
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Gerard M. London | -- | 1771 | 2023-01-30 18:06:51 | | | |
| 2 | Sirius Huang | Meta information modification | 1771 | 2023-01-31 02:02:17 | | |
Video Upload Options
Arterial dysfunction is major risk factor for cardiovascular complications, and arterial stiffness is an independent risk factor in end-stage renal disease patients. As the distance from the heart increases, arterial stiffness (pulse wave velocity) becomes progressively more marked. This generates a centrifugal stiffness gradient, which leads to partial, continuous local wave reflections, which in turn attenuate the transmission of pulsatile pressure into the microcirculation, thus limiting the potentially deleterious outcomes both upstream (on the heart: left-ventricular hypertrophy and coronary perfusion) and downstream (on the renal and cerebral microcirculation: reduced glomerular filtration and impaired cognitive functions). The impact of arterial aging is greater on the aorta and central capacitive arteries, and it is characterized by a loss or reversal of the physiological stiffness gradient between central and peripheral arteries.
1. Introduction
2. Aging and Arterial Stiffness
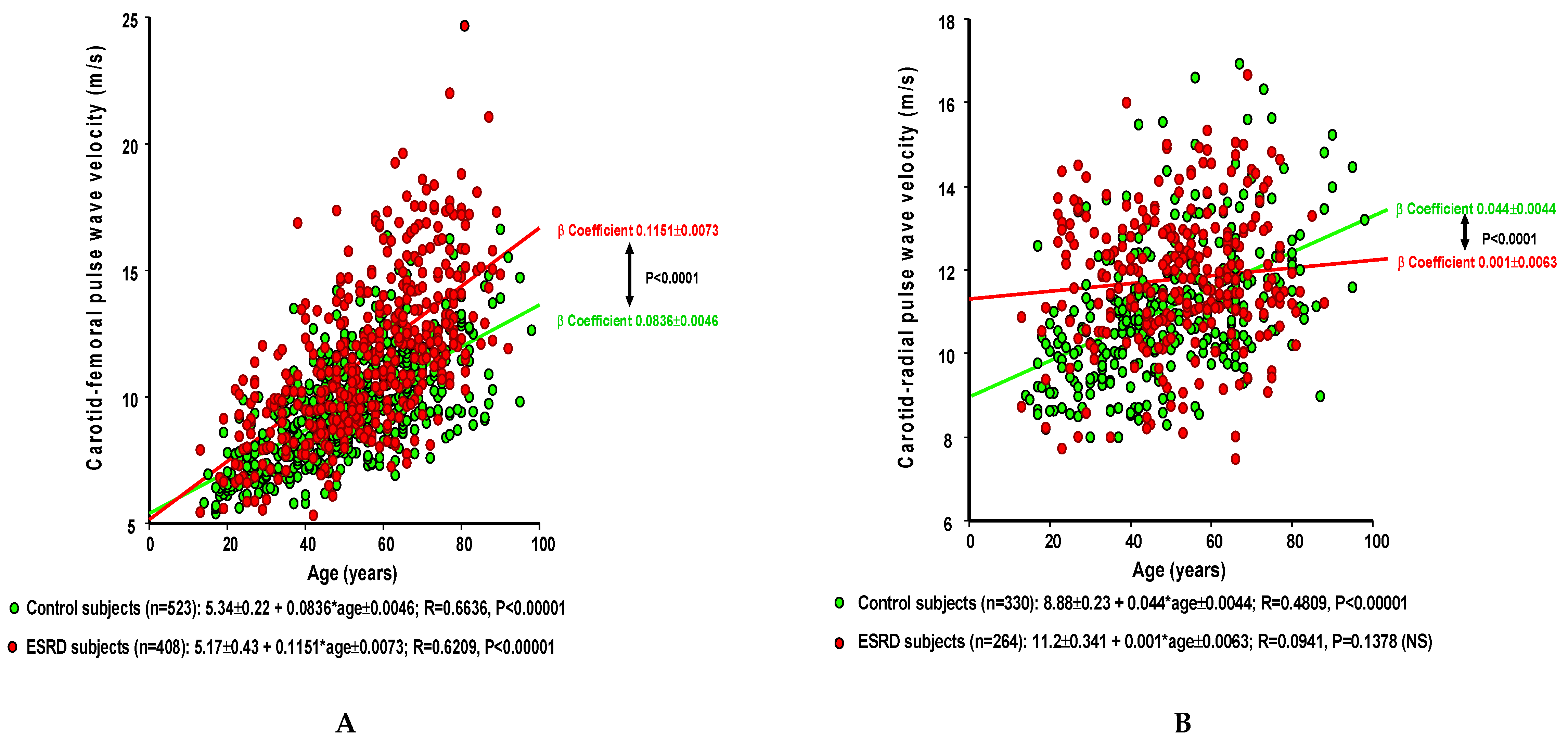
| A. Carotid–Femoral PWV (cm/s ± SEM) Multiple Regression Report in Control and ESRD Populations | |||||||
| Control Group (n = 526) 9.63 ± 2.13 |
ESRD Patients (n = 412) 11.67 ± 3.15 |
||||||
| β Coefficient | p-Value | R2 | β Coefficient | p-Value | R2 | p-Value 1 vs. 2 |
|
| Age (years) | 6.4 ± 0.38 | <0.00001 | 0.2149 | 11.5 ± 0.65 | <0.00001 | 0.400 | <0.00001 |
| Mean BP (mmHg) | 3.45 ± 0.26 | <0.00001 | 0.130 | 3.7 ± 0.44 | <0.00001 | 0.09 | NS |
| Gender (female) | −44.20 ± 11.9 | 0.0002 | 0.0002 | −1.1 ± 23.2 | 0.0780 | 0.004 | NS |
| Heart period (ms) | −0.15 ± 0.04 | 0.0201 | 0.011 | −0.19 ± 0.008 | 0.0137 | 0.008 | NS |
| 0.6140 p < 0.0001 |
0.4958 p < 0.0001 |
||||||
| B. Carotid–Radial Pulse Wave Velocity (cm/s ± SEM) Multiple Regression Report in Control and ESRD Populations | |||||||
| Control (n = 410) | ESRD (n = 343) |
||||||
| β Coefficient | T Value | pValue | β Coefficient | T Value | pValue | pValue 1 vs. 2 |
|
| Age (years) | 3.05 ± 0.38 | 7.831 | <0.00001 | 1.73 ± 0.46 | 3.795 | 0.0002 | 0.0389 |
| Mean BP (mmHg) | 3.85 ± 0.39 | 9.831 | <0.00001 | 5.00 ± 0.46 | 10.774 | <0.00001 | NS (0.056) |
| Gender (female) | −42.9 ± 13.0 | −12.70 | 0.0073 | −34.42 ± 15.58 | −2.309 | 0.0205 | NS |
| R2 = 0.4126 p < 0.00001 |
R2 = 0.2783 p < 0.00001 |
||||||
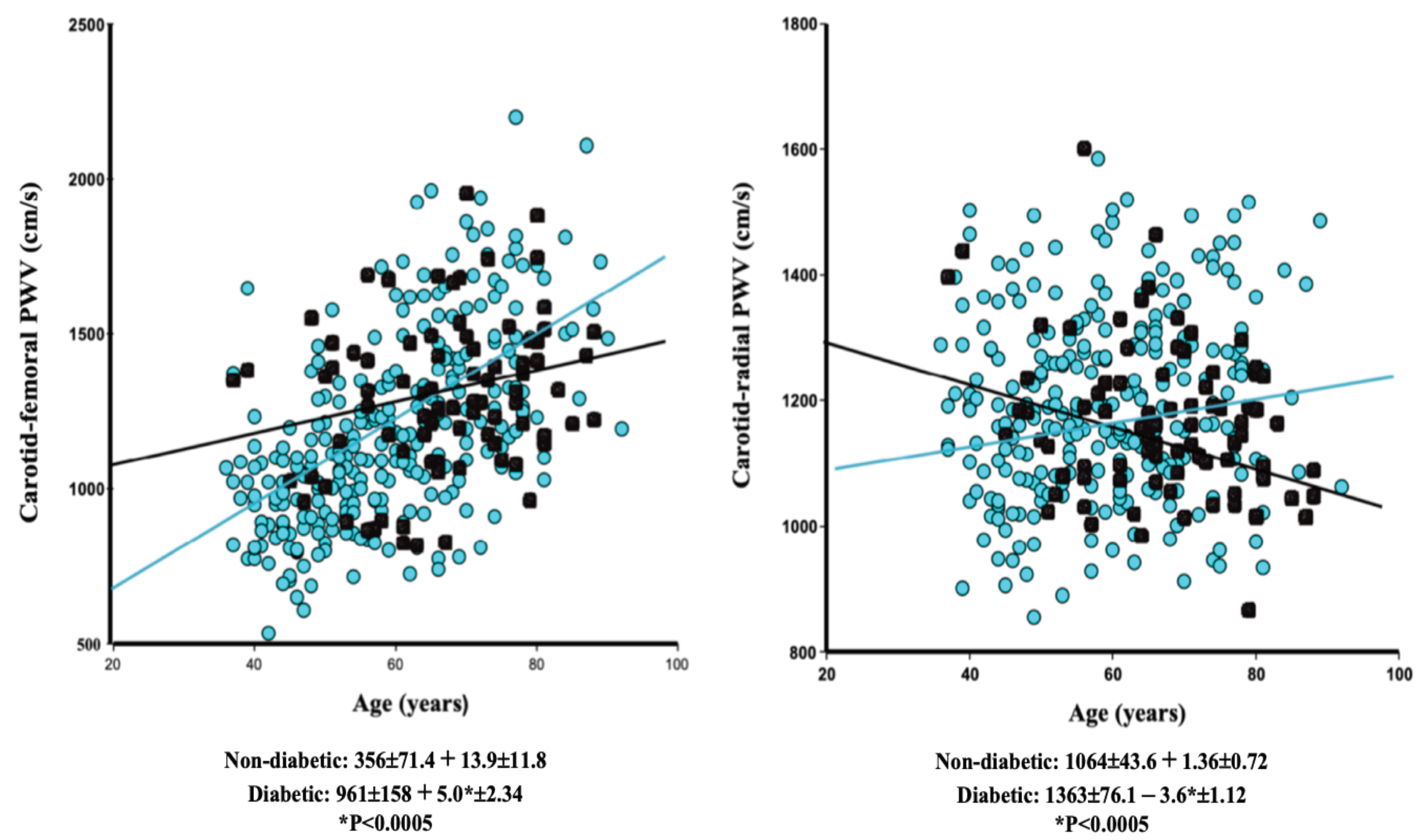
| A. Carotid–Femoral PWV (cm/s ± SEM) | |||||||
| Nondiabetic (n = 326) |
Diabetic (n = 83) |
||||||
| β Coefficient | p-Value | R2 | β Coefficient | p-Value | R2 | p-Value 1 vs. 2 |
|
| Age (years) | 14.80 ± 1.14 | <0.00001 | 0.3782 | 8.10 ± 2.50 | 0.0017 | 0.1131 | 0.0149 |
| Mean BP (mmHg) | 4.48 ± 0.95 | <0.00001 | 0.0539 | 4.90 ± 1.75 | 0.0068 | 0.0833 | NS |
| 0.4830 p < 0.0001 |
0.1403 p < 0.001 |
||||||
| B. Carotid–Radial PWV (cm/s ± SEM) | |||||||
| Nondiabetic (n = 264) |
Diabetic (n = 83) |
p | |||||
| β Coefficient | p-Value | R2 | β Coefficient | p-Value | R2 | p-Value 1 vs. 2 |
|
| Age (years) | 2.15 ± 0.66 | 0.0016 | 0.032 | −0.02 ± 1.00 | NS | 0.00005 | NS (0.0696) |
| Mean BP (mmHg) | 3.85 ± 0.53 | <0.00001 | 0.1656 | 4.70 ± 0.70 | <0.00001 | 0.3451 | NS |
| 0.1792 p < 0.0001 |
0.4394 p < 0.0001 |
||||||
References
- North, B.J.; Sinclair, D.A. The intersection between aging and cardiovascular disease. Circ. Res. 2012, 110, 1097–1108.
- Donato, A.J.; Machin, D.R.; Lesniewski, L.A. Mechanisms of dysfunction in the aging vasculature and role in age-related diseases. Circ. Res. 2018, 123, 825–848.
- Ungvari, Z.; Tarantini, S.; Donato, A.J.; Galvan, V.; Csiszar, A. Mechanisms of vascular aging. Circ. Res. 2018, 123, 849–867.
- Vatner, S.F.; Zhang, J.; Vyzas, C.; Mishra, K.; Graham, R.M.; Vatner, D.E. Vascular stiffness in aging and disease. Front. Physiol. 2021, 12, 762437.
- The Reference Values for Arterial Stiffness’ Collaboration. Determinants of pulse wave velocity in healthy people and in the presence of cardiovascular risk factors: ‘Establishing normal and reference values’. Eur. Heart J. 2010, 31, 2338–2350.
- Blacher, J.; Guérin, A.P.; Pannier, B.; Marchais, S.J.; Safar, M.E.; London, G.M. Impact of aortic stiffness on survival in end-stage renal disease. Circulation 1999, 99, 2434–2439.
- Shoji, T.; Emoto, M.; Shinohara, K.; Kakiya, R.; Tsujimoto, Y.; Kishimoto, H.; Ishimura, E.; Tabata, T.; Nishizawa, Y. Diabetes mellitus, aortic stiffness, and cardiovascular mortality in end-stage renal disease. J. Am. Soc. Nephrol. 2001, 12, 2117–2124.
- Laurent, S.; Boutouyrie, P.; Asmar, R.; Gautier, I.; Laloux, B.; Guize, L.; Ducimetiere, P.; Benetos, A. Aortic stiffness is an independent predictor of all-cause and cardiovascular mortality in hypertensive patients. Hypertension 2001, 37, 1236–1241.
- Cruickshank, K.; Riste, L.; Anderson, S.G.; Wright, J.S.; Dunn, G.; Gosling, R.G. Aortic pulse-wave velocity and its relationship to mortality in diabetes and glucose intolerance: An index of vascular function. Circulation 2002, 106, 2085–2090.
- Boutouyrie, P.; Tropeano, A.I.; Asmar, R.; Gautier, I.; Benetos, A.; Lacolley, P.; Laurent, S. Aortic stiffness is an independent predictor of primary coronary events in hypertensive patients: A longitudinal study. Hypertension 2002, 39, 10–15.
- Majesky, M.W. Developmental basis of vascular smooth muscle diversity. Arterioscler. Thromb. Vasc. Biol. 2007, 27, 1248–1258.
- Avolio, A.P.; Chen, S.G.; Wang, R.P.; Zhang, C.L.; Li, M.F.; O’Rourke, M.F. Effects of aging on changing arterial compliance and left ventricular load in a northern Chinese urban community. Circulation 1983, 68, 50–58.
- Nichols, W.W.; O’Rourke, M.F. McDonald’s Blood Flow in Arteries: Theoretical, Experimental and Clinical Principles, 5th ed.; Hodder Arnold Publisher: London, UK, 2005; pp. 193–233, 233–267, 299–337.
- O’Rourke, M.F. Arterial aging: Pathophysiological principles. Vasc. Med. 2007, 12, 329–341.
- Mitchell, G.F. Effects of central arterial aging on the structure and function of the peripheral vasculature: Implications for end-organ damage. J. Appl. Physiol. 2008, 105, 1652–1660.
- Bortolotto, L.A.; Hanon, O.; Franconi, G.; Boutouyrie, P.; Legrain, S.; Girerd, X. The aging process modifies the distensibility of elastic but not muscular arteries. Hypertension 1999, 34, 889–892.
- Mitchell, G.F.; van Buchem, M.A.; Sigurdsson, S.; Gotal, J.D.; Jonsdottir, M.K.; Kjartansson, Ó.; Garcia, M.; Aspelund, T.; Harris, T.B.; Gudnason, V.; et al. Arterial stiffness, pressure and flow pulsatility and brain structure and function: The Age, Gene/Environment Susceptibility–Reykjavik study. Brain 2011, 134, 3398–3407.
- Mitchell, G.F. Aortic stiffness, pressure and flow pulsatility, and target organ damage. J. Appl. Physiol. 2018, 125, 1871–1880.
- London, G.M.; Safar, M.E.; Pannier, B. Aortic aging in ESRD: Structural, hemodynamic, and mortality implications. J. Am. Soc. Nephrol. 2016, 27, 1837–1846.
- Pannier, B.; Guérin, A.P.; Marchais, S.J.; Safar, M.E.; London, G.M. Stiffness of capacitive and conduit arteries. Prognostic significance for end-stage renal disease patients. Hypertension 2005, 45, 592–596.
- Kimoto, E.; Shoji, T.; Shinohara, K.; Inaba, M.; Okuno, Y.; Miki, T.; Koyama, H.; Emoto, M.; Nishizawa, Y. Preferential stiffening of central over peripheral arteries in type 2 diabetes. Diabetes 2003, 52, 448–452.
- Safar, M.E.; Asmar, R.; Benetos, A.; Blacher, J.; Boutouyrie, P.; Lacolley, P.; Laurent, S.; London, G.; Pannier, B.; Protogerou, A.; et al. French Study Group on Arterial Stiffness. Interaction between hypertension and arterial stiffness. Hypertension 2018, 72, 796–805.
- Niiranen, T.J.; Kalesan, B.; Larson, M.G.; Hamburg, N.M.; Benjamin, E.J.; Mitchell, G.F.; Vasan, R.S. Aortic-brachial arterial stiffness gradient and cardiovascular risk in the community: The Framingham heart study. Hypertension 2017, 69, 1022–1028.
- London, G.M.; Pannier, B.; Safar, M.E. Arterial stiffness gradient, systemic reflection coefficient, and pulsatile pressure wave transmission in essential hypertension. Hypertension 2019, 74, 1366–1372.
- Fortier, C.; Mac-Way, F.; Desmeules, S.; Marquis, K.; De Serres, S.A.; Lebel, M.; Boutouyrie, P.; Agharazii, M. Aortic-brachial stiffness mismatch and mortality in dialysis population. Hypertension 2015, 65, 378–384.
- Cameron, J.D.; Bulpitt, C.J.; Pinto, E.S.; Rajkumar, C. The aging of elastic and muscular arteries: A comparison of diabetic and nondiabetic subjects. Diabetes Care 2003, 26, 2133–2138.
- DeBakey, M.E.; Glaeser, D.H. Patterns of atherosclerosis: Effect of risk factors on recurrence and survival—Analysis of 11,890 cases with more than 25-year follow-up. Am. J. Cardiol. 2000, 85, 1045–1053.
- Tsamis, A.; Krawiec, J.T.; Vorp, D.A. Elastin and collagen fibre microstructure of the human aorta in ageing and disease: A review. J. R. Soc. Interface 2013, 10, 20121004.
- Ribeiro-Silva, J.C.; Nolasco, P.; Krieger, J.E.; Miyakawa, A.A. Dynamic crosstalk between vascular smooth muscle cells and the aged extracellular matrix. Int. J. Mol. Sci. 2021, 22, 10175.
- Cocciolone, A.J.; Hawes, J.Z.; Staiculescu, M.C.; Johnson, E.O.; Murshed, M.; Wagenseil. J.E. Elastin, arterial mechanics, and cardiovascular disease. Am. J. Physiol. Heart Circ. Physiol. 2018, 315, H189–H205.
- Lacolley, P.; Regnault, V.; Segers, P.; Laurent, S. Vascular smooth muscle cells and arterial stiffening: Relevance in development, aging, and disease. Physiol. Rev. 2017, 97, 1555–1617.
- Shao, J.-S.; Cheng, S.-L.; Sadhu, J.; Towler, D.A. Inflammation and the osteogenic regulation of vascular calcification. A review and perspective. Hypertension 2010, 55, 579–592.
- Yasmin; McEniery, C.M.; O’Shaughnessy, K.M.; Harnett, P.; Arshad, A.; Wallace, S.; Maki-Petaja, K.; McDonnell, B.; Ashby, M.J.; Brown, J.; et al. Variation in the human matrix metalloproteinase-9 gene is associated with arterial stiffness in healthy individuals. Arterioscler. Thomb. Vasc. Biol. 2006, 26, 1799–1805.
- Shroff, R.C.; McNair, R.; Figg, N.; Skepper, J.N.; Schurgers, L.; Gupta, A.; Hiorns, M.; Donald, A.E.; Deanfield, J.; Rees, L.; et al. Dialysis accelerates medial vascular calcification in part by triggering smooth muscle cell apoptosis. Circulation 2008, 118, 1748–1757.
- London, G.M.; Guérin, A.P.; Marchais, S.J.; Métivier, F.; Pannier, B.; Adda, H. Arterial media calcification in end-stage renal disease: Impact on all-cause and cardiovascular mortality. Nephrol. Dial. Transplant. 2003, 18, 1731–1740.
- Laurent, S.; Boutouyrie, P.; Cunha, P.G.; Lacolley, P.; Nilsson, P.M. Concept of extremes in vascular aging. From early vascular aging to supernormal vascular aging. Hypertension 2019, 74, 218–228.
- London, G.M.; Blacher, J.; Pannier, B.; Guérin, A.P.; Marchais, S.J.; Safar, M.E. Arterial wave reflections and survival in end-stage renal failure. Hypertension 2001, 38, 434–438.
- Wanner, C.; Amann, K.; Shoji, T. The heart and vascular system in dialysis. Lancet 2016, 388, 276–284.
- Briet, M.; Boutouyrie, P.; Laurent, S.; London, G.M. Arterial stiffness and pulse pressure in CKD and ESRD. Kidney Int. 2012, 82, 388–400.
- Hayoz, D.; Rutschmann, B.; Perret, F.; Niederberger, M.; Tardy, Y.; Mooser, V.; Nussberger, J.; Waeber, B.; Brunner, H.R. Conduit artery compliance and distensibility are not necessarily reduced in hypertension. Hypertension 1992, 20, 1–6.




