The degradation of HA is executed by endogenous hyaluronidases, endo-beta-N-acetylhexosaminidases that hydrolyze endogenous and exogenous HA. In humans, six homologous genes encoding for hyaluronidases have historically been described: HYAL-1 through HYAL-4, PHYAL-1, and SPAM-1
[34]. Of these, HYAL-1 and 2 are by far the most active in human tissues, with HYAL-2 existing as a free, unbound enzyme responsible for the breakdown of most extracellular HA into intermediate-sized polysaccharides and HYAL-1 serving as the membrane-bound form in lysosomes capable of further degrading endocytosed HA into its constituent monosaccharides
[35]. The intravascular half-life of hyaluronidases is short, spanning only 2–3 min because of the presence of plasma glycoprotein inhibitors
[36]. In tissues, hyaluronidases have a more prolonged activity, remaining active for 24–48 h; nevertheless, some murine studies have shown a complete drop in activity after 3–6 h
[37][38]. For this reason, hyaluronidase re-dosing every 1–6 h has been recommended in cases of FIVO
[39]. Additionally, other HA degradation pathways have been described recently that also bear significance. Specifically, the clearance of intravascular HA appears to rely on endocytosis via HARE (HA receptor for endocytosis)-mediated binding by the sinusoidal endothelial cells in the liver and spleen
[40]. In addition, a new membrane-bound protein, HYBID (hyaluronan binding protein involved in hyaluronan depolymerization), has been identified and shown to play a significant role in HA turnover in the skin. HYBID appears to participate in an endocytosis-mediated breakdown of extracellular HA and its senescence-related dysfunction has been implicated in the pathophysiology of skin elastosis and aging
[41].
The commercial manufacturing of raw HA precursors constitutes a multi-billion-dollar industry subserving a wide range of cosmetic, dietary, and pharmaceutical-grade products
[42]. The production of injectable HA gels requires HMW (>1000 kDa) raw HA that must adhere to established safety and purity standards
[43]. Bacterial fermentation is currently the largest source of HMW HA, having largely supplanted the more-costly, lower-yield, animal-derived preparations from rooster combs and bovine vitreous. Specifically, the bacterium
S. equis, subspecies
zoopidemicus—a gram-positive, capsule-forming Lancefield type C streptococcus—is the most-commonly employed strain used in HA production
[44]. Compared with animal-derived sources, bacterial-based methods demonstrate enhanced-purity, higher molecular weight, lower immunogenicity, and greater product yield
[45]. Nonetheless, new heterologous recombinant expression systems harnessing
B. subtilis and even cell-free in vitro production systems employing a soluble form of Class II HA synthases show promise in further achieving enhanced yield rates, higher molecular weight chains, and diminished polydispersity
[46][47][48]. Prior to serving as the raw ingredient in the fabrication of dermal fillers, HMW HA (500–2500 kDa) derived from bacterial cultures is precipitated in isopropanol before undergoing a robust purification process that removes endogenous toxin remnants from the streptococcal source
[49].
3. Pathophysiology of HA-Mediated Vascular Occlusion
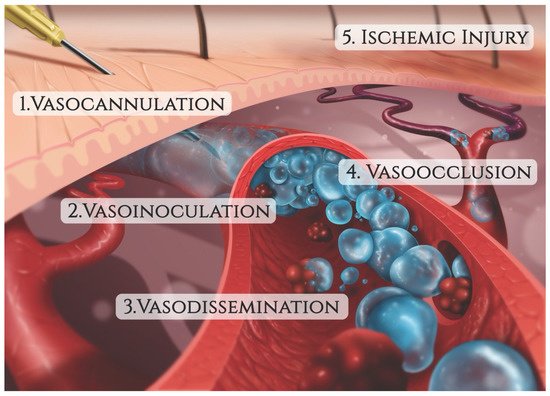
The mechanism of injury in FIVO represents a multifactorial cascade of events that includes vasocannulation, vasoinoculation, vasodissemination, and vasoocclusion, resulting in tissue underperfusion and ischemia (
Figure 1). Although arterial compression by extravascular filler boluses is recognized as a valid alternative etiology of FIVO, such a mechanism is rare outside of instances involving surgerized tissues with a tenuous blood supply or those nourished by end-arteries with absent cross-perfusion from adjacent angiosomes. In normal tissues, compression is likely to result in diminished blood flow, inducing pallor and decreased capillary refill, but without complete loss of perfusion or tissue necrosis
[55]. In mouse and rabbit FIVO models, arterial compression by filler could not be induced and did not result in any prolonged period of significant underperfusion or ischemia
[56][57]. In humans, single-point obstructions of facial vessels are easily overcome by a vastly redundant blood supply from adjacent angiosomes, via true anastomoses, which dilate post filler-placement
[58]. Even in instances of bilateral external carotid artery (ECA) ligation, historically performed for intractable epistaxis, compensatory flow from the internal carotid artery (ICA) system has been sufficient to avoid tissue necrosis
[59][60][61]. Therefore, outside of compression of distal arterial branches in patients with abnormally underperfused tissues, the intravascular model of FIVO is likely to be the most prevalent. In this section, researchers review the pathophysiology of this intravascular model and outline preventative and therapeutic opportunities that exist along each phase of injury.
Figure 1. The sequence of events leading to filler-induced vascular occlusion (FIVO).
3.1. Vaso-Cannulation
The accidental penetration of a blood vessel during active filler injection represents the triggering event that immediately precedes FIVO
[62][63]. Blunt-tipped microcannulas and sharp hypodermic needles, both routinely employed in aesthetic injectable treatments, can potentially perforate vessel walls and initiate intraluminal inoculation of filler. Microcannulas, because of their flexible shaft and closed tip configuration, have generally been regarded as more prudent and are endorsed by multiple consensus panels on injection safety
[64][65]. Compared with needles, microcannulas cause less tissue trauma, pain, edema, and bruising, and can achieve a more reliable plane-specific placement of filler
[66][67][68][69]. When employed by specialized practitioners with knowledge of vascular anatomy, microcannula use has demonstrated a significantly lower risk of FIVO compared with needle injections
[70]. Nevertheless, higher gauge microcannulas (27 g and up) have vasopenetration forces equivalent to those of needles (1–2 kg⋅m/s
2), suggesting that their safety advantage is limited or nonexistent in many treatment applications
[71][72].
The likelihood of vessel cannulation also depends on the force necessary to advance a needle/cannula subcutaneously. Histologically, the central facial tissues of the perioral and perinasal regions feature thicker, more fibrous interconnections between the muscular aponeurosis and the skin (
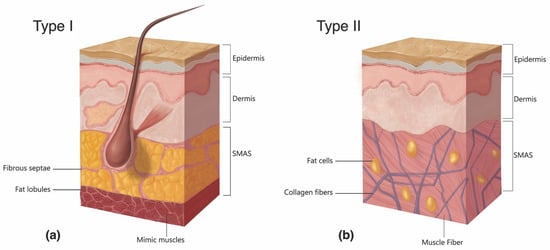
Figure 2)
[73]. In those regions, the superficial musculoaponeurotic system (SMAS) displays a type II morphology, which lacks the soft intervening adipose layer and smooth gliding plane that characterize the type I tissues of the lateral face. The more restrained nature of vessels within type II SMAS and the tissue’s greater resistance to cannulation mean that even blunt devices, such as microcannulas, may easily perforate through vascular structures, as evidenced by multiple illustrative case reports
[74][75][76][77][78].
Figure 2. The two types of histomorphology of the facial superficial musculoaponeurotic system (SMAS). (a) Type I morphology is found predominantly in the cheek, forehead, and lateral face and features a uniform layer of adipose tissue interspersed amidst the fibrous septa spanning the space between the SMAS and the dermis. (b) Type II morphology is present in the central facial tissues of the perioral and perinasal regions and is characterized by thick fibromuscular insertions emanating from the SMAS directly into the dermis, forming a more rigid adhesion between the two planes.
Because of the central role of vaso-cannulation in the mechanism of FIVO, preventative steps have been suggested that help reduce the odds of intraluminal placement. Pre-injection aspiration, in which the plunger of the syringe is pulled back to generate a negative-pressure screening for visible blood, has been controversial at best
[79][80]. Although a positive aspiration may equate with a higher likelihood of intravascular placement, the unsteady movements transmitted to the tip during aspiration may arguably negate any preventative value from this maneuver beyond that of false reassurance. Furthermore, the routine use of a stationary injection technique, itself necessitated by the practice of aspiration, mandates the bolus-based placement of filler that could magnify the potential degree of injury
[81]. In addition, filler-primed needle hubs, which characterize the majority of injections, carry a high incidence of false-negative aspirations, creating a misleading perception of safety
[82]. Nonetheless, aspiration with both air- and saline-primed needles has demonstrated excellent sensitivity in both in vitro and in vivo testing in medium-sized arteries, though its incorporation into clinical practice could prove cumbersome and time-consuming
[83].
The use of Doppler ultrasound (US) has recently grown in acceptance as a means of identifying aberrant/anomalous vascular structures prior to dermal filler injection and avoiding accidental vaso-cannulation
[84][85]. Proponents of US advocate its routine use predominantly in high-risk areas—such as the ophthalmic artery-supplied territories of the forehead, glabella, and nasal dorsum —where it can be employed for both arterial mapping and ultrasound-guided filling
[86][87][88]. US may also prove useful in cases of FIVO, helping to identify sites of vascular occlusion and assisting with the precise delivery of reversal agents
[89][90]. However, the significant cost, skill training, and time-consuming aspects of US use in clinical practice have thus far limited its widespread adoption
[91]. As portable US technology continues to evolve, this real-time imaging modality is likely to play a more pivotal role in the prevention and management of vascular occlusion injuries.
3.2. Vaso-Inoculation
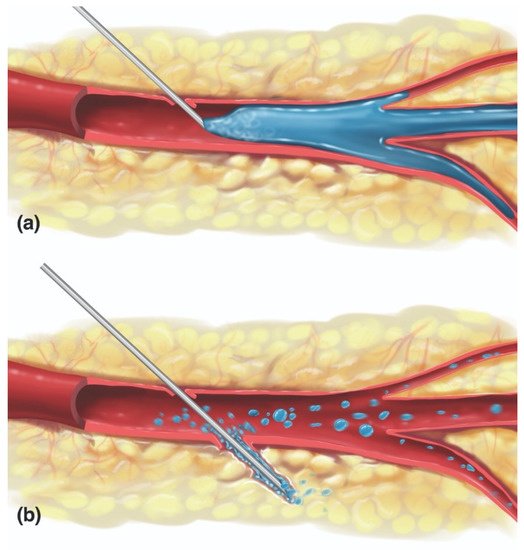
In FIVO, the intraluminal inoculation of a blood vessel represents a brief, but significant event in which a variable amount of filler undergoes a pressurized delivery into the intravascular milieu. Conceptually, different mechanisms of inoculation exist depending on the positioning of the needle/cannula tip relative to the lumen of the vessel: intraluminal versus extraluminal (
Figure 3)
[92]. Intraluminal positioning results in a more efficient delivery of inoculum than extraluminal placement, in which the material must work back into a vessel along the track created by the needle/cannula. Given the blind nature of filler injections and the substantial needle movements that occur during filling, especially in light of the small diameters of most facial vessels, a combination of extraluminal and intraluminal mechanisms is likely to occur.
Figure 3. Mechanisms of vaso-inoculation. (a) Direct intraluminal injection. (b) Indirect extraluminal inoculation following trans-arterial perforation.
The injection of a viscoelastic hydrogel into an arterial lumen requires a favorable pressure gradient, such that sufficient force must be applied to the plunger to overcome the mean arterial pressure
[93]. In a fresh cadaver head perfusion model, Cho et al. found that an average injection pressure of 166 mm Hg was sufficient to inoculate the supratrochlear artery (STrA) with Juvéderm Ultra and retrogradely fill the ophthalmic artery back to the takeoff point of the retinal artery
[94]. Because of the pseudoplastic nature of HA dermal fillers, ejection pressures required to overcome the gel’s yield stress—upon which gel fillers begin to flow smoothly through the narrow lumen of a needle—are well above mean arterial values
[95]. Lee et al. demonstrated that even soft fillers with a low shear elastic modulus (G’) and high tan delta extruded from a 25 g needle at a pressure of 580 mm Hg, with maximal extrusion pressures as high as 6500 mm Hg for high G’ fillers injected through 30 g needles
[96]. Given these elevated ejection pressures, any cannulation of a vessel that occurs during active filler injection is likely to result in vaso-inoculation, underscoring the need for better preventative steps that help minimize the former.
In FIVO, the volume of inoculum strongly influences the extent of the resultant injury. Small, microscopic amounts of HA gel are likely to be immediately dispersed and embolized distally, whereas large boluses may form an advancing plug that completely occludes a segment of the vascular lumen
[97]. Because even the largest extracranial facial vessels feature narrow luminal sizes ranging between 1 and 2 mm in diameter, the volumes of filler required to completely occlude a large segment of an artery are small
[98][99][100][101][102]. Cho et al. and Kahn et al. revealed that as little as 0.05–0.1 mL can extensively occlude the 5 cm segment of ophthalmic artery located between its supratrochlear and retinal branches
[94][103]. Given the rapid, high-pressure extrusion dynamics characteristic of filler injections against the relatively small volume/low resistance characteristics of facial vessels, even brief inoculation periods can deliver sufficient filler to cause obstruction
[94]. In addition, because of the high viscosity and cohesivity of many HA fillers—with drop weights ranging from 15 to 50 mg—even small amounts of HA filler may potentially achieve a complete blockage of facial vessels
[104]. Thus, the injection force and speed strongly influence the volume of intravascular inoculum, and thus also the extent of injury. Consequently, several safety consensus panels have recommended that practitioners employ a slow, low-pressure injection technique during treatment and limit filler bolus sizes to less than 0.1 mL
[105][106].
3.3. Vaso-Dissemination
The intravascular behavior of HA gels is incompletely understood, but several animal studies and post hoc histopathological analyses have offered insight into the patterns of dissemination of dermal fillers
[107][108][109]. The type of blockade induced by HA gels seemingly depends on the volume of inoculum as well as the rheological properties and particle size profile of the offending product. Small amounts of a low-viscosity filler injected into a large-caliber artery likely result in complete distal dispersion, while large volumes of a high-viscosity filler are more likely to produce an obstructive plug. Nie et al. proved this to be true by showing a higher rate of total, irreversible vessel occlusion with HA (Restylane
®) than compared with injections of a lower viscosity, small-particle polymethylmethacrylate (PMMA) filler (Artecoll
®; Hafod BV, Rotterdam, The Netherlands) in the rabbit-ear model
[97]. However, a comparative rabbit ear study employing equivalent amounts of different HA (Restylane
®, Juvederm
® Ultra, and Belotero
®) and non-HA (Radiesse
®; Merz USA, Greensboro, NC, USA) products did not identify differences in the extent of ischemic injury or necrosis, suggesting that most HA fillers are more alike than they are dissimilar in their intravascular dispersal
[57].
The vaso-disseminating behavior of a gel inoculum is also dictated by whether the affected vessel is arterial or venous in nature. Arterial inoculations are probably responsible for most of the local injuries occurring in the head and neck, while venous cannulations likely account for the majority of distant injuries (
Table 2), although exceptions may occur owing to the presence of arteriovenous shunts, which have been described within the head and neck
[110]. Intravenously placed facial filler can remain stationary—inciting a locoregional thrombophlebitic reaction that may intensify up to cerebral sinus thrombosis—or may undergo cardiopetal embolization to ultimately lodge within the pulmonary arterial tree, resulting in a pulmonary embolism
[111][112]. Furthermore, venous occlusions can contribute to tissue ischemia even in cases stemming from arterial-cannulation because of the presence of arteriovenous shunting, contributing to superimposed congestive venous failure
[113]. Ultimately, however, whether they are local, distant, venous, or arterial, the ischemic injury mechanism incited by FIVO bears an arterio-occlusive etiology. As a result, in this section, the intra-arterial mechanisms of filler dispersal will be the predominant focus of discussion.
Table 2. Examples of proximal and distant arteriovenous occlusive sequelae that may arise from filler-induced vascular occlusion (FIVO) of facial-onset.
| Arterial * |
Venous |
| Muco-Cutaneous/Soft Tissue Necrosis |
Local Venous Thrombophlebitis |
| Vision Loss +/− Ophthalmoplegia |
Cerebral Sinus Thrombosis |
| Ischemic Cerebral Stroke |
Pulmonary Embolism |
| Facial Paralysis/Peripheral Nerve Injury |
Myocardial Infarction (PFO **) |
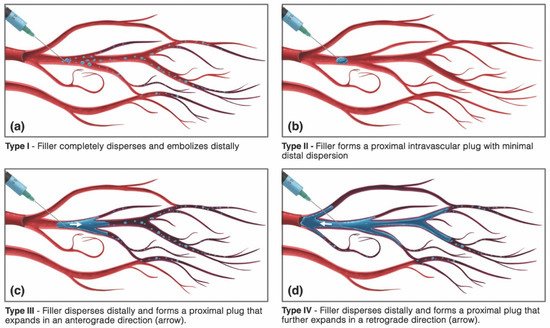
Conceptually, four different patterns of vaso-dissemination of HA filler are possible, depending on the volume of inoculum and properties of the filler (Figure 4).
Figure 4. Possible vaso-dissemination mechanisms of intravascular hyaluronan gels. (a) Type I, filler completely disperses and embolizes distally, clearing the main lumen. (b) Type II, filler does not disperse and instead forms a proximally occlusive intraluminal plug. (c) Type III, filler disperses distally and forms a proximal intravascular plug that expands in an anterograde direction. (d) Type IV, filler disperses distally and forms a proximal intravascular plug that further expands in a retrograde direction, causing the additional occlusion of upstream branches.
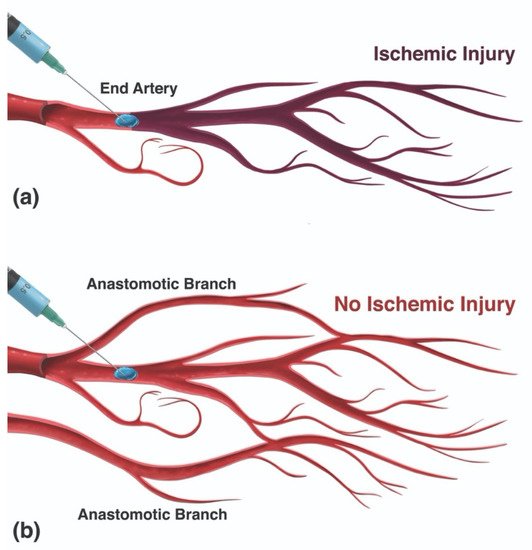
In type I, the filler is completely dispersed and embolized into the distal vascular tree, resulting in the complete elimination of the gel material from within the main arterial lumen. Type I vaso-dissemination is likely to occur with low-volume injections of low-viscosity/non-cohesive fillers into large-caliber vessels. Conversely, type II dissemination represents the formation of an isolated proximally obstructive plug at the site of injection within the main arterial lumen without any significant distal dispersion. A single-point occlusion can result in varying outcomes, from a minimal perfusion defect to an extensive injury, depending on the availability of distal anastomotic collateral circulation (Figure 5). Type II dissemination requires a higher viscosity/cohesivity filler injected in sufficiently large volumes to form a plug. Finally, type III and IV patterns feature a combination of both distal dispersion and proximal luminal obstruction and are likely the most common patterns, occurring with soft, moderately dispersible filler materials injected in sufficiently large volumes. Type IV patterns differ from type III by having the additional retrograde advancement of filler, which can result in the embolization and blockage of further upstream branches.
Figure 5. Influence of the configuration of a vascular network on the likelihood of tissue underperfusion/ischemia with a type II dissemination pattern. (a) In an end-arterial configuration, such as that seen with the retinal arterial system, a proximally obstructive plug can result in a significant decrease in tissue perfusion and a higher likelihood of ischemia. (b) In the presence of collateral perfusion supplied by anastomotic branches, a proximal plug is not likely to result in significant underperfusion or ischemia.
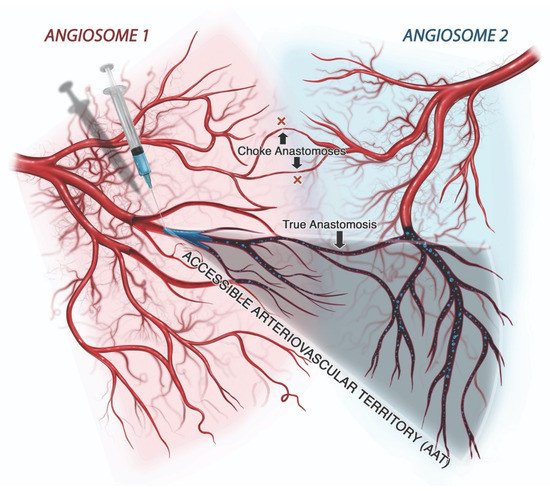
The extent of filler dissemination, and thus the potential severity of injury that may be incited by the inoculation of an artery, depends on the effective size of its accessible arteriovascular territory (AAT). The AAT represents the segments of all affected angiosomes that are susceptible to filler occlusion, i.e., the conglomerate of all arterial branches located distal to the most proximal site of occlusion into which filler may naturally spread, causing obstruction (
Figure 6)
[114]. As described by Taylor and others, the size of the functional angiosome, and hence the AAT, depends on the presence of true anastomoses and the behavior of choke vessels
[115][116]. True anastomoses function as permanent connections between adjacent arterial territories or across arteriovenous shunts, effectively increasing the size of the AAT, often dramatically
[117]. In contrast, choke vessels tend to restrict access to adjacent arterial territories in a reflexive manner that is thought to be protective, reducing the AAT
[118]. However, the constriction of choke vessels probably contributes to decreased tissue perfusion in cases of FIVO, just as it does in surgical flaps, potentially compounding the degree of ischemia
[119][120]. Thus, the dissemination of intravascular filler depends on multiple variables, many of which are patient-, tissue-, and filler-specific, resulting in differing patterns of occlusion.
Figure 6. Conceptual illustration of the accessible arteriovascular territory (AAT). The AAT represents the conglomerate of vessels and their downstream anastomotic connections into which filler particles may disseminate following accidental intravascular inoculation. The AAT may involve more than one angiosome because of the presence of true anastomoses, which serve as vascular connections linking two angiosomes or, more distally, two perforasomes. Choke vessels, which function as gatekeepers, act as dynamic anastomoses that either permit cross-perfusion of tissues or, in cases of filler-induced vascular occlusion, limit the ability of filler to spread to adjacent angiosomes through a protective vasoconstrictive reflex.