Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Vincent Auffret | -- | 2278 | 2022-11-10 10:51:40 | | | |
| 2 | Rita Xu | Meta information modification | 2278 | 2022-11-10 10:59:31 | | | | |
| 3 | Rita Xu | -5 word(s) | 2273 | 2022-11-21 02:24:24 | | | | |
| 4 | Rita Xu | Meta information modification | 2273 | 2022-11-21 03:19:30 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Auffret, V.; Ridard, C.; Salerno, N.; Sorrentino, S. Unmet Needs in Transcatheter Aortic Valve Replacement. Encyclopedia. Available online: https://encyclopedia.pub/entry/33941 (accessed on 07 February 2026).
Auffret V, Ridard C, Salerno N, Sorrentino S. Unmet Needs in Transcatheter Aortic Valve Replacement. Encyclopedia. Available at: https://encyclopedia.pub/entry/33941. Accessed February 07, 2026.
Auffret, Vincent, Carine Ridard, Nadia Salerno, Sabato Sorrentino. "Unmet Needs in Transcatheter Aortic Valve Replacement" Encyclopedia, https://encyclopedia.pub/entry/33941 (accessed February 07, 2026).
Auffret, V., Ridard, C., Salerno, N., & Sorrentino, S. (2022, November 10). Unmet Needs in Transcatheter Aortic Valve Replacement. In Encyclopedia. https://encyclopedia.pub/entry/33941
Auffret, Vincent, et al. "Unmet Needs in Transcatheter Aortic Valve Replacement." Encyclopedia. Web. 10 November, 2022.
Copy Citation
Transcatheter aortic valve replacement (TAVR) swiftly evolved from a disrupting technology towards mainstream therapy in the field of severe symptomatic aortic stenosis. A series of randomized evaluations established its role in treating severe aortic stenosis patients across all surgical risk categories, paving the way for an extension of its indications to younger low-risk patients with a longer life expectancy.
transcatheter aortic valve replacement
transcatheter aortic valve implantation
coronary artery disease
myocardial infarction
1. Introduction
Since its introduction in clinical practice in 2002, transcatheter aortic valve replacement (TAVR) has become the gold standard for the treatment of patients at high surgical risk and is steadily becoming a valuable option for patients deemed at intermediate as well as low operative risk [1].
For instance, the longer life expectancy estimated in patients with a lower operative risk, further highlights the importance of limiting procedural complications, such as stroke, myocardial infarction, bleedings, vascular complications, and conduction or rhythmic disturbance, and proposes new challenges for patients’ management [2][3][4][5].
2. Conduction Disturbances
Conduction disturbances, i.e., high-degree atrioventricular block (HAVB) requiring permanent pacemaker implantation (PPI) and new-onset left bundle branch block (LBBB), represent the most common complication of transcatheter aortic valve replacement (TAVR). Thus, researchers will briefly review the current knowledge regarding the incidence and clinical impact of these conduction disturbances and reflect upon the challenges posed by these complications going forward in the TAVR setting. An extensive discussion of the mechanisms underlying these conduction disturbances, their natural history, predictors, and management is beyond the scope of the present research and can be found elsewhere [6][7][8][9][10].
3. New-Onset Persistent Left Bundle Branch Block
3.1. Incidence
With newer-generation devices, rates of 6% to 77% have been reported [6][7]. The incidence of new-onset LBBB with the SAPIEN 3 prosthesis ranges from 6% to 29% [11][12][13][14][15][16][17][18]. The prospective MARE study reported the lowest rate with this iteration of the balloon-expandable device at 6.0% while the randomized PARTNER 3 trial demonstrated a 22% rate of 30 days new-onset LBBB, which was 3-fold higher than the rate of the surgical group [11][19]. Regarding the self-expandable EVOLUT R/PRO system, the MARE study also found a low 8.0% rate of persistent LBBB. Nonetheless, other studies reported an incidence ranging from 18.0% to 44.2% [20][21][22][23]. Regarding other self-expandable systems, the PORTICO valve (Abbott Medical) showed rates of approximately 12% [24][25] while rates of 10.3% to 13.1% have been reported with the ACURATE Neo prosthesis (Boston Scientific) [22][23][26][27].
3.2. Clinical Impact
3.2.1. High-Degree Atrioventricular Block and Permanent Pacemaker Implantation
Three meta-analyses reported an approximately 2-fold higher rate of PPI associated with new-onset LBBB at mid-term (≈1 year) follow-up [28][29][30]. A significant impact of new-onset LBBB upon the risk of progression towards HAVB and PPI has consistently been reported either in-hospital [13][31][32][33][34] or at follow-up [32][33][35][36][37][38]. Furthermore, with the exception of the PARTNER I trial analysis [32], the vast majority of studies reported HAVB to be the leading indication (>70%) for PPI at follow-up. Some studies suggested that a QRS duration > 150–160 ms in the setting of new-onset LBBB was associated with a higher risk of late onset HAVB and sudden death [39][40], particularly when associated with a PR interval prolongation (>240 ms) [40][41][42].
3.2.2. Left Ventricular Ejection Fraction (LVEF) and Hospitalization for Heart Failure (HHF)
LBBB may be associated with deleterious ventricular remodeling and deterioration of left ventricular function [43]. Several studies have reported an impaired LVEF recovery after TAVR among new-onset LBBB patients [32][33][35][36][37][38][44][45]. This observation did not translate into a consistently increased risk of hospitalization for heart failure (HHF) in individual studies. Nevertheless, the largest meta-analysis to date reported an increased 1-year HHF risk associated with new-onset LBBB (RR = 1.35; 95% CI: 1.05–1.72) [30].
3.2.3. Mortality
Although it may act through the risk of progression to HAVB (and sudden death) and progressive heart failure as a result of LBBB-induced dyssynchrony, the effect of LBBB on all-cause and cardiovascular mortality has been inconsistent across studies. Regueiro et al. found an increased cardiovascular mortality risk in a meta-analysis of 5 studies, while only a trend was apparent for all-cause mortality combining data from 8 studies [28]. In their updated meta-analysis, Faroux et al. confirmed the deleterious impact upon cardiovascular mortality (RR = 1.46; 95% CI: 1.20–1.72), and unraveled a detrimental impact on all-cause mortality (RR = 1.32; 95% CI: 1.17–1.49) pooling data from 8 studies (5906 patients) and 12 studies (7792 patients), respectively [30].
4. Permanent Pacemaker Implantation
4.1. Incidence
According to a recent systematic review, post-TAVR rates of PPI with newer-generation devices range from 2.3% to 36.1% [8][46]. Rates were 4% to 24% with the Edwards SAPIEN 3 valve, lower than those reported with the Medtronic EVOLUT R/PRO ranging from 14.7% to 31.3% [21][46]. Interestingly, the risk of PPI at 30 days post-procedure was not significantly different between the TAVR and surgical group in the PARTNER 3 trial, whereas it remained higher after implantation of a self-expandable valve in the EVOLUT Low-Risk trial [19][47]. With the PORTICO valve, rates ranging from 9.8% to 28.1% have been reported [24][48]. Overall, the ACURATE Neo prosthesis demonstrated the lowest rates ranging from 2.3% to 11.5% [26][49]. In the SCOPE I and SCOPE II randomized comparisons, the post-procedural rate of PPI with the ACURATE Neo was similar to the incidence observed with the SAPIEN 3 and significantly lower than the rate reported with the EVOLUT R/PRO, respectively [23][49].
4.2. Clinical Impact
Left Ventricular Ejection Fraction and Hospitalization for Heart Failure
The impact of PPI on the evolution of LVEF after TAVR has been inconsistent from one study to another. Some studies suggested a significant decrease in LVEF at follow-up among patients undergoing PPI [36][50][51][52], while others reported no meaningful association [53][54][55][56][57]. These discrepancies may stem from differing pacing indications, pacing dependency, and populations across studies as deleterious effects of right ventricular pacing are more likely to occur in younger patients subjected to a high ventricular pacing percentage over a longer period [45].
PPI post-TAVR has been linked to a higher 1-year risk of HHF in a recent meta-analysis of crude study-level data (RR = 1.18 95% CI: 1.03–1.36) [30]. However, individual studies with a longer follow-up reached conflicting adjusted results [45][54][58].
4.3. Mortality
Faroux et al., reported an increased risk of 1-year all-cause mortality among pacemaker recipients post-TAVR (RR = 1.17 95% CI: 1.11–1.25) [30]. As previously discussed for HHF, long-term studies with a multivariable analysis reached inconsistent results regarding the independent impact of PPI in this finding [45][54][58]. This observation, along with the fact that PPI was not associated with an increased 1-year cardiovascular mortality in the meta-analysis by Faroux et al. [30], raises the issue of potential residual confounding in the association between PPI and post-TAVR mortality. Figure 1 summarizes the effects of new-onset LBBB and PPI on TAVR outcomes.
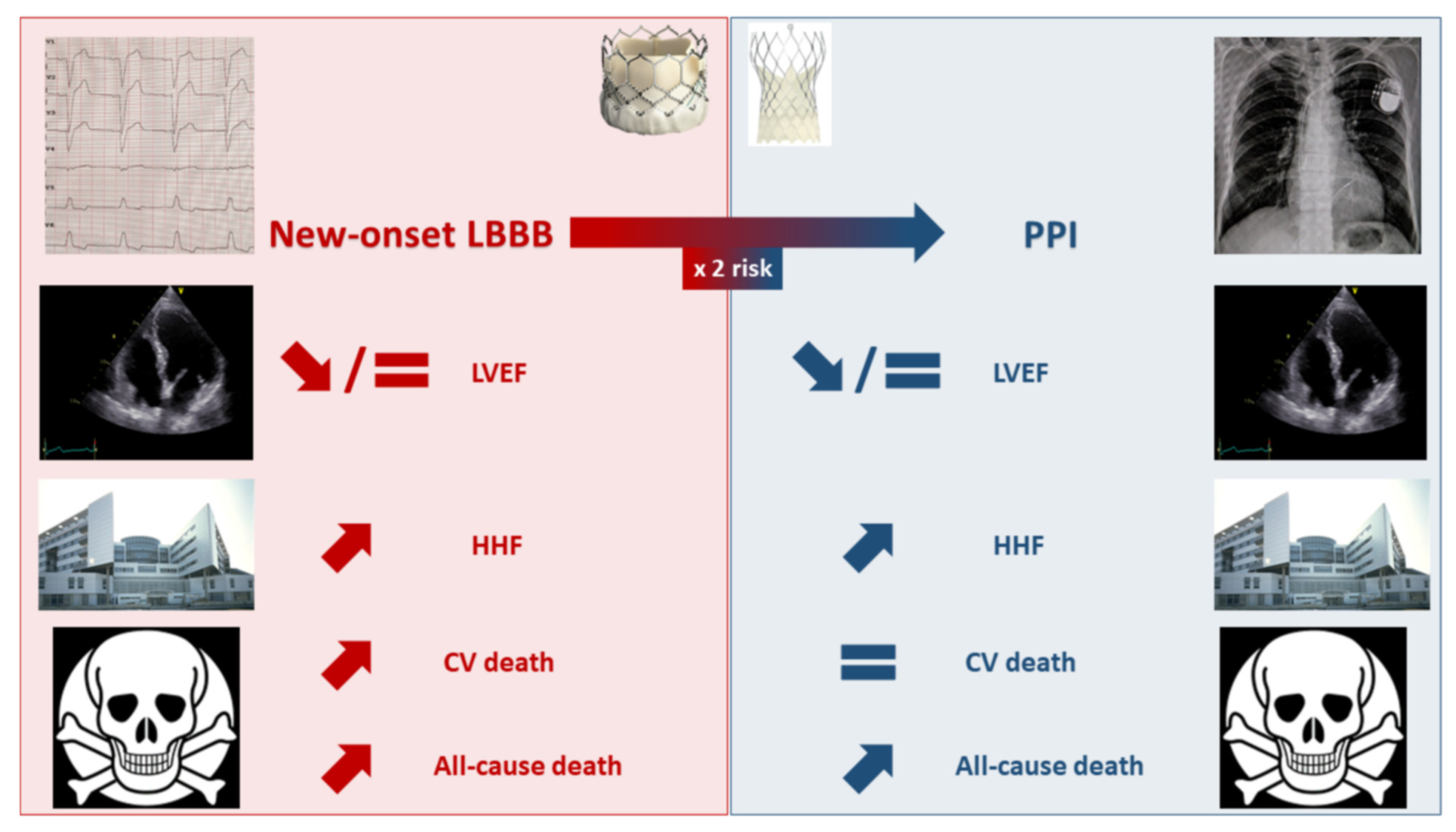
Figure 1. Effects of new-onset left bundle branch block and permanent pacemaker implantation on transcatheter aortic valve replacement outcomes. CV: cardiovascular; HHF: hospitalization for heart failure; LBBB: left bundle branch block; LVEF: left ventricular ejection fraction; PPI: permanent pacemaker implantation.
5. Unmet Needs
5.1. Pre-Procedural Management
Several studies have demonstrated that a significant proportion of TAVR candidates displayed HAVB or severe bradyarrhythmia during pre-procedural ECG monitoring either with 24-h in-hospital telemetry [59] or with ambulatory systems (patch ECG recorder, mobile telemetry), allowing a prolonged (≥7 days) recording [60][61]. Overall, approximately 3% of patients had HAVB episodes pre-TAVR, among whom 2/3 underwent pre-procedural PPI [62]. Furthermore, almost half of the patients with pre-TAVR bradyarrhythmic events benefited from a treatment change [59][60]. Bradyarrhythmic events were especially frequent among patients with 1st-degree AVB and right bundle branch block (RBBB) occurring in 30% and 47% of them, respectively [60]. Finally, among patients who received a pacemaker post-TAVR, 30% had HAVB episodes pre-TAVR [59][60]. These data suggest that pre-procedural ECG monitoring may be an appealing strategy to streamline patients care, especially those with the highest conduction disturbances risk (e.g., pre-existent RBBB and/or 1st-degree AVB). Nonetheless, further randomized studies are necessary to delineate the optimal indications, duration, clinical impact, and cost-effectiveness of pre-TAVR ambulatory ECG monitoring.
5.2. Procedural Management
Several approaches have been proposed in recent years to reduce the occurrence of conduction disturbances during TAVR. Jilaihawi et al. reported the MInimizing Depth According to the membranous Septum (MIDAS) approach, which suggests that a systematic pre-procedural evaluation of the length of the membranous septum below the aortic annulus plane may help tailor the implantation strategy to each patient anatomy [63]. Indeed, the performance of TAVR among increasingly younger and “healthier” patients may imply a need for future coronary re-access. Therefore, the optimal patient-specific implantation depth may result from a compromise between the need to prevent conduction disturbances and to access coronary artery during long-term follow-up. Consequently, in patients with a membranous septum length > 5 mm, considered at low risk of conduction disturbances by Jilaihawi et al., a deeper prosthesis position may be tolerated as long as it does not result in significant paravalvular leak [63]. Moreover, several studies have advocated for a higher implantation of transcatheter heart valves, especially using the cusp-overlap projection, which overlap coronary cusps and isolates the non-coronary cusp, thus providing a better appreciation of the implantation depth [64][65][66]. These reports usually demonstrated an approximately 2-fold lower rate of PPI associated with the use of the cusp-overlap technique.
5.3. Post-Procedural Management
One of the main issues regarding post-TAVR conduction disturbances has been the differing management strategies across centers and operators resulting from the lack of consensus, which explain the major differences observed in PPI rates and impact post-TAVR. Several experts’ consensus and guidelines have been published in recent years [9][10][67], which should facilitate a uniform post-procedural management, and allow the performance of large-scale, prospective studies to better describe the long-term impact of these conduction disturbances. Another persistent challenge is the management of conduction disturbances not representing firm PPI indications, i.e., new-onset LBBB and significant PR or QRS prolongation (≥40 ms, especially if PR is >240 ms or QRS > 150 ms). Several studies have demonstrated the safety of using ambulatory ECG monitoring post-TAVR to expedite patients’ discharge and guide PPI in such cases [11][62][68][69][70][71]. Overall, in these studies, delayed HAVB rates have ranged from 5% to 10% and from 10% to 15% approximately, at 30 days and 1-year post-TAVR, respectively. Interestingly, in the largest study to date, encompassing 459 TAVR recipients, the rate of delayed HAVB was higher among patients with new-onset first degree AVB than in patients with new-onset LBBB [70]. Another study demonstrated that the delta between baseline and day 2 post-procedure in PR interval but not in QRS duration was significantly associated with episodes of delayed HAVB [71]. These data suggest that the prolongation of the atrioventricular conduction on the surface ECG may not be a benign occurrence resulting from a supra Hisian injury and that researchers may need to pay greater attention to this modification. On the other hand, some groups have proposed the use of in-hospital electrophysiological studies (EPS) to guide PPI post-TAVR. Studies focusing on this strategy are usually of limited sample size and used various EPS protocols as well as different HV interval cut-offs to retain an indication for PPI [2][72]. Therefore, the level of evidence seems weaker than for ambulatory ECG monitoring. Nonetheless, these studies have overall demonstrated an excellent negative predictive value of EPS in the post-TAVR setting with a somewhat lower positive predictive value [2][72]. The recent European pacing guidelines granted ambulatory ECG monitoring and EPS-guided strategies (EPS being performed at day 3 post-procedure and an HV interval > 70 ms being used to retain an indication for PPI) the same grade of recommendations in TAVR recipients with new-onset or worsened conduction disturbances [10]. Defining whether ambulatory ECG monitoring or EPS-guided strategies represent the best and more cost-effective option in the post-procedural management of TAVR-related conduction disturbances remains a major unmet need, which is currently addressed by the Clinical Monitoring Strategy Versus Electrophysiology-guided Algorithmic Approach With a New LBBB After TAVI (COME-TAVI) study (NCT03303612). Finally, among TAVR recipients with pre-existent depressed LVEF (<50%) and requiring PPI or with large new-onset LBBB (>150 ms), the role of cardiac resynchronization has not been properly studied yet. Table 1 summarizes ongoing studies regarding conduction disturbances in the setting of TAVR.
Table 1. Ongoing studies regarding conduction disturbances in the setting of transcatheter aortic valve replacement.
| NCT Number | Study Name | Planned Number of Patients | Target Population | Design and Timing | Intervention | Main Outcomes |
|---|---|---|---|---|---|---|
| NCT03810820 | Remote ECG Monitoring of TAVI Patients | 240 | Consecutive candidates to outpatient TAVR | Observational, prospective, pre and post-procedure | Mobile cardiac telemetry (m-CARDS) before and after TAVR | Feasibility/patients’ adherence. Timeliness of medical assessment. Any new conduction disturbances up to 30 days. |
| NCT04139616 | PROMOTE | 2000 | All TAVR recipients without prior pacemaker | Observational, prospective, post-procedure | Application of a pre-specified algorithm for the management of conduction disturbances post-TAVR | Implementation of the algorithm. Incidence of PPI and sudden cardiac death up to 1 year |
| NCT02659137 | HESITATE | 100 | All TAVR recipients without pre-existent conduction disturbances | Observational, prospective, per and post-procedure | EPS during the procedure | Measurement of the HV interval upon occurrence of a LBBB. Location of the LBBB |
| NCT04454177 | SMART TAVR | 100 | All TAVR patients | Observational, prospective, post-procedure |
Huawei smart watch | Composite of death and rehospitalization, rates of conduction disturbances and PPI at 30 days |
| NCT04489095 | Conduction Disease After Transcatheter Aortic Valve Replacement | 200 | All TAVR recipients without prior pacemaker | Prospective, observational, per and post-procedure | EPS immediately before and after TAVR and the next day | Correlation between delta values of EPS findings and high-grade conduction disturbances at 1 year |
| NCT02482844 | LBBB-TAVI | 200 | TAVR recipients with new-onset LBBB | Observational, prospective, post-procedure |
EPS with PPI if HV interval >70 ms and implantable cardiac monitoring if <70 ms. |
Incidence of HAVB at 1 year |
| NCT04128384 | HOM TAVI | 200 | All TAVR recipients without prior pacemaker | Observational, prospective, per and post-procedure | Limited EPS including HV- and AH-intervals measurements pre- and post-TAVR | Incidence of HAVB and persistence of new-onset LBBB at 2 years |
| NCT03303612 | COME TAVI | 200 | TAVR recipients with new-onset LBBB | Randomized, prospective, post-procedure | Group 1: EPS-based strategy Group 2: Clinical follow-up with implantable cardiac monitoring. |
Incidence of the composite of cardiovascular hospitalization, syncope or death at 1 year. Incidence of HAVB at 1 year. Cost-effectiveness. |
| NCT02768064 | PAMIT | 120 | All TAVR recipients without prior pacemaker | Randomized, prospective, per and post-procedure | Experimental: Flexible screwed temporary pacemaker Active Comparator: Stiff standard temporary pacemaker |
Incidence of pericardial effusion, electrode dislocation, and other temporary pacing complications at 1 week |
| NCT04482816 | PHYS-TAVI | 24 | TAVR recipients with HAVB pacing indication after TAVR and LVEF > 50% | Randomized, prospective, post-procedure | Experimental: Physiological (His system) pacing Active Comparator: Right ventricular pacing |
Composite of survival, NYHA improvement and >25% increase in the 6MWT at 1 year. LVEF at 1 year. |
References
- Sorrentino, S.; Giustino, G.; Moalem, K.; Indolfi, C.; Mehran, R.; Dangas, G.D. Antithrombotic Treatment after Transcatheter Heart Valves Implant. Semin. Thromb. Hemost. 2018, 44, 38–45.
- Bourenane, H.; Galand, V.; Boulmier, D.; Leclercq, C.; Leurent, G.; Bedossa, M.; Behar, N.; Pichard, C.; Polin, B.; Tomasi, J.; et al. Electrophysiological Study-Guided Permanent Pacemaker Implantation in Patients With Conduction Disturbances Following Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2021, 149, 78–85.
- Giustino, G.; Sorrentino, S.; Mehran, R.; Faggioni, M.; Dangas, G. Cerebral Embolic Protection During TAVR. J. Am. Coll. Cardiol. 2017, 69, 465–466.
- Guedeney, P.; Tchétché, D.; Petronio, A.S.; Mehilli, J.; Sartori, S.; Lefèvre, T.; Presbitero, P.; Capranzano, P.; Iadanza, A.; Sardella, G.; et al. Impact of coronary artery disease and percutaneous coronary intervention in women undergoing transcatheter aortic valve replacement: From the WIN-TAVI registry. Catheter. Cardiovasc. Interv. 2019, 93, 1124–1131.
- Guedeney, P.; Sorrentino, S.; Mesnier, J.; De, R.S.; Indolfi, C.; Zeitouni, M.; Kerneis, M.; Silvain, J.; Montalescot, G.; Collet, J.-P. Single Versus Dual Antiplatelet Therapy Following TAVR. JACC Cardiovasc. Interv. 2021, 14, 234–236.
- Auffret, V.; Puri, R.; Urena, M.; Chamandi, C.; Rodriguez-Gabella, T.; Philippon, F.; Rodes-Cabau, J. Conduction Disturbances After Transcatheter Aortic Valve Replacement: Current Status and Future Perspectives. Circulation 2017, 136, 1049–1069.
- Muntané-Carol, G.; Guimaraes, L.; Ferreira-Neto, A.N.; Wintzer-Wehekind, J.; Junquera, L.; Del Val, D.; Faroux, L.; Philippon, F.; Rodés-Cabau, J. How does new-onset left bundle branch block affect the outcomes of transcatheter aortic valve repair? Expert Rev. Med. Devices 2019, 16, 589–602.
- Sammour, Y.; Krishnaswamy, A.; Kumar, A.; Puri, R.; Tarakji, K.G.; Bazarbashi, N.; Harb, S.; Griffin, B.; Svensson, L.; Wazni, O.; et al. Incidence, Predictors, and Implications of Permanent Pacemaker Requirement After Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2021, 14, 115–134.
- Rodes-Cabau, J.; Ellenbogen, K.A.; Krahn, A.D.; Latib, A.; Mack, M.; Mittal, S.; Muntane-Carol, G.; Nazif, T.M.; Sondergaard, L.; Urena, M.; et al. Management of Conduction Disturbances Associated With Transcatheter Aortic Valve Replacement: JACC Scientific Expert Panel. J. Am. Coll. Cardiol. 2019, 74, 1086–1106.
- Glikson, M.; Nielsen, J.C.; Kronborg, M.B.; Michowitz, Y.; Auricchio, A.; Barbash, I.M.; Barrabés, J.A.; Boriani, G.; Braunschweig, F.; Brignole, M.; et al. 2021 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy. Eur. Heart J. 2021, 42, 3427–3520.
- Rodes-Cabau, J.; Urena, M.; Nombela-Franco, L.; Amat-Santos, I.; Kleiman, N.; Munoz-Garcia, A.; Atienza, F.; Serra, V.; Deyell, M.W.; Veiga-Fernandez, G.; et al. Arrhythmic Burden as Determined by Ambulatory Continuous Cardiac Monitoring in Patients With New-Onset Persistent Left Bundle Branch Block Following Transcatheter Aortic Valve Replacement: The MARE Study. JACC Cardiovasc. Interv. 2018, 11, 1495–1505.
- De Torres-Alba, F.; Kaleschke, G.; Diller, G.P.; Vormbrock, J.; Orwat, S.; Radke, R.; Reinke, F.; Fischer, D.; Reinecke, H.; Baumgartner, H. Changes in the Pacemaker Rate After Transition From Edwards SAPIEN XT to SAPIEN 3 Transcatheter Aortic Valve Implantation: The Critical Role of Valve Implantation Height. JACC Cardiovasc Interv 2016, 9, 805–813.
- Gonska, B.; Seeger, J.; Kessler, M.; von Keil, A.; Rottbauer, W.; Wohrle, J. Predictors for permanent pacemaker implantation in patients undergoing transfemoral aortic valve implantation with the Edwards Sapien 3 valve. Clin. Res. Cardiol. 2017, 106, 590–597.
- Schwerg, M.; Fulde, F.; Dreger, H.; Poller, W.C.; Stangl, K.; Laule, M. Optimized Implantation Height of the Edwards SAPIEN 3 Valve to Minimize Pacemaker Implantation After TAVI. J. Intervent. Cardiol. 2016, 29, 370–374.
- Husser, O.; Pellegrini, C.; Kessler, T.; Burgdorf, C.; Thaller, H.; Mayr, N.P.; Kasel, A.M.; Kastrati, A.; Schunkert, H.; Hengstenberg, C. Predictors of Permanent Pacemaker Implantations and New-Onset Conduction Abnormalities With the SAPIEN 3 Balloon-Expandable Transcatheter Heart Valve. JACC Cardiovasc. Interv. 2016, 9, 244–254.
- Webb, J.; Gerosa, G.; Lefèvre, T.; Leipsic, J.; Spence, M.; Thomas, M.; Thielmann, M.; Treede, H.; Wendler, O.; Walther, T. Multicenter evaluation of a next-generation balloon-expandable transcatheter aortic valve. J. Am. Coll. Cardiol. 2014, 64, 2235–2243.
- Vahanian, A.; Urena, M.; Walther, T.; Treede, H.; Wendler, O.; Lefèvre, T.; Spence, M.S.; Redwood, S.; Kahlert, P.; Rodes-Cabau, J.; et al. Thirty-day outcomes in patients at intermediate risk for surgery from the SAPIEN 3 European approval trial. EuroInterv. J. Eur. Collab. Work. Group Interv. Cardiol. Eur. Soc. Cardiol. 2016, 12, e235–e243.
- Finkelstein, A.; Birati, E.Y.; Abramowitz, Y.; Steinvil, A.; Sheinberg, N.; Biner, S.; Bazan, S.; Ben Gal, Y.; Halkin, A.; Arbel, Y.; et al. Transcatheter aortic valve implantation: A single-center experience of 300 cases. Isr. Med. Assoc. J. 2013, 15, 613–616.
- Mack, M.J.; Leon, M.B.; Thourani, V.H.; Makkar, R.; Kodali, S.K.; Russo, M.; Kapadia, S.R.; Malaisrie, S.C.; Cohen, D.J.; Pibarot, P.; et al. Transcatheter Aortic-Valve Replacement with a Balloon-Expandable Valve in Low-Risk Patients. N. Engl. J. Med. 2019, 380, 1695–1705.
- Zaid, S.; Sengupta, A.; Okoli, K.; Tsoi, M.; Khan, A.; Ahmad, H.; Goldberg, J.B.; Undemir, C.; Rozenshtein, A.; Patel, N.; et al. Novel Anatomic Predictors of New Persistent Left Bundle Branch Block After Evolut Transcatheter Aortic Valve Implantation. Am. J. Cardiol. 2020, 125, 1222–1229.
- Rao, G.; Sheth, S.; Donnelly, J.; Scatola, A.; Tariq, U.; Laighold, S.; Grines, C.; Rutkin, B. Early Real-World Experience with CoreValve Evolut PRO and R Systems for Transcatheter Aortic Valve Replacement. J. Intervent. Cardiol. 2019, 2019, 1906814.
- Sticchi, A.; Gallo, F.; Marzo, V.D.; Won-keun, K.; Khokhar, A.A.; Zeus, T.; Toggweiler, S.; Marco, F.D.; Reimers, B.; Nombela-franco, L.; et al. Comparison of incidence and predictors of new left bundle branch block and permanent pacemaker implantation in a large multicentre contemporary TAVI registry using the Evolut R/pro system vs. the accurate neo valve. Eur. Heart J. Suppl. 2021, 23, suab134.044.
- Tamburino, C.; Bleiziffer, S.; Thiele, H.; Scholtz, S.; Hildick-Smith, D.; Cunnington, M.; Wolf, A.; Barbanti, M.; Tchetchè, D.; Garot, P.; et al. Comparison of Self-Expanding Bioprostheses for Transcatheter Aortic Valve Replacement in Patients With Symptomatic Severe Aortic Stenosis. Circulation 2020, 142, 2431–2442.
- Manoharan, G.; Linke, A.; Moellmann, H.; Redwood, S.; Frerker, C.; Kovac, J.; Walther, T. Multicentre clinical study evaluating a novel resheathable annular functioning self-expanding transcatheter aortic valve system: Safety and performance results at 30 days with the Portico system. EuroIntervention 2016, 12, 768–774.
- Walther, T.; Manoharan, G.; Linke, A.; Möllmann, H.; Holzhey, D.; Worthley, S.G.; Kim, W.-K.; Schäfer, U. Incidence of new-onset left bundle branch block and predictors of new permanent pacemaker following transcatheter aortic valve replacement with the PorticoTM valve. Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 2018, 54, 467–474.
- Toggweiler, S.; Nissen, H.; Mogensen, B.; Cuculi, F.; Fallesen, C.; Veien, K.T.; Brinkert, M.; Kobza, R.; Rück, A. Very low pacemaker rate following ACURATE neo transcatheter heart valve implantation. EuroInterv. J. Eur. Collab. Work. Group Interv. Cardiol. Eur. Soc. Cardiol. 2017, 13, 1273–1280.
- Brinkert, M.; Wolfrum, M.; Moccetti, F.; Bossard, M.; Berte, B.; Cuculi, F.; Kobza, R.; Toggweiler, S. Relevance of New Conduction Disorders After Implantation of the ACURATE Neo Transcatheter Heart Valve in the Aortic Valve Position. Am. J. Cardiol. 2020, 125, 783–787.
- Regueiro, A.; Abdul-Jawad Altisent, O.; Del Trigo, M.; Campelo-Parada, F.; Puri, R.; Urena, M.; Philippon, F.; Rodes-Cabau, J. Impact of New-Onset Left Bundle Branch Block and Periprocedural Permanent Pacemaker Implantation on Clinical Outcomes in Patients Undergoing Transcatheter Aortic Valve Replacement: A Systematic Review and Meta-Analysis. Circ. Cardiovasc. Interv. 2016, 9, e003635.
- Ando, T.; Takagi, H. The Prognostic Impact of New-Onset Persistent Left Bundle Branch Block Following Transcatheter Aortic Valve Implantation: A Meta-analysis. Clin. Cardiol. 2016, 39, 544–550.
- Faroux, L.; Chen, S.; Muntané-Carol, G.; Regueiro, A.; Philippon, F.; Sondergaard, L.; Jørgensen, T.H.; Lopez-Aguilera, J.; Kodali, S.; Leon, M.; et al. Clinical impact of conduction disturbances in transcatheter aortic valve replacement recipients: A systematic review and meta-analysis. Eur. Heart J. 2020, 41, 2771–2781.
- Akin, I.; Kische, S.; Paranskaya, L.; Schneider, H.; Rehders, T.C.; Trautwein, U.; Turan, G.; Bansch, D.; Thiele, O.; Divchev, D.; et al. Predictive factors for pacemaker requirement after transcatheter aortic valve implantation. BMC Cardiovasc. Disord. 2012, 12, 87.
- Nazif, T.M.; Williams, M.R.; Hahn, R.T.; Kapadia, S.; Babaliaros, V.; Rodes-Cabau, J.; Szeto, W.Y.; Jilaihawi, H.; Fearon, W.F.; Dvir, D.; et al. Clinical implications of new-onset left bundle branch block after transcatheter aortic valve replacement: Analysis of the PARTNER experience. Eur. Heart J. 2014, 35, 1599–1607.
- Urena, M.; Mok, M.; Serra, V.; Dumont, E.; Nombela-Franco, L.; DeLarochellière, R.; Doyle, D.; Igual, A.; Larose, E.; Amat-Santos, I.; et al. Predictive factors and long-term clinical consequences of persistent left bundle branch block following transcatheter aortic valve implantation with a balloon-expandable valve. J. Am. Coll. Cardiol. 2012, 60, 1743–1752.
- Keßler, M.; Gonska, B.; Seeger, J.; Rottbauer, W.; Wöhrle, J. Long-term clinical outcome of persistent left bundle branch block after transfemoral aortic valve implantation. Catheter. Cardiovasc. Interv. Off. J. Soc. Card. Angiogr. Interv. 2019, 93, 538–544.
- Urena, M.; Webb, J.G.; Cheema, A.; Serra, V.; Toggweiler, S.; Barbanti, M.; Cheung, A.; Ye, J.; Dumont, E.; DeLarochellière, R.; et al. Impact of new-onset persistent left bundle branch block on late clinical outcomes in patients undergoing transcatheter aortic valve implantation with a balloon-expandable valve. JACC Cardiovasc. Interv. 2014, 7, 128–136.
- Carrabba, N.; Valenti, R.; Migliorini, A.; Marrani, M.; Cantini, G.; Parodi, G.; Dovellini, E.V.; Antoniucci, D. Impact on left ventricular function and remodeling and on 1-year outcome in patients with left bundle branch block after transcatheter aortic valve implantation. Am. J. Cardiol. 2015, 116, 125–131.
- Nazif, T.M.; Chen, S.; George, I.; Dizon, J.M.; Hahn, R.T.; Crowley, A.; Alu, M.C.; Babaliaros, V.; Thourani, V.H.; Herrmann, H.C.; et al. New-onset left bundle branch block after transcatheter aortic valve replacement is associated with adverse long-term clinical outcomes in intermediate-risk patients: An analysis from the PARTNER II trial. Eur. Heart J. 2019, 40, 2218–2227.
- Chamandi, C.; Barbanti, M.; Munoz-Garcia, A.; Latib, A.; Nombela-Franco, L.; Gutierrez-Ibanez, E.; Veiga-Fernandez, G.; Cheema, A.N.; Cruz-Gonzalez, I.; Serra, V.; et al. Long-Term Outcomes in Patients With New-Onset Persistent Left Bundle Branch Block Following TAVR. JACC Cardiovasc. Interv. 2019, 12, 1175–1184.
- Urena, M.; Webb, J.G.; Eltchaninoff, H.; Muñoz-García, A.J.; Bouleti, C.; Tamburino, C.; Nombela-Franco, L.; Nietlispach, F.; Moris, C.; Ruel, M.; et al. Late cardiac death in patients undergoing transcatheter aortic valve replacement: Incidence and predictors of advanced heart failure and sudden cardiac death. J. Am. Coll. Cardiol. 2015, 65, 437–448.
- Jørgensen, T.H.; De Backer, O.; Gerds, T.A.; Bieliauskas, G.; Svendsen, J.H.; Søndergaard, L. Immediate Post-Procedural 12-Lead Electrocardiography as Predictor of Late Conduction Defects After Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2018, 11, 1509–1518.
- Toggweiler, S.; Stortecky, S.; Holy, E.; Zuk, K.; Cuculi, F.; Nietlispach, F.; Sabti, Z.; Suciu, R.; Maier, W.; Jamshidi, P.; et al. The Electrocardiogram After Transcatheter Aortic Valve Replacement Determines the Risk for Post-Procedural High-Degree AV Block and the Need for Telemetry Monitoring. JACC Cardiovasc. Interv. 2016, 9, 1269–1276.
- Mangieri, A.; Lanzillo, G.; Bertoldi, L.; Jabbour, R.J.; Regazzoli, D.; Ancona, M.B.; Tanaka, A.; Mitomo, S.; Garducci, S.; Montalto, C.; et al. Predictors of Advanced Conduction Disturbances Requiring a Late (≥48 H) Permanent Pacemaker Following Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2018, 11, 1519–1526.
- Auffret, V.; Martins, R.P.; Daubert, C.; Leclercq, C.; Le Breton, H.; Mabo, P.; Donal, E. Idiopathic/Iatrogenic Left Bundle Branch Block-Induced Reversible Left Ventricle Dysfunction: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2018, 72, 3177–3188.
- Dobson, L.E.; Musa, T.A.; Uddin, A.; Fairbairn, T.A.; Bebb, O.J.; Swoboda, P.P.; Haaf, P.; Foley, J.; Garg, P.; Fent, G.J.; et al. The impact of trans-catheter aortic valve replacement induced left-bundle branch block on cardiac reverse remodeling. J. Cardiovasc. Magn. Reson. 2017, 19, 22.
- Jorgensen, T.H.; De Backer, O.; Gerds, T.A.; Bieliauskas, G.; Svendsen, J.H.; Sondergaard, L. Mortality and Heart Failure Hospitalization in Patients With Conduction Abnormalities After Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2019, 12, 52–61.
- van Rosendael, P.J.; Delgado, V.; Bax, J.J. Pacemaker implantation rate after transcatheter aortic valve implantation with early and new-generation devices: A systematic review. Eur. Heart J. 2018, 39, 2003–2013.
- Popma, J.J.; Deeb, G.M.; Yakubov, S.J.; Mumtaz, M.; Gada, H.; O’Hair, D.; Bajwa, T.; Heiser, J.C.; Merhi, W.; Kleiman, N.S.; et al. Transcatheter Aortic-Valve Replacement with a Self-Expanding Valve in Low-Risk Patients. N. Engl. J. Med. 2019, 380, 1706–1715.
- Makkar, R.R.; Cheng, W.; Waksman, R.; Satler, L.F.; Chakravarty, T.; Groh, M.; Abernethy, W.; Russo, M.J.; Heimansohn, D.; Hermiller, J.; et al. Self-expanding intra-annular versus commercially available transcatheter heart valves in high and extreme risk patients with severe aortic stenosis (PORTICO IDE): A randomised, controlled, non-inferiority trial. Lancet 2020, 396, 669–683.
- Lanz, J.; Kim, W.-K.; Walther, T.; Burgdorf, C.; Möllmann, H.; Linke, A.; Redwood, S.; Thilo, C.; Hilker, M.; Joner, M.; et al. Safety and efficacy of a self-expanding versus a balloon-expandable bioprosthesis for transcatheter aortic valve replacement in patients with symptomatic severe aortic stenosis: A randomised non-inferiority trial. Lancet 2019, 394, 1619–1628.
- Urena, M.; Webb, J.G.; Tamburino, C.; Muñoz-García, A.J.; Cheema, A.; Dager, A.E.; Serra, V.; Amat-Santos, I.J.; Barbanti, M.; Immè, S.; et al. Permanent pacemaker implantation after transcatheter aortic valve implantation: Impact on late clinical outcomes and left ventricular function. Circulation 2014, 129, 1233–1243.
- Biner, S.; Michowitz, Y.; Leshem-Rubinow, E.; Topilsky, Y.; Ben-Assa, E.; Shimiaie, J.; Banai, S.; Keren, G.; Steinvil, A.; Finkelstein, A. Hemodynamic impact and outcome of permanent pacemaker implantation following transcatheter aortic valve implantation. Am. J. Cardiol. 2014, 113, 132–137.
- Costa, G.; Zappulla, P.; Barbanti, M.; Cirasa, A.; Todaro, D.; Rapisarda, G.; Picci, A.; Platania, F.; Tosto, A.; Di Grazia, A.; et al. Pacemaker dependency after transcatheter aortic valve implantation: Incidence, predictors and long-term outcomes. EuroInterv. J. Eur. Collab. Work. Group Interv. Cardiol. Eur. Soc. Cardiol. 2019, 15, 875–883.
- Nazif, T.M.; Dizon, J.M.; Hahn, R.T.; Xu, K.; Babaliaros, V.; Douglas, P.S.; El-Chami, M.F.; Herrmann, H.C.; Mack, M.; Makkar, R.R.; et al. Predictors and clinical outcomes of permanent pacemaker implantation after transcatheter aortic valve replacement: The PARTNER (Placement of AoRtic TraNscathetER Valves) trial and registry. JACC Cardiovasc. Interv. 2015, 8, 60–69.
- Sharobeem, S.; Boulmier, D.; Leurent, G.; Bedossa, M.; Leclercq, C.; Mabo, P.; Martins, R.P.; Tomasi, J.; Verhoye, J.-P.; Donal, E.; et al. Prognostic impact of permanent pacemaker implantation following transcatheter aortic valve replacement. Heart Rhythm 2022, 19, 1124–1132.
- Alasti, M.; Rashid, H.; Rangasamy, K.; Kotschet, E.; Adam, D.; Alison, J.; Gooley, R.; Zaman, S. Long-term pacemaker dependency and impact of pacing on mortality following transcatheter aortic valve replacement with the LOTUS valve. Catheter. Cardiovasc. Interv. Off. J. Soc. Card. Angiogr. Interv. 2018, 92, 777–782.
- Dumonteil, N.; Meredith, I.T.; Blackman, D.J.; Tchétché, D.; Hildick-Smith, D.; Spence, M.S.; Walters, D.L.; Harnek, J.; Worthley, S.G.; Rioufol, G.; et al. Insights into the need for permanent pacemaker following implantation of the repositionable LOTUS valve for transcatheter aortic valve replacement in 250 patients: Results from the REPRISE II trial with extended cohort. EuroInterv. J. Eur. Collab. Work. Group Interv. Cardiol. Eur. Soc. Cardiol. 2017, 13, 796–803.
- Meduri, C.U.; Kereiakes, D.J.; Rajagopal, V.; Makkar, R.R.; O’Hair, D.; Linke, A.; Waksman, R.; Babliaros, V.; Stoler, R.C.; Mishkel, G.J.; et al. Pacemaker Implantation and Dependency After Transcatheter Aortic Valve Replacement in the REPRISE III Trial. J. Am. Heart Assoc. 2019, 8, e012594.
- Chamandi, C.; Barbanti, M.; Munoz-Garcia, A.; Latib, A.; Nombela-Franco, L.; Gutierrez-Ibanez, E.; Veiga-Fernandez, G.; Cheema, A.N.; Cruz-Gonzalez, I.; Serra, V.; et al. Long-Term Outcomes in Patients With New Permanent Pacemaker Implantation Following Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2018, 11, 301–310.
- Urena, M.; Hayek, S.; Cheema, A.N.; Serra, V.; Amat-Santos, I.J.; Nombela-Franco, L.; Ribeiro, H.B.; Allende, R.; Paradis, J.-M.; Dumont, E.; et al. Arrhythmia burden in elderly patients with severe aortic stenosis as determined by continuous electrocardiographic recording: Toward a better understanding of arrhythmic events after transcatheter aortic valve replacement. Circulation 2015, 131, 469–477.
- Asmarats, L.; Nault, I.; Ferreira-Neto, A.N.; Muntané-Carol, G.; Del Val, D.; Junquera, L.; Paradis, J.-M.; Delarochellière, R.; Mohammadi, S.; Kalavrouziotis, D.; et al. Prolonged Continuous Electrocardiographic Monitoring Prior to Transcatheter Aortic Valve Replacement: The PARE Study. JACC Cardiovasc. Interv. 2020, 13, 1763–1773.
- Winter, J.L.; Healey, J.S.; Sheth, T.N.; Velianou, J.L.; Schwalm, J.-D.; Smith, A.; Reza, S.; Natarajan, M.K. Remote Ambulatory Cardiac Monitoring Before and After Transcatheter Aortic Valve Replacement. CJC Open 2020, 2, 416–419.
- Muntané-Carol, G.; Philippon, F.; Nault, I.; Faroux, L.; Alperi, A.; Mittal, S.; Rodés-Cabau, J. Ambulatory Electrocardiogram Monitoring in Patients Undergoing Transcatheter Aortic Valve Replacement: JACC State-of-the-Art Review. J. Am. Coll. Cardiol. 2021, 77, 1344–1356.
- Jilaihawi, H.; Zhao, Z.; Du, R.; Staniloae, C.; Saric, M.; Neuburger, P.J.; Querijero, M.; Vainrib, A.; Hisamoto, K.; Ibrahim, H.; et al. Minimizing Permanent Pacemaker Following Repositionable Self-Expanding Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2019, 12, 1796–1807.
- Sammour, Y.; Banerjee, K.; Kumar, A.; Lak, H.; Chawla, S.; Incognito, C.; Patel, J.; Kaur, M.; Abdelfattah, O.; Svensson, L.G.; et al. Systematic Approach to High Implantation of SAPIEN-3 Valve Achieves a Lower Rate of Conduction Abnormalities Including Pacemaker Implantation. Circ. Cardiovasc. Interv. 2021, 14, e009407.
- Pascual, I.; Almendárez, M.; Avanzas, P.; Álvarez, R.; Arboine, L.A.; Del Valle, R.; Hernández-Vaquero, D.; Alfonso, F.; Morís, C. Cusp-overlapping TAVI technique with a self-expanding device optimizes implantation depth and reduces permanent pacemaker requirement. Rev. Espanola Cardiol. Engl. Ed. 2021, 75, 412–420.
- Pascual, I.; Hernández-Vaquero, D.; Alperi, A.; Almendarez, M.; Avanzas, P.; Kalavrouziotis, D.; Lorca, R.; Mesnier, J.; Arboine, L.; Mohammadi, S.; et al. Permanent Pacemaker Reduction Using Cusp-Overlapping Projection in TAVR: A Propensity Score Analysis. JACC Cardiovasc. Interv. 2022, 15, 150–161.
- Lilly, S.M.; Deshmukh, A.J.; Epstein, A.E.; Ricciardi, M.J.; Shreenivas, S.; Velagapudi, P.; Wyman, J.F. 2020 ACC Expert Consensus Decision Pathway on Management of Conduction Disturbances in Patients Undergoing Transcatheter Aortic Valve Replacement: A Report of the American College of Cardiology Solution Set Oversight Committee. J. Am. Coll. Cardiol. 2020, 76, 2391–2411.
- Ream, K.; Sandhu, A.; Valle, J.; Weber, R.; Kaizer, A.; Wiktor, D.M.; Borne, R.T.; Tumolo, A.Z.; Kunkel, M.; Zipse, M.M.; et al. Ambulatory Rhythm Monitoring to Detect Late High-Grade Atrioventricular Block Following Transcatheter Aortic Valve Replacement. J. Am. Coll. Cardiol. 2019, 73, 2538–2547.
- Tian, Y.; Padmanabhan, D.; McLeod, C.J.; Zhang, P.; Xiao, P.; Sandhu, G.S.; Greason, K.L.; Gulati, R.; Nkomo, V.T.; Rihal, C.S.; et al. Utility of 30-Day Continuous Ambulatory Monitoring to Identify Patients With Delayed Occurrence of Atrioventricular Block After Transcatheter Aortic Valve Replacement. Circ. Cardiovasc. Interv. 2019, 12, e007635.
- Muntané-Carol, G.; Okoh, A.K.; Chen, C.; Nault, I.; Kassotis, J.; Mohammadi, S.; Coromilas, J.; Lee, L.Y.; Alperi, A.; Philippon, F.; et al. Ambulatory Electrocardiographic Monitoring Following Minimalist Transcatheter Aortic Valve Replacement. JACC Cardiovasc. Interv. 2021, 14, 2711–2722.
- Reiter, C.; Lambert, T.; Kellermair, J.; Blessberger, H.; Fellner, A.; Nahler, A.; Grund, M.; Steinwender, C. Delayed Total Atrioventricular Block After Transcatheter Aortic Valve Replacement Assessed by Implantable Loop Recorders. JACC Cardiovasc. Interv. 2021, 14, 2723–2732.
- Tovia-Brodie, O.; Michowitz, Y.; Belhassen, B. Use of Electrophysiological Studies in Transcatheter Aortic Valve Implantation. Arrhythmia Electrophysiol. Rev. 2020, 9, 20–27.
More
Information
Subjects:
Cardiac & Cardiovascular Systems
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.2K
Entry Collection:
Hypertension and Cardiovascular Diseases
Revisions:
4 times
(View History)
Update Date:
21 Nov 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




