
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Elizabeth Buchbinder | + 2595 word(s) | 2595 | 2021-12-15 04:11:55 | | | |
| 2 | Jessie Wu | -14 word(s) | 2581 | 2022-01-13 02:26:04 | | |
Video Upload Options
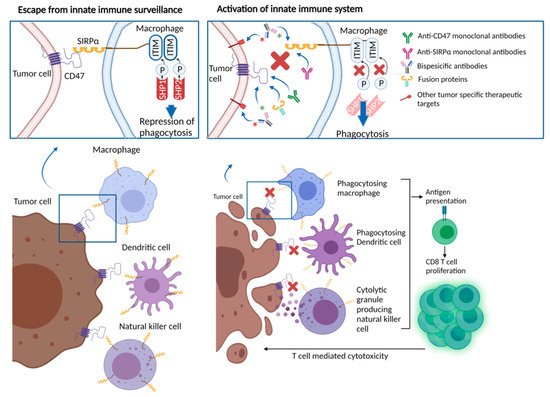
The interaction between cluster of differentiation 47 (CD47) on cancer cells and signal regulatory protein alpha (SIRPα) on immune cells, such as macrophages and dendritic cells, generates a “don’t eat me” signal. This is a common mechanism that provides cancer cells an escape from the innate immune system. Several therapeutics directed to CD47 or SIRPα have entered early clinical trials in recent years.
1. Background
In the past decade, the field of cancer immunotherapy has rapidly advanced, establishing a crucial role for immune checkpoint blockers in the treatment of a variety of cancer types. In parallel with these remarkable clinical developments, further efforts have focused on ways of unleashing adaptive immune responses against cancer. CD47, a cell surface molecule overexpressed by several cancer types that facilitates immune escape from macrophages, dendritic cells and natural killer cells, and its ligand SIRPα, have emerged as potential therapeutic targets. A number of agents directed to CD47/SIRPα have been developed and demonstrated preclinical activity. Early phase clinical trials are investigating CD47/SIRPα directed agents with available data, suggesting safety and preliminary activity.
2. Role of CD47/SIRPα in Cancer
3. Therapies Targeting CD47/SIRPα in Cancer
| Agent | Therapeutic Target |
Design | Phase | Disease Site | Accrual Goal | Identifier |
|---|---|---|---|---|---|---|
| Monoclonal Antibodies | ||||||
| IBI188 (Letaplimab) | CD47 | IBI188 +/− rituximab | I | Metastatic solid tumors or lymphoma | 92 | NCT03717103 |
| IBI188 +/− azacitidine | I | Myelodysplastic syndrome | 12 | NCT04485065 | ||
| Hu5F9-G4 (Magrolimab) | CD47 | Hu5F9-G4 (Magrolimab) + Pembrolizumab | II | Hodgkin’s lymphoma | 24 | NCT04788043 |
| Hu5F9-G4 (Magrolimab) | I | Hematologic malignancies | 20 | NCT02678338 | ||
| Hu5F9-G4 (Magrolimab) + acalabrutinib + rituximab or other combinations without Hu5F9-G4 (Magrolimab) | I | Non-Hodgkin’s Lymphoma | 30 | NCT03527147 | ||
| Hu5F9-G4 (Magrolimab) + Obinutuzumab + venetoclax | I | Non-Hodgkin’s Lymphoma | 76 | NCT04599634 | ||
| ZL-1201 | CD47 | ZL-1201 | I | Metastatic solid tumors or refractory lymphomas | 66 | NCT04257617 |
| STI-6643 | CD47 | STI-6643 | I | Metastatic solid tumors | 24 | NCT04900519 |
| CC-9002 | CD47 | CC-90002 +/−rituximab | Part A: Metastatic solid tumors, multiple Myeloma or non-Hodgkin’s lymphoma Part B, relapsed and/or refractory CD20-positive NHL |
60 | NCT02367196 | |
| AK117 | CD47 | AK117 | I | Metastatic solid tumors or lymphoma | 162 | NCT04728334 |
| AK117 + azacitidine | I/II | Myelodysplastic syndrome | 190 | NCT04900350 | ||
| AO-176 | CD47 | AO-176 +/− paclitaxel | I/II | Metastatic solid tumors | 132 | NCT03834948 |
| AO-176 +/− dexamethasone or dexhamethasone + bortezomide | I | Multiple myeloma | 102 | NCT04445701 | ||
| IMC-002 | CD47 | IMC-002 | I | Metastatic solid tumors or lymphoma | 24 | NCT04306224 |
| TQB2928 | CD47 | TQB2928 | I | Metastatic solid tumors or hematologic malignancies | 20 | NCT04854681 |
| FSI-189 | SIRPα | FSI-189 +/− rituximab | I | Non-Hodgkin’s lymphoma (B-cell) | 63 | NCT04502706 |
| BI 765063 | SIRPα | BI 765063 +/− PD-1 inhibitor | I | Metastatic solid tumors with SIRPα polymorphism | 116 | NCT03990233 |
| Bispecific antibodies | ||||||
| HX009 | CD47 and PD-1 | HX009 | II | Metastatic solid tumors | 210 | NCT04886271 |
| PF-07257876 | CD47 and PD-L1 | PF-07257876 | I | Non small-cell lung cancer, head and neck squamous cell carcinoma, ovarian cancer | 90 | NCT04881045 |
| CPO107 (JMP601) | CD47 and CD20 | CPO107 (JMP601) | I | Non-Hodgkin’s lymphoma (CD-20 positive) | 75 | NCT04853329 |
| IBI322 | CD47 and PD-L1 | IBI322 | I | Hematologic malignancies | 182 | NCT04795128 |
| IBI322 | Ia | Metastatic solid tumors | 45 | NCT04338659 | ||
| IBI322 | Ia/Ib | Metastatic solid tumors | 218 | NCT04328831 | ||
| SL-172154 | SIRPα and CD40L | SL-172154 (intravenous) | I | Ovarian cancer | 40 | NCT04406623 |
| SL-172154 (intratumoral) | I | Head and neck or cutaneous squamous cell carcinoma | 18 | NCT04502888 | ||
| TG-1801 | CD47 and CD19 | TG-1801 +/− ubitixumab | Ib | Hematologic malignancies | 60 | NCT04806035 |
| IMM0306 | CD47 and CD20 | IMM0306 | I | Refractory or Relapsed CD20-positive B cell Non-Hodgkin’s Lymphoma | 131 | NCT04746131 |
| Fusion proteins | ||||||
| TTI-622 | CD47 via SIRPαFc (IgG4) structure | TTI-622 + rituximab, PD-1 inhibitor, Proteasome inhibitor regimen or rituximab | Ia/Ib | Lymphoma or myeloma | 156 | NCT03530683 |
| ALX148 | CD47 via SIRPαFc (IgG1) structure | ALX148 + azacitidine | I/II | Myelodysplastic syndrome | 173 | NCT04417517 |
| ALX148 + venetoclax or azacitidine | I/II | Acute myleoid leukemia | 97 | NCT04755244 | ||
| ALX148 | II | Head and neck squamous cell carcinoma | 112 | NCT04675333 | ||
| ALX148 + pembrolizumab | II | Head and neck squamous cell carcinoma | 111 | NCT04675294 | ||
4. Anti-CD47 Antibodies and CD47-Targeting Recombinant Proteins
References
- Mawby, W.J.; Holmes, C.H.; Anstee, D.J.; Spring, F.A.; Tanner, M.J.A. Isolation and Characterization of CD47 Glycoprotein: A Multispanning Membrane Protein Which Is the Same as Integrin-Associated Protein (IAP) and the Ovarian Tumour Marker OA3. Biochem. J. 1994, 304, 525–530.
- Jaiswal, S.; Jamieson, C.H.M.; Pang, W.W.; Park, C.Y.; Chao, M.P.; Majeti, R.; Traver, D.; van Rooijen, N.; Weissman, I.L. CD47 Is Upregulated on Circulating Hematopoietic Stem Cells and Leukemia Cells to Avoid Phagocytosis. Cell 2009, 138, 271–285.
- Oldenborg, P.A.; Zheleznyak, A.; Fang, Y.F.; Lagenaur, C.F.; Gresham, H.D.; Lindberg, F.P. Role of CD47 as a Marker of Self on Red Blood Cells. Science 2000, 288, 2051–2054.
- Burger, P.; Hilarius-Stokman, P.; de Korte, D.; van den Berg, T.K.; van Bruggen, R. CD47 Functions as a Molecular Switch for Erythrocyte Phagocytosis. Blood 2012, 119, 5512–5521.
- Matlung, H.L.; Szilagyi, K.; Barclay, N.A.; van den Berg, T.K. The CD47-SIRPα Signaling Axis as an Innate Immune Checkpoint in Cancer. Immunol. Rev. 2017, 276, 145–164.
- Wu, L.; Yu, G.-T.; Deng, W.-W.; Mao, L.; Yang, L.-L.; Ma, S.-R.; Bu, L.-L.; Kulkarni, A.B.; Zhang, W.-F.; Zhang, L.; et al. Anti-CD47 Treatment Enhances Anti-Tumor T-Cell Immunity and Improves Immunosuppressive Environment in Head and Neck Squamous Cell Carcinoma. OncoImmunology 2018, 7, e1397248.
- Chao, M.P.; Tang, C.; Pachynski, R.K.; Chin, R.; Majeti, R.; Weissman, I.L. Extranodal Dissemination of Non-Hodgkin Lymphoma Requires CD47 and Is Inhibited by Anti-CD47 Antibody Therapy. Blood 2011, 118, 4890–4901.
- Willingham, S.B.; Volkmer, J.-P.; Gentles, A.J.; Sahoo, D.; Dalerba, P.; Mitra, S.S.; Wang, J.; Contreras-Trujillo, H.; Martin, R.; Cohen, J.D.; et al. The CD47-Signal Regulatory Protein Alpha (SIRPa) Interaction Is a Therapeutic Target for Human Solid Tumors. Proc. Natl. Acad. Sci. USA 2012, 109, 6662–6667.
- Molecular Pathways: Activating T Cells after Cancer Cell Phagocytosis from Blockade of CD47 “Don’t Eat Me” Signals|Clinical Cancer Research. Available online: https://clincancerres.aacrjournals.org/content/21/16/3597 (accessed on 24 August 2021).
- Weiskopf, K.; Jahchan, N.S.; Schnorr, P.J.; Cristea, S.; Ring, A.M.; Maute, R.L.; Volkmer, A.K.; Volkmer, J.-P.; Liu, J.; Lim, J.S.; et al. CD47-Blocking Immunotherapies Stimulate Macrophage-Mediated Destruction of Small-Cell Lung Cancer. J. Clin. Investig. 2016, 126, 2610–2620.
- Edris, B.; Weiskopf, K.; Volkmer, A.K.; Volkmer, J.-P.; Willingham, S.B.; Contreras-Trujillo, H.; Liu, J.; Majeti, R.; West, R.B.; Fletcher, J.A.; et al. Antibody Therapy Targeting the CD47 Protein Is Effective in a Model of Aggressive Metastatic Leiomyosarcoma. Proc. Natl. Acad. Sci. USA 2012, 109, 6656–6661.
- Majeti, R.; Chao, M.P.; Alizadeh, A.A.; Pang, W.W.; Jaiswal, S.; Gibbs, K.D.; van Rooijen, N.; Weissman, I.L. CD47 Is an Adverse Prognostic Factor and Therapeutic Antibody Target on Human Acute Myeloid Leukemia Stem Cells. Cell 2009, 138, 286–299.
- Xu, L.; Wang, S.; Li, J.; Li, B. CD47/SIRPα Blocking Enhances CD19/CD3-Bispecific T Cell Engager Antibody-Mediated Lysis of B Cell Malignancies. Biochem. Biophys. Res. Commun. 2019, 509, 739–745.
- Yoshida, K.; Tsujimoto, H.; Matsumura, K.; Kinoshita, M.; Takahata, R.; Matsumoto, Y.; Hiraki, S.; Ono, S.; Seki, S.; Yamamoto, J.; et al. CD47 Is an Adverse Prognostic Factor and a Therapeutic Target in Gastric Cancer. Cancer Med. 2015, 4, 1322–1333.
- Xiao, Z.; Chung, H.; Banan, B.; Manning, P.T.; Ott, K.C.; Lin, S.; Capoccia, B.J.; Subramanian, V.; Hiebsch, R.R.; Upadhya, G.A.; et al. Antibody Mediated Therapy Targeting CD47 Inhibits Tumor Progression of Hepatocellular Carcinoma. Cancer Lett. 2015, 360, 302–309.
- Ring, N.G.; Herndler-Brandstetter, D.; Weiskopf, K.; Shan, L.; Volkmer, J.-P.; George, B.M.; Lietzenmayer, M.; McKenna, K.M.; Naik, T.J.; McCarty, A.; et al. Anti-SIRPα Antibody Immunotherapy Enhances Neutrophil and Macrophage Antitumor Activity. Proc. Natl. Acad. Sci. USA 2017, 114, E10578–E10585.
- Vaeteewoottacharn, K.; Kariya, R.; Pothipan, P.; Fujikawa, S.; Pairojkul, C.; Waraasawapati, S.; Kuwahara, K.; Wongkham, C.; Wongkham, S.; Okada, S. Attenuation of CD47-SIRPα Signal in Cholangiocarcinoma Potentiates Tumor-Associated Macrophage-Mediated Phagocytosis and Suppresses Intrahepatic Metastasis. Transl. Oncol. 2018, 12, 217–225.
- Solinas, G.; Germano, G.; Mantovani, A.; Allavena, P. Tumor-Associated Macrophages (TAM) as Major Players of the Cancer-Related Inflammation. J. Leukoc. Biol. 2009, 86, 1065–1073.
- Gordon, S. Alternative Activation of Macrophages. Nat. Rev. Immunol. 2003, 3, 23–35.
- Mantovani, A.; Marchesi, F.; Malesci, A.; Laghi, L.; Allavena, P. Tumour-Associated Macrophages as Treatment Targets in Oncology. Nat. Rev. Clin. Oncol. 2017, 14, 399–416.
- Zhang, M.; Hutter, G.; Kahn, S.A.; Azad, T.D.; Gholamin, S.; Xu, C.Y.; Liu, J.; Achrol, A.S.; Richard, C.; Sommerkamp, P.; et al. Anti-CD47 Treatment Stimulates Phagocytosis of Glioblastoma by M1 and M2 Polarized Macrophages and Promotes M1 Polarized Macrophages In Vivo. PLoS ONE 2016, 11, e0153550.
- Nath, P.R.; Pal-Nath, D.; Mandal, A.; Cam, M.C.; Schwartz, A.L.; Roberts, D.D. Natural Killer Cell Recruitment and Activation Are Regulated by CD47 Expression in the Tumor Microenvironment. Cancer Immunol. Res. 2019, 7, 1547–1561.
- Deuse, T.; Hu, X.; Agbor-Enoh, S.; Jang, M.K.; Alawi, M.; Saygi, C.; Gravina, A.; Tediashvili, G.; Nguyen, V.Q.; Liu, Y.; et al. The SIRPα–CD47 Immune Checkpoint in NK Cells. J. Exp. Med. 2021, 218, e20200839.
- Kim, M.J.; Lee, J.-C.; Lee, J.-J.; Kim, S.; Lee, S.G.; Park, S.-W.; Sung, M.W.; Heo, D.S. Association of CD47 with Natural Killer Cell-Mediated Cytotoxicity of Head-and-Neck Squamous Cell Carcinoma Lines. Tumor Biol. 2008, 29, 28–34.
- Veillette, A.; Chen, J. SIRPα–CD47 Immune Checkpoint Blockade in Anticancer Therapy. Trends Immunol. 2018, 39, 173–184.
- Kikuchi, Y.; Uno, S.; Kinoshita, Y.; Yoshimura, Y.; Iida, S.-I.; Wakahara, Y.; Tsuchiya, M.; Yamada-Okabe, H.; Fukushima, N. Apoptosis Inducing Bivalent Single-Chain Antibody Fragments against CD47 Showed Antitumor Potency for Multiple Myeloma. Leuk Res. 2005, 29, 445–450.
- Boukhari, A.; Alhosin, M.; Bronner, C.; Sagini, K.; Truchot, C.; Sick, E.; Schini-Kerth, V.B.; André, P.; Mély, Y.; Mousli, M.; et al. CD47 Activation-Induced UHRF1 over-Expression Is Associated with Silencing of Tumor Suppressor Gene P16INK4A in Glioblastoma Cells. Anticancer Res. 2015, 35, 149–157.
- Uluçkan, O.; Becker, S.N.; Deng, H.; Zou, W.; Prior, J.L.; Piwnica-Worms, D.; Frazier, W.A.; Weilbaecher, K.N. CD47 Regulates Bone Mass and Tumor Metastasis to Bone. Cancer Res. 2009, 69, 3196–3204.
- Huang, T.; Sun, L.; Yuan, X.; Qiu, H. Thrombospondin-1 Is a Multifaceted Player in Tumor Progression. Oncotarget 2017, 8, 84546–84558.
- Byrne, G.J.; Hayden, K.E.; McDowell, G.; Lang, H.; Kirwan, C.C.; Tetlow, L.; Kumar, S.; Bundred, N.J. Angiogenic Characteristics of Circulating and Tumoural Thrombospondin-1 in Breast Cancer. Int. J. Oncol. 2007, 31, 1127–1132.
- Borsotti, P.; Ghilardi, C.; Ostano, P.; Silini, A.; Dossi, R.; Pinessi, D.; Foglieni, C.; Scatolini, M.; Lacal, P.M.; Ferrari, R.; et al. Thrombospondin-1 Is Part of a Slug-Independent Motility and Metastatic Program in Cutaneous Melanoma, in Association with VEGFR-1 and FGF-2. Pigment. Cell Melanoma Res. 2015, 28, 73–81.
- Kamijo, H.; Miyagaki, T.; Takahashi-Shishido, N.; Nakajima, R.; Oka, T.; Suga, H.; Sugaya, M.; Sato, S. Thrombospondin-1 Promotes Tumor Progression in Cutaneous T-Cell Lymphoma via CD47. Leukemia 2020, 34, 845–856.
- Liu, X.; Pu, Y.; Cron, K.; Deng, L.; Kline, J.; Frazier, W.A.; Xu, H.; Peng, H.; Fu, Y.-X.; Xu, M.M. CD47 Blockade Triggers T Cell-Mediated Destruction of Immunogenic Tumors. Nat. Med. 2015, 21, 1209–1215.
- Chen, A.; Harrabi, O.; Fong, A.P.; Ruffner, K.L.; Forgie, A.J.; Sim, J.; Randolph, S.S.; Wan, H.; Pons, J.; Kuo, T.C. ALX148 Enhances the Depth and Durability of Response to Multiple AML Therapies. Blood 2020, 136, 15–16.
- Tseng, D.; Volkmer, J.-P.; Willingham, S.B.; Contreras-Trujillo, H.; Fathman, J.W.; Fernhoff, N.B.; Seita, J.; Inlay, M.A.; Weiskopf, K.; Miyanishi, M.; et al. Anti-CD47 Antibody-Mediated Phagocytosis of Cancer by Macrophages Primes an Effective Antitumor T-Cell Response. Proc. Natl. Acad. Sci. USA 2013, 110, 11103–11108.
- Yang, H.; Shao, R.; Huang, H.; Wang, X.; Rong, Z.; Lin, Y. Engineering Macrophages to Phagocytose Cancer Cells by Blocking the CD47/SIRPɑ Axis. Cancer Med. 2019, 8, 4245–4253.
- Gauttier, V.; Pengam, S.; Durand, J.; Biteau, K.; Mary, C.; Morello, A.; Néel, M.; Porto, G.; Teppaz, G.; Thepenier, V.; et al. Selective SIRPα Blockade Reverses Tumor T Cell Exclusion and Overcomes Cancer Immunotherapy Resistance. J. Clin. Investig. 2020, 130, 6109–6123.
- Soto-Pantoja, D.R.; Terabe, M.; Ghosh, A.; Ridnour, L.A.; DeGraff, W.G.; Wink, D.A.; Berzofsky, J.A.; Roberts, D.D. CD47 in the Tumor Microenvironment Limits Cooperation between Antitumor T-Cell Immunity and Radiotherapy. Cancer Res. 2014, 74, 6771–6783.
- Von Roemeling, C.A.; Wang, Y.; Qie, Y.; Yuan, H.; Zhao, H.; Liu, X.; Yang, Z.; Yang, M.; Deng, W.; Bruno, K.A.; et al. Therapeutic Modulation of Phagocytosis in Glioblastoma Can Activate Both Innate and Adaptive Antitumour Immunity. Nat. Commun. 2020, 11, 1508.
- Martinez-Torres, A.-C.; Quiney, C.; Attout, T.; Boullet, H.; Herbi, L.; Vela, L.; Barbier, S.; Chateau, D.; Chapiro, E.; Nguyen-Khac, F.; et al. CD47 Agonist Peptides Induce Programmed Cell Death in Refractory Chronic Lymphocytic Leukemia B Cells via PLCγ1 Activation: Evidence from Mice and Humans. PLoS Med. 2015, 12, e1001796.
- Tao, H.; Qian, P.; Wang, F.; Yu, H.; Guo, Y. Targeting CD47 Enhances the Efficacy of Anti-PD-1 and CTLA-4 in an Esophageal Squamous Cell Cancer Preclinical Model. Oncol. Res. 2017, 25, 1579–1587.
- Nagahara, M.; Mimori, K.; Kataoka, A.; Ishii, H.; Tanaka, F.; Nakagawa, T.; Sato, T.; Ono, S.; Sugihara, K.; Mori, M. Correlated Expression of CD47 and SIRPA in Bone Marrow and in Peripheral Blood Predicts Recurrence in Breast Cancer Patients. Clin. Cancer Res. 2010, 16, 4625–4635.
- Chao, M.P.; Alizadeh, A.A.; Tang, C.; Myklebust, J.H.; Varghese, B.; Gill, S.; Jan, M.; Cha, A.C.; Chan, C.K.; Tan, B.T.; et al. Anti-CD47 Antibody Synergizes with Rituximab to Promote Phagocytosis and Eradicate Non-Hodgkin Lymphoma. Cell 2010, 142, 699–713.
- Galli, S.; Zlobec, I.; Schürch, C.; Perren, A.; Ochsenbein, A.F.; Banz, Y. CD47 Protein Expression in Acute Myeloid Leukemia: A Tissue Microarray-Based Analysis. Leuk Res. 2015, 39, 749–756.
- Fu, W.; Li, J.; Zhang, W.; Li, P. High Expression of CD47 Predicts Adverse Prognosis in Chinese Patients and Suppresses Immune Response in Melanoma. Biomed. Pharmacother. 2017, 93, 1190–1196.
- Overexpression of CD47 Predicts Poor Prognosis and Promotes Cancer Cell Invasion in High-Grade Serous Ovarian Carcinoma. Available online: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5489890/ (accessed on 24 August 2021).
- Upton, R.; Banuelos, A.; Feng, D.; Biswas, T.; Kao, K.; McKenna, K.; Willingham, S.; Ho, P.Y.; Rosental, B.; Tal, M.C.; et al. Combining CD47 Blockade with Trastuzumab Eliminates HER2-Positive Breast Cancer Cells and Overcomes Trastuzumab Tolerance. Proc. Natl. Acad. Sci. USA 2021, 118, e2026849118.
- Briere, D.; Sudhakar, N.; Woods, D.M.; Hallin, J.; Engstrom, L.D.; Aranda, R.; Chiang, H.; Sodré, A.L.; Olson, P.; Weber, J.S.; et al. The Class I/IV HDAC Inhibitor Mocetinostat Increases Tumor Antigen Presentation, Decreases Immune Suppressive Cell Types and Augments Checkpoint Inhibitor Therapy. Cancer Immunol. Immunother. 2018, 67, 381–392.
- Orillion, A.; Hashimoto, A.; Damayanti, N.; Shen, L.; Adelaiye-Ogala, R.; Arisa, S.; Chintala, S.; Ordentlich, P.; Kao, C.; Elzey, B.; et al. Entinostat Neutralizes Myeloid-Derived Suppressor Cells and Enhances the Antitumor Effect of PD-1 Inhibition in Murine Models of Lung and Renal Cell Carcinoma. Clin. Cancer Res. 2017, 23, 5187–5201.
- Catani, L.; Sollazzo, D.; Ricci, F.; Polverelli, N.; Palandri, F.; Baccarani, M.; Vianelli, N.; Lemoli, R.M. The CD47 Pathway Is Deregulated in Human Immune Thrombocytopenia. Exp. Hematol. 2011, 39, 486–494.
- Khandelwal, S.; van Rooijen, N.; Saxena, R.K. Reduced Expression of CD47 during Murine Red Blood Cell (RBC) Senescence and Its Role in RBC Clearance from the Circulation. Transfusion 2007, 47, 1725–1732.
- Takimoto, C.H.; Chao, M.P.; Gibbs, C.; McCamish, M.A.; Liu, J.; Chen, J.Y.; Majeti, R.; Weissman, I.L. The Macrophage ‘Do Not Eat Me’ Signal, CD47, Is a Clinically Validated Cancer Immunotherapy Target. Ann. Oncol. 2019, 30, 486–489.
- Chao, M.P.; Majeti, R.; Weissman, I.L. Programmed Cell Removal: A New Obstacle in the Road to Developing Cancer. Nat. Rev. Cancer 2012, 12, 58–67.
- Zhang, W.; Huang, Q.; Xiao, W.; Zhao, Y.; Pi, J.; Xu, H.; Zhao, H.; Xu, J.; Evans, C.E.; Jin, H. Advances in Anti-Tumor Treatments Targeting the CD47/SIRPα Axis. Front. Immunol. 2020, 11, 18.
- Liu, J.; Wang, L.; Zhao, F.; Tseng, S.; Narayanan, C.; Shura, L.; Willingham, S.; Howard, M.; Prohaska, S.; Volkmer, J.; et al. Pre-Clinical Development of a Humanized Anti-CD47 Antibody with Anti-Cancer Therapeutic Potential. PLoS ONE 2015, 10, e0137345.
- Gholamin, S.; Mitra, S.S.; Feroze, A.H.; Liu, J.; Kahn, S.A.; Zhang, M.; Esparza, R.; Richard, C.; Ramaswamy, V.; Remke, M.; et al. Disrupting the CD47-SIRPα Anti-Phagocytic Axis by a Humanized Anti-CD47 Antibody Is an Efficacious Treatment for Malignant Pediatric Brain Tumors. Sci. Transl. Med. 2017, 9, eaaf2968.
- Advani, R.; Flinn, I.; Popplewell, L.; Forero, A.; Bartlett, N.L.; Ghosh, N.; Kline, J.; Roschewski, M.; LaCasce, A.; Collins, G.P.; et al. CD47 Blockade by Hu5F9-G4 and Rituximab in Non-Hodgkin’s Lymphoma. N. Engl. J. Med. 2018, 379, 1711–1721.
- Sikic, B.I.; Lakhani, N.; Patnaik, A.; Shah, S.A.; Chandana, S.R.; Rasco, D.; Colevas, A.D.; O’Rourke, T.; Narayanan, S.; Papadopoulos, K.; et al. First-in-Human, First-in-Class Phase I Trial of the Anti-CD47 Antibody Hu5F9-G4 in Patients with Advanced Cancers. J. Clin. Oncol. 2019, 37, 946–953.
- Brierley, C.K.; Staves, J.; Roberts, C.; Johnson, H.; Vyas, P.; Goodnough, L.T.; Murphy, M.F. The Effects of Monoclonal Anti-CD47 on RBCs, Compatibility Testing, and Transfusion Requirements in Refractory Acute Myeloid Leukemia. Transfusion 2019, 59, 2248–2254.
- Lakhani, N.; Orloff, M.; Fu, S.; Liu, Y.; Wang, Y.; Zhou, H.; Lin, K.; Liu, F.; Yan, S.; Patnaik, A. 295 First-in-Human Phase I Trial of IBI188, an Anti-CD47 Targeting Monoclonal Antibody, in Patients with Advanced Solid Tumors and Lymphomas. J. Immunother. Cancer 2020, 8.
- Gan, H.K.; Coward, J.; Mislang, A.R.A.; Cosman, R.; Nagrial, A.; Jin, X.; Li, B.; Wang, Z.M.; Kwek, K.Y.; Xia, D.; et al. Safety of AK117, an Anti-CD47 Monoclonal Antibody, in Patients with Advanced or Metastatic Solid Tumors in a Phase I Study. J. Clin. Oncol. 2021, 39, 2630.




