Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Ika Dewi Ana | -- | 4000 | 2023-04-27 17:23:29 | | | |
| 2 | Conner Chen | + 4 word(s) | 4004 | 2023-05-04 02:26:33 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Ana, I.D.; Sarasati, A.; Syahruddin, M.H.; Nuryanti, A.; Barlian, A.; Wijaya, C.H.; Ratnadewi, D.; Wungu, T.D.K.; Takemori, H. Plant-Derived Exosome-like Nanoparticle as Biomolecules. Encyclopedia. Available online: https://encyclopedia.pub/entry/43585 (accessed on 07 February 2026).
Ana ID, Sarasati A, Syahruddin MH, Nuryanti A, Barlian A, Wijaya CH, et al. Plant-Derived Exosome-like Nanoparticle as Biomolecules. Encyclopedia. Available at: https://encyclopedia.pub/entry/43585. Accessed February 07, 2026.
Ana, Ika Dewi, Andari Sarasati, Muhammad Hidayat Syahruddin, Archadian Nuryanti, Anggraini Barlian, Christofora Hanny Wijaya, Diah Ratnadewi, Triati Dewi Kencana Wungu, Hiroshi Takemori. "Plant-Derived Exosome-like Nanoparticle as Biomolecules" Encyclopedia, https://encyclopedia.pub/entry/43585 (accessed February 07, 2026).
Ana, I.D., Sarasati, A., Syahruddin, M.H., Nuryanti, A., Barlian, A., Wijaya, C.H., Ratnadewi, D., Wungu, T.D.K., & Takemori, H. (2023, April 27). Plant-Derived Exosome-like Nanoparticle as Biomolecules. In Encyclopedia. https://encyclopedia.pub/entry/43585
Ana, Ika Dewi, et al. "Plant-Derived Exosome-like Nanoparticle as Biomolecules." Encyclopedia. Web. 27 April, 2023.
Copy Citation
Plant-derived exosome-like nanoparticles (PDENs) comprise various bioactive biomolecules. As an alternative cell-free therapeutic approach, they have the potential to deliver nano-bioactive compounds to the human body, and thus lead to various anti-inflammatory, antioxidant, and anti-tumor benefits.
plant-derived exosome-like nanoparticles (PDENs)
biomedical application
regenerative therapy
1. Introduction
From a biomedical science perspective, a human tissue is a cellular hybrid system between cells and the complete organ [1]. Human tissue is an orchestrated organization composed of cells and their extracellular matrix (ECM) with specific composition and architecture, which carries out a specific function. Functional grouping of multiple tissues forms organs, in which a human body system is organized from an atomic scale, to molecular, macromolecular, organelle, cell, tissue, organ, and up to organ system scales. In the case of an injured, damaged, or missing tissue in the body, constructive remodeling and regenerative therapy are needed to provide engineered ECM with specific structural, mechanical, physical, and chemical properties that closely approximate to the replaced native tissue, which enables the remaining cells to attach, migrate, proliferate, differentiate, and regenerate for structural and functional replacement of the targeted tissue or organ [2][3][4]. This is the fundamental principle of tissue engineering.
In the framework of tissue engineering, the use of stem cells to increase tissue regenerative capacity has attracted scientists, especially mesenchymal stem cells (MSCs), due to the fact that their defining properties make them an ideal candidate to cure diseases. Although embryonic and fetal stem cells have the greatest potential to differentiate into different cell types, their application is limited due to ethical and safety issues [5][6][7][8][9][10], as well as the danger of unlimited and uncontrolled cells division [7][8][10][11][12][13][14][15]. Furthermore, the inherent heterogenicity and variation associated with cell expansion has become a major MSC limit for its clinical applications [16][17][18][19][20]. In addition, during in vitro cell processing and expansion, changes may occur to MSCs, thereby increasing the risk of MSC therapeutic application. Moreover, the risk of unwanted differentiation in vivo is a problem due to its clinical applications. This leads to alternative cell-free-based therapy with biomolecules secreted from MSCs, which are known as MSC-derived exosomes.
Extensive research has been carried out to identify the molecules involved in paracrine action of stem cells (SCs) for the opening of new therapeutic options in the concept of cell-free-based therapy. At this point, exosomes are nano-sized vesicular particles commonly secreted from eukaryotic cells into the extracellular space, and are intensively investigated as candidate therapeutic agents. These exosomes have known functions in cellular communication [19][20][21][22], nutrients [21][22], bioactive compounds delivery [19][20][22], and cellular immunity [19][20][22]. However, currently, there is no standardized procedure for the isolation, storage, and manufacturing of technology using a quality system for the safety of both donors and recipients in large-scale valorization of MSC-derived exosomes [19]. In the case of manufacturing, for instance, although extensive research has been conducted, the practical use of exosomes is still restricted by the limited exosome secretion capability of cells.
2. Plant-Derived Exosome-like Nanoparticle as Biomolecules
Exosomes were discovered in 1983 by Eberhard Trams and Rose Johnstone [23][24]. Exosomes are biologically small, nano-sized extracellular vesicles (EVs) with a diameter of 30–150 nm and density of 1.13–1.19 g/mL, secreted naturally by almost all eukaryotic cells [25][26][27][28][29][30][31]. Exosomes are important since these vesicles are similar to cargo-containing molecular components, such as DNA, RNA, lipid, and proteins, which are later released into the extracellular matrix as a form of intercellular communication [32][33][34]. Several studies have shown that exosomes comprise cytokines, transcription factor receptors, and other bioactive compounds [35][36].
The exact mechanism of exosome biogenesis remains controversial; however, they are generally synthesized in the multivesicular endosome compartments of the cell and released when these compartments fuse with the plasma membrane. Therefore, exosomes are also known as membrane-bound or membrane-derived vesicles [26][37][38][39]. Formerly, these exosomes were referred to as “ectosomes”, “shed vesicles”, and “small extracellular vesicles (sEVs)”. To date, however, the term “exosome” has received the most popularity [40][41][42]. In comparison to micro vesicles, apoptotic bodies, and oncosomes, exosomes are the smallest type of EVs [32][43][44][45].
Research proved EVs, such as exosomes, comprise their own specific cargo. This cargo becomes crucial since it represents the health and/or disease status of the source or parent cells, which has the capacity to alter recipient cells, both neighboring and distantly located ones, by adhering to the cell membrane and releasing its internal cargo. The release of this internal load induces physiological, phenotypic, and functional changes in the recipient cells [26][46][47][48][49][50]. These findings boost numerous investigations into the role of exosomes as novel biomarkers and potential therapeutic agents, which demonstrate that exosomes, as mediators of cell-to-cell communication, are related to physiological and pathological processes on the smallest scale, particularly between cells that occur in the living system [51][52].
Exosomes are divided into two categories: Natural and engineered exosomes. Natural exosomes are animal derived, mostly from mammals, and originate from cells [53][54][55][56] or biofluids [57][58][59][60], and plants as natural resources. Figure 1 and Figure 2 describe the biogenesis, sources, and contents of PDEN- and MSC-derived exosomes, whereas engineered exosomes are natural exosomes that have been artificially modified or loaded with therapeutic agents [39]. Animal-derived exosomes are further split into normal and tumor exosomes since exosomes can be produced in both normal and tumor conditions [39]. Studies related to mammalian-derived EVs, including exosomes, are documented in databases, such as Vesiclepedia (http://www.microvesicles.org, accessed on 17 February 2023) and ExoCarta at http://www.exocarta.org, (accessed on 17 February 2023) [61][62][63]. In addition to animals, plants are a source of exosomes, with good development prospects in the future. In recent years, studies have found that nano-sized EVs from plant cells have similar structures to the mammalian exosome [64][65][66][67], which is why these EVs are termed as “plant-derived exosome-like nano-particles” with various abbreviations, such as PDELNs [68], PLENs [69], or plant-derived exosome-like nanoparticles (PDENs) [70]. Other descriptive terms include “plant-derived nanovesicles (PDNVs)” [71], “plant-derived extracellular vesicles (PDEVs)” [72], “plant-derived exosomes” [73], “plant-derived edible nanoparticles” [74], or “edible plant-derived nanovesicles” [75]. The following contents uses the term “plant-derived exosome nanoparticles”, which is abbreviated as PDENs.
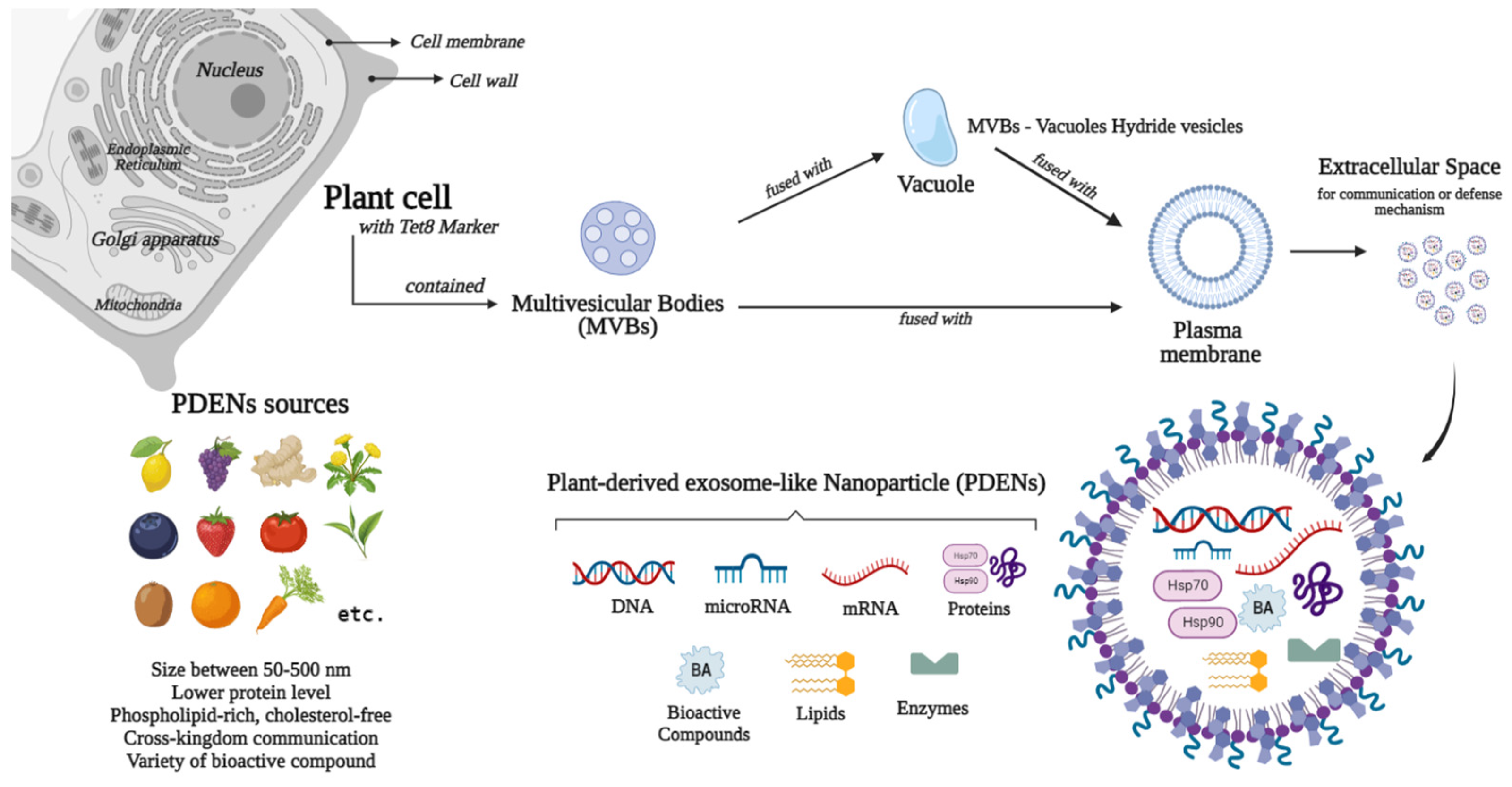
Figure 1. Sources, biogenesis, and contents of plant-derived exosome-like nanoparticles (PDENs).
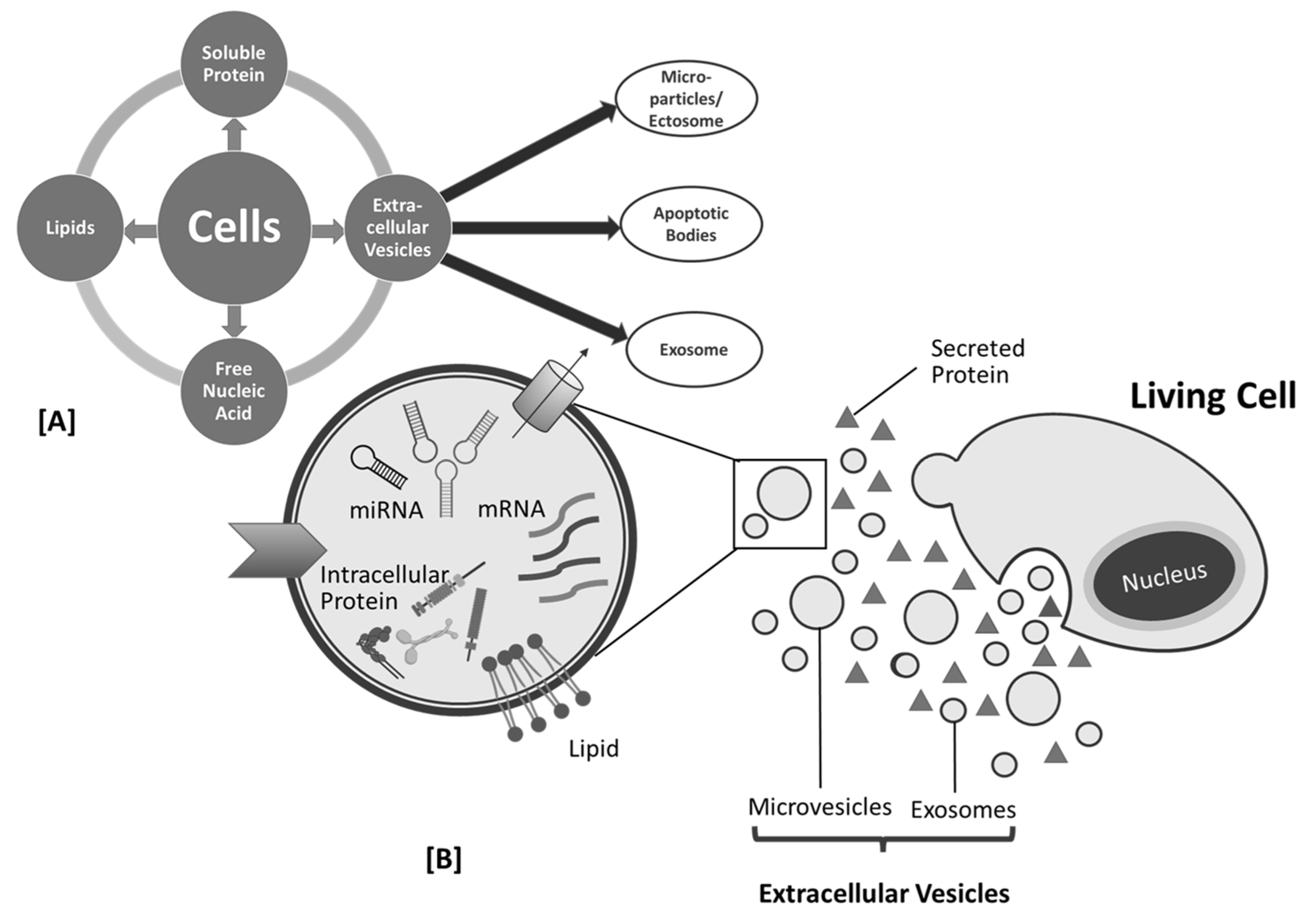
Figure 2. Cell products (A) and biogenesis of mesenchymal stem cell (MSC)-derived exosome (B).
Plant-derived exosome-like nanoparticles are still not as popular as mammalian-derived exosomes, which have been extensively investigated, but the research trend has been increasing [71][75][76][77]. This positive trend is driven by the idea that consumption of certain foods or their associated components is often linked to health benefits and disease risk reduction [75]. Furthermore, concerns have been raised regarding the utilization of human exosomes for therapeutic chemical delivery since evidence stated that human exosomes may constitute one of our body’s scavenging processes, restricting large-scale production, and often carrying potentially transferable harmful substances, such as tumor-derived molecules and foreign nucleic acid [78][79][80][81][82][83][84]. Similar to other allograft materials, the large-scale manufacturing and usage of exosomes derived from humans will face obstacles in the future due to exosome sources and ethical concerns.
In addition to plant-derived micronutrients, sterols, fibers, and phytochemicals, studies on plant-derived bioactive compounds and their impact on health have recently been broadened to include EVs [75]. The Food and Agriculture Organization (FAO) division of International Network of Food Data Systems (INFOODS) collects data on foods containing exosomes (or endosomal-derived vesicles) in their databases; https://www.fao.org/infoods (accessed on 17 February 2023). The database contains the following information regarding the plant-derived exosomes: Common name, group, scientific name, sample type, isolation method, and references [72][85]. PDENs, similar to mammalian-derived exosomes, comprise a variety of components, such as proteins, lipids, mRNA, microRNA, and their unique source-dependent bioactive constituents [86][87][88]. PDENs are composed of cytosolic and membrane proteins. They contain numerous types of confirmed proteins, such as heat shock proteins, which are accepted as exosome markers (e.g., CD9 and CD63), transmembrane proteins (e.g., actin, proteolysis, aquaporin, and chloride channels proteins), defense proteins, and other plasmalemma-associated proteins [89][90][91][92][93]. Research substantiated that PDENs from citrus fruits comprise proteins involved in diverse activities, including fructose bisphosphate for glycolysis, HSP80 and PTL39 for protein folding and transport, and PTL3 and clathrin-3 for cell growth and division. In addition, enzymes and antioxidants were identified [94]. In terms of protein level, PDENs are lower than mammalian exosomes [89].
Lipids in EVs can induce cellular responses in recipient cells, maintaining the structural stability of exosomes, facilitating their cargo components (uptake and retention), and playing an important role in intercellular communication [95][96]. PDENs are rich in phospholipids (e.g., phosphatidic acids (PA), phosphatidylethanolamines (PE), including plant lipids, such as galactolipids (e.g., monogalactosyldiacylglycerol (MGDG) and di-galactosyl di-acylglycerol (DGDG)) [89][97]. Based on previous studies, lipid composition approximations of some edible plants have been reported, such as exosome-like nanoparticles derived from ginger, which comprised 40% PA, 30–40% DGDG, and 20% MGDG [89][95], turmeric comprised 42% DGDG, 12% MGDG, 20% PA, and phosphatidylcholine (PC) as reported by Liu et al. (2022) [98], orange juice comprised 40% PE, 25% PC, and 5% PA [99], and grapefruit comprised 45.52% PE and 28.53% PC [65]. From the findings, it was known that the amounts of lipid compositions in PDENs vary depending on their sources. Moreover, it was observed that PDENs are different from mammalian exosomes since they are phospholipid-rich but cholesterol-free, whereas animal exosomes are cholesterol-rich [100][101].
Plant-derived exosome-like nanoparticles often comprise RNAs and a significant quantity of microRNAs (miRNAs), a class of small and noncoding RNAs (17–24 nucleotides). It has been found that miRNAs are capable of disrupting mRNA translation and transcription [102][103][104]. Moreover, based on previous studies regarding the potential for cross-kingdom communication by PDENs through gene expression modulation [105], which involves miRNA, it has been found that the internalization of PELNs is possible in plant cells, mammalian cells, fungi, and bacteria [101][106][107][108]. In addition, several bioactive compounds are found in PDENs, which have the potential to determine their effect. This naturally occurring metabolite varies not only based on plant origin, but also on the EV population size, preparation form, and isolation technique. Table 1 shows the compounds found in PDENs from several sources. In addition, PDENs comprise myo-inositol, quinic acid, and aucubin, which are anti-cancer and anti-inflammatory compounds [109].
Table 1. Metabolites found in PDENs from several sources.
| Sources of PDENs | Compounds | Remarks |
|---|---|---|
| Ginger | 6-gingerol, 8-gingerol, 10-gingerol, and 6-shogaol | [88][108] |
| Grapefruit | Naringenin | [65] |
| Lemon | Citrate, vitamin C, and galacturonic acid-enriched pectin-type polysaccharide | [66][110] |
| Strawberry | Vitamin C | [88] |
| Tea flower | Epigallo-catechin gallate, epicatechin gallate, epicatechin, vitexin, myricetin-3-O-rhamnoside, kaempferol-3-O-galactoside, and myricetin | [111] |
| Oat | Fiber β-glucan | [112] |
| Broccoli | Sulforaphane | [112] |
PDENs comprise 6-gingerol, 8-gingerol, 10-gingerol, and 6-shogaol, which are found in ginger [89][113]; naringenin found in grapefruit [65]; citrate, vitamin C, and galacturonic acid-enriched pectin-type polysaccharide found in lemon [66][110]; vitamin C found in strawberry [88]; epigallocatechin gallate, epicatechin gallate, epicatechin, vitexin, myricetin-3-O-rhamnoside, kaempferol-3-O-galactoside, and myricetin found in tea flower [66][111]; fiber β-glucan found in oat; and sulforaphane found in broccoli [112]. In addition, PDENs comprise myo-inositol, quinic acid, and aucubin, which are anti-cancer and anti-inflammatory compounds [109].
Plant-derived exosome-like nanoparticles need to undergo a series of processes before they can be used. After plant extraction, the first step is isolation and there are several isolation techniques used for PDENs. Most isolation methods are based on density, surface content, size, or precipitation [114]. Based on density, frequently used techniques are differential ultracentrifugation and density gradient centrifugation. These techniques are simple and cost-effective; therefore, they are considered as the “gold standard” for the isolation method [74][114][115][116]. Differential ultracentrifugation is the consecutive removal of particles based on size and density using progressive centrifugal durations and forces. The procedure is carried out via a step-by-step methodology, starting from the separation of cells, and then gradually cell debris, apoptotic cells, and micro-vesicles. As the remaining particles become smaller, the spinning speed is gradually increased (100,000–200,000 g) throughout the process [117][118][119]. The formation of sediment vesicles, protein aggregates [4], and exosomal aggregates [74][120], the extended duration, labor intensiveness, and the necessity for highly expensive equipment are the major drawbacks of this procedure [121][122][123][124]. In contrast to differential ultracentrifugation, density gradient ultracentrifugation isolate PDENs are based on size, mass, and density. This method differentiates between PDENs and contaminants with different densities using a subsequent phase with a sucrose density gradient (10–90%) or other material (e.g., iodixanol) [125][126]. Furthermore, density gradient ultracentrifugation is still extensively used today since this method increases the final purity of PDENs isolate [74][117]. Nevertheless, this technique yields few exosomes, is time-consuming, and requires expensive equipment and specialized knowledge [127][128].
Sized-based isolation methods including ultrafiltration and size exclusion chromatography (SEC) are commonly used to separate PDENs. Ultrafiltration, a faster alternative to ultracentrifugation, comprises the use of membrane filters with different molecular weight cutoffs (MWCO) and pressure to remove large molecular size impurities, followed by exosome isolation [67][129]. In this method, larger sample components including cells, cell debris, and macromolecules are not permitted to pass through the membrane pores [39]. Utilizing filters with pore sizes of 0.80 and 0.45 microns, larger particles can be eliminated. After collecting the remaining sample, a filter with pores of smaller diameters than exosomes (0.22–0.1 m) is used to remove particles smaller than exosomes. This approach obtains exosomes between filters with maximum and minimum pore diameters [130]. Ultrafiltration is simple and efficient without affecting the exosomes activity technique; however, it is low in purity and not suitable for wide usage [131]. SEC is another size-based method using gel-filtration. The mobile phase is an aqueous solution that transports the sample along the column, while the stationary phase is a porous filtration polymer that permits differential elution. With the support of gravity, larger particles are eluted before smaller ones. However, other factors, such as molecular weight and shape, can also influence this separation process [21][115][132]. The advantages of this technique include good homogeneity and preservation of the integrity, morphology, and functionality of nanoparticles. However, this technique is not widely used due to low purity production and absence of selectivity in extracting exosomes from particles of almost identical size [133][134][135][136]. Asymmetric flow field-flow fractionation (AF4) is a recent, size-based isolation method. AF4 separates nanoparticles with sizes ranging from a few nanometers to an undetermined amount of micrometers, depending on their hydrodynamic diameters, in a thin, flat channel with a semipermeable wall membrane [136].
Moreover, the polymer precipitation method can be used to isolate PDENs, although this method is originally used to isolate viruses [137][138][139]. The scientific reasoning is due to the fact that both viruses and small PDENs have similar biophysical characteristics [39]. This method uses polyethylene glycol (PEG), specifically PEG6000, which is capable of forming a net-like structure to trap PDENs before precipitation. These precipitated and aggregated PDENs are harvested through lower centrifugation rates [140]. This technique is easy to operate, time-efficient, and capable of processing large doses of samples [39]. Furthermore, this study illustrates that this technique is less expensive and outperforms ultracentrifugation in terms of purity and recovery [141]. Polymer precipitation using concentration-adjusted PEG6000 produced PDENs with a smaller particle size than ultracentrifugation [142]. However, impurity and low recovery time are the primary disadvantages of this technique [39][143].
Another method for isolating PDENs is the affinity-based isolation method or immunoaffinity chromatography (IAC). IAC is a separation and purification method based on the specific interaction of antibodies and ligands to isolate desired components from the heterogenous mixture [39][115]. The biomarker or antigen should be a high-abundance protein on the surface of exosome membranes, such as the four-transmembrane protein superfamily and ESCRT complex-related proteins [39][143]. Several methods have been proven to be successful for isolation-related IAC, among these are magnetic beads [144] or FeO3 nano-cubes [145] loaded or coated with antibodies, as well as heat shock proteins [146], heparin [147], or epithelial cell adhesion molecules [148]. These methods accommodate high-purity exosomes and selectively isolate exosomes that carry a specific marker [114]. Nevertheless, the drawbacks of these methods include the heterogenous nature of PDENs and the loss of exosomes integrity by removal of the antibody process [149][150]. In addition to the aforementioned common methods, few other advanced methods can be used to isolate the PDENs, such as microfluidics-based isolation by trapping PDENs in a porous microstructure with a selective micropillar design of 40–100 nm in diameter [151]. This can be performed via the acoustics-based approach using a combination of microfluidic chip and acoustic waves [152], or a commercially available exosomes isolation kit that is time-saving but costly, such as total Exosome Isolation kit (Invitrogen), exoEasy Maxi kit (QIAGEN), MagCapture™ Exosome Isolation Kit PS (Wako), Eloquence (System Biosciences), Exo-spin (Cell guidance systems), and Minute™ Hi-Efficiency Exosome Precipitation Reagent [39][153]. These kits can be used to separate exosomes from biological samples, such as serum, plasma, and CSF. However, the purity, amount, and size distribution of the collected exosomes are very different [154][155].
Plant-derived exosome-like nanoparticles, such as mammalian exosomes, can be characterized using the ultrasensitive microscopic technique, such as scanning electron microscopy (SEM), transmission electron microscopy (TEM), atomic force microscopy (AFM), or using cryo-electron microscopy for structural analysis in subcellular level [119][156]. Optical characterization approaches cannot identify PDENs due to their small diameters; therefore, various methods of electron microscopy are essential to determine their morphological size and shape [157]. SEM can be used to observe the surface structure; however, it is lower in resolution. Meanwhile, the high-resolution TEM provides information regarding the internal structure and particles distribution; however, it is not suitable for rapid measurement since the pre-processing step is more complex [158][159]. Sample preparation for TEM proved to be responsible for the observed morphology variations [160][161].
Particles charge and size of PDENs can be observed using dynamic light scattering (DLS); however, this technique cannot detect the concentration and is not suitable for measuring complex exosomes with large size range. The concentration of PDENs can be measured using the nanoparticle tracking analysis (NTA) [39][119]. This technology emerged as the “gold standard” for exosomes characterization since PDENs can be observed in real-time due to their fast detection speed; however, the operation is complex and can affect the PDENs quantification [39][135][162]. To determine the size and concentration of PDENs in suspension, resistive pulse sensing (RPS) technology can be used. Since a voltage is applied, the detection of exosomes by RPS with the transfer of single nanoparticles through the nanopore is established [156][163]. Western blot and enzyme-linked immunosorbent analysis (ELISA) can be used to detect the expression of PDENs marker proteins [41][164]. Flow cytometry can be used to detect the biomarker of PDENs. Flow cytometry is a high-throughput technology and capable of high-speed multi-channel analysis with low sample concentration [39][156]. However, the newest generations of digital flow cytometry instruments, with a lower limit of measurement of 100 nm, are still unreliable in terms of accuracy and resolution [156]. Another technique to characterize PDENs specifically for the determination of the PDENs weight can be performed using the developed nanomechanical resonator. Moreover, zeta analyzer can be used to observe the repulsive nature against aggregation or dispersity and the membrane potential [119][165].
Similar to the most common exosomes, PDENs cannot be maintained for a long period of time. Therefore, it is necessary to preserve PDENs in order to maintain their biological activities and for readily accessible clinical application. Plant extracts stored prior to PDENs isolation may influence the separation, content, and function of PDENs, such as those reported in EVs derived from biofluids. Before the isolation process, samples were mainly stored in freezing conditions for short or long periods. Although 4 and −80 °C or lower are mentioned and generally used in laboratories today, the problem is that no optimal storage condition has been determined for isolated EVs [166][167][168][169][170][171]. EVs may alter to varying degrees during storage, resulting in size, shape, function, and content loss [172]. Current techniques to accommodate this include cryopreservation, freeze-drying, and spray-drying [39][173].
Cryopreservation is the application of low temperatures below those needed for biochemical reactions (4 °C, −80 °C, or −196 °C) to preserve the functional stability of biological particles, including PDENs, using cryoprotectants [166][172][173][174]. There are two types of cryoprotectants which are differentiated based on their permeability or penetration and both aimed to reduce the injury of EVs. Penetrating cryoprotectants (e.g., glycerol, DMSO, and ethylene glycol) have a small molecular weight that can penetrate the cell membrane, while non-penetrating cryoprotectants (e.g., sucrose, mannose, and trehalose) form a hydrogen bond with water to prevent ice crystal formation [159][175][176]. A previous study has proven that cryopreservation in −80 °C with or without cryoprotectants, such as trehalose 25 mM, DMSO 6 and 10%, and glycerol 30%, can maintain the concentration of EVs up to 6 months [176]. However, storage conditions may vary depending on the source of EVs. Regarding safety, trehalose as a non-penetrating type, is the best option and most effective antifreeze [175][177].
Freeze-drying process is a technology that involves sublimation and desorption, where moisture-containing materials are frozen to a solid below the freezing point prior to their use [39][172]. Freeze-drying is a new technique for preserving EVs, including PDENs, and the optimal storage temperature for freeze-dried EVs is 4 °C [178][179]. Freeze-drying is advantageous in the expansion of the lifespan of heat-sensitive materials, such as EVs, vaccines, and proteins since it can maintain the material’s original activity, while causing less damage to biological tissues and cell bodies. Moreover, the material can be easily stored in a constant state and reconstituted by simply adding water. However, due to the freezing and dehydration pressures generated during the freeze-drying process, the molecular structure of the biomolecule may be destroyed [39][172]. Based on previous studies, cryoprotectant products, such as trehalose, may be used to prevent aggregation during the freeze-drying process and reduce the alteration in the stability and morphology of EVs, including PDENs [179][180][181]. Spray-drying, on the other hand, is an option. Spray-drying is a one-step method that is simpler than freeze-drying [172]. This technique is more economical, can be used with a variety of agents, and allows for product size adjustment. First, PDENs solution is atomized in a drying room, and then when moisture interacts with hot air, it quickly vaporizes, resulting in dry powders [39][174]. PDENs stability can be affected by factors, such as EV solution feed, atomization pressure, and output temperature. Furthermore, residual moisture may cause chemical instability by lowering the solid particle state’s glass transition temperature [172].
The advantages of PDENs as biomolecules are: (1) Provided by nature and can be involved in intercellular communications, (2) phospholipid-rich characteristics in order that the lipid membrane can protect the cargo from the external agent, which can deteriorate the bioactive compound inside the PDENs, (3) natural mechanism of cellular uptake in order that they may have the ability to pass through some of the barriers in our body, such as blood brain barrier and the placenta, (4) tolerated by the immune system as they are currently present in foods ingested by humans, (5) verified scalability and suitability for industrial applications, (6) non-toxic, as they are produced from organic fruits and vegetables [71], and (7) long-term availability from numerous types of plants, which can be cultivated. These PDENs are worth development in various fields, especially in the field of biomolecular medicine. This can be accomplished by exploring the cargo, in particular, the contents and functions of bioactive constituents. Then, they can be related to the necessary various problem-solving strategies. A better understanding of PDENs in the future has the potential to usher in a new paradigm for natural medicine, which employs compounds that are abundantly available, more effective, efficient, and have significantly fewer adverse effects than the currently accessible medications.
Exosomes have been investigated in animal models and clinical trials in recent years to obtain their biological properties. Grape-derived PDENs have been proven to be nontoxic to intestinal macrophages, splenic, and liver cells of mouse model [65][100]. Ginger-derived PDENs are nontoxic to colon-26 epithelial-like cell lines, and RAW 264.7 macrophage-like cell lines in the colon’s mouse model [89]. Another study proved that citrus lemon-derived PDENs inhibit the growth of CML tumors in vivo by reaching the tumor site and activating TRAIL-mediated apoptotic cell processes in the liver, spleen, and kidney of mouse model [182]. Moreover, ginseng-derived PDENs proved to be nontoxic to BMDMs (bone marrow-derived macrophages), B16F10 (mouse melanoma cell line), 4T1 (mouse mammary carcinoma line), and HEK293T (human embryonic kidney cell line) in the liver and spleen of mouse model [81]. The development of human exosomes and PDENs as potential biomolecules has reached the clinical trial stage [183][184]. According to a ClinicalTrials.gov survey (https://clinicaltrials.gov/, accessed on 17 February 2023), exosomes are used for clinical trial as biomarkers (50%), exosome-therapy (28.44%), drug delivery systems (5.17%), cancer vaccines (1.72%), and other analysis (14.66%) [183]. Two reported clinical trials using PDENs aimed to encapsulate curcumin into grape-derived (NCT01294072) PDENs and ginger-derived (NCT04879810) PDENs for the treatment of colon cancer and irritable bowel disease, respectively. Another clinical trial using grape-derived PDENs (NCT01668849) aimed to investigate the ability of grape-derived PDENs to prevent oral mucositis associated with head and neck cancer chemoradiation treatment. However, none of these trials have been completed, and the results are not yet available [183][184]. Furthermore, although several experimental studies have been documented, there is less evidence on GMP manufacturing for plant-derived exosomes [21][185].
References
- Farley, A.; McLafferty, E.; Hendry, C. Cells, Tissues, Organs and Systems. Nurs. Stand. 2012, 26, 40–45.
- Caplan, A.I. Design Parameters For Functional Tissue Engineering. In Functional Tissue Engineering; Guilak, F., Butler, D.L., Goldstein, S.A., Mooney, D.J., Eds.; Springer: New York, NY, USA, 2003; Volume 1.
- Farach-Carson, M.C.; Wagner, R.C.; Kiick, K.L. Extracellular Matrix: Structure, Function, and Appliations to Tissue Engineering. In Tissue Engineering; Fisher, J.P., Mikos, A.G., Bronzino, J.D., Eds.; CRC Press: Boca Raton, FL, USA, 2007; Volume 1, pp. 1–17.
- Badylak, S.; Gilbert, T.; Myers-Irvin, J. The Extracellular Matrix as a Biologic Scaffold for Tissue Engineering. In Tissue Engineering; Bronzino, J., Thomsen, P., Lindahl, A., Hubbel, J., Williams, D., Cancedda, R., de Brujin, J., Sohier, J., Eds.; Academic Press: San Diego, CA, USA, 2008; Volume 1, pp. 121–143.
- Hare, J.M.; Traverse, J.H.; Henry, T.D.; Dib, N.; Strumpf, R.K.; Schulman, S.P.; Gerstenblith, G.; DeMaria, A.N.; Denktas, A.E.; Gammon, R.S.; et al. A Randomized, Double-Blind, Placebo-Controlled, Dose-Escalation Study of Intravenous Adult Human Mesenchymal Stem Cells (Prochymal) After Acute Myocardial Infarction. J. Am. Coll. Cardiol. 2009, 54, 2277–2286.
- Beyth, S.; Schroeder, J.; Liebergall, M. Stem Cells in Bone Diseases: Current Clinical Practice. Br. Med. Bull. 2011, 99, 199–210.
- Casteilla, L.; Planat-Benard, V.; Laharrague, P.; Cousin, B. Adipose-Derived Stromal Cells: Their Identity and Uses in Clinical Trials, an Update. World. J. Stem. Cells 2011, 3, 25–33.
- Mingliang, R.; Bo, Z.; Zhengguo, W. Stem Cells for Cardiac Repair: Status, Mechanisms, and New Strategies. Stem. Cells Int. 2011, 2011, 310928.
- Yokoo, T.; Matsumoto, K.; Yokote, S. Potential Use of Stem Cells for Kidney Regeneration. Int. J. Nephrol. 2011, 2011, 591731.
- Zakrzewski, W.; Dobrzyński, M.; Szymonowicz, M.; Rybak, Z. Stem Cells: Past, Present, and Future. Stem. Cell Res. 2019, 10, 68.
- Kunter, U.; Rong, S.; Boor, P.; Eitner, F.; Müller-Newen, G.; Djuric, Z.; van Roeyen, C.R.; Konieczny, A.; Ostendorf, T.; Villa, L.; et al. Mesenchymal Stem Cells Prevent Progressive Experimental Renal Failure but Maldifferentiate into Glomerular Adipocytes. J. Am. Soc. Nephrol. 2007, 18, 1754–1764.
- Michalopoulos, G.K. Liver Regeneration. J. Cell Physiol. 2007, 213, 286–300.
- Rubina, K.; Kalinina, N.; Efimenko, A.; Lopatina, T.; Melikhova, V.; Tsokolaeva, Z.; Sysoeva, V.; Tkachuk, V.; Parfyonova, Y. Adipose Stromal Cells Stimulate Angiogenesis via Promoting Progenitor Cell Differentiation, Secretion of Angiogenic Factors, and Enhancing Vessel Maturation. Tissue. Eng. Part A 2009, 15, 2039–2048.
- Tögel, F.E.; Westenfelder, C. The Role of Multipotent Marrow Stromal Cells (MSCs) in Tissue Regeneration. Organogenesis 2011, 7, 96–100.
- Mahanani, E.S.; Bachtiar, I.; Ana, I.D. Human Mesenchymal Stem Cells Behavior on Synthetic Coral Scaffold. Key. Eng. Mater. 2016, 696, 205–211.
- Breitbach, M.; Bostani, T.; Roell, W.; Xia, Y.; Dewald, O.; Nygren, J.M.; Fries, J.W.U.; Tiemann, K.; Bohlen, H.; Hescheler, J.; et al. Potential Risks of Bone Marrow Cell Transplantation into Infarcted Hearts. Blood 2007, 110, 1362–1369.
- Wang, J.J.; Ye, F.; Cheng, L.J.; Shi, Y.J.; Bao, J.; Sun, H.Q.; Wang, W.; Zhang, P.; Bu, H. Osteogenic Differentiation of Mesenchymal Stem Cells Promoted by Overexpression of Connective Tissue Growth Factor. J. Zhejiang Univ. Sci. B 2009, 10, 355–367.
- Gomzikova, M.O.; Rizvanov, A.A. Current Trends in Regenerative Medicine: From Cell to Cell-Free Therapy. Bionanoscience 2017, 7, 240–245.
- Ana, I.D.; Barlian, A.; Hidajah, A.C.; Wijaya, C.H.; Notobroto, H.B.; Kencana Wungu, T.D. Challenges and Strategy in Treatment with Exosomes for Cell-Free-Based Tissue Engineering in Dentistry. Future Sci. OA 2021, 7, 1–21.
- Amsar, R.M.; Wijaya, C.H.; Ana, I.D.; Hidajah, A.C.; Notobroto, H.B.; Kencana Wungu, T.D.; Barlian, A. Extracellular Vesicles: A Promising Cell-Free Therapy for Cartilage Repair. Future Sci. OA 2022, 8, FSO774.
- Suharta, S.; Barlian, A.; Hidajah, A.C.; Notobroto, H.B.; Ana, I.D.; Indariani, S.; Wungu, T.D.K.; Wijaya, C.H. Plant-Derived Exosome-like Nanoparticles: A Concise Review on Its Extraction Methods, Content, Bioactivities, and Potential as Functional Food Ingredient. J. Food Sci. 2021, 86, 2838–2850.
- Ratnadewi, D.; Widjaja, C.H.; Barlian, A.; Amsar, R.M.; Ana, I.D.; Hidajah, A.C.; Notobroto, H.B.; Wungu, T.D.K. Isolation of Native Plant-Derived Exosome-like Nanoparticles and Their Uptake by Human Cells. Hayati 2023, 30, 182–192.
- Trams, E.G.; Lauter, C.J.; Salem, N.J.; Heine, U. Exfoliation of Membrane Ecto-Enzymes in the Form of Micro-Vesicles. Biochim. Biophys. Acta 1981, 645, 63–70.
- Johnstone, R.M. Revisiting the Road to the Discovery of Exosomes. Blood Cells Mol. Dis. 2005, 34, 214–219.
- Théry, C.; Zitvogel, L.; Amigorena, S. Exosomes: Composition, Biogenesis and Function. Nat. Rev. Immunol. 2002, 2, 569–579.
- Théry, C. Exosomes: Secreted Vesicles and Intercellular Communications. F1000 Biol. Rep. 2011, 3, 1–8.
- el Andaloussi, S.; Mäger, I.; Breakefield, X.O.; Wood, M.J.A. Extracellular Vesicles: Biology and Emerging Therapeutic Opportunities. Nat. Rev. Drug Discov. 2013, 12, 347–357.
- Lötvall, J.; Hill, A.F.; Hochberg, F.; Buzás, E.I.; di Vizio, D.; Gardiner, C.; Gho, Y.S.; Kurochkin, I.; Mathivanan, S.; Quesenberry, P.; et al. Minimal Experimental Requirements for Definition of Extracellular Vesicles and Their Functions: A Position Statement from the International Society for Extracellular Vesicles. J. Extracell. Vesicles 2014, 3, 26913.
- Cocucci, E.; Meldolesi, J. Ectosomes and Exosomes: Shedding the Confusion between Extracellular Vesicles. Trends Cell Biol. 2015, 25, 364–372.
- Pluchino, S.; Smith, J.A. Explicating Exosomes: Reclassifying the Rising Stars of Intercellular Communication. Cell 2019, 177, 225–227.
- Weaver, J.W.; Zhang, J.; Rojas, J.; Musich, P.R.; Yao, Z.; Jiang, Y. The Application of Exosomes in the Treatment of Triple-Negative Breast Cancer. Front. Mol. Biosci. 2022, 9, 1022725.
- Zaborowski, M.P.; Balaj, L.; Breakefield, X.O.; Lai, C.P. Extracellular Vesicles: Composition, Biological Relevance, and Methods of Study. Bioscience 2015, 65, 783–797.
- Lopez-Verrilli, M.A.; Caviedes, A.; Cabrera, A.; Sandoval, S.; Wyneken, U.; Khoury, M. Mesenchymal Stem Cell-Derived Exosomes from Different Sources Selectively Promote Neuritic Outgrowth. Neurosci 2016, 320, 129–139.
- Willms, E.; Johansson, H.J.; Mäger, I.; Lee, Y.; Blomberg, K.E.M.; Sadik, M.; Alaarg, A.; Smith, C.I.E.; Lehtiö, J.; el Andaloussi, S.; et al. Cells Release Subpopulations of Exosomes with Distinct Molecular and Biological Properties. Sci. Rep. 2016, 6, 22519.
- Jeppesen, D.K.; Fenix, A.M.; Franklin, J.L.; Higginbotham, J.N.; Zhang, Q.; Zimmerman, L.J.; Liebler, D.C.; Ping, J.; Liu, Q.; Evans, R.; et al. Reassessment of Exosome Composition. Cell 2019, 177, 428–445.e18.
- Yang, X.-X.; Sun, C.; Wang, L.; Guo, X.-L. New Insight into Isolation, Identification Techniques and Medical Applications of Exosomes. J. Control. Release 2019, 308, 119–129.
- Harry Heijnen, B.F.; Schiel, A.E.; Fijnheer, R.; Geuze, H.J.; Sixma, J.J. Activated Platelets Release Two Types of Membrane Vesicles: Microvesicles by Surface Shedding and Exosomes Derived From Exocytosis of Multivesicular Bodies and-Granules. Blood 1999, 94, 3791–3799.
- Stremersch, S.; de Smedt, S.C.; Raemdonck, K. Therapeutic and Diagnostic Applications of Extracellular Vesicles. JCR 2016, 244, 167–183.
- Zhang, Y.; Bi, J.; Huang, J.; Tang, Y.; Du, S.; Li, P. Exosome: A Review of Its Classification, Isolation Techniques, Storage, Diagnostic and Targeted Therapy Applications. Int. J. Nanomed. 2020, 15, 6917–6934.
- Cassarà, D.; Ginestra, A.; Dolo, V.; Miele, M.; Caruso, G.; Lucania, G.; Vittorelli, M.L. Modulation of Vesicle Shedding in 8701 BC Human Breast Carcinoma Cells. J. Submicrosc. Cytol. Pathol. 1998, 30, 45–53.
- Théry, C.; Witwer, K.W.; Aikawa, E.; Alcaraz, M.J.; Anderson, J.D.; Andriantsitohaina, R.; Antoniou, A.; Arab, T.; Archer, F.; Atkin-Smith, G.K.; et al. Minimal Information for Studies of Extracellular Vesicles 2018 (MISEV2018): A Position Statement of the International Society for Extracellular Vesicles and Update of the MISEV2014 Guidelines. J. Extracell. Vesicles 2018, 7, 1535750.
- Stein, J.M.; Luzio, J.P. Ectocytosis Caused by Sublytic Autologous Complement Attack on Human Neutrophils. The Sorting of Endogenous Plasma-Membrane Proteins and Lipids into Shed Vesicles. Biochem. J. 1991, 274 Pt 2, 381–386.
- Marote, A.; Teixeira, F.G.; Mendes-Pinheiro, B.; Salgado, A.J. MSCs-Derived Exosomes: Cell-Secreted Nanovesicles with Regenerative Potential. Front. Pharm. 2016, 7, 231.
- McGough, I.J.; Vincent, J.-P. Exosomes in Developmental Signalling. Development 2016, 143, 2482–2493.
- Whiteside, T.L. Exosomes and Tumor-Mediated Immune Suppression. J. Clin. Investig. 2016, 126, 1216–1223.
- Schorey, J.S.; Bhatnagar, S. Exosome Function: From Tumor Immunology to Pathogen Biology. Traffic 2008, 9, 871–881.
- Bang, C.; Thum, T. Exosomes: New Players in Cell-Cell Communication. Int. J. Biochem. Cell Biol. 2012, 44, 2060–2064.
- Eitan, E.; Suire, C.; Zhang, S.; Mattson, M.P. Impact of Lysosome Status on Extracellular Vesicle Content and Release. Ageing Res. Rev. 2016, 32, 65–74.
- Kalluri, R. The Biology and Function of Exosomes in Cancer. J. Clin. Investig. 2016, 126, 1208–1215.
- Sarko, D.K.; McKinney, C.E. Exosomes: Origins and Therapeutic Potential for Neurodegenerative Disease. Front. Neurosci. 2017, 11, 82.
- Properzi, F.; Logozzi, M.; Fais, S. Exosomes: The Future of Biomarkers in Medicine. Biomark. Med. 2013, 7, 769–778.
- Lin, J.; Li, J.; Huang, B.; Liu, J.; Chen, X.; Chen, X.-M.; Xu, Y.-M.; Huang, L.-F.; Wang, X.-Z. Exosomes: Novel Biomarkers for Clinical Diagnosis. Sci. World J. 2015, 2015, 657086.
- Cheng, L.; Zhang, K.; Wu, S.; Cui, M.; Xu, T. Focus on Mesenchymal Stem Cell-Derived Exosomes: Opportunities and Challenges in Cell-Free Therapy. Stem. Cells Int. 2017, 2017, 6305295.
- He, C.; Hua, W.; Liu, J.; Fan, L.; Hua, W.; Sun, G. Exosomes Derived from Endoplasmic Reticulum-Stressed Liver Cancer Cells Enhance the Expression of Cytokines in Macrophages via the STAT3 Signaling Pathway. Oncol. Lett. 2020, 20, 589–600.
- Li, D.; Wang, Y.; Jin, X.; Hu, D.; Xia, C.; Xu, H.; Hu, J. NK Cell-Derived Exosomes Carry MiR-207 and Alleviate Depression-like Symptoms in Mice. J. Neuroinflammation 2020, 17, 126.
- Zhao, D.; Yu, Z.; Li, Y.; Wang, Y.; Li, Q.; Han, D. GelMA Combined with Sustained Release of HUVECs Derived Exosomes for Promoting Cutaneous Wound Healing and Facilitating Skin Regeneration. J. Mol. Histol. 2020, 51, 251–263.
- Agrawal, A.K.; Aqil, F.; Jeyabalan, J.; Spencer, W.A.; Beck, J.; Gachuki, B.W.; Alhakeem, S.S.; Oben, K.; Munagala, R.; Bondada, S.; et al. Milk-Derived Exosomes for Oral Delivery of Paclitaxel. Nanomedicine 2017, 13, 1627–1636.
- Srivastava, A.; Moxley, K.; Ruskin, R.; Dhanasekaran, D.N.; Zhao, Y.D.; Ramesh, R. A Non-Invasive Liquid Biopsy Screening of Urine-Derived Exosomes for MiRNAs as Biomarkers in Endometrial Cancer Patients. AAPS J. 2018, 20, 82.
- Shaimardanova, A.A.; Solovyeva, V.V.; Chulpanova, D.S.; James, V.; Kitaeva, K.V.; Rizvanov, A.A. Extracellular Vesicles in the Diagnosis and Treatment of Central Nervous System Diseases. Neural. Regen. Res. 2020, 15, 586–596.
- Zhuo, C.J.; Hou, W.H.; Jiang, D.G.; Tian, H.J.; Wang, L.N.; Jia, F.; Zhou, C.H.; Zhu, J.J. Circular RNAs in Early Brain Development and Their Influence and Clinical Significance in Neuropsychiatric Disorders. Neural. Regen. Res. 2020, 15, 817–823.
- Kalra, H.; Simpson, R.J.; Ji, H.; Aikawa, E.; Altevogt, P.; Askenase, P.; Bond, V.C.; Borràs, F.E.; Breakefield, X.; Budnik, V.; et al. Vesiclepedia: A Compendium for Extracellular Vesicles with Continuous Community Annotation. PLoS Biol. 2012, 10, e1001450.
- Keerthikumar, S.; Chisanga, D.; Ariyaratne, D.; al Saffar, H.; Anand, S.; Zhao, K.; Samuel, M.; Pathan, M.; Jois, M.; Chilamkurti, N.; et al. ExoCarta: A Web-Based Compendium of Exosomal Cargo. J. Mol. Biol. 2016, 428, 688–692.
- Pathan, M.; Fonseka, P.; Chitti, S.; Kang, T.; Sanwlani, R.; van Deun, J.; Hendrix, A.; Mathivanan, S. Vesiclepedia 2019: A Compendium of RNA, Proteins, Lipids and Metabolites in Extracellular Vesicles. Nucleic. Acids. Res. 2019, 47, D516–D519.
- Regente, M.; Corti-Monzón, G.; Maldonado, A.M.; Pinedo, M.; Jorrín, J.; de la Canal, L. Vesicular Fractions of Sunflower Apoplastic Fluids Are Associated with Potential Exosome Marker Proteins. FEBS Lett. 2009, 583, 3363–3366.
- Wang, B.; Zhuang, X.; Deng, Z.-B.; Jiang, H.; Mu, J.; Wang, Q.; Xiang, X.; Guo, H.; Zhang, L.; Dryden, G.; et al. Targeted Drug Delivery to Intestinal Macrophages by Bioactive Nanovesicles Released from Grapefruit. Mol. Ther. 2014, 22, 522–534.
- Baldini, N.; Torreggiani, E.; Roncuzzi, L.; Perut, F.; Zini, N.; Avnet, S. Exosome-like Nanovesicles Isolated from Citrus Limon L. Exert Antioxidative Effect. Curr. Pharm. Biotechnol. 2018, 19, 877–885.
- Akuma, P.; Okagu, O.D.; Udenigwe, C.C. Naturally Occurring Exosome Vesicles as Potential Delivery Vehicle for Bioactive Compounds. Front. Sustain. Food Syst. 2019, 3, 23.
- Li, D.; Yao, X.; Yue, J.; Fang, Y.; Cao, G.; Midgley, A.C.; Nishinari, K.; Yang, Y. Advances in Bioactivity of MicroRNAs of Plant-Derived Exosome-Like Nanoparticles and Milk-Derived Extracellular Vesicles. J. Agric. Food Chem. 2022, 70, 6285–6299.
- Zhang, Z.; Yu, Y.; Zhu, G.; Zeng, L.; Xu, S.; Cheng, H.; Ouyang, Z.; Chen, J.; Pathak, J.L.; Wu, L.; et al. The Emerging Role of Plant-Derived Exosomes-Like Nanoparticles in Immune Regulation and Periodontitis Treatment. Front. Immunol. 2022, 13, 896745.
- Chen, N.; Sun, J.; Zhu, Z.; Cribbs, A.P.; Xiao, B. Edible Plant-Derived Nanotherapeutics and Nanocarriers: Recent Progress and Future Directions. Expert. Opin. Drug Deliv. 2022, 19, 409–419.
- Logozzi, M.; di Raimo, R.; Mizzoni, D.; Fais, S. The Potentiality of Plant-Derived Nanovesicles in Human Health-A Comparison with Human Exosomes and Artificial Nanoparticles. Int. J. Mol. Sci. 2022, 23, 4919.
- Karamanidou, T.; Tsouknidas, A. Plant-Derived Extracellular Vesicles as Therapeutic Nanocarriers. Int. J. Mol. Sci. 2022, 23, 191.
- Cai, Y.; Zhang, L.; Zhang, Y.; Lu, R. Plant-Derived Exosomes as a Drug-Delivery Approach for the Treatment of Inflammatory Bowel Disease and Colitis-Associated Cancer. Pharmaceutics 2022, 14, 822.
- Zhang, M.; Viennois, E.; Xu, C.; Merlin, D. Plant Derived Edible Nanoparticles as a New Therapeutic Approach against Diseases. Tissue Barriers 2016, 4, e1134415.
- Kim, S.Q.; Kim, K.-H. Emergence of Edible Plant-Derived Nanovesicles as Functional Food Components and Nanocarriers for Therapeutics Delivery: Potentials in Human Health and Disease. Cells 2022, 11, 2232.
- Ding, Y.; Wang, J.; Wang, J.; Stierhof, Y.-D.; Robinson, D.G.; Jiang, L. Unconventional Protein Secretion. Trends. Plant Sci. 2012, 17, 606–615.
- Regente, M.; Pinedo, M.; Elizalde, M.; de la Canal, L. Apoplastic Exosome-like Vesicles: A New Way of Protein Secretion in Plants? Plant Signal Behav. 2012, 7, 544–546.
- Canitano, A.; Venturi, G.; Borghi, M.; Ammendolia, M.G.; Fais, S. Exosomes Released in Vitro from Epstein-Barr Virus (EBV)-Infected Cells Contain EBV-Encoded Latent Phase MRNAs. Cancer Lett. 2013, 337, 193–199.
- Cossetti, C.; Lugini, L.; Astrologo, L.; Saggio, I.; Fais, S.; Spadafora, C. Soma-to-Germline Transmission of RNA in Mice Xenografted with Human Tumour Cells: Possible Transport by Exosomes. PLoS ONE 2014, 9, e101629.
- Federici, C.; Petrucci, F.; Caimi, S.; Cesolini, A.; Logozzi, M.; Borghi, M.; D’Ilio, S.; Lugini, L.; Violante, N.; Azzarito, T.; et al. Exosome Release and Low PH Belong to a Framework of Resistance of Human Melanoma Cells to Cisplatin. PLoS ONE 2014, 9, e88193.
- Properzi, F.; Logozzi, M.; Abdel-Haq, H.; Federici, C.; Lugini, L.; Azzarito, T.; Cristofaro, I.; Sevo, D.; Ferroni, E.; Cardone, F.; et al. Detection of Exosomal Prions in Blood by Immunochemistry Techniques. J. Gen. Virol. 2015, 96, 1969–1974.
- Lugini, L.; Valtieri, M.; Federici, C.; Cecchetti, S.; Meschini, S.; Condello, M.; Signore, M.; Fais, S. Exosomes from Human Colorectal Cancer Induce a Tumor-like Behavior in Colonic Mesenchymal Stromal Cells. Oncotarget 2016, 7, 50086–50098.
- Iessi, E.; Logozzi, M.; Lugini, L.; Azzarito, T.; Federici, C.; Spugnini, E.P.; Mizzoni, D.; di Raimo, R.; Angelini, D.F.; Battistini, L.; et al. Acridine Orange/Exosomes Increase the Delivery and the Effectiveness of Acridine Orange in Human Melanoma Cells: A New Prototype for Theranostics of Tumors. J. Enzym. Inhib. Med. Chem. 2017, 32, 648–657.
- Logozzi, M.; Mizzoni, D.; Bocca, B.; di Raimo, R.; Petrucci, F.; Caimi, S.; Alimonti, A.; Falchi, M.; Cappello, F.; Campanella, C.; et al. Human Primary Macrophages Scavenge AuNPs and Eliminate It through Exosomes. A Natural Shuttling for Nanomaterials. Eur. J. Pharm. Biopharm. 2019, 137, 23–36.
- Pérez-Bermúdez, P.; Blesa, J.; Soriano, J.M.; Marcilla, A. Extracellular Vesicles in Food: Experimental Evidence of Their Secretion in Grape Fruits. Eur. J. Pharm. Sci. 2017, 98, 40–50.
- Nemati, M.; Singh, B.; Mir, R.A.; Nemati, M.; Babaei, A.; Ahmadi, M.; Rasmi, Y.; Golezani, A.G.; Rezaie, J. Plant-Derived Extracellular Vesicles: A Novel Nanomedicine Approach with Advantages and Challenges. Cell Commun. Signal 2022, 20, 69.
- Crescitelli, R.; Lässer, C.; Jang, S.C.; Cvjetkovic, A.; Malmhäll, C.; Karimi, N.; Höög, J.L.; Johansson, I.; Fuchs, J.; Thorsell, A.; et al. Subpopulations of Extracellular Vesicles from Human Metastatic Melanoma Tissue Identified by Quantitative Proteomics after Optimized Isolation. J. Extracell. Vesicles 2020, 9, 1722433.
- Perut, F.; Roncuzzi, L.; Avnet, S.; Massa, A.; Zini, N.; Sabbadini, S.; Giampieri, F.; Mezzetti, B.; Baldini, N. Strawberry-Derived Exosome-like Nanoparticles Prevent Oxidative Stress in Human Mesenchymal Stromal Cells. Biomolecules 2021, 11, 87.
- Zhang, M.; Viennois, E.; Prasad, M.; Zhang, Y.; Wang, L.; Zhang, Z.; Han, M.K.; Xiao, B.; Xu, C.; Srinivasan, S.; et al. Edible Ginger-Derived Nanoparticles: A Novel Therapeutic Approach for the Prevention and Treatment of Inflammatory Bowel Disease and Colitis-Associated Cancer. Biomaterials 2016, 101, 321–340.
- Jimenez-Jimenez, S.; Hashimoto, K.; Santana, O.; Aguirre, J.; Kuchitsu, K.; Cárdenas, L. Emerging Roles of Tetraspanins in Plant Inter-Cellular and Inter-Kingdom Communication. Plant Signal Behav. 2019, 14, 1581559.
- Dad, H.A.; Gu, T.W.; Zhu, A.Q.; Huang, L.Q.; Peng, L.H. Plant Exosome-like Nanovesicles: Emerging Therapeutics and Drug Delivery Nanoplatforms. Mol. Ther. 2021, 29, 13–31.
- Özkan, İ.; Koçak, P.; Yıldırım, M.; Ünsal, N.; Yılmaz, H.; Telci, D.; Şahin, F. Garlic (Allium Sativum)-Derived SEVs Inhibit Cancer Cell Proliferation and Induce Caspase Mediated Apoptosis. Sci. Rep. 2021, 11, 14773.
- Savcı, Y.; Kırbaş, O.K.; Bozkurt, B.T.; Abdik, E.A.; Taşlı, P.N.; Şahin, F.; Abdik, H. Grapefruit-Derived Extracellular Vesicles as a Promising Cell-Free Therapeutic Tool for Wound Healing. Food Funct. 2021, 12, 5144–5156.
- Pocsfalvi, G.; Turiák, L.; Ambrosone, A.; del Gaudio, P.; Puska, G.; Fiume, I.; Silvestre, T.; Vékey, K. Protein Biocargo of Citrus Fruit-Derived Vesicles Reveals Heterogeneous Transport and Extracellular Vesicle Populations. J. Plant Physiol. 2018, 229, 111–121.
- Chen, X.; Zhou, Y.; Yu, J. Exosome-like Nanoparticles from Ginger Rhizomes Inhibited NLRP3 Inflammasome Activation. Mol. Pharm. 2019, 16, 2690–2699.
- Sarvarian, P.; Samadi, P.; Gholipour, E.; Shams Asenjan, K.; Hojjat-Farsangi, M.; Motavalli, R.; Motavalli Khiavi, F.; Yousefi, M. Application of Emerging Plant-Derived Nanoparticles as a Novel Approach for Nano-Drug Delivery Systems. Immunol. Investig. 2022, 51, 1039–1059.
- Ju, S.; Mu, J.; Dokland, T.; Zhuang, X.; Wang, Q.; Jiang, H.; Xiang, X.; Deng, Z.-B.; Wang, B.; Zhang, L.; et al. Grape Exosome-like Nanoparticles Induce Intestinal Stem Cells and Protect Mice from DSS-Induced Colitis. Mol. Ther. 2013, 21, 1345–1357.
- Liu, C.; Yan, X.; Zhang, Y.; Yang, M.; Ma, Y.; Zhang, Y.; Xu, Q.; Tu, K.; Zhang, M. Oral Administration of Turmeric-Derived Exosome-like Nanovesicles with Anti-Inflammatory and pro-Resolving Bioactions for Murine Colitis Therapy. J. Nanobiotechnology 2022, 20, 206.
- Berger, E.; Colosetti, P.; Jalabert, A.; Meugnier, E.; Wiklander, O.P.B.; Jouhet, J.; Errazurig-Cerda, E.; Chanon, S.; Gupta, D.; Rautureau, G.J.P.; et al. Use of Nanovesicles from Orange Juice to Reverse Diet-Induced Gut Modifications in Diet-Induced Obese Mice. Mol. Ther. Methods Clin. Dev. 2020, 18, 880–892.
- Wang, Q.; Zhuang, X.; Mu, J.; Deng, Z.-B.; Jiang, H.; Zhang, L.; Xiang, X.; Wang, B.; Yan, J.; Miller, D.; et al. Delivery of Therapeutic Agents by Nanoparticles Made of Grapefruit-Derived Lipids. Nat. Commun. 2013, 4, 1867.
- Teng, Y.; Ren, Y.; Sayed, M.; Hu, X.; Lei, C.; Kumar, A.; Hutchins, E.; Mu, J.; Deng, Z.; Luo, C.; et al. Plant-Derived Exosomal MicroRNAs Shape the Gut Microbiota. Cell Host. Microbe. 2018, 24, 637–652.e8.
- Zhang, J.; Li, S.; Li, L.; Li, M.; Guo, C.; Yao, J.; Mi, S. Exosome and Exosomal MicroRNA: Trafficking, Sorting, and Function. Genom. Proteom. Bioinform. 2015, 13, 17–24.
- O’Brien, J.; Hayder, H.; Zayed, Y.; Peng, C. Overview of MicroRNA Biogenesis, Mechanisms of Actions, and Circulation. Front. Endocrinol. 2018, 9, 402.
- Correia de Sousa, M.; Gjorgjieva, M.; Dolicka, D.; Sobolewski, C.; Foti, M. Deciphering MiRNAs’ Action through MiRNA Editing. Int. J. Mol. Sci. 2019, 20, 6249.
- Wang, Y.; Wei, Y.; Liao, H.; Fu, H.; Yang, X.; Xiang, Q.; Zhang, S. Plant Exosome-like Nanoparticles as Biological Shuttles for Transdermal Drug Delivery. Bioengineering 2023, 10, 104.
- He, B.; Cai, Q.; Qiao, L.; Huang, C.-Y.; Wang, S.; Miao, W.; Ha, T.; Wang, Y.; Jin, H. RNA-Binding Proteins Contribute to Small RNA Loading in Plant Extracellular Vesicles. Nat. Plants 2021, 7, 342–352.
- Liu, G.; Kang, G.; Wang, S.; Huang, Y.; Cai, Q. Extracellular Vesicles: Emerging Players in Plant Defense Against Pathogens. Front. Plant Sci. 2021, 12, 757925.
- Stotz, H.U.; Brotherton, D.; Inal, J. Communication Is Key: Extracellular Vesicles as Mediators of Infection and Defence during Host-Microbe Interactions in Animals and Plants. FEMS Microbiol. Rev. 2022, 46, fuab044.
- Stanly, C.; Alfieri, M.; Ambrosone, A.; Leone, A.; Fiume, I.; Pocsfalvi, G. Grapefruit-Derived Micro and Nanovesicles Show Distinct Metabolome Profiles and Anticancer Activities in the A375 Human Melanoma Cell Line. Cells 2020, 9, 722.
- Lei, C.; Teng, Y.; He, L.; Sayed, M.; Mu, J.; Xu, F.; Zhang, X.; Kumar, A.; Sundaram, K.; Sriwastva, M.K.; et al. Lemon Exosome-like Nanoparticles Enhance Stress Survival of Gut Bacteria by RNase P-Mediated Specific TRNA Decay. iScience. 2021, 24, 102511.
- Chen, Q.; Li, Q.; Liang, Y.; Zu, M.; Chen, N.; Canup, B.S.B.; Luo, L.; Wang, C.; Zeng, L.; Xiao, B. Natural Exosome-like Nanovesicles from Edible Tea Flowers Suppress Metastatic Breast Cancer via ROS Generation and Microbiota Modulation. Acta Pharm. Sin. B 2022, 12, 907–923.
- Man, F.; Meng, C.; Liu, Y.; Wang, Y.; Zhou, Y.; Ma, J.; Lu, R. The Study of Ginger-Derived Extracellular Vesicles as a Natural Nanoscale Drug Carrier and Their Intestinal Absorption in Rats. AAPS PharmSciTech. 2021, 22, 206.
- Zhuang, X.; Deng, Z.-B.; Mu, J.; Zhang, L.; Yan, J.; Miller, D.; Feng, W.; McClain, C.J.; Zhang, H.-G. Ginger-Derived Nanoparticles Protect against Alcohol-Induced Liver Damage. J. Extracell. Vesicles 2015, 4, 28713.
- Hadizadeh, N.; Bagheri, D.; Shamsara, M.; Hamblin, M.R.; Farmany, A.; Xu, M.; Liang, Z.; Razi, F.; Hashemi, E. Extracellular Vesicles Biogenesis, Isolation, Manipulation and Genetic Engineering for Potential in Vitro and in Vivo Therapeutics: An Overview. Front. Bioeng. Biotechnol. 2022, 10, 1019821.
- Li, P.; Kaslan, M.; Lee, S.H.; Yao, J.; Gao, Z. Progress in Exosome Isolation Techniques. Theranostics 2017, 7, 789–804.
- Bosque, A.; Dietz, L.; Gallego-Lleyda, A.; Sanclemente, M.; Iturralde, M.; Naval, J.; Alava, M.A.; Martínez-Lostao, L.; Thierse, H.-J.; Anel, A. Comparative Proteomics of Exosomes Secreted by Tumoral Jurkat T Cells and Normal Human T Cell Blasts Unravels a Potential Tumorigenic Role for Valosin-Containing Protein. Oncotarget 2016, 7, 29287–29305.
- Sidhom, K.; Obi, P.O.; Saleem, A. A Review of Exosomal Isolation Methods: Is Size Exclusion Chromatography the Best Option? Int. J. Mol. Sci. 2020, 21, 466.
- Livshts, M.A.; Khomyakova, E.; Evtushenko, E.G.; Lazarev, V.N.; Kulemin, N.A.; Semina, S.E.; Generozov, E.v.; Govorun, V.M. Isolation of Exosomes by Differential Centrifugation: Theoretical Analysis of a Commonly Used Protocol. Sci. Rep. 2015, 5, 17319.
- Subudhi, P.D.; Bihari, C.; Sarin, S.K.; Baweja, S. Emerging Role of Edible Exosomes-Like Nanoparticles (ELNs) as Hepatoprotective Agents. Nanotheranostics 2022, 6, 365–375.
- Linares, R.; Tan, S.; Gounou, C.; Arraud, N.; Brisson, A.R. High-Speed Centrifugation Induces Aggregation of Extracellular Vesicles. J. Extracell. Vesicles 2015, 4, 29509.
- Street, J.M.; Barran, P.E.; Mackay, C.L.; Weidt, S.; Balmforth, C.; Walsh, T.S.; Chalmers, R.T.A.; Webb, D.J.; Dear, J.W. Identification and Proteomic Profiling of Exosomes in Human Cerebrospinal Fluid. J. Transl. Med. 2012, 10, 5.
- Szatanek, R.; Baran, J.; Siedlar, M.; Baj-Krzyworzeka, M. Isolation of Extracellular Vesicles: Determining the Correct Approach (Review). Int. J. Mol. Med. 2015, 36, 11–17.
- Yu, L.L.; Zhu, J.; Liu, J.X.; Jiang, F.; Ni, W.K.; Qu, L.S.; Ni, R.Z.; Lu, C.H.; Xiao, M.B. A Comparison of Traditional and Novel Methods for the Separation of Exosomes from Human Samples. Biomed. Res. Int. 2018, 2018, 3634563.
- Ebert, B.; Rai, A.J. Isolation and Characterization of Amniotic Fluid-Derived Extracellular Vesicles for Biomarker Discovery. In Methods in Molecular Biology; Humana Press Inc.: Totova, NJ, USA, 2019; Volume 1885, pp. 287–294.
- Alexander, R.P.; Chiou, N.-T.; Ansel, K.M. Improved Exosome Isolation by Sucrose Gradient Fractionation of Ultracentrifuged Crude Exosome Pellets. Protoc. Exch. 2016, 1–4.
- Tauro, B.J.; Greening, D.W.; Mathias, R.A.; Ji, H.; Mathivanan, S.; Scott, A.M.; Simpson, R.J. Comparison of Ultracentrifugation, Density Gradient Separation, and Immunoaffinity Capture Methods for Isolating Human Colon Cancer Cell Line LIM1863-Derived Exosomes. Methods 2012, 56, 293–304.
- Lobb, R.J.; Becker, M.; Wen, S.W.; Wong, C.S.F.; Wiegmans, A.P.; Leimgruber, A.; Möller, A. Optimized Exosome Isolation Protocol for Cell Culture Supernatant and Human Plasma. J. Extracell. Vesicles 2015, 4, 27031.
- Konoshenko, M.Y.; Lekchnov, E.A.; Vlassov, A.v.; Laktionov, P.P. Isolation of Extracellular Vesicles: General Methodologies and Latest Trends. Biomed. Res. Int. 2018, 2018, 8545347.
- van Deun, J.; Mestdagh, P.; Agostinis, P.; Akay, Ö.; Anand, S.; Anckaert, J.; Martinez, Z.A.; Baetens, T.; Beghein, E.; Bertier, L.; et al. EV-TRACK: Transparent Reporting and Centralizing Knowledge in Extracellular Vesicle Research. Nat. Methods 2017, 14, 228–232.
- Zhao, L.; Gu, C.; Gan, Y.; Shao, L.; Chen, H.; Zhu, H. Exosome-Mediated SiRNA Delivery to Suppress Postoperative Breast Cancer Metastasis. J. Control. Release 2020, 318, 1–15.
- Vergauwen, G.; Dhondt, B.; van Deun, J.; de Smedt, E.; Berx, G.; Timmerman, E.; Gevaert, K.; Miinalainen, I.; Cocquyt, V.; Braems, G.; et al. Confounding Factors of Ultrafiltration and Protein Analysis in Extracellular Vesicle Research. Sci. Rep. 2017, 7, 2704.
- Böing, A.N.; van der Pol, E.; Grootemaat, A.E.; Coumans, F.A.W.; Sturk, A.; Nieuwland, R. Single-Step Isolation of Extracellular Vesicles by Size-Exclusion Chromatography. J. Extracell. Vesicles 2014, 3, 23430.
- Gámez-Valero, A.; Monguió-Tortajada, M.; Carreras-Planella, L.; Franquesa, M.; Beyer, K.; Borràs, F.E. Size-Exclusion Chromatography-Based Isolation Minimally Alters Extracellular Vesicles’ Characteristics Compared to Precipitating Agents. Sci. Rep. 2016, 6, 33641.
- Chen, Q.; Wu, D.; Wang, Y.; Chen, Z. Exosomes as Novel Delivery Systems for Application in Traditional Chinese Medicine. Molecules 2022, 27, 7789.
- Gercel-Taylor, C.; Atay, S.; Tullis, R.H.; Kesimer, M.; Taylor, D.D. Nanoparticle Analysis of Circulating Cell-Derived Vesicles in Ovarian Cancer Patients. Anal. Biochem. 2012, 428, 44–53.
- Zhang, H.; Lyden, D. Asymmetric-Flow Field-Flow Fractionation Technology for Exomere and Small Extracellular Vesicle Separation and Characterization. Nat. Protoc. 2019, 14, 1027–1053.
- Lewis, G.D.; Metcalf, T.G. Polyethylene Glycol Precipitation for Recovery of Pathogenic Viruses, Including Hepatitis A Virus and Human Rotavirus, from Oyster, Water, and Sediment Samples. Appl. Env. Microbiol. 1988, 54, 1983–1988.
- Yamamoto, K.R.; Alberts, B.M.; Benzinger, R.; Lawhorne, L.; Treiber, G. Rapid Bacteriophage Sedimentation in the Presence of Polyethylene Glycol and Its Application to Large-Scale Virus Purification. Virology 1970, 40, 734–744.
- Oh, D.K.; Hyun, C.K.; Kim, J.H.; Park, Y.H. Production of Penicillin in a Fluidized-Bed Bioreactor: Control of Cell Growth and Penicillin Production by Phosphate Limitation. Biotechnol. Bioeng. 1988, 32, 569–573.
- Tian, J.; Casella, G.; Zhang, Y.; Rostami, A.; Li, X. Potential Roles of Extracellular Vesicles in the Pathophysiology, Diagnosis, and Treatment of Autoimmune Diseases. Int. J. Biol. Sci. 2020, 16, 620–632.
- Rider, M.A.; Hurwitz, S.N.; Meckes, D.G. ExtraPEG: A Polyethylene Glycol-Based Method for Enrichment of Extracellular Vesicles. Sci. Rep. 2016, 6, 23978.
- Kalarikkal, S.P.; Prasad, D.; Kasiappan, R.; Chaudhari, S.R.; Sundaram, G.M. A Cost-Effective Polyethylene Glycol-Based Method for the Isolation of Functional Edible Nanoparticles from Ginger Rhizomes. Sci. Rep. 2020, 10, 4456.
- Zarovni, N.; Corrado, A.; Guazzi, P.; Zocco, D.; Lari, E.; Radano, G.; Muhhina, J.; Fondelli, C.; Gavrilova, J.; Chiesi, A. Integrated Isolation and Quantitative Analysis of Exosome Shuttled Proteins and Nucleic Acids Using Immunocapture Approaches. Methods 2015, 87, 46–58.
- Koliha, N.; Wiencek, Y.; Heider, U.; Jüngst, C.; Kladt, N.; Krauthäuser, S.; Johnston, I.C.D.; Bosio, A.; Schauss, A.; Wild, S. A Novel Multiplex Bead-Based Platform Highlights the Diversity of Extracellular Vesicles. J. Extracell. Vesicles 2016, 5, 29975.
- Boriachek, K.; Masud, M.K.; Palma, C.; Phan, H.P.; Yamauchi, Y.; Hossain, M.S.A.; Nguyen, N.T.; Salomon, C.; Shiddiky, M.J.A. Avoiding Pre-Isolation Step in Exosome Analysis: Direct Isolation and Sensitive Detection of Exosomes Using Gold-Loaded Nanoporous Ferric Oxide Nanozymes. Anal. Chem. 2019, 91, 3827–3834.
- Ghosh, A.; Davey, M.; Chute, I.C.; Griffiths, S.G.; Lewis, S.; Chacko, S.; Barnett, D.; Crapoulet, N.; Fournier, S.; Joy, A.; et al. Rapid Isolation of Extracellular Vesicles from Cell Culture and Biological Fluids Using a Synthetic Peptide with Specific Affinity for Heat Shock Proteins. PLoS ONE 2014, 9, 110443.
- Balaj, L.; Atai, N.A.; Chen, W.; Mu, D.; Tannous, B.A.; Breakefield, X.O.; Skog, J.; Maguire, C.A. Heparin Affinity Purification of Extracellular Vesicles. Sci. Rep. 2015, 5, 10266.
- Zhou, Y.G.; Mohamadi, R.M.; Poudineh, M.; Kermanshah, L.; Ahmed, S.; Safaei, T.S.; Stojcic, J.; Nam, R.K.; Sargent, E.H.; Kelley, S.O. Interrogating Circulating Microsomes and Exosomes Using Metal Nanoparticles. Small 2016, 12, 727–732.
- Reiner, A.T.; Witwer, K.W.; van Balkom, B.W.M.; de Beer, J.; Brodie, C.; Corteling, R.L.; Gabrielsson, S.; Gimona, M.; Ibrahim, A.G.; de Kleijn, D.; et al. Concise Review: Developing Best-Practice Models for the Therapeutic Use of Extracellular Vesicles. Stem Cells Transl. Med. 2017, 6, 1730–1739.
- Théry, C.; Clayton, A.; Amigorena, S.; Raposo, G. Isolation and Characterization of Exosomes from Cell Culture Supernatants and Biological Fluids. Curr. Protoc. Cell Biol. 2006, 30, 3.22.1–3.22.29.
- Wang, Z.; Wu, H.J.; Fine, D.; Schmulen, J.; Hu, Y.; Godin, B.; Zhang, J.X.J.; Liu, X. Ciliated Micropillars for the Microfluidic-Based Isolation of Nanoscale Lipid Vesicles. Lab. Chip. 2013, 13, 2879–2882.
- Wu, M.; Ouyang, Y.; Wang, Z.; Zhang, R.; Huang, P.H.; Chen, C.; Li, H.; Li, P.; Quinn, D.; Dao, M.; et al. Isolation of Exosomes from Whole Blood by Integrating Acoustics and Microfluidics. Proc. Natl. Acad. Sci. USA 2017, 114, 10584–10589.
- Chen, J.; Li, P.; Zhang, T.; Xu, Z.; Huang, X.; Wang, R.; Du, L. Review on Strategies and Technologies for Exosome Isolation and Purification. Front. Bioeng. Biotechnol. 2022, 9, 811971.
- Helwa, I.; Cai, J.; Drewry, M.D.; Zimmerman, A.; Dinkins, M.B.; Khaled, M.L.; Seremwe, M.; Dismuke, W.M.; Bieberich, E.; Stamer, W.D.; et al. A Comparative Study of Serum Exosome Isolation Using Differential Ultracentrifugation and Three Commercial Reagents. PLoS ONE 2017, 12, 0170628.
- Martins, T.S.; Catita, J.; Rosa, I.M.; da Cruz e Silva, O.A.B.; Henriques, A.G. Exosome Isolation from Distinct Biofluids Using Precipitation and Column-Based Approaches. PLoS ONE 2018, 13, 198820.
- Zhang, M.; Jin, K.; Gao, L.; Zhang, Z.; Li, F.; Zhou, F.; Zhang, L. Methods and Technologies for Exosome Isolation and Characterization. Small Methods 2018, 2, 21.
- van der Pol, E.; Hoekstra, A.G.; Sturk, A.; Otto, C.; van Leeuwen, T.G.; Nieuwland, R. Optical and Non-Optical Methods for Detection and Characterization of Microparticles and Exosomes. J. Thromb. Haemost. 2010, 8, 2596–2607.
- Pisitkun, T.; Shen, R.-F.; Knepper, M.A. Identification and Proteomic Profiling of Exosomes in Human Urine. Proc. Natl. Acad. Sci. USA 2004, 101, 13368–13373.
- Wu, Y.; Deng, W.; Klinke, D.J. Exosomes: Improved Methods to Characterize Their Morphology, RNA Content, and Surface Protein Biomarkers. Analyst 2015, 140, 6631–6642.
- György, B.; Szabó, T.G.; Pásztói, M.; Pál, Z.; Misják, P.; Aradi, B.; László, V.; Pállinger, É.; Pap, E.; Kittel, Á.; et al. Membrane Vesicles, Current State-of-the-Art: Emerging Role of Extracellular Vesicles. Cell. Mol. Life Sci. 2011, 68, 2667–2688.
- Raposo, G.; Stoorvogel, W. Extracellular Vesicles: Exosomes, Microvesicles, and Friends. J. Cell Biol. 2013, 200, 373–383.
- Maas, S.L.N.; de Vrij, J.; van der Vlist, E.J.; Geragousian, B.; van Bloois, L.; Mastrobattista, E.; Schiffelers, R.M.; Wauben, M.H.M.; Broekman, M.L.D.; Nolte-’T Hoen, E.N.M. Possibilities and Limitations of Current Technologies for Quantification of Biological Extracellular Vesicles and Synthetic Mimics. J. Control. Release 2015, 200, 87–96.
- Maas, S.L.N.; de Vrij, J.; Broekman, M.L.D. Quantification and Size-Profiling of Extracellular Vesicles Using Tunable Resistive Pulse Sensing. J. Vis. Exp 2014, 92, 51623.
- Shao, H.; Im, H.; Castro, C.M.; Breakefield, X.; Weissleder, R.; Lee, H. New Technologies for Analysis of Extracellular Vesicles. Chem. Rev. 2018, 118, 1917–1950.
- Zhang, Y.; Liu, Y.; Liu, H.; Tang, W.H. Exosomes: Biogenesis, Biologic Function and Clinical Potential. Cell Biosci. 2019, 9, 19.
- Jeyaram, A.; Jay, S.M. Preservation and Storage Stability of Extracellular Vesicles for Therapeutic Applications. AAPS J. 2018, 20, 1.
- Maroto, R.; Zhao, Y.; Jamaluddin, M.; Popov, V.L.; Wang, H.; Kalubowilage, M.; Zhang, Y.; Luisi, J.; Sun, H.; Culbertson, C.T.; et al. Effects of Storage Temperature on Airway Exosome Integrity for Diagnostic and Functional Analyses. J. Extracell. Vesicles 2017, 6, 1359478.
- Madison, M.N.; Jones, P.H.; Okeoma, C.M. Exosomes in Human Semen Restrict HIV-1 Transmission by Vaginal Cells and Block Intravaginal Replication of LP-BM5 Murine AIDS Virus Complex. Virology 2015, 482, 189–201.
- Welch, J.L.; Madison, M.N.; Margolick, J.B.; Galvin, S.; Gupta, P.; Martínez-Maza, O.; Dash, C.; Okeoma, C.M. Effect of Prolonged Freezing of Semen on Exosome Recovery and Biologic Activity. Sci. Rep. 2017, 7, 45034.
- Yuana, Y.; Böing, A.N.; Grootemaat, A.E.; van der Pol, E.; Hau, C.M.; Cizmar, P.; Buhr, E.; Sturk, A.; Nieuwland, R. Handling and Storage of Human Body Fluids for Analysis of Extracellular Vesicles. J. Extracell. Vesicles 2015, 4, 29260.
- Oosthuyzen, W.; Sime, N.E.L.; Ivy, J.R.; Turtle, E.J.; Street, J.M.; Pound, J.; Bath, L.E.; Webb, D.J.; Gregory, C.D.; Bailey, M.A.; et al. Quantification of Human Urinary Exosomes by Nanoparticle Tracking Analysis. J. Physiol. 2013, 591, 5833–5842.
- Sivanantham, A.; Jin, Y. Impact of Storage Conditions on EV Integrity/Surface Markers and Cargos. Life 2022, 12, 697.
- Bahr, M.M.; Amer, M.S.; Abo-El-Sooud, K.; Abdallah, A.N.; El-Tookhy, O.S. Preservation Techniques of Stem Cells Extracellular Vesicles: A Gate for Manufacturing of Clinical Grade Therapeutic Extracellular Vesicles and Long-Term Clinical Trials. Int. J. Vet. Sci. Med. 2020, 8, 1704992.
- Kusuma, G.D.; Barabadi, M.; Tan, J.L.; Morton, D.A.V.; Frith, J.E.; Lim, R. To Protect and to Preserve: Novel Preservation Strategies for Extracellular Vesicles. Front. Pharm. 2018, 9, 1199.
- Budgude, P.; Kale, V.; Vaidya, A. Cryopreservation of Mesenchymal Stromal Cell-Derived Extracellular Vesicles Using Trehalose Maintains Their Ability to Expand Hematopoietic Stem Cells in Vitro. Cryobiology 2021, 98, 152–163.
- Gelibter, S.; Marostica, G.; Mandelli, A.; Siciliani, S.; Podini, P.; Finardi, A.; Furlan, R. The Impact of Storage on Extracellular Vesicles: A Systematic Study. J. Extracell. Vesicles 2022, 11, 12162.
- Bosch, S.; de Beaurepaire, L.; Allard, M.; Mosser, M.; Heichette, C.; Chrétien, D.; Jegou, D.; Bach, J.M. Trehalose Prevents Aggregation of Exosomes and Cryodamage. Sci. Rep. 2016, 6, 36162.
- Kreke, M.; Smith, R.; Hanscome, P.; Peck, K.; Ibrahim, A. Processes for Producing Stable Exosome Formulations. US Patent US20160158291A, 3 December 2015.
- Charoenviriyakul, C.; Takahashi, Y.; Nishikawa, M.; Takakura, Y. Preservation of Exosomes at Room Temperature Using Lyophilization. Int. J. Pharm. 2018, 553, 32.
- Richter, M.; Fuhrmann, K.; Fuhrmann, G. Evaluation of the Storage Stability of Extracellular Vesicles. J. Vis. Exp. 2019, 2019, 1–9.
- el Baradie, K.B.Y.; Nouh, M.; O’Brien, F.; Liu, Y.; Fulzele, S.; Eroglu, A.; Hamrick, M.W. Freeze-Dried Extracellular Vesicles From Adipose-Derived Stem Cells Prevent Hypoxia-Induced Muscle Cell Injury. Front. Cell Dev. Biol. 2020, 8, 181.
- Raimondo, S.; Naselli, F.; Fontana, S.; Monteleone, F.; lo Dico, A.; Saieva, L.; Zito, G.; Flugy, A.; Manno, M.; di Bella, M.A.; et al. Citrus Limon-Derived Nanovesicles Inhibit Cancer Cell Proliferation and Suppress CML Xenograft Growth by Inducing TRAIL-Mediated Cell Death. Oncotarget 2015, 6, 19514–19527.
- Rezaie, J.; Feghhi, M.; Etemadi, T. A Review on Exosomes Application in Clinical Trials: Perspective, Questions, and Challenges. Cell Commun. Signal 2022, 20, 145.
- Chen, Y.S.; Lin, E.Y.; Chiou, T.W.; Harn, H.J. Exosomes in Clinical Trial and Their Production in Compliance with Good Manufacturing Practice. Tzu. Chi. Med. J. 2020, 32, 113–120.
- Teng, Y.; Xu, F.; Zhang, X.; Mu, J.; Sayed, M.; Hu, X.; Lei, C.; Sriwastva, M.; Kumar, A.; Sundaram, K.; et al. Plant-Derived Exosomal MicroRNAs Inhibit Lung Inflammation Induced by Exosomes SARS-CoV-2 Nsp12. Mol. Ther. 2021, 29, 2424–2440.
More
Information
Subjects:
Dentistry, Oral Surgery & Medicine
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
3.2K
Revisions:
2 times
(View History)
Update Date:
04 May 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




