Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Sandro Rossi | + 4753 word(s) | 4753 | 2022-03-01 03:34:10 | | | |
| 2 | Bruce Ren | -76 word(s) | 4677 | 2022-03-07 02:28:10 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Rossi, S. Hadron Therapy Achievements and Challenges. Encyclopedia. Available online: https://encyclopedia.pub/entry/20200 (accessed on 07 February 2026).
Rossi S. Hadron Therapy Achievements and Challenges. Encyclopedia. Available at: https://encyclopedia.pub/entry/20200. Accessed February 07, 2026.
Rossi, Sandro. "Hadron Therapy Achievements and Challenges" Encyclopedia, https://encyclopedia.pub/entry/20200 (accessed February 07, 2026).
Rossi, S. (2022, March 04). Hadron Therapy Achievements and Challenges. In Encyclopedia. https://encyclopedia.pub/entry/20200
Rossi, Sandro. "Hadron Therapy Achievements and Challenges." Encyclopedia. Web. 04 March, 2022.
Copy Citation
Protons and carbon ions (hadrons) have useful properties for the treatments of patients affected by oncological pathologies. They are more precise than conventional X-rays and possess radiobiological characteristics suited for treating radio-resistant or inoperable tumours.
hadron therapy
carbon ions therapy
proton therapy
medical synchrotron
gantry
1. Introduction
“Hadron therapy”, a word that has entered the vocabulary of medicine, indicates the therapeutic use of “hadrons”, nuclear particles known in the past only in physics research centres. Hadrons derive their name from the Greek ‘hadrós’ (‘strong’), which identifies the force with which their main constituents, the quarks, interact (coined by Soviet physicist Lev B. Okun). The hadrons used today in hadron therapy centres all over the world are protons, containing three quarks, and carbon ions—made of six protons and six neutrons and thus containing 36 constituent quarks—and very recently also helium ions [1], composed of two protons and two neutrons, hence containing 12 quarks. The treatments with carbon ion beams are often referred to as CIRT, which stands for Carbon Ions Radiation Therapy. In particle physics, carbon ions are relatively light particles and therefore they are called light ions. The convention is different in radiotherapy where carbon ions are often referred to as heavy particles to distinguish them from protons.
Rationale and Diffusion of Hadron Therapy in the World
Charged atomic nuclei, such as protons or carbon ions, have a completely different energy deposition curve with respect to X-rays, showing the characteristic Bragg peak at the end of their path in tissues (Figure 1) [2].
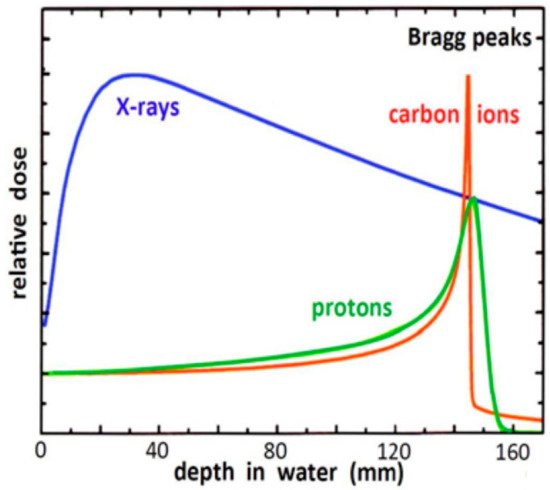
Figure 1. Energy deposition in water by X-ray photons, protons and carbon ions. The energy of the X-rays is 21 MeV. The energy of the two particles is selected to provide the same range: 148 MeV/u for protons and 270 MeV/u for carbon ions [2].
The energy deposited per gram of matter (i.e., the ‘dose’) is low when the hadron beam enters the body and is mainly concentrated at the end of the range. The so-called Bragg peak is rather narrow (few millimetres) and to cover the full longitudinal extension of the tumour a superposition of Bragg peaks with different heights and depths is necessary, creating a Spread Out Bragg Peak (SOBP). The use of a focused beam of millimetric transverse dimensions-displaced by scanning magnets in the plane perpendicular to the beam direction-allows the painting of slices of a tumour. The combination of longitudinal (varying the beam energy) and transversal (by magnetic scanning) displacement of the beam creates an almost ideal coverage of the tumour volume and a low radiation dose deposited outside. Carbon ions are more precise than protons because, due to the larger mass, they have a reduced longitudinal range variation (straggling) and a smaller lateral scattering thus a sharper lateral penumbra [3].
Carbon ions have a different action on the cells of the traversed organs with respect to protons or X-rays. At the end of their range the energy deposition per unit length (the ‘Linear Energy Transfer’ or LET) is producing a larger number of irreparable double strand DNA (deoxyribonucleic acid) breaks with a much higher probability of cell killing [4]. This action is usually expressed in terms of the relative biological effectiveness (RBE), which is defined as the ratio of the photon dose and the dose of the particle radiation leading to the same biological effect. RBE of carbon ions on the tumour can be as high as 3, thus allowing the delivery of a higher biological dose in the tumour target with respect to photons and protons, while keeping the same ‘biological’ dose in the surrounding normal tissues, or the same dose in the tumour and reduced doses and damages to the normal tissues. Moreover, the higher fraction of clustered DNA lesions produced by ions, which cannot be repaired by the usual cellular mechanisms, is processed via alternative end-joining mechanisms [5] and opens the way to the use of smart radio-sensitizers that makes tumour cells more sensitive to ion therapy. Another quantitative advantage is that ions have a reduced Oxygen Enhancement Ratio (OER) and are hence less dependent on the availability of oxygen in the tumour tissue. This means that they are effective in the treatment of hypoxia-related radio-resistant tumours, so that they can eradicate tumours that are resistant to X-ray and proton therapy [6][7][8][9]. The latter represent 1–3% of all patients treated with X-rays, for whom CIRT is the only effective radiation treatment.
Recent data also point out even more significant biological effects of ion therapy, including reduced angiogenesis [10][11], reduced metastasis [12][13] and increased immune response following exposure to light ions [14]. This implies that ion therapy can be used to enhance the effectiveness of cancer immunotherapy.
The idea of using protons to treat tumours dates back to 1946, when the American scientist Bob Wilson [15] understood their potential due to the physical characteristics of the deposited dose. It is important to note that, until the end of the 1980s, patients were irradiated at accelerators built for nuclear and sub-nuclear physics research and adapted to radiotherapy, with all the associated drawbacks. At the beginnings of the 1990s, the era of modern hadron therapy finally began, with centres dedicated exclusively to clinical activity. The first proton therapy facility is the Loma Linda University Medical Centre, in California [16]. Three rooms are equipped with rotating magnetic systems (isocentric ‘gantries’) of about ten meters diameter and a mass of about 100 tons that allow—for the first time—to vary the direction of incidence of the proton beam on the patient, as usually happens in conventional radiotherapy. In Japan, in June 1994, the first patient was treated with a carbon ion beam of about 4000 MeV at the Heavy Ion Medical Accelerator Centre in Chiba [17]. In this case, the beams are fixed, horizontal and vertical, and they serve three treatment rooms. A few years ago, the centre was upgraded with the addition of new treatment rooms, one of which equipped with a carbon ion gantry made of superconducting magnets.
The National Centre for Oncological Hadronterapy (CNAO) operates in Pave, Italy. Patient treatments started in 2011 and both protons and carbon ions are routinely delivered in three treatment rooms. Each room has a horizontal beam and room 2 has an additional vertical beamline. A fourth room, with a horizontal beamline, is fully devoted to research. Figure 2 shows the hospital facility and the synchrotron accelerator.

Figure 2. Left: in front the Centre for Oncological Hadron therapy (CNAO) hospital building, in the back the power station and the roof of the synchrotron vault. Right: view of the synchrotron and of the beam transport lines.
The growth and diffusion of hadron therapy requires many efforts and international collaborations. To this end, the European Network for Light Ion Hadron Therapy (ENLIGHT) [18] continues to play a central role in the development and diffusion of hadron therapy and in meeting the needs of the community for the education of specialised professionals.
More recently, the four European hadron therapy facilities offering CIRT, together with 18 Partners from 14 European countries, launched a four-year collaboration project named HITRIplus (Heavy Ion Therapy Research Integration plus), that has been approved in the framework of the Horizon 2020 research and innovation programme (agreement GA N. 101008548).
HITRIplus is a multidisciplinary collaborative project, aiming to open the existing facilities to the clinical and research communities, to integrate and advance biophysics and medical research in cancer treatment with ions and, in parallel, to develop innovative technologies for the next generation of centres.
Currently, proton therapy and CIRT are expanding worldwide with 94 proton therapy centres, as reported by the Particle Therapy Group website [19]; the synchrotrons of twelve centres perform CIRT with maximum ion energy of about 400 MeV/nucleon, which corresponds to 27 cm range in water. Proton therapy centres are mainly located in the United States (41 centres), Europe (19 centres), Japan (17 centres) and the UK (5 centres). Carbon ion centres are located in Japan (6 centres), Europe (4 centres) and China (2 centres). Four European clinical centres (CNAO, Heidelberg Ion Therapy Center—HIT, MedAustron and Marburger Ionenstrahl-Therapiezentrum—MIT), one Japanese and one Chinese centre produce both carbon ions and protons, thus they are called ‘multi-particle centres’. There are at present 32 proton centres and 6 carbon ions centres under construction. In addition, 26 new proton facilities and 2 carbon ions centres, including the first one in USA, are in the planning phase.
2.Hadron Therapy Achievements and Challenges
2.1. Pre-Clinical Radiobiology Research
In recent years, radiation biology is experiencing a shift in the research topics, from more classical cellular end points, such as DNA damage and RBE quantification, to studies of the tissues and of the microenvironment [20]. For example, it is well recognized that low-LET ionizing radiation might promote migration and invasion of tumour cells, while the few data collected so-far with high-LET radiation studies do not lead to clear conclusions [21]. What is known to be fundamental in the modulation of migration of tumour cells exposed to ionizing radiation is the influence of the microenvironment. Therefore, the study of the influence of radiation on the migratory and invasive capacity cannot ignore the cells that populate the tumour stroma, especially in the case of pancreatic cancers, that is characterized by abundant stroma cells including cancer-associated fibroblasts, which are known to orchestrate the crosstalk with tumour cells [22].
For this reason, thanks to a collaboration with Polyclinic San Matteo, CNAO is evaluating the cellular effects of carbon ion irradiated pancreatic adenocarcinoma cells and mucosal melanoma cells using extracellular matrix (ECM) scaffolds obtained through organ decellularization. Compared to 2D cell cultures, these ECM-derived bio-scaffolds retain growth factors, cytokines and chemokines that facilitate cell attachment, tissue integration, remodelling and differentiation. Furthermore, these scaffolds guarantee the transport of oxygen and nutrients to the seeded cells and ensure the physiological exit of the waste metabolites produced by the cells [23]. With this experimental approach, one can create in vitro a 3D growth microenvironment that mimics very closely the native tissue and it is, therefore, possible to evaluate more comprehensively the biological effects of radiations.
Together with direct invasion of surrounding tissues, perineural invasion is another crucial route of cancer spread, since numerous tumour cells have an innate ability to actively migrate along nerves, thanks to the signals of various molecules secreted by both tumour cells and non-tumour cells of the microenvironment [24]. Very few studies have addressed the influence of photon radiotherapy on this type of spreading, although it is considered as a marker of poor prognosis for numerous malignant neoplasms, including head-and-neck, pancreatic, prostate, colorectal, and salivary cancers. With the aim of providing useful information for the treatment with hadron therapy of these types of tumours, at CNAO a research group has started to investigate in vitro the influence of high LET radiation on migration and invasion of salivary gland adenoid cystic carcinoma and mucosal melanoma cells after different irradiation protocols, using also Neurotrophin-3 and specific inhibitors/antagonists.
To date, the reasons for the inter-individual variability of the response to radiotherapy within the same group of tumours with the same histology/site/stage are not known, nor is the origin of the different radiosensitivity of the irradiated healthy tissues. Thus, pre-clinical carbon ion radiobiology urgently needs also studies aiming at guiding patient selection and treatment protocols to achieve optimal clinical results. In this direction, CNAO researchers have recently started an experimental project to study the radio-sensitivity and induced molecular alterations of different radiation types on cancer-derived models and on organoids of head-and-neck squamous cell carcinomas [25]. Although local control is generally very high with carbon ion beams in most malignancies, in some cases radiotherapy must be combined with systemic therapies to control metastasis and increase survival. Nevertheless, to date very few radiobiology studies specifically investigated the potential synergistic interactions of chemotherapeutic agents/radio-sensitizer and ion irradiations. CNAO research is moving towards the evaluation of an inhibitor of apoptosis proteins as radio-sensitizer combined with protons or carbon ions, to provide the biological background supporting future clinical trials with particles radiotherapy combined with these drugs in head-and-neck cancer patients.
Finally, since the use of immunotherapy has become a critical treatment modality in many advanced cancers, one of the most asked questions in clinical radiobiology of carbon ions concerns the speculations that these irradiations may enhance tumour immunogenicity and, consequently, whether abscopal effects and the combination CIRT with immunotherapy can produce better clinical outcomes [26].
2.2. Clinical Activities: Pathologies and Results
CNAO treated more than 3700 patients with a wide range of pathologies, whose incidence rates are indicated in Figure 3. A little more than half of them (55%) were treated with carbon ions.
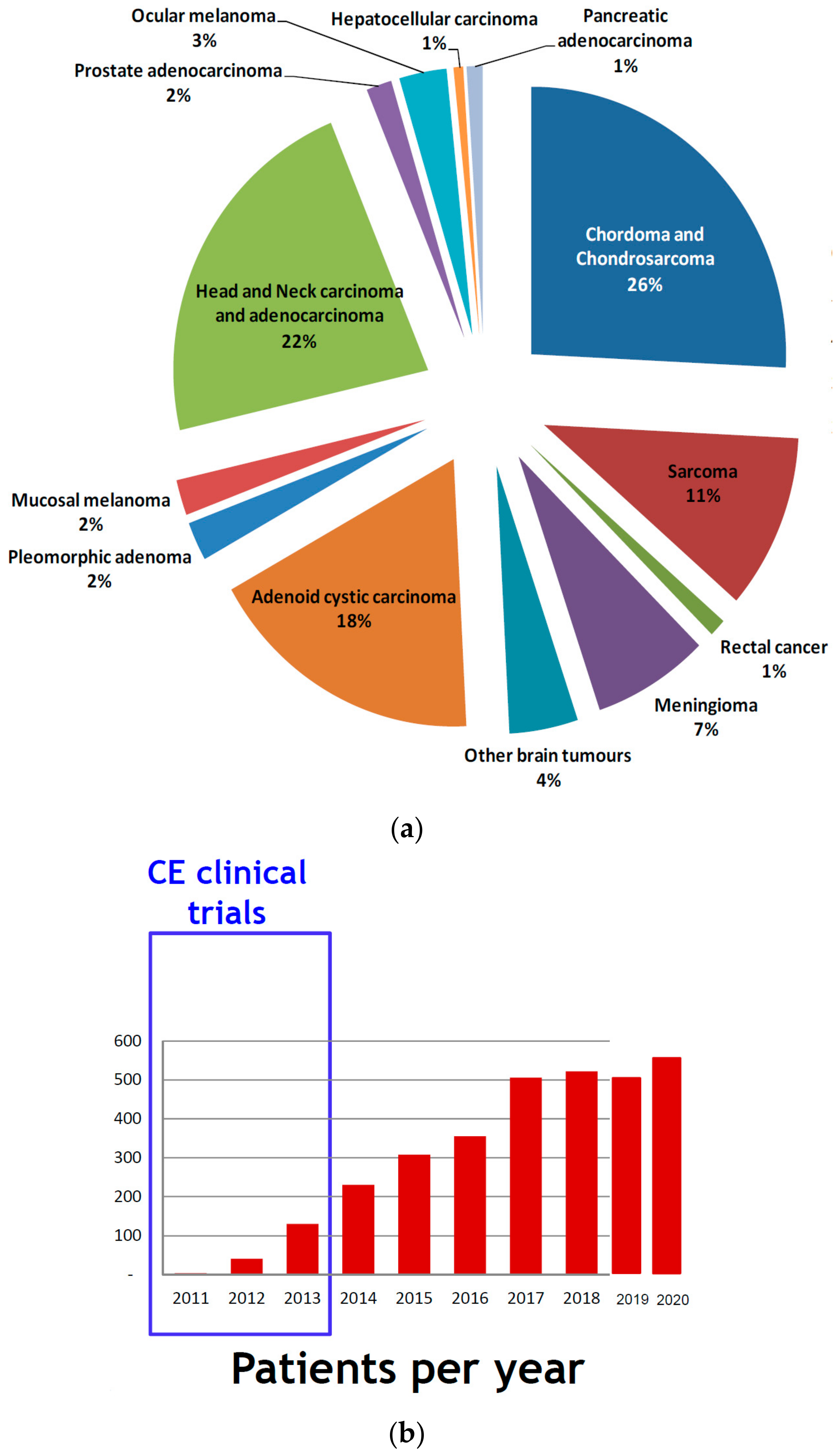
Figure 10. (a) Incidence of tumour pathologies treated at CNAO; (b) Number of patients treated each year at CNAO.
After an initial clinical trial stage, it is necessary to obtain the CE certification for the CNAO medical device. The number of treated patients per year has grown year after year (Figure 10). Currently, the Centre treats almost 600 patients yearly and its operational capacity might be increased by about 20%. The Italian Ministry of Health has introduced a list of pathologies for which treatments are authorized and reimbursed by the National Health System, the so-called Essential Levels of Assistance (LEA). The admitted pathologies are the following ten:
- chordomas and chondrosarcomas (of the skull base and of the spine);
- meningioma;
- brain tumours (trunk);
- adenoid cystic carcinomas of the salivary glands;
- orbit tumours including eye melanoma;
- sino-nasal carcinomas;
- soft tissue and bone sarcomas (all sites);
- recurrent tumours (retreatment);
- patients with immunological disorders;
- paediatric solid tumours.
The Health Ministry is currently discussing other categories considering selection criteria based on the evolution of NTCP or Tumour Control Probability (TCP). NTCP-based patient selection for haematological malignancies is currently being implemented at CNAO in collaboration with Institut Curie of Paris (France). Within the ten categories identified by the LEA, it is estimated that each year, in Italy, around 5000 patients should be treated with protons and around 1000 with carbon ions over a total population of 60 million.
For this reason, it appears essential to create a network, where CNAO operates as a hub, connected to other future national proton therapy centres. This distribution model is ideally interesting, but it needs solid and defined patient selection mechanisms and strong interdisciplinary interactions between CNAO and other hospitals, to manage the all-around complexity of particle therapy patients.
Patients’ data show that almost 25–30% were treated at CNAO in a re-irradiation setting and 15% of patients have large tumour volumes (>500 cc); nevertheless, the local control appears promising and consistent with the literature data available for similar hadron therapy treatments.
The loco regional toxicities, routinely scored with Common Toxicity Criteria Adverse Events (CTCAE), are mild and in some cases even better than literature, thanks also to the performance of the active scanning system and the careful treatment planning.
During the last two years more than 100 papers were published in scientific journals by CNAO researchers. In 2021, 50 publications with overall Impact Factor 290.5 were published. It is not the purpose of this text to present the clinical results related to the single pathologies, but a small summary of the most common diseases treated at CNAO is here outlined, presenting data on skull bases chordomas, head-and-neck tumours and malignant mucosal melanoma. Data are taken from a literature review of the Scientific Direction, in collaboration with the medical staff and with the Istituto Mario Negri (Milan, Italy).
2.3. Skull Base Chordoma and Chondrosarcoma
Chordoma is a rare primary bone tumour arising from notochord remnants with an incidence of 0.8–1 per million, with approximately one-third arising from the midline clivus and skull-base. Chondrosarcomas are malignant cartilaginous tumours that occur in approximately 1.0 per 2 million at the skull base. For both these tumours, the importance of surgery has been well established. Complete resection is desired as optimal goal of surgical procedure; however, it is often precluded by tumour location and the surrounding critical structure such as brainstem or optic pathways.
As a result, any residual or microscopic disease is targeted by radiation therapies to reduce the risk of disease recurrence or progression and improve prognosis. To date, photon radiation is the most accessible radiation modality; however, the major limitation of this modality for skull base chordomas and chondrosarcomas is that the delivery of the required dose is limited by the risk of injury to adjacent normal structures, such as the brainstem and visual pathway. Particle beam therapy (proton therapy (PT) and CIRT) appears to be the most effective radiation modality in the management of skull-base chordomas, allowing the delivery of high radiation dose levels, maximizing the positive balance between Gross Tumour Volume (GTV) optimal dose coverage and organ at risk sparing. Moreover, CIRT has several theoretical advantages: (1) it has a sharper penumbra than PT, allowing even better normal tissue sparing; (2) it is less dependent on fractionation; and (3) it has a higher relative biologic effectiveness in comparison to other modalities with respect to tumour cell death.
For the case of chordoma, in Iannalfi et al. 2020 [27], a collection of 135 patients (70 PT and 65 CIRT) treated at CNAO between November 2011 and December 2018 has been analysed. PT was delivered with a total dose of 74 Gy in 37 fractions, while CIRT total dose was 70.4 Gy(RBE), delivered in 16 fractions. CIRT has been used in more complicated cases. After a median follow-up of 44 (range, 6–87) months, 14 (21%) and 8 (11%) local failures were observed in CIRT and PT group, respectively. Five-year local control (LC) rate was 71% in CIRT cohort and 84% in PT cohort. The estimated 5-year overall survival (OS) rate in the CIRT and PT group was 82% and 83%, respectively. On multivariate analysis, optic pathways and/or brainstem compression and dose coverage are independent prognostic factors of local failure risk. High-rate toxicity grades ≥ 3 were reported in 11% of patients. Generally, the main role of particle radiotherapy in the treatment of chordomas has obtained wide consensus. Prospective observational studies and/or registries can help to find prognostic factors for local control and survival and to provide criteria for a patient-customized treatment strategy. Model-based approach can be useful to define toxicity risks for critical issues as temporal lobe necrosis.
2.4. Head-and-Neck Tumours
Historically, radiation therapy has played an essential role in the management of head-and-neck cancers (HNCs), in various clinical settings. Modern technologies, including intensity modulated radiation therapy (IMRT) and volumetric modulated arc therapy (VMAT), have aided decreasing beam-on treatment time and making the delivery of photon radiation therapy more conformal and precise. Consequently, these technologies have reduced late toxicities, such as xerostomia, trismus, temporal lobe necrosis, neurological injury, and hearing impairment. In the landscape of treatment advancement for HNCs, particle therapy plays an important role. Recently, IMPT, thanks to its physical and biological features, has emerged as a potentially advantageous technique for treating HNCs, reducing dose to organs at risk (OARs) without jeopardizing tumour control, theoretically allowing a safe dose escalation. Proton therapy offers a dosimetric advantage over IMRT in the management of HNCs. While respecting dose constraints for normal tissues, IMPT is a promising technique for treatment-related toxicity reduction and potential dose escalation. In dosimetric comparisons, both techniques often sufficiently covered the target volume without issues. However, average minimum, maximum, and mean doses to the target volume are in general all higher for IMPT. Furthermore, IMPT appears to have an overall advantage in OAR doses in the brain stem, spinal cord, optic structures, cochlea, larynx, contralateral parotid and oral cavity with only a few exceptions. Dosimetric evidence of the superiority of IMPT compared to IMRT needs to be confirmed through evidence based clinical advantages. Several clinical studies are currently underway to provide compelling evidence for the clinical benefit of IMPT in HNCs. While IMPT has been employed purely for dosimetric properties, CIRT offers similar favourable physical characteristics, as well as an additional radiobiological advantage for radio-resistant tumours, such as salivary glands HNCs, malignant mucosal melanomas and sarcomas.
Salivary gland tumours (SGTs) are uncommon diseases that represent about <1% of the all HNCs diagnosed in Europe. They arise either in the major or minor salivary glands, which are both located in the head and neck and include >20 histotypes [28][29]. SGTs have a known radio-resistance as well as frequently horseshoe-shaped volume and proximity to radiosensitive normal structures. For resectable cases, the mainstay of treatment is complete surgical resection with adequate free margins. In high-risk patients with adverse prognostic factors, based on the pathology results (close/positive margins, high grade, T size, vascular/perineural invasion and lymph node involvement), postoperative radiotherapy (PORT) is recommended. Patients with unresectable or inoperable SGTs undergo radiation therapy (RT) alone. Among SGTs, adenoid cystic carcinoma (ACC) is characterized by a high frequency of local recurrence; in the literature, it is the most investigated histotype to be treated with particles.
For SGTs, Vischioni et al. [30] reported a retrospective study of 51 patients (pts) with inoperable recurrent SGTs retreated with CIRT. Acute toxicity was G1 in 19 pts (37.3%), G2 in 19 pts (37.3%) and G3 in 2 pts (3.9%). The median follow-up time was 19 months. Twenty-one (41.2%) patients had Stable Disease (SD) and 30 (58.8%) tumour progression at the time of last follow-up. Furthermore, 9 (18%) patients had G1 late toxicity (scored according to CTCAE), 19 (37%) had G2 and 9 (17. 5%) had G3. Two-year PFS and OS were 52.2% and 64%, respectively.
SGTs are rare conditions that are difficult to manage; therefore, they need to be treated in referral high-volume centres with a strong multidisciplinary expertise. Both CIRT and PT have been shown to be effective and safe in SGTs, though possibly with different indications. In a setting of high-risk patients without macroscopic tumour after surgery and proximity to radiosensitive normal structures, PT might be considered, while CIRT might be used in most inoperable or operable, but locally advanced, cases. A body of compelling evidence shows that CIRT improves LC, OS and toxicity in patients diagnosed with adenoid cystic carcinoma (ACC) [31]. The definition of a tumour signature allowing to select CIRT vs. PT or IMRT is an open question. Given the high efficacy of CIRT at CNAO, multidisciplinary follow-up in high expertise centres with well-trained oncologists in particle therapy should be pursued for each patient.
2.5. Malignant Mucosal Melanoma
Malignant mucosal melanomas (MM) are extremely rare and aggressive cancers. Compared to cutaneous melanomas, MM show different epidemiological and molecular features leading to unpredictable biological behaviour and worse prognosis. The incidence is very low, with an estimated annual rate of 1.5 per million in Europe [32]. Despite recent advances in treatment options, patients’ survival remains very short, with a five-year OS rate of only 25% regardless of stage [33][34]. MM more frequently affect the upper aero-digestive tract, with the paranasal sinuses and nasal cavity as the most common sites. Among all melanomas, primary melanomas originating from the gynaecological tract are the rarest and really aggressive [35]. Head-and-neck mucosal melanoma (HNMM) comprise about 1% of all head-and-neck malignancies. Due to HNMM rarity and unpredictable clinical course, prospective studies are challenging, and to date no optimal treatment modality has been fully established. The mainstay of treatment for HNMM is surgery. Clear surgical margins are one of the most important prognostic factors [36][37][38], but are often difficult to obtain due to the anatomical complexity of the region and its proximity to vital structures.
Considering literature data, hadron therapy and CIRT in particular should be considered as a safe and effective treatment modality in curative setting for HNMM [39] and gynaecological [40][41] patients not amenable to surgery. This is valid thanks to the dosimetrical advantage over conventional photon radiotherapy in case of strict proximity of organs at risk and to the radiobiological potential to overcome MM radio-resistance. This suggests that the addition of a systemic treatment to CIRT in a multimodal approach may improve patients’ outcome, even though the contribution of concomitant chemotherapy was not confirmed in other Japanese studies [42]. Indeed, the major concern for HNMM is the mortality resulting from the propensity to metastasize early and widely.
Literature data and preliminary CNAO clinical results confirm that particle therapy, and in particular CIRT, is a safe and effective approach in the management of locally advanced HNMM. Preliminary data concerning the combination between Immune Checkpoint Inhibitors (ICIs) and CIRT appear promising in this setting [43]. These considerations lead to conclude that it is extremely important to manage patients considering CIRT in a multidisciplinary context in high expertise centres, in order to improve outcomes. Despite the good results in terms of LC and toxicity, overall survival remains poor, and prospective studies, preferably multi-centric, given the rarity of this disease, are needed to try to improve patients’ outcomes.
2.6. Clinical Research Trials
Currently, CNAO is also performing clinical research and, for the following studies, the enrolment is ongoing:
- PIOPPO (preoperative treatment of borderline operable pancreatic adenocarcinomas with chemotherapy and radiotherapy with carbon ions) [44]: a phase 2 study, to evaluate the neo-adjuvant combination approach with chemotherapy followed by short-course carbon-ion radiotherapy for borderline pancreatic adenocarcinomas [45];
- CYCLE (carbon ion radiation therapy in the treatment of mucosal melanomas of the female lower genital tract): a phase 2 study to test the efficacy and the tolerability of carbon-ion treatments of unresectable gynaecological mucosal melanomas;
- CYCLOPS (Phase II clinical study on the re-irradiation of lateral pelvic recurrences of gynecological malignancies) a phase 2 study, to evaluate the efficacy and tolerability of carbon-ion re-irradiation for not central relapses of gynaecological neoplasms at the edge of the previous photon beam radiotherapy;
- 4D-MRI (guidance for organ motion management in particle treatments of thoraco-abdominal tumours): a clinical trial to study the organ motion of thoraco-abdominal neoplasms through 4D MRI;
- INSIDE: an experimental observational real-time live study of the particle range. This study is aimed at the early identification of potential morphological modifications of the target or of the adjacent areas, which might cause an anomaly in the dose distribution.
CNAO is also actively participating in the implementation of international clinical trials, such as:
- STOPSTORM (a prospective European validation cohort for stereotactic therapy of Re-entrant tachycardia): aimed at the definition and harmonization of ventricular tachycardia radiation therapy treatment options (both medical and ablation therapy); to note that, at the end of 2019, in collaboration with Fondazione IRCSS Polyclinic San Matteo of Pave, for the first time in the literature, a patient affected by ventricular tachycardia (VT) has been successfully treated with proton beams at CNAO [46].
- PROTECT (PROton versus photon Therapy for Esophageal Cancer—a Trimodality strategy): a randomized clinical study aimed at building scientific evidence (in terms of efficacy and toxicity) on the proton pre-op treatment, combined with chemotherapy, for oesophageal cancer. This clinical trial is then compared to the current gold standard treatment, which is a combination of chemotherapy and IMRT.
Moreover, CNAO is an active partner of ETOILE, an international randomized study, aiming to compare the carbon ion treatment to the traditional low-LET radiotherapy techniques (photons and protons) for radio-resistant histologies. In addition, it is involved in the randomized observational SACRO study, promoted by the Italian Sarcoma Group (ISG), that aims to compare upfront surgery to particle therapy in patients with sacral chordoma.
CNAO is also a partner, together with the Fondazione IRCSS Istituto Nazionale dei Tumori of Milan, of a prospective study promoted by the Istituto Europeo di Oncologia (Milan) and funded by AIRC (Italian Association of Cancer Research). The goal of this study is to evaluate the efficacy and toxicity of an early carbon ion boost, followed by Image Guided IG-IMRT for high-risk prostate cancers.
Lastly, CNAO is analysing the results of the two Italian multicentre phase 2 clinical studies SINTART1 and SINTART2, designed to primarily assess the efficacy of a multimodality treatment (induction chemotherapy, surgery, photon and/or heavy ion radiotherapy) of patients with operable (SINTART1) and inoperable (SINTART2) sinonasal carcinoma.
A different model-based approach is worthwhile to mention as an alternative to clinical trials for hadron/proton therapy. The relationship between dose distribution and the risk of radiation-induced toxicity is described by NTCP [47]. Based on an in silico NTCP analysis on predicted toxicity between photons RT and proton therapy, Langendjik et al. [48] first suggested a step-wise RT methodology for selecting patients for proton therapy, accepted for the treatment refund by the Dutch health authorities. Moreover, this approach, known as model-based method, is implemented in the Netherlands to identify patients with head and neck cancer who may benefit most from proton therapy [49]. In brief, for each patient who may benefit from proton radiotherapy, a comparison between the most optimal photon and proton therapy plans were performed with the aim of estimating the NTCP profiles (considering the dose distribution and other clinical/treatment variables) for both techniques. The subtraction of photon-based from the proton-based NTCP (ΔNTCP) gives the probability of toxicity and patients are considered eligible for proton therapy if the model predicts less clinically relevant toxicity [50][51].
References
- Haberer, T. Ion Beam Therapy at HIT: Options for Multi-Ion Treatment and Research. In Talk at the 3rd HITRIplus Seminar; Heidelberg University Hospital: Heidelberg, Germany, 13 October 2021; Available online: https://indico.cern.ch/event/1081649/ (accessed on 30 November 2021).
- Krämer, K.; Durante, M. Ion beam transport calculations and treatment plans in particle therapy. Eur. Phys. J. 2010, 60, 195–202.
- Suit, H.; DeLaney, T.; Goldberg, S.; Paganetti, H.; Clasie, B.; Gerweck, L.; Niemierko, A.; Hall, E.; Flanz, J.; Hallman, J.; et al. Proton vs carbon ion beams in the definitive radiation treatment of cancer patients. Radiother. Oncol. 2010, 95, 3–22.
- Durante, M.; Loeffler, J.S. Charged particles in radiation oncology. Pub. Med. 2009, 7, 37–43.
- Averbeck, N.B.; Topsch, J.; Scholz, M.; Kraft-Weyrather, W.; Durante, M.; Taucher-Scholz, G. Efficient Rejoining of DNA Double-strand breaks despite increased cell-killing effectiveness following spread-out bragg peak carbon-ion irradiation. Front. Oncol. 2016, 6, 1–8.
- Chiblak, S.; Tang, Z.; Campos, B.; Gal, Z.; Unterberg, A.; Debus, J.; Herold-Mendel, C.; Abdollahi, A. Radiosensitivity of patient-derived glioma stem cell 3-dimensional cultures to photon, proton, and carbon irradiation. Int. J. Radiat. Oncol. Biol. Phys. 2016, 95, 112–119.
- Peschke, P.; Debus, J. Relative biological effectiveness of carbon ions for local tumor control of a radioresistant prostate carcinoma in the rat. Int. J. Radiat. Oncol. Biol Phys. 2011, 79, 239–246.
- Debus, J.; Abdollahi, A. For the next trick: New discoveries in radiobiology applied to glioblastoma. Am. Soc. Clin. Oncol. Educ. Book 2014, 34, e95–e99.
- Klein, C.; Dokic, I.; Mairani, A.; Mein, S.; Brons, S.; Haring, P.; Haberer, T.; Jakel, O.; Zimmerman, A.; Zenke, F.; et al. Overcoming hypoxia-induced tumor radiore-sistance in non-small cell lung cancer by tar-geting DNA-dependent protein kinase in com-bination with carbon ion irradiation. Radiat. Oncol. 2017, 12, 208.
- Takahashi, Y.; Teshima, T.; Kawaguchi, N.; Hamada, Y.; Mori, S.; Madachi, A.; Ikeda, S.; Mizuno, H.; Ogata, T.; Nojima, K.; et al. Heavy ion irradiation inhibits in vitro angiogenesis even at sublethal dose. Cancer Res. 2003, 63, 4253–4257.
- Kamlah, F.; Hänze, J.; Arenz, A.; Seay, U.; Hasan, D.; Juricko, J.; Bischoff, B.; Gottschald, O.R.; Fournier, C.; Taucher-Scholz, G.; et al. Comparison of the effects of carbon ion and photon irradiation on the angiogenic response in human lung adenocarcinoma cells. Int. J. Radiat. Oncol. Biol. Phys. 2011, 80, 1541–1549.
- Ogata, T.; Teshima, T.; Kagawa, K.; Teshima, T.; Kagawa, K.; Hishikawa, Y.; Takahashi, Y.; Kawaguchi, A.; Suzumoto, Y.; Nojima, K.; et al. Particle irradiation suppresses metastatic potential of cancer cells. Cancer Res. 2005, 65, 113–120.
- Rieken, S.; Rieber, J.; Brons, S.; Rieber, J.; Brons, S.; Habermehl, D.; Rief, H.; Orschiedt, L.; Lindel, K.; Weber, K.J.; et al. Radiation-induced motility alterations in medulloblastoma cells. J. Radiat. Res. 2015, 56, 430–436.
- Durante, M.; Brenner, D.J.; Formenti, S.C. Does heavy ion therapy work through the immune system? Int. J. Radiat. Oncol. Biol. Phys. 2016, 96, 934–936.
- Wilson, R.R. Radiological use of fast protons. Radiology 1946, 47, 487–491.
- Slater, J.M.; Archambeau, J.O.; Dicello, J.F.; Slate, J.D. Proton beam irradiation: Toward routin clinical utilization. In Hadrontherapy in Oncology: Proceedings of the First International Symposium on Hadrontherapy, Como, Italy, 18–21 October 1993; Amaldi, U., Larsson, B., Eds.; Elsevier Science: Amsterdam, The Netherland, 1994; p. 130.
- Kawachi, K.; Yamada, S.; Sato, K.; Ogawa, H.; Soga, F.; Kanai, T.; Endo, M.; Hirao, Y. Heavy ion medical accelerator facility in Japan. In Hadrontherapy in Oncology: Proceedings of the First International Symposium on Hadrontherapy, Como, Italy, 18–21 October 1993; Amaldi, U., Larsson, B., Eds.; Elsevier Science: Amsterdam, The Netherlands, 1994; p. 229.
- ENLIGHT. ENLIGHT Coordination. Available online: https://enlight.web.cern.ch/enlight (accessed on 30 November 2021).
- An Organization for Those Interested in Proton, Light Ion and Heavy Charged Particle Radiotherapy. Particle Therapy Co-Operative Group. Available online: www.ptcog.ch (accessed on 30 November 2021).
- Loeffler, J.S.; Durante, M. Charged particle therapy—optimization, challenges and future directions. Nat. Rev. Clin. Oncol. 2013, 10, 411–424.
- Fujita, M.; Yamada, S.; Imai, T. Irradiation induces diverse changes in invasive potential in cancer cell lines. Semin. Cancer Biol. 2015, 35, 45–52.
- Facoetti, A.; Di Gioia, C.; Pasi, F.; Di Liberto, R.; Corbella, F.; Nano, R.; Ciocca, M.; Valvo, F.; Orecchia, R. Morphological analysis of amoeboid-mesenchymal transition plasticity after low and high LET radiation on migrating and invading pancreatic cancer cells. Anticancer Res. 2018, 38, 4585–4591.
- Croce, S.; Peloso, A.; Zoro, T.; Avanzini, M.A.; Cobianchi, L. A Hepatic scaffold from decellularized liver tissue: Food for thought. Biomolecules 2019, 9, 813.
- Zhang, M.; Zhu, Z.-L.; Gao, X.-L.; Wu, J.-S.; Liang, X.-H.; Tang, Y.-L. Functions of chemokines in the perineural invasion of tumors (Review). Int. J. Oncol. 2018, 52, 1369–1379.
- Di Renzo, M.F.; Corso, S. Patient-derived cancer models. Cancers 2020, 12, 3779.
- Friedrich, T.; Henthorn, N.; Durante, M. Modeling radioimmune response-current status and perspectives. Front. Oncol. 2021, 11, 647272.
- Iannalfi, A.; D’Ippolito, E.; Riva, G.; Molinelli, S.; Gandini, S.; Viselner, G.; Fiore, M.R.; Vischioni, B.; Vitolo, V.; Bonora, M.; et al. Proton and carbon ion radiotherapy in skull base chordomas: A prospective study based on a dual particle and a patient-customized treatment strategy. Neurol. Oncol. 2020, 22, 1348–1358.
- Van Dijk, B.A.; Gatta, G.; Capocaccia, R.; Pierannunzio, D.; Strojan, P.; Licitra, L.; The RARECARE Working Group. Rare cancers of the head and neck area in Europe. Eur. J. Cancer 2012, 48, 783–796.
- El-Naggar, A.K.; Chan, J.F.K.; Grandis, J.R.; Takata, T.; Slootweg, P.J. WHO Classification of Head and Neck Tumours, 4th ed.; World Health Organization: Geneva, Switzerland, 2017; Volume 9.
- Vischioni, B.; Dhanireddy, B.; Severo, C.; Bonora, M.; Ronchi, S.; Vitolo, V.; Fiore, M.R.; D’Ippolito, E.; Petrucci, R.; Barcellini, A.; et al. Reirradiation of salivary gland tumors with carbon ion radiotherapy at CNAO. Radiother. Oncol. 2020, 145, 172–177.
- Loap, P.; Vischioni, B.; Bonora, M.; Ingargiola, R.; Ronchi, S.; Vitolo, V.; Barcellini, A.; Goanta, L.; De Marzi, L.; Dendale, R.; et al. Biological rationale and clinical evidence of carbon ion radiation therapy for adenoid cystic carcinoma: A narrative review. Front. Oncol. 2021, 11, 789079.
- RARECAREnet. Information Network on Rare Cancers. 2017. Available online: http://www.rarecarenet.eu/rarecarenet/ (accessed on 30 November 2021).
- Kirchoff, D.D.; Deutsch, G.B.; Foshag, L.J.; Lee, J.H.; Sim, M.-S.; Faries, M.B. Evolving therapeutic strategies in mucosal melanoma have notiImproved survival over five decades. Am. Surg. 2016, 82, 1–5.
- Teterycz, P.; Czarnecka, A.M.; Indini, A.; Spałek, M.J.; Labianca, A.; Rogala, P.; Cybulska-Stopa, B.; Quaglino, P.; Ricardi, U.; Badellino, S.; et al. Multimodal treatment of advanced mucosal melanoma in the era of modern immunotherapy. Cancers 2020, 12, 3131.
- Gadducci, A.; Carinelli, S.; Guerrieri, M.E.; Aletti, G.D. Melanoma of the lower genital tract: Prognostic factors and treatment modalities. Gynecol. Oncol. 2018, 150, 180–189.
- Penel, N.; Mallet, Y.; Mirabel, X.; Van, J.T.; Lefebvre, J.-L. Primary mucosal melanoma of head and neck: Prognostic value of clear margins. Laryngoscope 2006, 116, 993–995.
- Shuman, A.G.; Light, E.; Olsen, S.H.; Pynnonen, M.A.; Taylor, J.M.; Johnson, T.M.; Bradford, C.R. Mucosal melanoma of the head and neck: Predictors of prognosis. Arch. Otolaryngol. Head Neck Surg. 2011, 137, 331–337.
- Lee, S.P.; Shimizu, K.T.; Tran, L.M.; Juillard, G.; Calcaterra, T.C. Mucosal melanoma of the head and neck: The impact of local control on survival. Laryngoscope 1994, 104, 121–126.
- Ebner, D.K.; Malouff, T.D.; Frank, S.J.; Koto, M. The role of particle therapy in adenoid cystic carcinoma and mucosal melanoma of the head and neck. Int. J. Part Ther. 2021, 8, 273–284.
- Murata, H.; Okonogi, N.; Wakatsuki, M.; Kato, S.; Kiyohara, H.; Karasawa, K.; Ohno, T.; Nakano, T.; Kamada, T.; Shozu, M.; et al. Long-term outcomes of carbon-ion radiotherapy for malignant gynecological melanoma. Cancers 2019, 11, 482.
- Barcellini, A.; Vitolo, V.; Facoetti, A.; Fossati, P.; Preda, L.; Fiore, M.R.; Vischioni, B.; Iannalfi, A.; Bonora, M.; Ronchi, S.; et al. Feasibility of carbon ion radiotherapy in the treatment of gynecological melanoma. In Vivo 2019, 33, 473–476.
- Takayasu, Y.; Kubo, N.; Shino, M.; Nikkuni, O.; Ida, S.; Musha, A.; Takahashi, K.; Hirato, J.; Shirai, K.; Saitoh, J.; et al. Working Group on Head and Neck Tumors. Carbon-ion radiotherapy combined with chemotherapy for head and neck mucosal melanoma: Prospective observational study. Cancer Med. 2019, 8, 7227–7235.
- Cavalieri, S.; Ronchi, S.; Barcellini, A.; Bonora, M.; Vischioni, B.; Vitolo, V.; Villa, R.; Del Vecchio, M.; Licitra, L.; Orlandi, E. Toxicity of carbon ion radiotherapy and immune checkpoint inhibitors in advanced melanoma. Radiother. Oncol. 2021, 164, 1–5.
- ClinicalTrials.gov. The U.S. National Library of Medicine. ID: NCT03822936. Available online: https://ClinicalTrials.gov (accessed on 30 November 2021).
- Vitolo, V.; Cobianchi, L.; Brugnatelli, S.; Barcellini, A.; Peloso, A.; Facoetti, A.; Vanoli, A.; Delfanti, S.; Preda, L.; Molinelli, S.; et al. Preoperative chemotherapy and carbon ions therapy for treatment of resectable and borderline resectable pancreatic adenocarcinoma: A prospective, phase II, multicentre, single-arm study. BMC Cancer 2019, 19, 922.
- Dusi, V.; Vitolo, V.; Frigerio, L.; Totaro, R.; Valentini, A.; Barcellini, A.; Mirandola, A.; Perego, G.B.; Coccia, M.; Greco, A.; et al. First-in-man case of non-invasive proton radiotherapy for the treatment of refractory ventricular tachycardia in advanced heart failure. Eur. J. Heart Fail. 2020, 23, 195–196.
- Niemierko, A.; Goitein, M. Calculation of normal tissue complication probability and dose-volume histogram reduction schemes for tissues with a critical element architecture. Radiother. Oncol. 1991, 20, 166–176.
- Langendijk, J.A.; Lambin, P.; De Ruysscher, D.; Widder, J.; Bos, M.; Verheij, M. Selection of patients for radiotherapy with protons aiming at reduction of side effects: The model-based approach. Radiother. Oncol. 2013, 107, 267–273.
- Langendijk, J.A.; Hoebers, F.J.P.; de Jong, M.A.; Doornaert, P.; Terhaard, C.H.J.; Steenbakkers, R.J.H.M.; Hamming-Vrieze, O.; van de Kamer, J.B.; Verbakel, W.F.A.R.; Keskin-Cambay, F.; et al. National protocol for model-based selection for proton therapy in head and neck cancer. Int. J. Part Ther. 2021, 8, 354–365.
- Tambas, M.; Steenbakkers, R.J.H.M.; van der Laan, H.P.; Wolters, A.M.; Kierkels, R.G.J.; Scandurra, D.; Korevaar, E.W.; Oldehinkel, E.; van Zon-Meijer, T.W.H.; Both, S.; et al. First experience with model-based selection of head and neck cancer patients for proton therapy. Radiother. Oncol. 2020, 151, 206–213.
- Dionisi, F.; Widesott, L.; Van Vulpen, M.; Fuller, C.D.; Frondizi, R.; Meneguzzo, M.; Blanchard, P.; Amichetti, M.; Sanguineti, G. Methodologies to increase the level of evidence of real-life proton therapy in head and neck tumors. Int. J. Part Ther. 2021, 8, 328–338.
More
Information
Subjects:
Health Care Sciences & Services
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.8K
Revisions:
2 times
(View History)
Update Date:
07 Mar 2022
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




