
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Cyril Fersing | -- | 3086 | 2023-03-28 17:38:50 | | | |
| 2 | Lindsay Dong | Meta information modification | 3086 | 2023-03-30 02:45:34 | | |
Video Upload Options
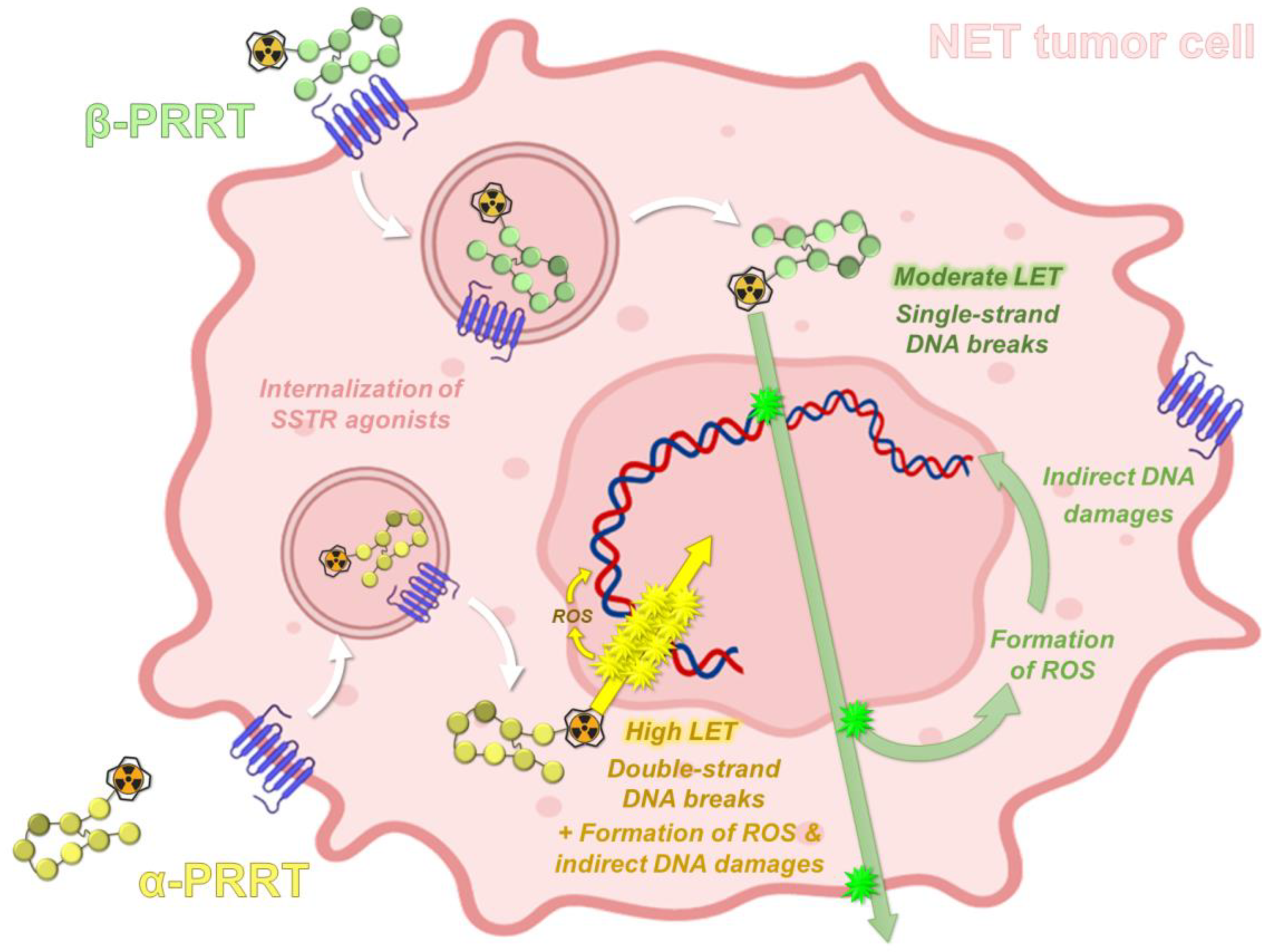
The widespread use of peptide receptor radionuclide therapy (PRRT) represents a major therapeutic breakthrough in nuclear medicine, particularly since the introduction of 177Lu-radiolabeled somatostatin analogs. These radiopharmaceuticals have especially improved progression-free survival and quality of life in patients with inoperable metastatic gastroenteropancreatic neuroendocrine tumors expressing somatostatin receptors. In the case of aggressive or resistant disease, the use of somatostatin derivatives radiolabeled with an alpha-emitter could provide a promising alternative. Among the currently available alpha-emitting radioelements, actinium-225 has emerged as the most suitable candidate, especially regarding its physical and radiochemical properties.
1. Introduction
1.1. About Neuroendocrine Tumors
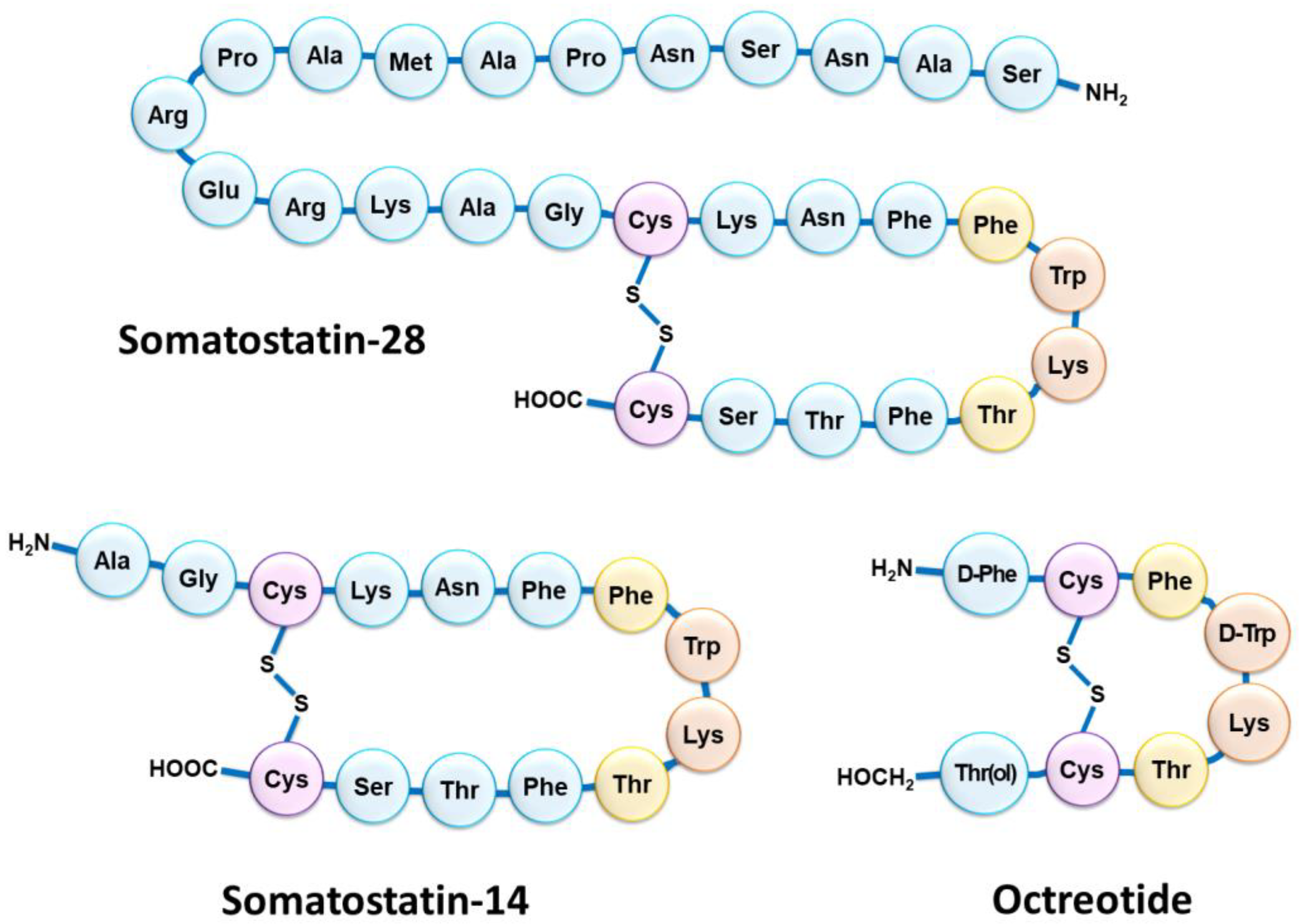
1.2. Somatostatin Receptors and Octreotide Analogs
1.3. SSTR Targeting for Peptide Receptor Radionuclide Therapy
1.4. PRRT Using Somatostatin Analogs Radiolabeled with Alpha-Emitters
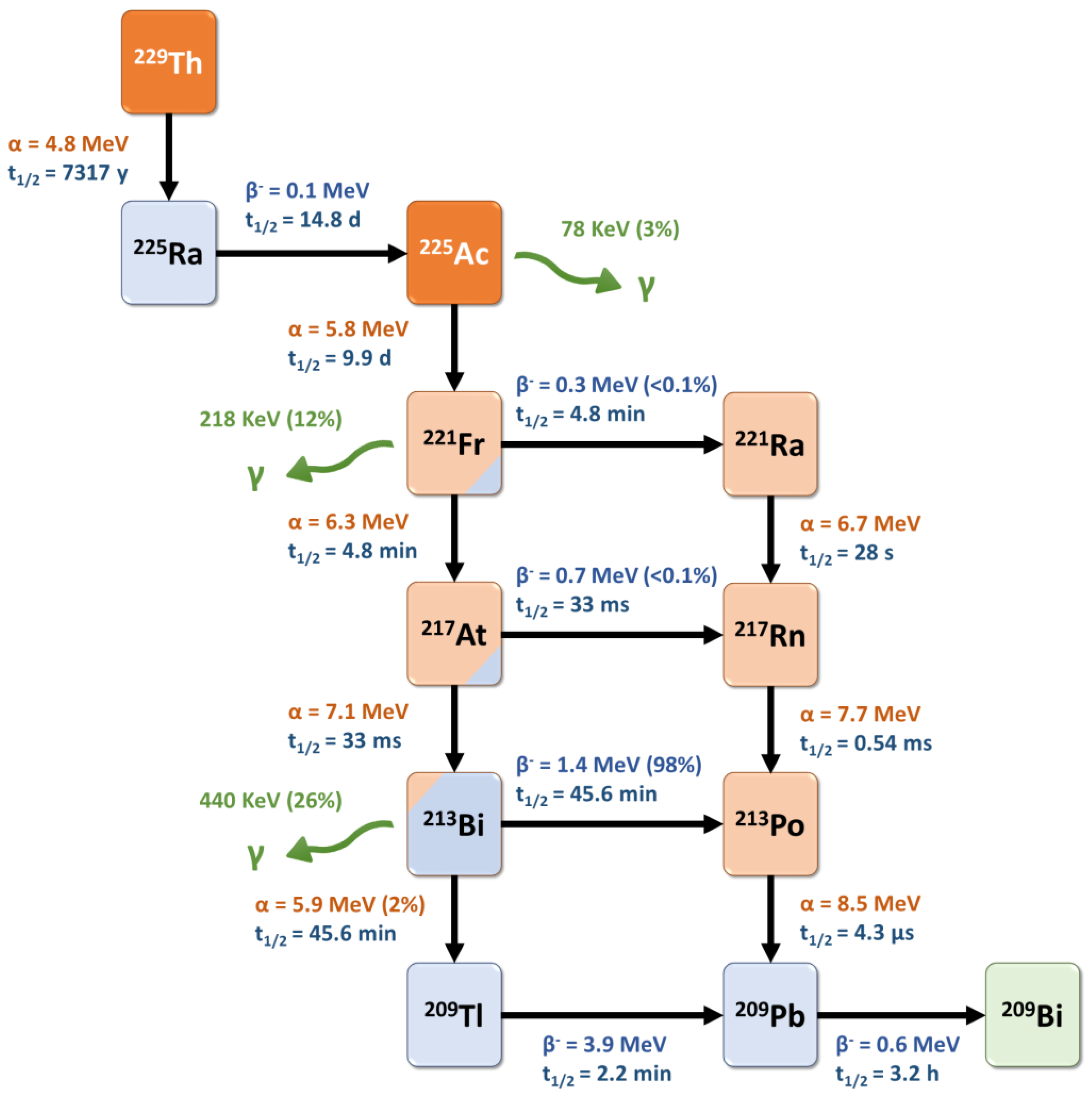
2. Actinium-225: Decay Characteristics, Radiobiological and Dosimetry Considerations
2.1. Physical Properties of Actinium-225
2.2. Radiobiological Properties of Actinium-225
2.3. Dosimetry for Targeted Alpha-Therapy with 225Ac
3. Radiochemical and Preclinical Development of [225Ac]Ac–DOTATATE
3.1. Production of Actinium-225
3.2. Chemistry of Actinium
3.2.1. Actinium in Aqueous Solution
3.2.2. Coordination Chemistry of Actinium
3.2.3. Relevance of DOTA in Actinium Radiopharmaceuticals
3.3. Somatostatin Analogs Radiolabeled with 225Ac: Preclinical Studies
Only a few studies have reported preclinical efficacy results of 225Ac-radiolabeled somatostatin analogues, due to this group of vector molecules having already been widely studied with beta-emitters such as 90Y or 177Lu [70].
Activities between 10 and 60 kBq were well-tolerated by the mice; however, activities over 30 kBq induced pathologic changes in the renal cortex, suggesting radiation-induced acute tubular necrosis in both the distal and proximal tubules. Similar results were obtained in another study on Sprague Dawley rats that received 111 or 370 kBq [225Ac]Ac–DOTATOC and developed renal tubular nephrosis or renal glomerulopathy [71]. Only a slight accumulation in the liver was objectified, probably due to the release of free 225Ac. After a single administration of the highest non-toxic activity (20 kBq), tumor weights 14 days after treatment were lower with [225Ac]Ac–DOTATOC than with [177Lu]Lu–DOTATOC (1 MBq), in accordance with previous studies investigating [213Bi]Bi–DOTATOC [30][31].
4. Clinical Use of 225Ac–DOTATATE
5. Conclusions
References
- Basu, B.; Sirohi, B.; Corrie, P. Systemic Therapy for Neuroendocrine Tumours of Gastroenteropancreatic Origin. Endocr. Relat. Cancer 2010, 17, R75–R90.
- Scalettar, B.A.; Jacobs, C.; Fulwiler, A.; Prahl, L.; Simon, A.; Hilken, L.; Lochner, J.E. Hindered Submicron Mobility and Long-Term Storage of Presynaptic Dense-Core Granules Revealed by Single-Particle Tracking. Dev. Neurobiol. 2012, 72, 1181–1195.
- Kaltsas, G.A.; Besser, G.M.; Grossman, A.B. The Diagnosis and Medical Management of Advanced Neuroendocrine Tumors. Endocr. Rev. 2004, 25, 458–511.
- Hankus, J.; Tomaszewska, R. Neuroendocrine Neoplasms and Somatostatin Receptor Subtypes Expression. Nucl. Med. Rev. 2016, 19, 111–117.
- Reubi, J.C.; Waser, B.; Schaer, J.C.; Laissue, J.A. Somatostatin Receptor Sst1-Sst5 Expression in Normal and Neoplastic Human Tissues Using Receptor Autoradiography with Subtype-Selective Ligands. Eur. J. Nucl. Med. 2001, 28, 836–846.
- Schaer, J.C.; Waser, B.; Mengod, G.; Reubi, J.C. Somatostatin Receptor Subtypes Sst1, Sst2, Sst3 and Sst5 Expression in Human Pituitary, Gastroentero-Pancreatic and Mammary Tumors: Comparison of MRNA Analysis with Receptor Autoradiography. Int. J. Cancer 1997, 70, 530–537.
- Reubi, J.C. Peptide Receptors as Molecular Targets for Cancer Diagnosis and Therapy. Endocr. Rev. 2003, 24, 389–427.
- Böhlen, P.; Brazeau, P.; Benoit, R.; Ling, N.; Esch, F.; Guillemin, R. Isolation and Amino Acid Composition of Two Somatostatin-like Peptides from Ovine Hypothalamus: Somatostatin-28 and Somatostatin-25. Biochem. Biophys. Res. Commun. 1980, 96, 725–734.
- Shen, L.P.; Pictet, R.L.; Rutter, W.J. Human Somatostatin I: Sequence of the CDNA. Proc. Natl. Acad. Sci. USA 1982, 79, 4575–4579.
- Rai, U.; Thrimawithana, T.R.; Valery, C.; Young, S.A. Therapeutic Uses of Somatostatin and Its Analogues: Current View and Potential Applications. Pharmacol. Ther. 2015, 152, 98–110.
- Veber, D.F.; Holly, F.W.; Nutt, R.F.; Bergstrand, S.J.; Brady, S.F.; Hirschmann, R.; Glitzer, M.S.; Saperstein, R. Highly Active Cyclic and Bicyclic Somatostatin Analogues of Reduced Ring Size. Nature 1979, 280, 512–514.
- Veber, D.F.; Freidlinger, R.M.; Perlow, D.S.; Paleveda, W.J.; Holly, F.W.; Strachan, R.G.; Nutt, R.F.; Arison, B.H.; Homnick, C.; Randall, W.C.; et al. A Potent Cyclic Hexapeptide Analogue of Somatostatin. Nature 1981, 292, 55–58.
- Bauer, W.; Briner, U.; Doepfner, W.; Haller, R.; Huguenin, R.; Marbach, P.; Petcher, T.J.; Pless, J. SMS 201-995: A Very Potent and Selective Octapeptide Analogue of Somatostatin with Prolonged Action. Life Sci. 1982, 31, 1133–1140.
- Al-Toubah, T.; Strosberg, J. Peptide Receptor Radiotherapy Comes of Age. Endocrinol. Metab. Clin. N. Am. 2018, 47, 615–625.
- Krenning, E.P.; Kooij, P.P.; Bakker, W.H.; Breeman, W.A.; Postema, P.T.; Kwekkeboom, D.J.; Oei, H.Y.; de Jong, M.; Visser, T.J.; Reijs, A.E. Radiotherapy with a Radiolabeled Somatostatin Analogue, -Octreotide. A Case History. Ann. N. Y. Acad. Sci. 1994, 733, 496–506.
- Krenning, E.P.; Kooij, P.P.M.; Pauwels, S.; Breeman, W.A.P.; Postema, P.T.E.; DeHerder, W.W.; Valkema, R.; Kwekkeboom, D.J. Somatostatin Receptor: Scintigraphy and Radionuclide Therapy. Digestion 1996, 57, 57–61.
- Krenning, E.P.; de Jong, M.; Kooij, P.P.M.; Breeman, W.A.P.; Bakker, W.H.; de Herder, W.W.; van Eijck, C.H.J.; Kwekkeboom, D.J.; Jamar, F.; Pauwels, S.; et al. Radiolabelled Somatostatin Analogue(s) for Peptide Receptor Scintigraphy and Radionuclide Therapy. Ann. Oncol. 1999, 10, S23–S30.
- Valkema, R.; De Jong, M.; Bakker, W.H.; Breeman, W.A.P.; Kooij, P.P.M.; Lugtenburg, P.J.; De Jong, F.H.; Christiansen, A.; Kam, B.L.R.; De Herder, W.W.; et al. Phase I Study of Peptide Receptor Radionuclide Therapy with Octreotide: The Rotterdam Experience. Semin. Nucl. Med. 2002, 32, 110–122.
- Cybulla, M.; Weiner, S.; Otte, A. End-Stage Renal Disease after Treatment with 90Y-DOTATOC. Eur. J. Nucl. Med. Mol. Imaging 2001, 28, 1552–1554.
- Valkema, R.; Pauwels, S.; Kvols, L.K.; Barone, R.; Jamar, F.; Bakker, W.H.; Kwekkeboom, D.J.; Bouterfa, H.; Krenning, E.P. Survival and Response after Peptide Receptor Radionuclide Therapy with Octreotide in Patients with Advanced Gastroenteropancreatic Neuroendocrine Tumors. Semin. Nucl. Med. 2006, 36, 147–156.
- Bushnell, D.L.; O’Dorisio, T.M.; O’Dorisio, M.S.; Menda, Y.; Hicks, R.J.; Van Cutsem, E.; Baulieu, J.-L.; Borson-Chazot, F.; Anthony, L.; Benson, A.B.; et al. 90Y-Edotreotide for Metastatic Carcinoid Refractory to Octreotide. J. Clin. Oncol. 2010, 28, 1652–1659.
- Imhof, A.; Brunner, P.; Marincek, N.; Briel, M.; Schindler, C.; Rasch, H.; Mäcke, H.R.; Rochlitz, C.; Müller-Brand, J.; Walter, M.A. Response, Survival, and Long-Term Toxicity after Therapy with the Radiolabeled Somatostatin Analogue -TOC in Metastasized Neuroendocrine Cancers. J. Clin. Oncol. 2011, 29, 2416–2423.
- Kwekkeboom, D.J.; Bakker, W.H.; Kooij, P.P.; Konijnenberg, M.W.; Srinivasan, A.; Erion, J.L.; Schmidt, M.A.; Bugaj, J.L.; de Jong, M.; Krenning, E.P. Octreotate: Comparison with Octreotide in Patients. Eur. J. Nucl. Med. 2001, 28, 1319–1325.
- Kam, B.L.R.; Teunissen, J.J.M.; Krenning, E.P.; de Herder, W.W.; Khan, S.; van Vliet, E.I.; Kwekkeboom, D.J. Lutetium-Labelled Peptides for Therapy of Neuroendocrine Tumours. Eur. J. Nucl. Med. Mol. Imaging 2012, 39, 103–112.
- McClellan, K.; Chen, E.Y.; Kardosh, A.; Lopez, C.D.; Del Rivero, J.; Mallak, N.; Rocha, F.G.; Koethe, Y.; Pommier, R.; Mittra, E.; et al. Therapy Resistant Gastroenteropancreatic Neuroendocrine Tumors. Cancers 2022, 14, 4769.
- Krenning, E.P.; Kwekkeboom, D.J.; Valkema, R.; Pauwels, S.; Kvols, L.K.; Jong, M. Peptide Receptor Radionuclide Therapy. Ann. N. Y. Acad. Sci. 2004, 1014, 234–245.
- Navalkissoor, S.; Grossman, A. Targeted Alpha Particle Therapy for Neuroendocrine Tumours: The Next Generation of Peptide Receptor Radionuclide Therapy. Neuroendocrinology 2019, 108, 256–264.
- Parker, C.; Nilsson, S.; Heinrich, D.; Helle, S.I.; O’Sullivan, J.M.; Fosså, S.D.; Chodacki, A.; Wiechno, P.; Logue, J.; Seke, M.; et al. Alpha Emitter Radium-223 and Survival in Metastatic Prostate Cancer. N. Engl. J. Med. 2013, 369, 213–223.
- Eychenne, R.; Chérel, M.; Haddad, F.; Guérard, F.; Gestin, J.-F. Overview of the Most Promising Radionuclides for Targeted Alpha Therapy: The “Hopeful Eight”. Pharmaceutics 2021, 13, 906.
- Norenberg, J.P.; Krenning, B.J.; Konings, I.R.H.M.; Kusewitt, D.F.; Nayak, T.K.; Anderson, T.L.; de Jong, M.; Garmestani, K.; Brechbiel, M.W.; Kvols, L.K. 213Bi-Octreotide Peptide Receptor Radionuclide Therapy of Pancreatic Tumors in a Preclinical Animal Model. Clin. Cancer Res. 2006, 12, 897–903.
- Nayak, T.K.; Norenberg, J.P.; Anderson, T.L.; Prossnitz, E.R.; Stabin, M.G.; Atcher, R.W. Somatostatin-Receptor-Targeted Alpha-Emitting 213Bi Is Therapeutically More Effective than Beta(-)-Emitting 177Lu in Human Pancreatic Adenocarcinoma Cells. Nucl. Med. Biol. 2007, 34, 185–193.
- Chan, H.S.; Konijnenberg, M.W.; de Blois, E.; Koelewijn, S.; Baum, R.P.; Morgenstern, A.; Bruchertseifer, F.; Breeman, W.A.; de Jong, M. Influence of Tumour Size on the Efficacy of Targeted Alpha Therapy with 213Bi--Octreotate. EJNMMI Res. 2016, 6, 6.
- Chan, H.S.; Konijnenberg, M.W.; Daniels, T.; Nysus, M.; Makvandi, M.; de Blois, E.; Breeman, W.A.; Atcher, R.W.; de Jong, M.; Norenberg, J.P. Improved Safety and Efficacy of 213Bi-DOTATATE-Targeted Alpha Therapy of Somatostatin Receptor-Expressing Neuroendocrine Tumors in Mice Pre-Treated with l-Lysine. EJNMMI Res. 2016, 6, 83.
- Kratochwil, C.; Giesel, F.L.; Bruchertseifer, F.; Mier, W.; Apostolidis, C.; Boll, R.; Murphy, K.; Haberkorn, U.; Morgenstern, A. 213Bi-DOTATOC Receptor-Targeted Alpha-Radionuclide Therapy Induces Remission in Neuroendocrine Tumours Refractory to Beta Radiation: A First-in-Human Experience. Eur. J. Nucl. Med. Mol. Imaging 2014, 41, 2106–2119.
- Morgenstern, A.; Apostolidis, C.; Kratochwil, C.; Sathekge, M.; Krolicki, L.; Bruchertseifer, F. An Overview of Targeted Alpha Therapy with 225Actinium and 213Bismuth. CRP 2018, 11, 200–208.
- Pouget, J.-P.; Lozza, C.; Deshayes, E.; Boudousq, V.; Navarro-Teulon, I. Introduction to Radiobiology of Targeted Radionuclide Therapy. Front. Med. 2015, 2, 12.
- Robertson, A.K.H.; Ramogida, C.F.; Rodríguez-Rodríguez, C.; Blinder, S.; Kunz, P.; Sossi, V.; Schaffer, P. Multi-Isotope SPECT Imaging of the 225Ac Decay Chain: Feasibility Studies. Phys. Med. Biol. 2017, 62, 4406–4420.
- Ocak, M.; Toklu, T.; Demirci, E.; Selçuk, N.; Kabasakal, L. Post-Therapy Imaging of 225Ac-DOTATATE Treatment in a Patient with Recurrent Neuroendocrine Tumor. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 2711–2712.
- Kratochwil, C.; Bruchertseifer, F.; Rathke, H.; Bronzel, M.; Apostolidis, C.; Weichert, W.; Haberkorn, U.; Giesel, F.L.; Morgenstern, A. Targeted α-Therapy of Metastatic Castration-Resistant Prostate Cancer with 225Ac-PSMA-617: Dosimetry Estimate and Empiric Dose Finding. J. Nucl. Med. 2017, 58, 1624–1631.
- Belli, M.L.; Sarnelli, A.; Mezzenga, E.; Cesarini, F.; Caroli, P.; Di Iorio, V.; Strigari, L.; Cremonesi, M.; Romeo, A.; Nicolini, S.; et al. Targeted Alpha Therapy in MCRPC (Metastatic Castration-Resistant Prostate Cancer) Patients: Predictive Dosimetry and Toxicity Modeling of 225Ac-PSMA (Prostate-Specific Membrane Antigen). Front. Oncol. 2020, 10, 531660.
- Sgouros, G.; He, B.; Ray, N.; Ludwig, D.L.; Frey, E.C. Dosimetric Impact of Ac-227 in Accelerator-Produced Ac-225 for Alpha-Emitter Radiopharmaceutical Therapy of Patients with Hematological Malignancies: A Pharmacokinetic Modeling Analysis. EJNMMI Phys. 2021, 8, 60.
- Tranel, J.; Feng, F.Y.; James, S.S.; Hope, T.A. Effect of Microdistribution of Alpha and Beta-Emitters in Targeted Radionuclide Therapies on Delivered Absorbed Dose in a GATE Model of Bone Marrow. Phys. Med. Biol. 2021, 66, 035016.
- Sato, T.; Furuta, T.; Liu, Y.; Naka, S.; Nagamori, S.; Kanai, Y.; Watabe, T. Individual Dosimetry System for Targeted Alpha Therapy Based on PHITS Coupled with Microdosimetric Kinetic Model. EJNMMI Phys. 2021, 8, 4.
- Fry, C.; Thoennessen, M. Discovery of Actinium, Thorium, Protactinium, and Uranium Isotopes. At. Data Nucl. Data Tables 2013, 99, 345–364.
- Boll, R.A.; Malkemus, D.; Mirzadeh, S. Production of Actinium-225for Alpha Particle Mediated Radioimmunotherapy. Appl. Radiat. Isot. 2005, 62, 667–679.
- Apostolidis, C.; Molinet, R.; Rasmussen, G.; Morgenstern, A. Production of Ac-225from Th-229 for Targeted α Therapy. Anal. Chem. 2005, 77, 6288–6291.
- Kotovskii, A.A.; Nerozin, N.A.; Prokof’ev, I.V.; Shapovalov, V.V.; Yakovshchits, Y.A.; Bolonkin, A.S.; Dunin, A.V. Isolation of Actinium-225for Medical Purposes. Radiochemistry 2015, 57, 285–291.
- Zielinska, B.; Apostolidis, C.; Bruchertseifer, F.; Morgenstern, A. An Improved Method for the Production of Ac-225/Bi-213 from Th-229 for Targeted Alpha Therapy. Solvent Extr. Ion Exch. 2007, 25, 339–349.
- Perron, R.; Gendron, D.; Causey, P.W. Construction of a Thorium/Actinium Generator at the Canadian Nuclear Laboratories. Appl. Radiat. Isot. 2020, 164, 109262.
- Apostolidis, C.; Molinet, R.; McGinley, J.; Abbas, K.; Möllenbeck, J.; Morgenstern, A. Cyclotron Production of Ac-225for Targeted Alpha Therapy. Appl. Radiat. Isot. 2005, 62, 383–387.
- Nagatsu, K.; Suzuki, H.; Fukada, M.; Ito, T.; Ichinose, J.; Honda, Y.; Minegishi, K.; Higashi, T.; Zhang, M.-R. Cyclotron Production of 225Ac from an Electroplated 226Ra Target. Eur. J. Nucl. Med. Mol. Imaging 2021, 49, 279–289.
- Morss, L.R.; Edelstein, N.M.; Fuger, J. The Chemistry of the Actinide and Transactinide Elements, 3rd ed.; Springer Science & Business Media: Berlin/Heidelberg, Germany, 2007; ISBN 978-1-4020-3598-2.
- Yamana, H.; Mitsugashira, T.; Shiokawa, Y.; Sato, A.; Suzuki, S. Possibility of the Existence of Divalent Actinium in Aqueous Solution. J. Radioanal. Chem. 1983, 76, 19–26.
- Malý, J. The Amalgamation Behavior of Heavy Elements—III Extraction of Radium, Lead and the Actinides by Sodium Amalgam from Acetate Solutions. J. Inorg. Nucl. Chem. 1969, 31, 1007–1017.
- Kozempel, J.; Mokhodoeva, O.; Vlk, M. Progress in Targeted Alpha-Particle Therapy. What We Learned about Recoils Release from In Vivo Generators. Molecules 2018, 23, 581.
- Thiele, N.A.; Wilson, J.J. Actinium-225for Targeted α Therapy: Coordination Chemistry and Current Chelation Approaches. Cancer Biother. Radiopharm. 2018, 33, 336–348.
- Pearson, R.G. Hard and Soft Acids and Bases. J. Am. Chem. Soc. 1963, 85, 3533–3539.
- Cotton, S.A. Lanthanide and Actinide Chemistry; Inorganic Chemistry; Wiley: Chichester, UK; Hoboken, NJ, USA, 2006; ISBN 978-0-470-01005-1.
- Davis, I.A.; Glowienka, K.A.; Boll, R.A.; Deal, K.A.; Brechbiel, M.W.; Stabin, M.; Bochsler, P.N.; Mirzadeh, S.; Kennel, S.J. Comparison of 225actinium Chelates: Tissue Distribution and Radiotoxicity. Nucl. Med. Biol. 1999, 26, 581–589.
- Deal, K.A.; Davis, I.A.; Mirzadeh, S.; Kennel, S.J.; Brechbiel, M.W. Improved in Vivo Stability of Actinium-225Macrocyclic Complexes. J. Med. Chem. 1999, 42, 2988–2992.
- Kennel, S.J.; Brechbiel, M.W.; Milenic, D.E.; Schlom, J.; Mirzadeh, S. Actinium-225Conjugates of Mab CC49 and Humanized ΔCH2 CC49. Cancer Biother. Radiopharm. 2002, 17, 219–231.
- Maguire, W.F.; McDevitt, M.R.; Smith-Jones, P.M.; Scheinberg, D.A. Efficient 1-Step Radiolabeling of Monoclonal Antibodies to High Specific Activity with 225Ac for α-Particle Radioimmunotherapy of Cancer. J. Nucl. Med. 2014, 55, 1492–1498.
- Pandya, D.N.; Hantgan, R.; Budzevich, M.M.; Kock, N.D.; Morse, D.L.; Batista, I.; Mintz, A.; Li, K.C.; Wadas, T.J. Preliminary Therapy Evaluation of 225Ac-DOTA-c(RGDyK) Demonstrates That Cerenkov Radiation Derived from 225Ac Daughter Decay Can Be Detected by Optical Imaging for In Vivo Tumor Visualization. Theranostics 2016, 6, 698–709.
- Pruszynski, M.; D’Huyvetter, M.; Bruchertseifer, F.; Morgenstern, A.; Lahoutte, T. Evaluation of an Anti-HER2 Nanobody Labeled with 225Ac for Targeted α-Particle Therapy of Cancer. Mol. Pharm. 2018, 15, 1457–1466.
- Majkowska-Pilip, A.; Rius, M.; Bruchertseifer, F.; Apostolidis, C.; Weis, M.; Bonelli, M.; Laurenza, M.; Królicki, L.; Morgenstern, A. In Vitro Evaluation of 225Ac-DOTA-Substance P for Targeted Alpha Therapy of Glioblastoma Multiforme. Chem. Biol. Drug Des. 2018, 92, 1344–1356.
- McDevitt, M.R.; Ma, D.; Simon, J.; Frank, R.K.; Scheinberg, D.A. Design and Synthesis of 225Ac Radioimmunopharmaceuticals. Appl. Radiat. Isot. 2002, 57, 841–847.
- Schwartz, J.; Jaggi, J.S.; O’Donoghue, J.A.; Ruan, S.; McDevitt, M.; Larson, S.M.; Scheinberg, D.A.; Humm, J.L. Renal Uptake of Bismuth-213 and Its Contribution to Kidney Radiation Dose Following Administration of Actinium-225-Labeled Antibody. Phys. Med. Biol. 2011, 56, 721–733.
- Singh Jaggi, J.; Kappel, B.J.; McDevitt, M.R.; Sgouros, G.; Flombaum, C.D.; Cabassa, C.; Scheinberg, D.A. Efforts to Control the Errant Products of a Targeted In Vivo Generator. Cancer Res. 2005, 65, 4888–4895.
- Yoshimoto, M.; Yoshii, Y.; Matsumoto, H.; Shinada, M.; Takahashi, M.; Igarashi, C.; Hihara, F.; Tachibana, T.; Doi, A.; Higashi, T.; et al. Evaluation of Aminopolycarboxylate Chelators for Whole-Body Clearance of Free 225Ac: A Feasibility Study to Reduce Unexpected Radiation Exposure during Targeted Alpha Therapy. Pharmaceutics 2021, 13, 1706.
- Uccelli, L.; Boschi, A.; Cittanti, C.; Martini, P.; Panareo, S.; Tonini, E.; Nieri, A.; Urso, L.; Caracciolo, M.; Lodi, L.; et al. 90Y/177Lu-DOTATOC: From Preclinical Studies to Application in Humans. Pharmaceutics 2021, 13, 1463.
- Norenberg, J.; Daniels, T.; Kevin, J.; Heloisa, S.; Kusewitt, D.; Hesterman, J.; Orcutt, K.; Nysus, M.; Goff, C.; Jacquez, Q.; et al. Pre-Clinical Evaluation of 225Ac-DOTATOC Pharmacokinetics, Dosimetry, and Istopathology to Enable Phase-1 Clinical Trial in Patients with Neuroendocrine Tumors. J. Med. Imaging Radiat. Sci. 2019, 50, S105.
- Strosberg, J.R.; Caplin, M.E.; Kunz, P.L.; Ruszniewski, P.B.; Bodei, L.; Hendifar, A.; Mittra, E.; Wolin, E.M.; Yao, J.C.; Pavel, M.E.; et al. 177Lu-Dotatate plus Long-Acting Octreotide versus High-dose Long-Acting Octreotide in Patients with Midgut Neuroendocrine Tumours (NETTER-1): Final Overall Survival and Long-Term Safety Results from an Open-Label, Randomised, Controlled, Phase 3 Trial. Lancet Oncol. 2021, 22, 1752–1763.
- Strosberg, J.R.; Caplin, M.E.; Kunz, P.L.; Ruszniewski, P.B.; Bodei, L.; Hendifar, A.E.; Mittra, E.; Wolin, E.M.; Yao, J.C.; Pavel, M.E.; et al. Final Overall Survival in the Phase 3 NETTER-1 Study of Lutetium-177-DOTATATE in Patients with Midgut Neuroendocrine Tumors. JCO 2021, 39, 4112.
- Strosberg, J.; El-Haddad, G.; Wolin, E.; Hendifar, A.; Yao, J.; Chasen, B.; Mittra, E.; Kunz, P.L.; Kulke, M.H.; Jacene, H.; et al. Phase 3 Trial of 177Lu-Dotatate for Midgut Neuroendocrine Tumors. N. Engl. J. Med. 2017, 376, 125–135.
- Zhang, J.; Singh, A.; Kulkarni, H.R.; Schuchardt, C.; Müller, D.; Wester, H.-J.; Maina, T.; Rösch, F.; van der Meulen, N.P.; Müller, C.; et al. From Bench to Bedside—The Bad Berka Experience with First-in-Human Studies. Semin. Nucl. Med. 2019, 49, 422–437.
- Kratochwil, C.; Bruchertseifer, F.; Rathke, H.; Hohenfellner, M.; Giesel, F.L.; Haberkorn, U.; Morgenstern, A. Targeted α-Therapy of Metastatic Castration-Resistant Prostate Cancer with 225Ac-PSMA-617: Swimmer-Plot Analysis Suggests Efficacy Regarding Duration of Tumor Control. J. Nucl. Med. 2018, 59, 795–802.
- Sathekge, M.; Bruchertseifer, F.; Knoesen, O.; Reyneke, F.; Lawal, I.; Lengana, T.; Davis, C.; Mahapane, J.; Corbett, C.; Vorster, M.; et al. 225Ac-PSMA-617 in Chemotherapy-Naive Patients with Advanced Prostate Cancer: A Pilot Study. Eur. J. Nucl. Med. Mol. Imaging 2019, 46, 129–138.
- Sathekge, M.; Bruchertseifer, F.; Vorster, M.; Lawal, I.O.; Knoesen, O.; Mahapane, J.; Davis, C.; Reyneke, F.; Maes, A.; Kratochwil, C.; et al. Predictors of Overall and Disease-Free Survival in Metastatic Castration-Resistant Prostate Cancer Patients Receiving 225Ac-PSMA-617 Radioligand Therapy. J. Nucl. Med. 2020, 61, 62–69.
- Yadav, M.P.; Ballal, S.; Sahoo, R.K.; Tripathi, M.; Seth, A.; Bal, C. Efficacy and Safety of 225Ac-PSMA-617 Targeted Alpha Therapy in Metastatic Castration-Resistant Prostate Cancer Patients. Theranostics 2020, 10, 9364–9377.
- Khreish, F.; Ebert, N.; Ries, M.; Maus, S.; Rosar, F.; Bohnenberger, H.; Stemler, T.; Saar, M.; Bartholomä, M.; Ezziddin, S. 225Ac-PSMA-617/177Lu-PSMA-617 Tandem Therapy of Metastatic Castration-Resistant Prostate Cancer: Pilot Experience. Eur. J. Nucl. Med. Mol. Imaging 2020, 47, 721–728.
- Rosenblat, T.L.; McDevitt, M.R.; Carrasquillo, J.A.; Pandit-Taskar, N.; Frattini, M.G.; Maslak, P.G.; Park, J.H.; Douer, D.; Cicic, D.; Larson, S.M.; et al. Treatment of Patients with Acute Myeloid Leukemia with the Targeted Alpha-Particle Nanogenerator Actinium-225-Lintuzumab. Clin. Cancer Res. 2022, 28, 2030–2037.
- Hope, T.; Mehr, S.; Morris, M.; Li, D.; Halperin, M.D.; Strosberg, J.; Soares, H.; Jacene, H.; Pavel, M.; Pamela, L.; et al. ACTION-1: A Randomized Phase Ib/3 Trial of RYZ101 Compared with SoC in SSTR2+ Well-Differentiated GEP-NET with Progression Following Lu-177 SSA. EJEA 2023.
- Yadav, M.P.; Ballal, S.; Sahoo, R.K.; Bal, C. Efficacy and Safety of 225Ac-DOTATATE Targeted Alpha Therapy in Metastatic Paragangliomas: A Pilot Study. Eur. J. Nucl. Med. Mol. Imaging 2021, 49, 1595–1606.
- Peng, D.; Liu, H.; Huang, L.; Cao, J.; Chen, Y. 225Ac-DOTATATE Therapy in a Case of Metastatic Pheochromocytoma. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 3596–3597.




