
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Nicolas Germain | -- | 4674 | 2022-04-07 14:59:36 | | | |
| 2 | Nicolas Germain | Meta information modification | 4674 | 2022-04-07 15:00:52 | | | | |
| 3 | Vivi Li | + 742 word(s) | 5416 | 2022-04-08 04:51:34 | | |
Video Upload Options
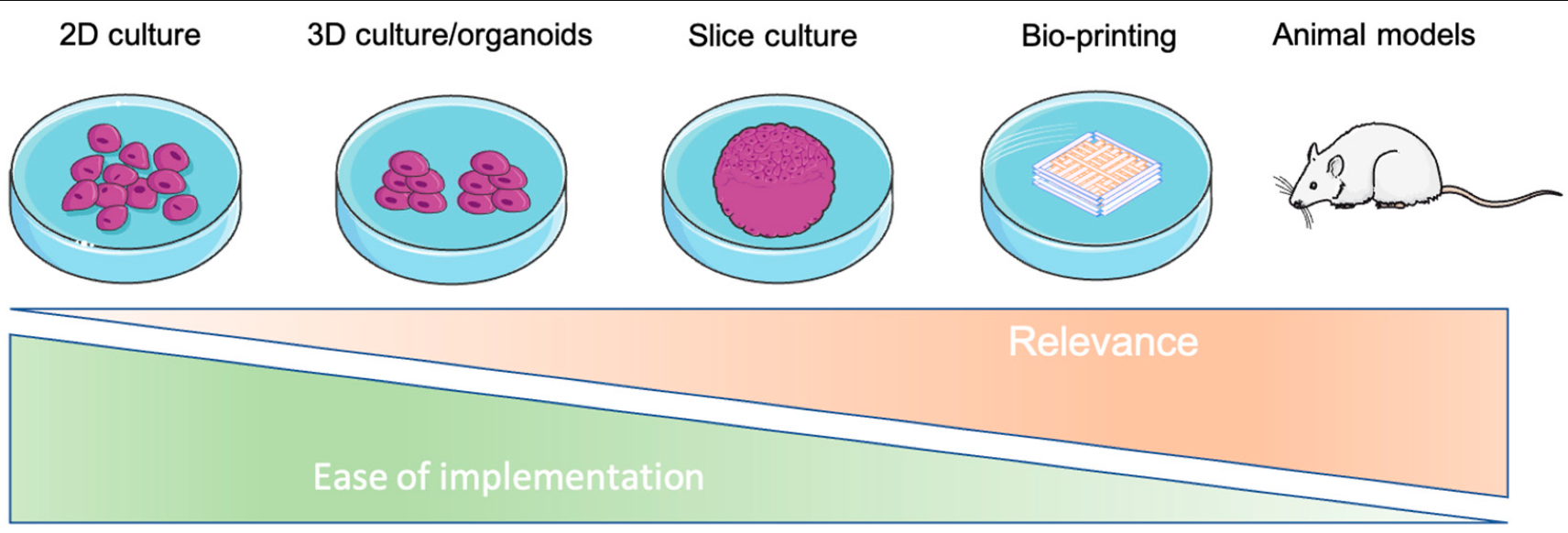
Tumor cells evolve in a complex and heterogeneous environment composed of different cell types and an extracellular matrix. Current 2D culture methods are very limited in their ability to mimic the cancer cell environment. Various 3D models of cancer cells have been developed, notably in the form of spheroids/organoids, using scaffold or cancer-on-chip devices. However, these models have the disadvantage of not being able to precisely control the organization of multiple cell types in complex architecture and are sometimes not very reproducible in their production, and this is especially true for spheroids. Three-dimensional bioprinting can produce complex, multi-cellular, and reproducible constructs in which the matrix composition and rigidity can be adapted locally or globally to the tumor model studied. For these reasons, 3D bioprinting seems to be the technique of choice to mimic the tumor microenvironment in vivo as closely as possible.
1. 3D Bioprinting at a Glance
1.1. Introduction
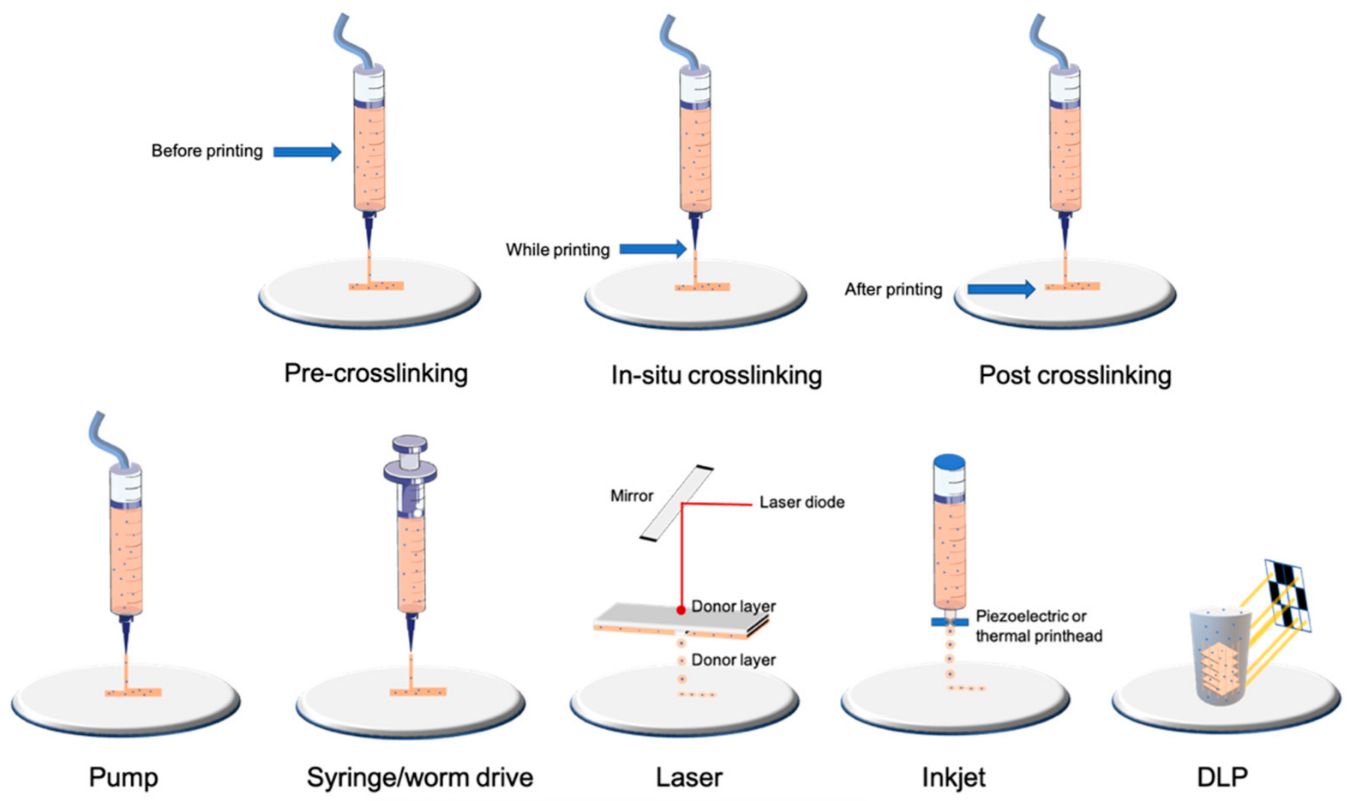
1.2. Bioprinting Technologies
| Type of Technology | Example of Printing Method | Advantages | Disadvantages | Cell Density | Average Cell Viability | Crosslinking | References |
|---|---|---|---|---|---|---|---|
| Droplet-based | Laser | Very high accuracy and resolution Low shear stress Very expensive |
Only low-viscosity bioinks Only 2D patterns (limited high) |
Low (less than 10 million per mL) | High | Depends on biomaterial used | [14][15] |
| Inkjet | High accuracy Low shear stress |
[16][17] | |||||
| Filament-based | Worm drive Pneumatic Syringe/piston |
Large panel of bioinks available Low cost Highly tunable |
Higher shear stress and lower cell viability than other bioprinting technologies | High (more than 10 million per mL) | Medium/high depending on nozzle and pressure | Depends on biomaterial used | [13][18][19][20] |
| Plane-based/Volumetric | DLP/SLA | Fast for large and complex 3D models Very high accuracy |
Few bioinks available Waste of bioink due to its conception |
High (more than 10 million per mL) | High | Photocurable by DLP/SLA technology | [21][22][23][24][25] |
2. Characterization of Cells after Bioprinting
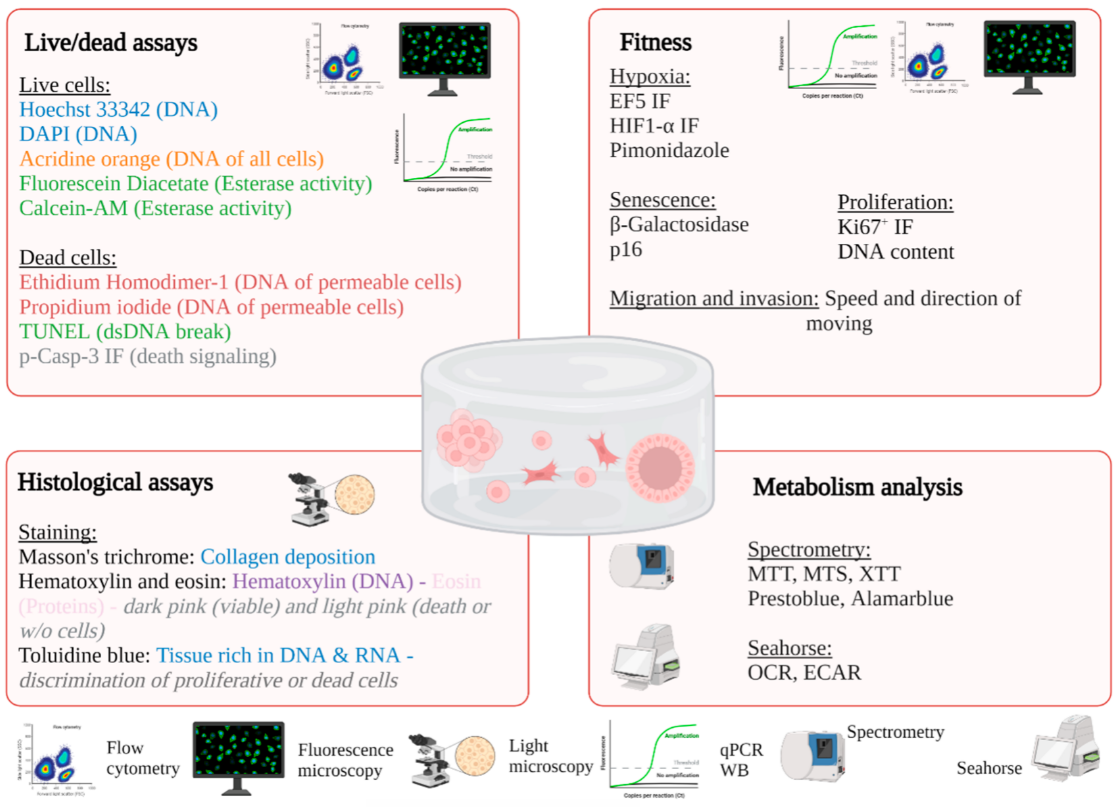
2.1. In Situ Characterization of Cells
2.1.1. Light Microscopy
2.1.2. Fluorescence Microscopy
| Material | Type of Bioink | Bioprinting Technology | Tissue Engineering Model | Cancer Models | Advantages | Drawbacks | Type of Crosslinking | References | |
|---|---|---|---|---|---|---|---|---|---|
| Bioink derived from natural biomaterials | Alginate-based | Natural polysaccharide (brown algae) |
Drop-based Filament-based |
Vascular, cartilage, bone, neural tissue, fibroblast, and many more | Drug delivery Cancer stem cell research Breast cancer, melanoma, and many more cancers Tumor spheroids |
Low cost Good printability Excellent bio-compatibility |
Poor cell adhesion Fast degradation |
Ionic | [46][47][48][49][50][51][52] |
| Gelatin-based | Natural protein (bovine skin and tendon) |
Drop-based Filament-based Plane-based |
Vascular, cartilage, bone, muscle, fibroblast, and many more | Cholangiocarcinoma, bladder cancer, and many more cancers Tumor spheroids |
Excellent bio-compatibility Low-cost High cellular adhesion |
Low viscosity at room or higher temperatures Need a temperature-controlled (cooled printhead) and a cooled printbed Low mechanical strength (higher if blended with methacrylate) |
Chemical Thermal UV Covalent Enzymatic |
[50][53][54][55][56][57][58] | |
| Cellulose and nanocellulose-based | Natural polysaccharide obtained from the biosynthesis of plants or bacteria | Filament-based | Cartilage and bone | Drug delivery Gastric, cervical, pancreatic, and many more cancers |
Great similarity with ECM Excellent bio-compatibility |
Low viscosity for cellulose nanocrystals Mainly used mixed with other natural biomaterials |
Enzymatic UV |
[59][60][61][62][63] | |
| Matrigel | Solubilized basement membrane matrix secreted by Engelbreth-Holm-Swarm (EHS) mouse sarcoma cells | Filament-based Drop-based |
Vascular, liver, bone, lung, and many more | Tumor spheroids Many types of cancer |
Most used material in cancer research Excellent bio-compatibility Very well characterized for organoid/spheroid formation |
Cannot be used alone due to its complex rheological behavior and low mechanical properties Limited use in vivo due to its mouse tumor origin Expensive High batch variability |
Thermal | [64][65][66][67][68] | |
| Collagen-I-based | Natural protein (rat tail or bovine skin and tendon) | Drop-based Filament-based |
Hard tissues (bone, osteochondral, cartilage) Skin, cardiovascular, and liver tissues; nervous system; and cornea |
Tumor spheroids Neuroblastoma, breast cancer |
Excellent bio-compatibility High cellular adhesion Minimal immunogenicity Excellent printability Enzymatically degradableMechanical and structural properties close to native tissue |
Low shape fidelity | pH Thermal |
[69][70][71][72] | |
| Hyaluronic-acid-based | Natural polysaccharide (bacterial fermentation or animal products) | Filament-based | Hard tissues (bone, osteochondral, cartilage) | Tumor spheroids Melanoma, breast cancer |
Excellent bio-compatibility Highly tunable (wide variety and high degree of potential chemical modifications) Interact with cell receptors |
Poor mechanical strength Mainly used mixed with other natural biomaterials |
Depends on the other biomaterial/chemical modifications Physical or covalent |
[73][74][75][76] | |
| Agarose-based | Natural polysaccharide derived from red seaweed | Filament-based | Bone, vascular, neural, and adipose tissue | Leukemia | Good biocompatibility Great similarity with ECM Thermo-reversible gelling |
Poor cell survival if not blended with another biomaterial Poor printability (needs high temperature for dispensing (70 °C) and gels at low temperatures) |
Thermal Ionic |
[65][77][78] | |
| Fibrin-based | Natural protein (human plasma) |
Filament-based Drop-based |
Muscular, neural, skin, and adipose tissue, wound healing model | Drug release Glioblastoma |
High shape fidelity (depending on fibrinogen–thrombin concentration) Excellent biocompatibility Enzymatically degradable |
Medium cell adhesion Low mechanical properties |
Enzymatic (fibrinogen–thrombin) | [79][80][81] | |
| Silk-derived | Natural protein (bombyx mory) |
Filament-based | Hard tissues (bone, osteochondral, cartilage), vascular tissue | Drug delivery | High shape fidelity Low Cost Good biocompatibility |
Lacks cell-binding domains Medium cell viability Needs other supportive material for cell proliferation (alginate, gelatin, etc.) Poor printability performance |
Enzymatic Physical |
[82][83][84][85] | |
| Gellan gum | Natural polysaccharide | Filament-based | Hard tissues (bone, osteochondral, cartilage), brain-like structures | Drug delivery | Excellent biocompatibility Low cost Rapid gelation |
Poor printability performance | Thermal | [86][87][88] | |
| Chitosan | Natural polysaccharide produced by deacetylation of chitin (extract from shrimps) | Filament-based Drop-based Plane-based |
Hard tissues (bone, osteochondral, cartilage), vascular, skin, and hepatic tissues | Drug delivery | Good biocompatibility Medium to high cell viability |
Medium cell adhesion Low shape fidelity Low mechanical properties |
Ionic UV |
[89][90][91] | |
| Polypeptides | Corning (PuraMatrix) | Filament-based Droplet-based Plane-based |
Liver, neural | Ovarian cancer | Self-assembly Adapted for soft-tissue applications and in conjunction with other materials |
Low pH leading to low cell viability | Ionic-complementary self-assembly | [92][93] | |
| De-cellularized matrix-based (dECM) | Natural matrix | Filament-based | Adipose, hepatic, and heart tissues; MSCs; cancer models | Many tumor models depending on dECM | Renders natural ECM Tissue-specific |
Low mechanical properties Protein denaturation during fabrication processes Poor printability if not mixed with another biomaterial Long procedure |
Depends on the other biomaterial/chemical modifications | [94][95][96][97] | |
| Bioink derived from synthetic biomaterials | AM (acrylamide) | Polyacrylamide | Filament-based Plane-based Droplet-based |
Different stiffness models | Melanoma, breast cancer | Wide range of elasticity Most standardized protocol |
Suitable for 2D culture only or necessary to couple it with another material | UV | [98][99] |
| PCL/PLGA | Poly(caprolactone)/Poly(lactic–glycolic acid) | Filament-based Drop-based |
Hard tissues (bone, osteochondral, cartilage) | Mainly depends on the natural biomaterial used | Good mechanical strength Controllable rate of degradation |
Mainly used as a scaffold (melting temperature around 60 °C not compatible with cell viability) Needs other supportive material for cell proliferation (alginate, gelatin, etc.) |
Depends on the natural biomaterial used | [100][101][102] | |
| PEG | Polymer of ethylene oxide | Filament-based | Vascular and bone tissue | Highly tunable (mechanical properties, polymerization, chemical composition) | Needs chemical modification to be printed Requires the addition of bioactive molecules to allow cellular interaction (high hydrophobicity) |
UV if mixed with a photoinitiator Condensation Michael-type addition Click chemistry Native chemical ligation Enzymatic reaction |
[103][104][105] | ||
| Pluronic | Triblock copolymer of poly(ethylene glycol)-poly(propylene oxide)-poly(propylene glycol) | Filament-based | Cartilage | High shape fidelity Good printability |
Lacks cell-binding domains Low cell viability Poor mechanical strength |
Covalent | [106][107] | ||
| PU | Polyurethane | Filament-based | Cartilage Neural stem cells |
Good biocompatibility and biodegradability High mechanical strength |
Needs other supportive material for cell proliferation (alginate, gelatin, etc.) | Depends on the natural biomaterial used | [108][109] |
2.1.3. Electronic Microscopy
2.2. Characterization of Cells after Isolation or Lysis
2.2.1. Molecular Biology
2.2.2. Flow Cytometry
| Methods | Description | Pros and Cons | Markers | REF | |
|---|---|---|---|---|---|
| Microscopy | |||||
| Light | Phase contrast | Monitoring of proliferation and morphology of cells | +: • Nondestructive • No markers are added • Low cost • Easy with transparent gels (GelMA, matrigel) −: • No possibility to identify subcellular structures • Difficult with opaque or non-transparent gels (e.g.,: alginate with nanocellulose) |
Not suitable | [31][32][33] |
| Bright field | The transmission of light is more or less attenuated depending on the density or marking of the sample | +: • Suitable for large samples −: • Requires histological staining • Preparation of sample • Quantification of thick sample |
Hematoxylin–eosin Masson’s trichrome Trypan blue |
[32][33][34] | |
| Fluorescence | LSM Epifluorescence Confocal |
The use of a fluorescent marker is necessary to highlight a subcellular structure; possibility of monitoring structures over time (if vital markers) | +: • Monitoring of many possible structures −: • Requires cutting for oversized constructions for epi and confocal microscopy • Need to fix for certain markers • Important autofluorescence for chitosan or alginate/cellulose hydrogels in UV |
Live/dead staining Or calcein AM/propidium iodide Or ethidium homodimer Active-caspase3/7 green Hoechst 33342 HIF1-α, Ki67 |
[39][40][41][42][123] |
| Electronic | Scanning | Surface is scanned with a beam of electrons, emitted signal provides images | +: • High resolution −: • The preparation procedure is tedious • Frequent preparation artifacts (collapse) |
Not suitable | [33] |
| Transmission | The part of beam of electrons is transmitted into specimens allowed to obtain images | Not suitable | [33][110] | ||
| Flow cytometry | |||||
| Flow cytometry | Analysis of physical parameters (size and granularity) for each cell but also the level of fluorescence | +: • Quantitative analysis −: • Disaggregation can be a problem • Necessity to have a large cell number due to loss of cells during dissociation |
7-AAD CFSE |
[33][117] | |
| Spectroscopy | |||||
| Spectrometry or fluorimetry | Production or utilization of a fluorescent or chromatic compound | +: • Well-described for 2D culture and frequently used • Can be used for kinetic monitoring −: • Ensure that the efficiency is adapted for 3D |
ACP, LDH, prestoblue, alamar blue, DNA content | [43][124][125][126] | |
| Molecular biology | |||||
| RTqPCR Western blot |
Quantification of gene expression at mRNA or protein level | +: • Quantitative analysis • Easier by using the enzymatic method on natural inks (e.g., collagenase for GelMA or ColMA, hyaluronidase for hyaluronic acid) −: •Adaptation of the homogenization and extraction protocol to obtain an adequate quantity and quality of RNA/proteins for analyses |
Bax/Bcl2 HIF1-α, Ki67 |
[34][110][119] | |
| Metabolism | |||||
| GC–MS (Gas chromatography–mass spectrometry) | Detection of molecules of interest according to their mass/charge ratio after ionization | +: • Considerably less cellular material compared to NMR, high sensitivity, −: • Use of radioisotopes, complex sample preparation, high cost |
13C-Glucose | [127][128] | |
| NMR (nuclear magnetic resonance) spectroscopy | Determination of the composition of a sample by applying a magnetic field via the orientation of the nuclear spins of the atoms | +: • High reproducibility, sample can be analyzed directly, low cost −: • Use of radioisotopes, low sensitivity |
[129][130] | ||
| PET scan (positron emission tomography) | Injection of a radiographic tracer and monitoring by imaging to detect localization of [18F]FDG | +: • Classically used in medicine, monitoring over time −: • Low resolution (1.5 mm) |
[18F]FDG | [125][131] | |
| Seahorse | Quantification of the oxygen consumption rate (OCR) and the extracellular acidification rate (ECAR) | +: • High sensitivity (from 5000 cells, theoretically), possibility to test many conditions in parallel −: • Difficulties in normalizing results, limited number of injections, limited sample thickness |
Not suitable | [132][133] | |
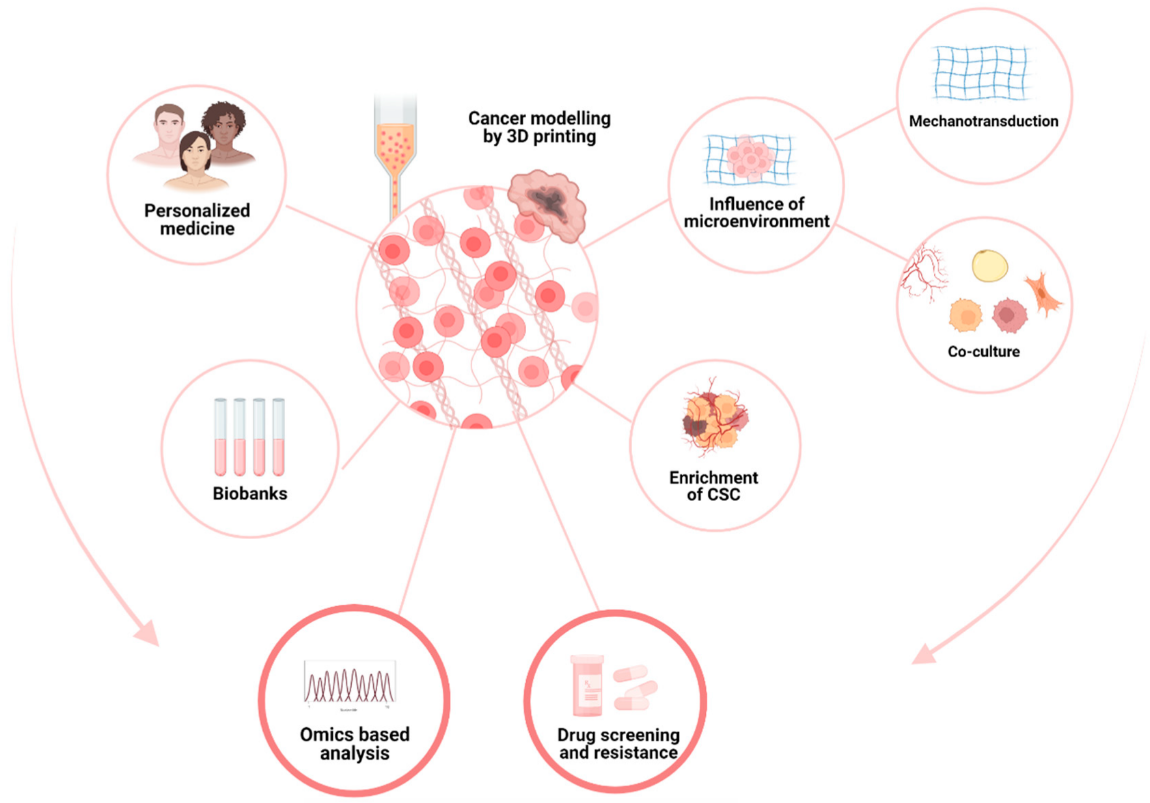
2.3. Recapitulate Cancer’s Relation to the Microenvironment
2.3.1. Cells–ECM Interaction
2.3.2. Neoangiogenesis
2.4. Mechanical Environment
2.4.1. Mechanotransduction
References
- Huang, S.H.; Liu, P.; Mokasdar, A.; Hou, L. Additive Manufacturing and Its Societal Impact: A Literature Review. Int. J. Adv. Manuf. Technol. 2013, 67, 1191–1203.
- Ho, C.M.B.; Ng, S.H.; Yoon, Y.-J. A Review on 3D Printed Bioimplants. Int. J. Precis. Eng. Man. 2015, 16, 1035–1046.
- Diment, L.E.; Thompson, M.S.; Bergmann, J.H.M. Clinical Efficacy and Effectiveness of 3D Printing: A Systematic Review. BMJ Open 2017, 7, e016891.
- Belhouideg, S. Impact of 3D Printed Medical Equipment on the Management of the Covid19 Pandemic. Int. J. Health Plan. Manag. 2020, 35, 1014–1022.
- Choong, Y.Y.C.; Tan, H.W.; Patel, D.C.; Choong, W.T.N.; Chen, C.-H.; Low, H.Y.; Tan, M.J.; Patel, C.D.; Chua, C.K. The Global Rise of 3D Printing during the COVID-19 Pandemic. Nat. Rev. Mater. 2020, 5, 637–639.
- Tino, R.; Moore, R.; Antoline, S.; Ravi, P.; Wake, N.; Ionita, C.N.; Morris, J.M.; Decker, S.J.; Sheikh, A.; Rybicki, F.J.; et al. COVID-19 and the Role of 3D Printing in Medicine. 3D Print. Med. 2020, 6, 11.
- Yan, Q.; Dong, H.; Su, J.; Han, J.; Song, B.; Wei, Q.; Shi, Y. A Review of 3D Printing Technology for Medical Applications. Engineering 2018, 4, 729–742.
- Nuseir, A.; Hatamleh, M.M.; Alnazzawi, A.; Al-Rabab’ah, M.; Kamel, B.; Jaradat, E. Direct 3D Printing of Flexible Nasal Prosthesis: Optimized Digital Workflow from Scan to Fit. J. Prosthodont. 2019, 28, 10–14.
- Faglin, P.; Gradwohl, M.; Depoortere, C.; Germain, N.; Drucbert, A.-S.; Brun, S.; Nahon, C.; Dekiouk, S.; Rech, A.; Azaroual, N.; et al. Rationale for the Design of 3D-Printable Bioresorbable Tissue-Engineering Chambers to Promote the Growth of Adipose Tissue. Sci. Rep. 2020, 10, 11779.
- Wang, X.; Ao, Q.; Tian, X.; Fan, J.; Wei, Y.; Hou, W.; Tong, H.; Bai, S. 3D Bioprinting Technologies for Hard Tissue and Organ Engineering. Materials 2016, 9, 802.
- Groll, J.; Burdick, J.A.; Cho, D.-W.; Derby, B.; Gelinsky, M.; Heilshorn, S.C.; Jüngst, T.; Malda, J.; Mironov, V.A.; Nakayama, K.; et al. A Definition of Bioinks and Their Distinction from Biomaterial Inks. Biofabrication 2018, 11, 013001.
- Murphy, S.V.; Coppi, P.D.; Atala, A. Opportunities and Challenges of Translational 3D Bioprinting. Nat. Biomed. Eng. 2020, 4, 370–380.
- Boland, T.; Mironov, V.; Gutowska, A.; Roth, E.A.; Markwald, R.R. Cell and Organ Printing 2: Fusion of Cell Aggregates in Three-dimensional Gels. Anat. Rec. Part A Discov. Mol. Cell. Evol. Biol. 2003, 272, 497–502.
- Ventura, R.D. An Overview of Laser-Assisted Bioprinting (LAB) in Tissue Engineering Applications. Med. Lasers 2021, 10, 76–81.
- Dou, C.; Perez, V.; Qu, J.; Tsin, A.; Xu, B.; Li, J. A State-of-the-Art Review of Laser-Assisted Bioprinting and Its Future Research Trends. ChemBioEng Rev. 2021, 8, 517–534.
- Li, X.; Liu, B.; Pei, B.; Chen, J.; Zhou, D.; Peng, J.; Zhang, X.; Jia, W.; Xu, T. Inkjet Bioprinting of Biomaterials. Chem. Rev. 2020, 120, 10596–10636.
- Kumar, P.; Ebbens, S.; Zhao, X. Inkjet Printing of Mammalian Cells—Theory and Applications. Bioprinting 2021, 23, e00157.
- Ramesh, S.; Zhang, Y.; Cormier, D.R.; Rivero, I.V.; Harrysson, O.L.A.; Rao, P.K.; Tamayol, A.; Tamayol, A. Extrusion Bioprinting: Recent Progress, Challenges, and Future Opportunities. Bioprinting 2020, 21, e00116.
- Zhang, Y.S.; Haghiashtiani, G.; Hübscher, T.; Kelly, D.J.; Lee, J.M.; Lutolf, M.; McAlpine, M.C.; Yeong, W.Y.; Zenobi-Wong, M.; Malda, J. 3D Extrusion Bioprinting. Nat. Rev. Methods Primers 2021, 1, 75.
- Cui, X.; Li, J.; Hartanto, Y.; Durham, M.; Tang, J.; Zhang, H.; Hooper, G.; Lim, K.; Woodfield, T. Advances in Extrusion 3D Bioprinting: A Focus on Multicomponent Hydrogel-Based Bioinks. Adv. Healthc. Mater. 2020, 9, 1901648.
- Zheng, Z.; Eglin, D.; Alini, M.; Richards, G.R.; Qin, L.; Lai, Y. Visible Light-Induced 3D Bioprinting Technologies and Corresponding Bioink Materials for Tissue Engineering: A Review. Engineering 2020, 7, 966–978.
- Kilian, D.; Ahlfeld, T.; Akkineni, A.R.; Lode, A.; Gelinsky, M. Three-Dimensional Bioprinting of Volumetric Tissues and Organs. Mrs. Bull. 2017, 42, 585–592.
- Wang, M.; Li, W.; Mille, L.S.; Ching, T.; Luo, Z.; Tang, G.; Garciamendez, C.E.; Lesha, A.; Hashimoto, M.; Zhang, Y.S. Digital Light Processing Based Bioprinting with Composable Gradients. Adv. Mater. 2022, 34, 2107038.
- Bernal, P.N.; Delrot, P.; Loterie, D.; Li, Y.; Malda, J.; Moser, C.; Levato, R. Volumetric Bioprinting of Complex Living-Tissue Constructs within Seconds. Adv. Mater. 2019, 31, e1904209.
- Li, J.; Parra-Cantu, C.; Wang, Z.; Zhang, Y.S. Improving Bioprinted Volumetric Tumor Microenvironments In Vitro. Trends Cancer 2020, 6, 745–756.
- Gudapati, H.; Dey, M.; Ozbolat, I. A Comprehensive Review on Droplet-Based Bioprinting: Past, Present and Future. Biomaterials 2016, 102, 20–42.
- Jentsch, S.; Nasehi, R.; Kuckelkorn, C.; Gundert, B.; Aveic, S.; Fischer, H. Multiscale 3D Bioprinting by Nozzle-Free Acoustic Droplet Ejection. Small Methods 2021, 5, 2000971.
- Ng, W.L.; Lee, J.M.; Yeong, W.Y.; Naing, M.W. Microvalve-Based Bioprinting—Process, Bio-Inks and Applications. Biomater. Sci. 2017, 5, 632–647.
- Costa, E.C.; Moreira, A.F.; de Melo-Diogo, D.; Gaspar, V.M.; Carvalho, M.P.; Correia, I.J. 3D Tumor Spheroids: An Overview on the Tools and Techniques Used for Their Analysis. Biotechnol. Adv. 2016, 34, 1427–1441.
- Pinto, B.; Henriques, A.C.; Silva, P.M.A.; Bousbaa, H. Three-Dimensional Spheroids as In Vitro Preclinical Models for Cancer Research. Pharmaceutics 2020, 12, 1186.
- Friedrich, J.; Seidel, C.; Ebner, R.; Kunz-Schughart, L.A. Spheroid-Based Drug Screen: Considerations and Practical Approach. Nat. Protoc. 2009, 4, 309–324.
- Zanoni, M.; Piccinini, F.; Arienti, C.; Zamagni, A.; Santi, S.; Polico, R.; Bevilacqua, A.; Tesei, A. 3D Tumor Spheroid Models for in Vitro Therapeutic Screening: A Systematic Approach to Enhance the Biological Relevance of Data Obtained. Sci. Rep. 2016, 6, 19103.
- Ma, H.; Jiang, Q.; Han, S.; Wu, Y.; Tomshine, J.C.; Wang, D.; Gan, Y.; Zou, G.; Liang, X.-J. Multicellular Tumor Spheroids as an in Vivo–Like Tumor Model for Three-Dimensional Imaging of Chemotherapeutic and Nano Material Cellular Penetration. Mol. Imaging 2012, 11, 7290.2012.00012.
- Longati, P.; Jia, X.; Eimer, J.; Wagman, A.; Witt, M.-R.; Rehnmark, S.; Verbeke, C.; Toftgård, R.; Löhr, M.; Heuchel, R.L. 3D Pancreatic Carcinoma Spheroids Induce a Matrix-Rich, Chemoresistant Phenotype Offering a Better Model for Drug Testing. BMC Cancer 2013, 13, 95.
- Loebsack, A.B.; Halberstadt, C.R.; Holder, W.D.; Culberson, C.R.; Beiler, R.J.; Greene, K.G.; Roland, W.D.; Burg, K.J.L. The Development of an Embedding Technique for Polylactide Sponges. J. Biomed. Mater. Res. 1999, 48, 504–510.
- Ruan, J.-L.; Tulloch, N.L.; Muskheli, V.; Genova, E.E.; Mariner, P.D.; Anseth, K.S.; Murry, C.E. An Improved Cryosection Method for Polyethylene Glycol Hydrogels Used in Tissue Engineering. Tissue Eng. Part C Methods 2013, 19, 794–801.
- James, R.; Jenkins, L.; Ellis, S.E.; Burg, K.J.L. Histological Processing of Hydrogel Scaffolds for Tissue-Engineering Applications. J. Histotechnol. 2004, 27, 133–139.
- Béduer, A.; Piacentini, N.; Aeberli, L.; Silva, A.D.; Verheyen, C.A.; Bonini, F.; Rochat, A.; Filippova, A.; Serex, L.; Renaud, P.; et al. Additive Manufacturing of Hierarchical Injectable Scaffolds for Tissue Engineering. Acta Biomater. 2018, 76, 71–79.
- Huisken, J.; Swoger, J.; Bene, F.D.; Wittbrodt, J.; Stelzer, E.H.K. Optical Sectioning Deep Inside Live Embryos by Selective Plane Illumination Microscopy. Science 2004, 305, 1007–1009.
- Schneckenburger, H.; Weber, P.; Wagner, M.; Schickinger, S.; Richter, V.; Bruns, T.; Strauss, W.S.l.; Wittig, R. Light Exposure and Cell Viability in Fluorescence Microscopy. J. Microsc. 2012, 245, 311–318.
- Smyrek, I.; Stelzer, E.H.K. Quantitative Three-Dimensional Evaluation of Immunofluorescence Staining for Large Whole Mount Spheroids with Light Sheet Microscopy. Biomed. Opt. Express 2017, 8, 484–499.
- Lazzari, G.; Vinciguerra, D.; Balasso, A.; Nicolas, V.; Goudin, N.; Garfa-Traore, M.; Fehér, A.; Dinnyés, A.; Nicolas, J.; Couvreur, P.; et al. Light Sheet Fluorescence Microscopy versus Confocal Microscopy: In Quest of a Suitable Tool to Assess Drug and Nanomedicine Penetration into Multicellular Tumor Spheroids. Eur. J. Pharm. Biopharm. 2019, 142, 195–203.
- Yu, F.; Han, X.; Zhang, K.; Dai, B.; Shen, S.; Gao, X.; Teng, H.; Wang, X.; Li, L.; Ju, H.; et al. Evaluation of a Polyvinyl Alcohol-Alginate Based Hydrogel for Precise 3D Bioprinting. J. Biomed. Mater. Res. A 2018, 106, 2944–2954.
- Li, X.; Chen, S.; Li, J.; Wang, X.; Zhang, J.; Kawazoe, N.; Chen, G. 3D Culture of Chondrocytes in Gelatin Hydrogels with Different Stiffness. Polymers 2016, 8, 269.
- Cambria, E.; Brunner, S.; Heusser, S.; Fisch, P.; Hitzl, W.; Ferguson, S.J.; Wuertz-Kozak, K. Cell-Laden Agarose-Collagen Composite Hydrogels for Mechanotransduction Studies. Front. Bioeng. Biotechnol. 2020, 8, 346.
- Axpe, E.; Oyen, M.L. Applications of Alginate-Based Bioinks in 3D Bioprinting. Int. J. Mol. Sci. 2016, 17, 1976.
- Schmid, R.; Schmidt, S.K.; Hazur, J.; Detsch, R.; Maurer, E.; Boccaccini, A.R.; Hauptstein, J.; Teßmar, J.; Blunk, T.; Schrüfer, S.; et al. Comparison of Hydrogels for the Development of Well-Defined 3D Cancer Models of Breast Cancer and Melanoma. Cancers 2020, 12, 2320.
- Qiao, S.; Zhao, Y.; Li, C.; Yin, Y.; Meng, Q.; Lin, F.-H.; Liu, Y.; Hou, X.; Guo, K.; Chen, X.; et al. An Alginate-Based Platform for Cancer Stem Cell Research. Acta Biomater. 2016, 37, 83–92.
- Piras, C.C.; Smith, D.K. Multicomponent Polysaccharide Alginate-Based Bioinks. J. Mater. Chem. B 2020, 8, 8171–8188.
- Jiang, T.; Munguia-Lopez, J.G.; Gu, K.; Bavoux, M.M.; Flores-Torres, S.; Kort-Mascort, J.; Grant, J.; Vijayakumar, S.; Leon-Rodriguez, A.D.; Ehrlicher, A.J.; et al. Engineering Bioprintable Alginate/Gelatin Composite Hydrogels with Tunable Mechanical and Cell Adhesive Properties to Modulate Tumor Spheroid Growth Kinetics. Biofabrication 2020, 12, 015024.
- Reig-Vano, B.; Tylkowski, B.; Montané, X.; Giamberini, M. Alginate-Based Hydrogels for Cancer Therapy and Research. Int. J. Biol. Macromol. 2020, 170, 424–436.
- Abasalizadeh, F.; Moghaddam, S.V.; Alizadeh, E.; akbari, E.; Kashani, E.; Fazljou, S.M.B.; Torbati, M.; Akbarzadeh, A. Alginate-Based Hydrogels as Drug Delivery Vehicles in Cancer Treatment and Their Applications in Wound Dressing and 3D Bioprinting. J. Biol. Eng. 2020, 14, 8.
- Ying, G.; Jiang, N.; Yu, C.; Zhang, Y.S. Three-Dimensional Bioprinting of Gelatin Methacryloyl (GelMA). Bio-Des. Manuf. 2018, 1, 215–224.
- He, H.; Li, D.; Lin, Z.; Peng, L.; Yang, J.; Wu, M.; Cheng, D.; Pan, H.; Ruan, C. Temperature-Programmable and Enzymatically Solidifiable Gelatin-Based Bioinks Enable Facile Extrusion Bioprinting. Biofabrication 2020, 12, 045003.
- Rajabi, N.; Rezaei, A.; Kharaziha, M.; Bakhsheshi-Rad, H.R.; Luo, H.; RamaKrishna, S.; Berto, F. Recent Advances on Bioprinted Gelatin Methacrylate-Based Hydrogels for Tissue Repair. Tissue Eng. Part A 2021, 27, 679–702.
- Yue, K.; Santiago, G.T.; Alvarez, M.M.; Tamayol, A.; Annabi, N.; Khademhosseini, A. Synthesis, Properties, and Biomedical Applications of Gelatin Methacryloyl (GelMA) Hydrogels. Biomaterials 2015, 73, 254–271.
- Mao, S.; He, J.; Zhao, Y.; Liu, T.; Xie, F.; Yang, H.; Mao, Y.; Pang, Y.; Sun, W. Bioprinting of Patient-Derived in Vitro Intrahepatic Cholangiocarcinoma Tumor Model: Establishment, Evaluation and Anti-Cancer Drug Testing. Biofabrication 2020, 12, 045014.
- Miranda, M.A.; Marcato, P.D.; Mondal, A.; Chowdhury, N.; Gebeyehu, A.; Surapaneni, S.K.; Bentley, M.V.L.B.; Amaral, R.; Pan, C.-X.; Singh, M. Cytotoxic and Chemosensitizing Effects of Glycoalkaloidic Extract on 2D and 3D Models Using RT4 and Patient Derived Xenografts Bladder Cancer Cells. Mater. Sci. Eng. C 2021, 119, 111460.
- Piras, C.C.; Fernández-Prieto, S.; Borggraeve, W.M.D. Nanocellulosic Materials as Bioinks for 3D Bioprinting. Biomater. Sci. 2017, 5, 1988–1992.
- Wang, X.; Wang, Q.; Xu, C. Nanocellulose-Based Inks for 3D Bioprinting: Key Aspects in Research Development and Challenging Perspectives in Applications—A Mini Review. Bioengineering 2020, 7, 40.
- Kim, J.; Jang, J.; Cho, D.-W. Controlling Cancer Cell Behavior by Improving the Stiffness of Gastric Tissue-Decellularized ECM Bioink With Cellulose Nanoparticles. Front. Bioeng. Biotechnol. 2021, 9, 605819.
- Gospodinova, A.; Nankov, V.; Tomov, S.; Redzheb, M.; Petrov, P.D. Extrusion Bioprinting of Hydroxyethylcellulose-Based Bioink for Cervical Tumor Model. Carbohyd. Polym. 2021, 260, 117793.
- Olmos-Juste, R.; Alonso-Lerma, B.; Pérez-Jiménez, R.; Gabilondo, N.; Eceiza, A. 3D Printed Alginate-Cellulose Nanofibers Based Patches for Local Curcumin Administration. Carbohyd. Polym. 2021, 264, 118026.
- Stefano, P.D.; Briatico-Vangosa, F.; Bianchi, E.; Pellegata, A.F.; de Hartungen, A.H.; Corti, P.; Dubini, G. Bioprinting of Matrigel Scaffolds for Cancer Research. Polymers 2021, 13, 2026.
- Fan, R.; Piou, M.; Darling, E.; Cormier, D.; Sun, J.; Wan, J. Bio-Printing Cell-Laden Matrigel–Agarose Constructs. J. Biomater. Appl. 2016, 31, 684–692.
- Snyder, J.E.; Hamid, Q.; Wang, C.; Chang, R.; Emami, K.; Wu, H.; Sun, W. Bioprinting Cell-Laden Matrigel for Radioprotection Study of Liver by pro-Drug Conversion in a Dual-Tissue Microfluidic Chip. Biofabrication 2011, 3, 034112.
- Horváth, L.; Umehara, Y.; Jud, C.; Blank, F.; Petri-Fink, A.; Rothen-Rutishauser, B. Engineering an in Vitro Air-Blood Barrier by 3D Bioprinting. Sci. Rep. 2015, 5, 7974.
- Benton, G.; Kleinman, H.K.; George, J.; Arnaoutova, I. Multiple Uses of Basement Membrane-like Matrix (BME/Matrigel) in Vitro and in Vivo with Cancer Cells. Int. J. Cancer 2011, 128, 1751–1757.
- Osidak, E.O.; Kozhukhov, V.I.; Osidak, M.S.; Domogatsky, S.P. Collagen as Bioink for Bioprinting: A Comprehensive Review. Int. J. Bioprint. 2020, 6, 270.
- Swaminathan, S.; Hamid, Q.; Sun, W.; Clyne, A.M. Bioprinting of 3D Breast Epithelial Spheroids for Human Cancer Models. Biofabrication 2019, 11, 025003.
- Marques, C.F.; Diogo, G.S.; Pina, S.; Oliveira, J.M.; Silva, T.H.; Reis, R.L. Collagen-Based Bioinks for Hard Tissue Engineering Applications: A Comprehensive Review. J. Mater. Sci. Mater. Med. 2019, 30, 32.
- Campos, D.F.D.; Marquez, A.B.; O’Seanain, C.; Fischer, H.; Blaeser, A.; Vogt, M.; Corallo, D.; Aveic, S. Exploring Cancer Cell Behavior In Vitro in Three-Dimensional Multicellular Bioprintable Collagen-Based Hydrogels. Cancers 2019, 11, 180.
- Noh, I.; Kim, N.; Tran, H.N.; Lee, J.; Lee, C. 3D Printable Hyaluronic Acid-Based Hydrogel for Its Potential Application as a Bioink in Tissue Engineering. Biomater. Res. 2019, 23, 3.
- Schmid, R.; Schmidt, S.K.; Detsch, R.; Horder, H.; Blunk, T.; Schrüfer, S.; Schubert, D.W.; Fischer, L.; Thievessen, I.; Heltmann-Meyer, S.; et al. A New Printable Alginate/Hyaluronic Acid/Gelatin Hydrogel Suitable for Biofabrication of In Vitro and In Vivo Metastatic Melanoma Models. Adv. Funct. Mater. 2021, 32, 2107993.
- Petta, D.; DAmora, U.; Ambrosio, L.; Grijpma, D.W.; Eglin, D.; DEste, M. Hyaluronic Acid as a Bioink for Extrusion-Based 3D Printing. Biofabrication 2020, 12, 032001.
- Horder, H.; Lasheras, M.G.; Grummel, N.; Nadernezhad, A.; Herbig, J.; Ergün, S.; Teßmar, J.; Groll, J.; Fabry, B.; Bauer-Kreisel, P.; et al. Bioprinting and Differentiation of Adipose-Derived Stromal Cell Spheroids for a 3D Breast Cancer-Adipose Tissue Model. Cells 2021, 10, 803.
- Lόpez-Marcial, G.R.; Zeng, A.Y.; Osuna, C.; Dennis, J.; García, J.M.; O’Connell, G.D. Agarose-Based Hydrogels as Suitable Bioprinting Materials for Tissue Engineering. ACS Biomater. Sci. Eng. 2018, 4, 3610–3616.
- Kim, J.E.; Kim, S.H.; Jung, Y. Current Status of Three-Dimensional Printing Inks for Soft Tissue Regeneration. Tissue Eng. Regen. Med. 2016, 13, 636–646.
- Abelseth, E.; Abelseth, L.; la Vega, L.D.; Beyer, S.T.; Wadsworth, S.J.; Willerth, S.M. 3D Printing of Neural Tissues Derived from Human Induced Pluripotent Stem Cells Using a Fibrin-Based Bioink. ACS Biomater. Sci. Eng. 2019, 5, 234–243.
- Lee, C.; Abelseth, E.; de la Vega, L.; Willerth, S.M. Bioprinting a Novel Glioblastoma Tumor Model Using a Fibrin-Based Bioink for Drug Screening. Mater. Today Chem. 2019, 12, 78–84.
- Sharma, R.; Smits, I.P.M.; Vega, L.D.L.; Lee, C.; Willerth, S.M. 3D Bioprinting Pluripotent Stem Cell Derived Neural Tissues Using a Novel Fibrin Bioink Containing Drug Releasing Microspheres. Front. Bioeng. Biotechnol. 2020, 8, 57.
- Chawla, S.; Midha, S.; Sharma, A.; Ghosh, S. Silk-Based Bioinks for 3D Bioprinting. Adv. Healthc. Mater. 2018, 7, 1701204.
- Gangrade, A.; Mandal, B.B. Drug Delivery of Anticancer Drugs from Injectable 3D Porous Silk Scaffold for Prevention of Gastric Cancer Growth and Recurrence. ACS Biomater. Sci. Eng. 2020, 6, 6195–6206.
- Qian, K.-Y.; Song, Y.; Yan, X.; Dong, L.; Xue, J.; Xu, Y.; Wang, B.; Cao, B.; Hou, Q.; Peng, W.; et al. Injectable Ferrimagnetic Silk Fibroin Hydrogel for Magnetic Hyperthermia Ablation of Deep Tumor. Biomaterials 2020, 259, 120299.
- Wang, Q.; Han, G.; Yan, S.; Zhang, Q. 3D Printing of Silk Fibroin for Biomedical Applications. Materials 2019, 12, 504.
- Pitarresi, G.; Martorana, A.; Palumbo, F.S.; Fiorica, C.; Giammona, G. New Gellan Gum-Graft-Poly(d,l-Lactide-co-Glycolide) Copolymers as Promising Bioinks: Synthesis and Characterization. Int. J. Biol. Macromol. 2020, 162, 1653–1667.
- Zhu, S.; Yao, L.; Pan, C.; Tian, J.; Li, L.; Luo, B.; Zhou, C.; Lu, L. 3D Printed Gellan Gum/Graphene Oxide Scaffold for Tumor Therapy and Bone Reconstruction. Compos. Sci. Technol. 2021, 208, 108763.
- Lozano, R.; Stevens, L.; Thompson, B.C.; Gilmore, K.J.; Gorkin, R.; Stewart, E.M.; in het Panhuis, M.; Romero-Ortega, M.; Wallace, G.G. 3D Printing of Layered Brain-like Structures Using Peptide Modified Gellan Gum Substrates. Biomaterials 2015, 67, 264–273.
- Tonda-Turo, C.; Carmagnola, I.; Chiappone, A.; Feng, Z.; Ciardelli, G.; Hakkarainen, M.; Sangermano, M. Photocurable Chitosan as Bioink for Cellularized Therapies towards Personalized Scaffold Architecture. Bioprinting 2020, 18, e00082.
- Babu, A.; Ramesh, R. Multifaceted Applications of Chitosan in Cancer Drug Delivery and Therapy. Mar. Drugs 2017, 15, 96.
- Sahranavard, M.; Zamanian, A.; Ghorbani, F.; Shahrezaee, M.H. A Critical Review on Three Dimensional-Printed Chitosan Hydrogels for Development of Tissue Engineering. Bioprinting 2020, 17, e00063.
- Roth, A.D.; Lama, P.; Dunn, S.; Hong, S.; Lee, M.-Y. Polymer Coating on a Micropillar Chip for Robust Attachment of PuraMatrix Peptide Hydrogel for 3D Hepatic Cell Culture. Mater. Sci. Eng. C Mater. Biol. Appl. 2018, 90, 634–644.
- Yang, Z.; Xu, H.; Zhao, X. Designer Self-Assembling Peptide Hydrogels to Engineer 3D Cell Microenvironments for Cell Constructs Formation and Precise Oncology Remodeling in Ovarian Cancer. Adv. Sci. 2020, 7, 1903718.
- Pati, F.; Jang, J.; Ha, D.-H.; Kim, S.W.; Rhie, J.-W.; Shim, J.-H.; Kim, D.-H.; Cho, D.-W. Printing Three-Dimensional Tissue Analogues with Decellularized Extracellular Matrix Bioink. Nat. Commun. 2014, 5, 3935.
- Ferreira, L.P.; Gaspar, V.M.; Mano, J.F. Decellularized Extracellular Matrix for Bioengineering Physiomimetic 3D in Vitro Tumor Models. Trends Biotechnol. 2020, 38, 1397–1414.
- Jang, J.; Park, H.-J.; Kim, S.-W.; Kim, H.; Park, J.Y.; Na, S.J.; Kim, H.J.; Park, M.N.; Choi, S.H.; Park, S.H.; et al. 3D Printed Complex Tissue Construct Using Stem Cell-Laden Decellularized Extracellular Matrix Bioinks for Cardiac Repair. Biomaterials 2017, 112, 264–274.
- Hwang, J.; San, B.H.; Turner, N.J.; White, L.J.; Faulk, D.M.; Badylak, S.F.; Li, Y.; Yu, S.M. Molecular Assessment of Collagen Denaturation in Decellularized Tissues Using a Collagen Hybridizing Peptide. Acta Biomater. 2017, 53, 268–278.
- He, Y.; Wang, F.; Wang, X.; Zhang, J.; Wang, D.; Huang, X. A Photocurable Hybrid Chitosan/Acrylamide Bioink for DLP Based 3D Bioprinting. Mater. Des. 2021, 202, 109588.
- Poellmann, M.J.; Johnson, A.J.W. Multimaterial Polyacrylamide: Fabrication with Electrohydrodynamic Jet Printing, Applications, and Modeling. Biofabrication 2014, 6, 035018.
- Poh, P.S.P.; Hutmacher, D.W.; Stevens, M.M.; Woodruff, M.A. Fabrication and in Vitro Characterization of Bioactive Glass Composite Scaffolds for Bone Regeneration. Biofabrication 2013, 5, 045005.
- Kundu, J.; Shim, J.-H.; Jang, J.; Kim, S.-W.; Cho, D.-W. An Additive Manufacturing-Based PCL-Alginate-Chondrocyte Bioprinted Scaffold for Cartilage Tissue Engineering. J. Tissue Eng. Regen. Med. 2013, 9, 1286–1297.
- Zamani, Y.; Mohammadi, J.; Amoabediny, G.; Helder, M.N.; Zandieh-Doulabi, B.; Klein-Nulend, J. Bioprinting of Alginate-Encapsulated Pre-Osteoblasts in PLGA/β-TCP Scaffolds Enhances Cell Retention but Impairs Osteogenic Differentiation Compared to Cell Seeding after 3D-Printing. Regen. Eng. Transl. Med. 2021, 7, 485–493.
- Abelardo, E. 3D Bioprinting for Reconstructive Surgery; Woodhead Publishing Series in Biomaterials; Elsevier: Amsterdam, The Netherlands, 2018; pp. 137–144.
- Zhu, J. Bioactive Modification of Poly(Ethylene Glycol) Hydrogels for Tissue Engineering. Biomaterials 2010, 31, 4639–4656.
- Hong, S.; Sycks, D.; Chan, H.F.; Lin, S.; Lopez, G.P.; Guilak, F.; Leong, K.W.; Zhao, X. 3D Printing of Highly Stretchable and Tough Hydrogels into Complex, Cellularized Structures. Adv. Mater. 2015, 27, 4035–4040.
- Müller, M.; Becher, J.; Schnabelrauch, M.; Zenobi-Wong, M. Nanostructured Pluronic Hydrogels as Bioinks for 3D Bioprinting. Biofabrication 2015, 7, 035006.
- Gioffredi, E.; Boffito, M.; Calzone, S.; Giannitelli, S.M.; Rainer, A.; Trombetta, M.; Mozetic, P.; Chiono, V. Pluronic F127 Hydrogel Characterization and Biofabrication in Cellularized Constructs for Tissue Engineering Applications. Proc. Cirp. 2016, 49, 125–132.
- Hsieh, F.-Y.; Lin, H.-H.; Hsu, S. 3D Bioprinting of Neural Stem Cell-Laden Thermoresponsive Biodegradable Polyurethane Hydrogel and Potential in Central Nervous System Repair. Biomaterials 2015, 71, 48–57.
- Hung, K.; Tseng, C.; Hsu, S. Synthesis and 3D Printing of Biodegradable Polyurethane Elastomer by a Water-Based Process for Cartilage Tissue Engineering Applications. Adv. Healthc. Mater. 2014, 3, 1578–1587.
- Norberg, K.J.; Liu, X.; Moro, C.F.; Strell, C.; Nania, S.; Blümel, M.; Balboni, A.; Bozóky, B.; Heuchel, R.L.; Löhr, J.M. A Novel Pancreatic Tumour and Stellate Cell 3D Co-Culture Spheroid Model. BMC Cancer 2020, 20, 475.
- Ewa-Choy, Y.W.; Pingguan-Murphy, B.; Abdul-Ghani, N.A.; Jahendran, J.; Chua, K.H. Effect of Alginate Concentration on Chondrogenesis of Co-Cultured Human Adipose-Derived Stem Cells and Nasal Chondrocytes: A Biological Study. Biomater. Res. 2017, 21, 19.
- Li, X.; Chen, Y.; Kawazoe, N.; Chen, G. Influence of Microporous Gelatin Hydrogels on Chondrocyte Functions. J. Mater. Chem. B 2017, 5, 5753–5762.
- Meinert, C.; Schrobback, K.; Hutmacher, D.W.; Klein, T.J. A Novel Bioreactor System for Biaxial Mechanical Loading Enhances the Properties of Tissue-Engineered Human Cartilage. Sci. Rep. 2017, 7, 16997.
- Park, H.; Temenoff, J.S.; Tabata, Y.; Caplan, A.I.; Mikos, A.G. Injectable Biodegradable Hydrogel Composites for Rabbit Marrow Mesenchymal Stem Cell and Growth Factor Delivery for Cartilage Tissue Engineering. Biomaterials 2007, 28, 3217–3227.
- Haugh, M.G.; Meyer, E.G.; Thorpe, S.D.; Vinardell, T.; Duffy, G.P.; Kelly, D.J. Temporal and Spatial Changes in Cartilage-Matrix-Specific Gene Expression in Mesenchymal Stem Cells in Response to Dynamic Compression. Tissue Eng. Part A 2011, 17, 3085–3093.
- Gauch, S.; Hermann, R.; Feuser, P.; Oelmüller, U.; Bastian, H. Isolation of Total RNA Using Silica-Gel Based Membranes. In Molecular Tools for Screening Biodiversity: Plants and Animals; Karp, I.A., Ingram, P.G., David, S., Eds.; Springer: Dordrecht, The Netherlands, 1998; pp. 67–70.
- Köster, N.; Schmiermund, A.; Grubelnig, S.; Leber, J.; Ehlicke, F.; Czermak, P.; Salzig, D. Single-Step RNA Extraction from Different Hydrogel-Embedded Mesenchymal Stem Cells for Quantitative Reverse Transcription–Polymerase Chain Reaction Analysis. Tissue Eng. Part C Methods 2016, 22, 552–560.
- Bougault, C.; Paumier, A.; Aubert-Foucher, E.; Mallein-Gerin, F. Investigating Conversion of Mechanical Force into Biochemical Signaling in Three-Dimensional Chondrocyte Cultures. Nat. Protoc. 2009, 4, 928–938.
- Sbrana, F.V.; Pinos, R.; Barbaglio, F.; Ribezzi, D.; Scagnoli, F.; Scarfò, L.; Redwan, I.N.; Martinez, H.; Farè, S.; Ghia, P.; et al. 3D Bioprinting Allows the Establishment of Long-Term 3D Culture Model for Chronic Lymphocytic Leukemia Cells. Front. Immunol. 2021, 12, 639572.
- Shin, D.-S.; You, J.; Rahimian, A.; Vu, T.; Siltanen, C.; Ehsanipour, A.; Stybayeva, G.; Sutcliffe, J.; Revzin, A. Photodegradable Hydrogels for Capture, Detection, and Release of Live Cells. Angew. Chem. Int. Ed. 2014, 53, 8221–8224.
- Friedrich, J.; Eder, W.; Castaneda, J.; Doss, M.; Huber, E.; Ebner, R.; Kunz-Schughart, L.A. A Reliable Tool to Determine Cell Viability in Complex 3-D Culture: The Acid Phosphatase Assay. J. Biomol. Screen. 2007, 12, 925–937.
- Beaumont, K.A.; Anfosso, A.; Ahmed, F.; Weninger, W.; Haass, N.K. Imaging- and Flow Cytometry-Based Analysis of Cell Position and the Cell Cycle in 3D Melanoma Spheroids. J. Vis. Exp. 2015, 106, 53486.
- Geng, Z.; Zhang, H.; Xiong, Q.; Zhang, Y.; Zhao, H.; Wang, G. A Fluorescent Chitosan Hydrogel Detection Platform for the Sensitive and Selective Determination of Trace Mercury(II) in Water. J. Mater. Chem. A 2015, 3, 19455–19460.
- Khattak, S.F.; Spatara, M.; Roberts, L.; Roberts, S.C. Application of Colorimetric Assays to Assess Viability, Growth and Metabolism of Hydrogel-Encapsulated Cells. Biotechnol. Lett. 2006, 28, 1361–1370.
- Polley, C.; Mau, R.; Lieberwirth, C.; Stenzel, J.; Vollmar, B.; Seitz, H. Bioprinting of Three Dimensional Tumor Models: A Preliminary Study Using a Low Cost 3D Printer. Curr. Dir. Biomed. Eng. 2017, 3, 135–138.
- Ho, W.Y.; Yeap, S.K.; Ho, C.L.; Rahim, R.A.; Alitheen, N.B. Development of Multicellular Tumor Spheroid (MCTS) Culture from Breast Cancer Cell and a High Throughput Screening Method Using the MTT Assay. PLoS ONE 2012, 7, e44640.
- Hunnewell, M.; Forbes, N.S. Active and Inactive Metabolic Pathways in Tumor Spheroids: Determination by GC-MS. Biotechnol. Prog. 2010, 26, 789–796.
- Klapa, M.I.; Aon, J.-C.; Stephanopoulos, G. Ion-Trap Mass Spectrometry Used in Combination with Gas Chromatography for High-Resolution Metabolic Flux Determination. Biotechniques 2003, 34, 832–849.
- Forbes, N.S.; Meadows, A.L.; Clark, D.S.; Blanch, H.W. Estradiol Stimulates the Biosynthetic Pathways of Breast Cancer Cells: Detection by Metabolic Flux Analysis. Metab. Eng. 2006, 8, 639–652.
- Kim, B.; Forbes, N.S. Flux Analysis Shows That Hypoxia-Inducible-Factor-1-Alpha Minimally Affects Intracellular Metabolism in Tumor Spheroids. Biotechnol. Bioeng. 2007, 96, 1167–1182.
- Tondera, C.; Hauser, S.; Krüger-Genge, A.; Jung, F.; Neffe, A.T.; Lendlein, A.; Klopfleisch, R.; Steinbach, J.; Neuber, C.; Pietzsch, J. Gelatin-Based Hydrogel Degradation and Tissue Interaction in Vivo: Insights from Multimodal Preclinical Imaging in Immunocompetent Nude Mice. Theranostics 2016, 6, 2114–2128.
- Noel, P.; Muñoz, R.; Rogers, G.W.; Neilson, A.; Hoff, D.D.V.; Han, H. Preparation and Metabolic Assay of 3-Dimensional Spheroid Co-Cultures of Pancreatic Cancer Cells and Fibroblasts. J. Vis. Exp. Jove. 2017, 126, e56081.
- Marchetti, P.; Fovez, Q.; Germain, N.; Khamari, R.; Kluza, J. Mitochondrial Spare Respiratory Capacity: Mechanisms, Regulation, and Significance in Non-Transformed and Cancer Cells. FASEB J. 2020, 34, 13106–13124.
- Muir, A.; Danai, L.V.; Heiden, M.G.V. Microenvironmental Regulation of Cancer Cell Metabolism: Implications for Experimental Design and Translational Studies. Dis. Model. Mech. 2018, 11, dmm035758.
- Mueller, M.M.; Fusenig, N.E. Friends or Foes—Bipolar Effects of the Tumour Stroma in Cancer. Nat. Rev. Cancer 2004, 4, 839–849.
- Hanahan, D.; Coussens, L.M. Accessories to the Crime: Functions of Cells Recruited to the Tumor Microenvironment. Cancer Cell 2012, 21, 309–322.
- Duong, M.N.; Geneste, A.; Fallone, F.; Li, X.; Dumontet, C.; Muller, C. The Fat and the Bad: Mature Adipocytes, Key Actors in Tumor Progression and Resistance. Oncotarget 2017, 8, 57622–57641.
- Germain, N.; Dhayer, M.; Boileau, M.; Fovez, Q.; Kluza, J.; Marchetti, P. Lipid Metabolism and Resistance to Anticancer Treatment. Biology 2020, 9, 474.
- Zhao, C.; Wu, M.; Zeng, N.; Xiong, M.; Hu, W.; Lv, W.; Yi, Y.; Zhang, Q.; Wu, Y. Cancer-Associated Adipocytes: Emerging Supporters in Breast Cancer. J. Exp. Clin. Cancer Res. 2020, 39, 156.
- Sahai, E.; Astsaturov, I.; Cukierman, E.; DeNardo, D.G.; Egeblad, M.; Evans, R.M.; Fearon, D.; Greten, F.R.; Hingorani, S.R.; Hunter, T.; et al. A Framework for Advancing Our Understanding of Cancer-Associated Fibroblasts. Nat. Rev. Cancer 2020, 20, 174–186.
- Fiori, M.E.; Franco, S.D.; Villanova, L.; Bianca, P.; Stassi, G.; Maria, R.D. Cancer-Associated Fibroblasts as Abettors of Tumor Progression at the Crossroads of EMT and Therapy Resistance. Mol. Cancer 2019, 18, 70.
- Hanley, C.J.; Thomas, G.J. T-Cell Tumour Exclusion and Immunotherapy Resistance: A Role for CAF Targeting. Br. J. Cancer 2020, 123, 1353–1355.
- Mondal, A.; Gebeyehu, A.; Miranda, M.; Bahadur, D.; Patel, N.; Ramakrishnan, S.; Rishi, A.K.; Singh, M. Characterization and Printability of Sodium Alginate -Gelatin Hydrogel for Bioprinting NSCLC Co-Culture. Sci Rep. 2019, 9, 19914.
- Datta, P.; Dey, M.; Ataie, Z.; Unutmaz, D.; Ozbolat, I.T. 3D Bioprinting for Reconstituting the Cancer Microenvironment. NPJ Precis. Oncol. 2020, 4, 18.
- Luo, Y.; Wei, X.; Huang, P. 3D Bioprinting of Hydrogel-based Biomimetic Microenvironments. J. Biomed. Mater. Res. Part B Appl. Biomater. 2019, 107, 1695–1705.
- Samadian, H.; Jafari, S.; Sepand, M.R.; Alaei, L.; Malvajerd, S.S.; Jaymand, M.; Ghobadinezhad, F.; Jahanshahi, F.; Hamblin, M.R.; Derakhshankhah, H.; et al. 3D Bioprinting Technology to Mimic the Tumor Microenvironment: Tumor-on-a-Chip Concept. Mater. Today Adv. 2021, 12, 100160.
- Albritton, J.L.; Miller, J.S. 3D Bioprinting: Improving in Vitro Models of Metastasis with Heterogeneous Tumor Microenvironments. Dis. Model. Mech. 2017, 10, 3–14.
- Richards, D.; Jia, J.; Yost, M.; Markwald, R.; Mei, Y. 3D Bioprinting for Vascularized Tissue Fabrication. Ann. Biomed. Eng. 2017, 45, 132–147.
- Rajabi, M.; Mousa, S.A. The Role of Angiogenesis in Cancer Treatment. Biomedicines 2017, 5, 34.
- Liao, D.; Johnson, R.S. Hypoxia: A Key Regulator of Angiogenesis in Cancer. Cancer Metast. Rev. 2007, 26, 281–290.
- Zervantonakis, I.K.; Hughes-Alford, S.K.; Charest, J.L.; Condeelis, J.S.; Gertler, F.B.; Kamm, R.D. Three-Dimensional Microfluidic Model for Tumor Cell Intravasation and Endothelial Barrier Function. Proc. Natl. Acad. Sci. USA 2012, 109, 13515–13520.
- Meng, F.; Meyer, C.M.; Joung, D.; Vallera, D.A.; McAlpine, M.C.; Panoskaltsis-Mortari, A. 3D Bioprinted In Vitro Metastatic Models via Reconstruction of Tumor Microenvironments. Adv. Mater. 2019, 31, 1806899.
- Chen, C.S. Mechanotransduction—a Field Pulling Together? J. Cell Sci. 2008, 121, 3285–3292.
- Kulangara, K.; Leong, K.W. Substrate Topography Shapes Cell Function. Soft Matter 2009, 5, 4072–4076.
- Ghibaudo, M.; Saez, A.; Trichet, L.; Xayaphoummine, A.; Browaeys, J.; Silberzan, P.; Buguin, A.; Ladoux, B. Traction Forces and Rigidity Sensing Regulate Cell Functions. Soft Matter 2008, 4, 1836–1843.
- Orr, A.W.; Helmke, B.P.; Blackman, B.R.; Schwartz, M.A. Mechanisms of Mechanotransduction. Dev. Cell 2006, 10, 11–20.
- Geiger, B.; Spatz, J.P.; Bershadsky, A.D. Environmental Sensing through Focal Adhesions. Nat. Rev. Mol. Cell Biol. 2009, 10, 21–33.
- Baumgart, F. Stiffness—an Unknown World of Mechanical Science? Injury 2000, 31, 14–84.
- Theocharis, A.D.; Skandalis, S.S.; Gialeli, C.; Karamanos, N.K. Extracellular Matrix Structure. Adv. Drug Deliv. Rev. 2016, 97, 4–27.
- Ge, H.; Tian, M.; Pei, Q.; Tan, F.; Pei, H. Extracellular Matrix Stiffness: New Areas Affecting Cell Metabolism. Front. Oncol. 2021, 11, 631991.
- Strickaert, A.; Saiselet, M.; Dom, G.; Deken, X.D.; Dumont, J.E.; Feron, O.; Sonveaux, P.; Maenhaut, C. Cancer Heterogeneity Is Not Compatible with One Unique Cancer Cell Metabolic Map. Oncogene 2017, 36, 2637–2642.




