale, S.; Bick, D.; Das, S.; Gastier-Foster, J.; Grody, W.W.; Hegde, M.; Lyon, E.; Spector, E.; et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 2015, 17, 405–424.
- Doh, C.Y.; Kampourakis, T.; Campbell, K.S.; Stelzer, J.E. Basic science methods for the characterization of variants of uncertain significance in hypertrophic cardiomyopathy. Front. Cardiovasc. Med. 2023, 10, 1238515.
- Zhang, X.; Walsh, R.; Whiffin, N.; Buchan, R.; Midwinter, W.; Wilk, A.; Govind, R.; Li, N.; Ahmad, M.; Mazzarotto, F.; et al. Disease-specific variant pathogenicity prediction significantly improves variant interpretation in inherited cardiac conditions. Genet. Med. 2021, 23, 69–79.
- Wong, E.K.; Bartels, K.; Hathaway, J.; Burns, C.; Yeates, L.; Semsarian, C.; Krahn, A.D.; Virani, A.; Ingles, J. Perceptions of genetic variant reclassification in patients with inherited cardiac disease. Eur. J. Hum. Genet. 2019, 27, 1134–1142.
- Ingles, J.; McGaughran, J.; Scuffham, P.A.; Atherton, J.; Semsarian, C. A cost-effectiveness model of genetic testing for the evaluation of families with hypertrophic cardiomyopathy. Heart 2012, 98, 625–630.
- Ingles, J.; Yeates, L.; O’Brien, L.; McGaughran, J.; Scuffham, P.A.; Atherton, J.; Semsarian, C. Genetic testing for inherited heart diseases: Longitudinal impact on health-related quality of life. Genet. Med 2012, 14, 749–752.
- Lambert, S.A.; Gil, L.; Jupp, S.; Ritchie, S.C.; Xu, Y.; Buniello, A.; McMahon, A.; Abraham, G.; Chapman, M.; Parkinson, H.; et al. The Polygenic Score Catalog as an open database for reproducibility and systematic evaluation. Nat. Genet. 2021, 53, 420–425.
- Lahrouchi, N.; Tadros, R.; Crotti, L.; Mizusawa, Y.; Postema, P.G.; Beekman, L.; Walsh, R.; Hasegawa, K.; Barc, J.; Ernsting, M.; et al. Transethnic genome-wide association study provides insights in the genetic architecture and heritability of long QT syndrome. Circulation 2020, 142, 324–338.
- Harper, A.R.; Goel, A.; Grace, C.; Thomson, K.L.; Petersen, S.E.; Xu, X.; Waring, A.; Ormondroyd, E.; Kramer, C.M.; Ho, C.Y.; et al. HCMR Investigators. Common genetic variants and modifiable risk factors underpin hypertrophic cardiomyopathy susceptibility and expressivity. Nat. Genet. 2021, 53, 135–142.
- Tadros, R.; Tan, H.L.; ESCAPE-NET Investigators; El Mathari, S.; Kors, J.A.; Postema, P.G.; Lahrouchi, N.; Beekman, L.; Radivojkov-Blagojevic, M.; Amin, A.S.; et al. Predicting cardiac electrical response to sodiumchannel blockade and Brugada syndrome using polygenic risk scores. Eur. Heart J. 2019, 40, 3097–3107.
- Turkowski, K.L.; Dotzler, S.M.; Tester, D.J.; Giudicessi, J.R.; Bos, J.M.; Speziale, A.D.; Vollenweider, J.M.; Ackerman, M.J. Corrected QT interval-polygenic risk score and its contribution to type 1, type 2, and type 3 long-QT syndrome in probands and genotype-positive family members. Circ. Genom. Precis. Med. 2020, 13, e002922.
- Connolly, S.J.; Hallstrom, A.P.; Cappato, R.; Schron, E.B.; Kuck, K.H.; Zipes, D.P.; Greene, H.L.; Boczor, S.; Domanski, M.; Follmann, D.; et al. Meta-analysis of the implantable cardioverter defibrillator secondary prevention trials. Eur. Heart J. 2000, 21, 2071–2078.
- Chivulescu, M.; Lie, Ø.H.; Popescu, B.A.; Skulstad, H.; Edvardsen, T.; Jurcut, R.O.; Haugaa, K.H. High penetrance and similar disease progression in probands and in family members with arrhythmogenic cardiomyopathy. Eur. Heart J. 2020, 41, 1401–1410.
- Cardim, N.; Freitas, A.; Brito, D. From hypertrophic cardiomyopathy centers to inherited cardiovascular disease centers in Europe. A small or a major step? A position paper from the Nucleus of the Working Group on Myocardial and Pericardial Diseases of the Portuguese Society of Cardiology. Rev. Port. Cardiol. 2011, 30, 829–835.
- Barriales-Villa, R.; Gimeno-Blanes, J.R.; Zorio-Grima, E.; Ripoll-Vera, T.; Evangelista-Masip, A.; Moya-Mitjans, A.; Serratosa-Fernández, L.; Albert-Brotons, D.C.; García-Pinilla, J.M.; García-Pavía, P. Plan of action for inherited cardiovascular diseases: Synthesis of recommendations and action algorithms. Rev. Esp. Cardiol. 2016, 69, 300–309.
- Edwards, A.; Gray, J.; Clarke, A.; Dundon, J.; Elwyn, G.; Gaff, C.; Hood, K.; Iredale, R.; Sivell, S.; Shaw, C.; et al. Interventions to improve risk communication in clinical genetics: Systematic review. Patient Educ. Couns. 2008, 71, 4–25.
- Whyte, S.; Green, A.; McAllister, M.; Shipman, H. Family communication in inherited cardiovascular conditions in Ireland. J. Genet. Couns. 2016, 25, 1317–1326.
- Daly, M.B.; Montgomery, S.; Bingler, R.; Ruth, K. Communicating genetic test results within the family: Is it lost in translation? A survey of relatives in the randomized six-step study. Fam. Cancer 2016, 15, 697–706.
- Kaphingst, K.A.; Blanchard, M.; Milam, L.; Pokharel, M.; Elrick, A.; Goodman, M.S. Relationships between health literacy and genomics-related knowledge, self-efficacy, perceived importance, and communication in a medically underserved population. J. Health Commun. 2016, 21, 58–68.
- de Boer, R.A.; Heymans, S.; Backs, J.; Carrier, L.; Coats, A.J.S.; Dimmeler, S.; Eschenhagen, T.; Filippatos, G.; Gepstein, L.; Hulot, J.S.; et al. Targeted therapies in genetic dilated and hypertrophic cardiomyopathies: From molecular mechanisms to therapeutic targets. A position paper from the Heart Failure Association (HFA) and the Working Group on Myocardial Function of the European Society of Cardiology (ESC). Eur. J. Heart Fail. 2022, 24, 406–420.
- Anzalone, A.V.; Koblan, L.W.; Liu, D.R. Genome editing with CRISPR-Cas nucleases, base editors, transposases and prime editors. Nat. Biotechnol. 2020, 38, 824–844.
- Fomin, A.; Gärtner, A.; Cyganek, L.; Tiburcy, M.; Tuleta, I.; Wellers, L.; Folsche, L.; Hobbach, A.J.; von Frieling-Salewsky, M.; Unger, A.; et al. Truncated titin proteins and titin haploinsufficiency are targets for functional recovery in human cardiomyopathy due to TTN mutations. Sci. Transl. Med. 2021, 13, eabd3079.
- Hinson, J.T.; Chopra, A.; Nafissi, N.; Polacheck, W.J.; Benson, C.C.; Swist, S.; Gorham, J.; Yang, L.; Schafer, S.; Sheng, C.C.; et al. Titin mutations in iPS cells define sarcomere insufficiency as a cause of dilated cardiomyopathy. Science 2015, 349, 982–986.
- Hershberger, R.E.; Hedges, D.J.; Morales, A. Dilated cardiomyopathy: The complexity of a diverse genetic architecture. Nat. Rev. Cardiol. 2013, 10, 531–547.
- Lee, D.S.; Pencina, M.J.; Benjamin, E.J.; Wang, T.J.; Levy, D.; O’Donnell, C.J.; Nam, B.H.; Larson, M.G.; D’Agostino, R.B.; Vasan, R.S. Association of parental heart failure with risk of heart failure in offspring. N. Engl. J. Med. 2006, 355, 138–147.
- Teekakirikul, P.; Zhu, W.; Huang, H.C.; Fung, E. Hypertrophic Cardiomyopathy: An Overview of Genetics and Management. Biomolecules 2019, 9, 878.
- Yousaf, M.; Khan, W.A.; Shahzad, K.; Khan, H.N.; Ali, B.; Hussain, M.; Awan, F.R.; Mustafa, H.; Sheikh, F.N. Genetic Association of Beta-Myosin Heavy-Chain Gene (MYH7) with Cardiac Dysfunction. Genes 2022, 13, 1554.
- Tudurachi, B.S.; Zăvoi, A.; Leonte, A.; Țăpoi, L.; Ureche, C.; Bîrgoan, S.G.; Chiuariu, T.; Anghel, L.; Radu, R.; Sascău, R.A.; et al. An Update on MYBPC3 Gene Mutation in Hypertrophic Cardiomyopathy. Int. J. Mol. Sci. 2023, 24, 10510.
- Velicki, L.; Jakovljevic, D.G.; Preveden, A.; Golubovic, M.; Bjelobrk, M.; Ilic, A.; Stojsic, S.; Barlocco, F.; Tefelmeier, M.; Okwose, N.; et al. Genetic determinants of clinical phenotype in hypertrophic cardiomyopathy. BMC Cardiovasc. Disord. 2020, 20, 516.
- Herrera-Rodríguez, D.L.; Totomoch-Serra, A.; Rosas-Madrigal, S.; Luna-Limón, C.; Marroquín-Ramírez, D.; Carnevale, A.; Rosendo-Gutiérrez, R.; Villarreal-Molina, M.T.; Márquez-Murillo, M.F. Genes frequently associated with sudden death in primary hypertrophic cardiomyopathy. Arch. Cardiol. Mex. 2020, 90, 58–68.
- Christensen, A.H.; Platonov, P.G.; Jensen, H.K.; Chivulescu, M.; Svensson, A.; Dahlberg, P.; Madsen, T.; Frederiksen, T.C.; Heliö, T.; Lie, Ø.H.; et al. Genotype-phenotype correlation in arrhythmogenic right ventricular cardiomyopathy-risk of arrhythmias and heart failure. J. Med. Genet. 2022, 59, 858–864.
- De Backer, J.; Narula, J. Cardiolaminopathies: Weighing in on the Concept of Genotype-First Screening. J. Am. Coll. Cardiol. 2022, 80, 60–62.
- Arbelo, E.; Protonotarios, A.; Gimeno, J.R.; Arbustini, E.; Barriales-Villa, R.; Basso, C.; Bezzina, C.R.; Biagini, E.; Blom, N.A.; de Boer, R.A.; et al. 2023 ESC Guidelines for the management of cardiomyopathies: Developed by the task force on the management of cardiomyopathies of the European Society of Cardiology (ESC). Eur. Heart J. 2023, 44, 3503–3626.
- Zeppenfeld, K.; Tfelt-Hansen, J.; de Riva, M.; Winkel, B.G.; Behr, E.R.; Blom, N.A.; Charron, P.; Corrado, D.; Dagres, N.; de Chillou, C.; et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur. Heart J. 2022, 43, 3997–4126.
- Kumar, S.; Baldinger, S.H.; Gandjbakhch, E.; Maury, P.; Sellal, J.M.; Androulakis, A.F.; Waintraub, X.; Charron, P.; Rollin, A.; Richard, P.; et al. Long-term arrhythmic and nonarrhythmic outcomes of lamin A/C mutation carriers. J. Am. Coll. Cardiol. 2016, 68, 2299–2307.
- Verstraelen, T.E.; van Lint, F.H.M.; Bosman, L.P.; de Brouwer, R.; Proost, M.V.; Abeln, B.G.S.; Taha, K.; Zwinderman, A.H.; Dickhoff, C.; Oomen, T.; et al. Prediction of ventricular arrhythmia in phospholamban p.Arg14del mutation carriersreaching the frontiers of individual risk prediction. Eur. Heart J. 2021, 42, 2842–2850.
- Mirelis, J.G.; Escobar-Lopez, L.; Ochoa, J.P.; Espinosa, M.Á.; Villacorta, E.; Navarro, M.; Casas, G.; Mora-Ayestarán, N.; Barriales-Villa, R.; Mogollón-Jiménez, M.V.; et al. Combination of late gadolinium enhancement and genotype improves prediction of prognosis in non-ischaemic dilated cardiomyopathy. Eur. J. Heart Fail. 2022, 24, 1183–1196.
- Ader, F.; De Groote, P.; Réant, P.; Rooryck-Thambo, C.; Dupin-Deguine, D.; Rambaud, C.; Khraiche, D.; Perret, C.; Pruny, J.F.; Mathieu-Dramard, M.; et al. FLNC pathogenic variants in patients with cardiomyopathies: Prevalence and genotype-phenotype correlations. Clin. Genet. 2019, 96, 317–329.
- de Frutos, F.; Ochoa, J.; Navarro-Peñalver, M.; Peñalver, M.; Baas, A.; Bjerre, J.V.; Zorio, E.; Méndez, I.; Lorca, R.; Verdonschot, J.A.J.; et al. Natural History of MYH7-Related Dilated Cardiomyopathy. J. Am. Coll. Cardiol. 2022, 80, 1447–1461.
- Gimeno, J.R.; Tomé-Esteban, M.; Lofiego, C.; Hurtado, J.; Pantazis, A.; Mist, B.; Lambiase, P.; McKenna, W.J.; Elliott, P.M. Exercise-induced ventricular arrhythmias and risk of sudden cardiac death in patients with hypertrophic cardiomyopathy. Eur. Heart J. 2009, 30, 2599–2605.
- Cooper, L.T., Jr.; Čiháková, D. Do Genes Influence Susceptibility to Myocarditis? JACC Basic. Transl. Sci. 2021, 6, 593–594.
- Fox, C.S.; Evans, J.C.; Larson, M.G.; Kannel, W.B.; Levy, D. Temporal trends in coronary heart disease mortality and sudden cardiac death from 1950 to 1999: The Framingham Heart Study. Circulation 2004, 110, 522–527.
- Lloyd-Jones, D.M.; Wilson, P.W.F. Framingham risk score and prediction of lifetime risk for coronary heart disease. Am. J. Cardiol. 2004, 94, 20–24.
- Skrzynia, C.; Berg, J.S.; Willis, M.S.; Jensen, B.C. Genetics and heart failure: A concise guide for the clinician. Curr. Cardiol. Rev. 2015, 11, 10–17.




