
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Natália Cruz-Martins | + 4549 word(s) | 4549 | 2021-09-09 05:44:51 | | | |
| 2 | Peter Tang | Meta information modification | 4549 | 2021-09-14 05:15:28 | | |
Video Upload Options
Prostate cancer is a heterogeneous disease, the second deadliest malignancy in men and the most commonly diagnosed cancer among men. Traditional plants have been applied to handle various diseases and to develop new drugs. Medicinal plants are potential sources of natural bioactive compounds that include alkaloids, phenolic compounds, terpenes, and steroids.
1. Introduction
1.1. A Brief Overview on Prostate Cancer
1.2. Prostate Cancer: Main Risk Factors
1.2.1. Non-Modified Risk Factors
|
Risk Group |
Relative Risk of Prostate Cancer |
|---|---|
|
Father and brother had prostate cancer |
9 |
|
≥2 first degree relatives having prostate cancer |
4.39 |
|
Brothers having prostate cancer |
3.14 |
|
First degree relative with prostate cancer at the age of<65 |
2.87 |
|
Second degree relative with prostate cancer |
2.52 |
|
One first degree relative with prostate cancer |
2.48 |
|
Father having prostate cancer |
2.35 |
|
First degree relative with prostate cancer at the age of ≥65 |
1.92 |
1.2.2. Modified Risk Factors
2. Therapeutic Strategies: A Brief Summary
|
Risk Group |
Clinical Stage |
PSA (ng/mL) |
Gleason Score |
Biopsy Criteria |
|---|---|---|---|---|
|
Low |
T1a or T1c |
<10 |
2–6 |
Unilateral or <50% of core involved |
|
Intermediate |
T1b, T1c, or T2a |
<10 |
3 + 4 = 7 |
Bilateral |
|
High |
T1b, T1c, T2b, or T3 |
10–20 |
4 + 3 = 7 |
>50% of core involved or perineural invasion or ductal differentiation |
|
Very high |
T4 |
>20 |
8–10 |
Lymphovascular invasion or neuroendocrine differentiation |
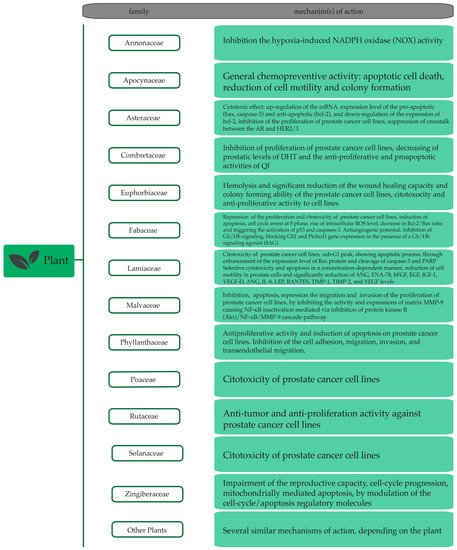
3. Plant Extracts and Plant-Derived Bioactives in Prostate Cancer
3.1. Plant Extracts with Anti-Prostate Cancer Potential
|
Plant Species |
Family |
In Vitro |
In Vivo |
References |
|---|---|---|---|---|
|
Acacia catechu |
Fabaceae |
+ |
- |
[110] |
|
Achillea santolinoides |
Asteraceae |
+ |
- |
[111] |
|
Achillea teretifolia |
Asteraceae |
+ |
- |
[112] |
|
Allium wallichii |
Amaryllidaceae |
+ |
- |
[113] |
|
Aloe perryi |
Xanthorrhoeaceae |
+ |
- |
[114] |
|
Anaxagorea brevipes |
Annonaceae |
+ |
- |
[115] |
|
Angelica gigas |
Apiaceae |
- |
+ |
|
|
Annona muricata |
Annonaceae |
+ |
- |
[118] |
|
Anogeissus latifolia |
Combretaceae |
+ |
- |
[110] |
|
Apocynum venetum |
Apocynaceae |
+ |
- |
[119] |
|
Arachis hypogaea |
Fabaceae |
+ |
- |
[120] |
|
Baliospermum montanum |
Euphorbiaceae |
+ |
+ |
[121] |
|
Berberis libanotica |
Berberidaceae |
+ |
- |
[122] |
|
Byrsonima crassifolia |
Malpighiaceae |
+ |
- |
[123] |
|
Calliandra portoricensis |
Fabaceae |
+ |
- |
[124] |
|
Capsicum chinense |
Solanaceae |
+ |
- |
[123] |
|
Carica papaya |
Caricaceae |
+ |
- |
[125] |
|
Cascabela peruviana |
Apocynaceae |
+ |
- |
[126] |
|
Chenopodium hybridum |
Amaranthaceae |
+ |
- |
[127] |
|
Cnidoscolus chayamansa |
Euphorbiaceae |
+ |
- |
[123] |
|
Cornus mas |
Cornaceae |
+ |
- |
[128] |
|
Costus pulverulentus |
Costaceae |
+ |
- |
[129] |
|
Crataegus Pinnatifida |
Rosaceae |
+ |
- |
[130] |
|
Crocus sativus |
Iridaceae |
+ |
+ |
|
|
Curcuma longa |
Zingiberaceae |
+ |
- |
|
|
Cymbopogon citratus |
Poaceae |
+ |
- |
[135] |
|
Cymbopogon giganteus |
Poaceae |
+ |
- |
[135] |
|
Euphorbia microsciadia |
Euphorbiaceae |
+ |
- |
[111] |
|
Euphorbia szovitsii |
Euphorbiaceae |
+ |
- |
[111] |
|
Eurycoma longifolia |
Simaroubaceae |
+ |
+ |
[136] |
|
Fagara zanthoxyloides |
Rutaceae |
+ |
- |
[137] |
|
Fagopyrum esculentum |
Polygonaceae |
+ |
- |
[138] |
|
Fagopyrum tataricum |
Polygonaceae |
+ |
- |
[138] |
|
Ficus deltoidea var. angustifolia |
Moraceae |
+ |
- |
[139] |
|
Ficus deltoidea var. deltoidea |
Moraceae |
+ |
- |
[139] |
|
Formosa lambsquarters |
Amaranthaceae |
+ |
- |
[138] |
|
Glycine max |
Fabaceae |
+ |
- |
[140] |
|
Glycyrrhiza uralensis |
Fabaceae |
+ |
- |
[141] |
|
Haplophyllum perforatum |
Rutaceae |
+ |
- |
[111] |
|
Helicteres hirsuta |
Malvaceae |
+ |
- |
[142] |
|
Hertia angustifolia |
Asteraceae |
+ |
- |
[111] |
|
Hibiscus sabdariffa |
Malvaceae |
+ |
+ |
[143] |
|
Leucaena leucocephala |
Fabaceae |
+ |
- |
[123] |
|
Lysimachia ciliata |
Primulaceae |
+ |
- |
[144] |
|
Malmea depressa |
Annonaceae |
+ |
- |
[123] |
|
Maytenus royleana |
Celastraceae |
+ |
+ |
[145] |
|
Medicago sativa |
Fabaceae |
+ |
- |
[111] |
|
Melissa officinalis |
Lamiaceae |
+ |
- |
|
|
Mentha arvensis |
Lamiaceae |
+ |
- |
[148] |
|
Mentha spicata |
Lamiaceae |
+ |
- |
[148] |
|
Mentha viridis |
Lamiaceae |
+ |
- |
[148] |
|
Moringa oleifera |
Moringaceae |
+ |
- |
[110] |
|
Nepeta cataria |
Lamiaceae |
+ |
- |
[149] |
|
Nigella sativa |
Ranunculaceae |
+ |
- |
|
|
Oryza sativa |
Poaceae |
+ |
- |
[151] |
|
Paeonia lactiflora |
Paeoniaceae |
+ |
- |
[152]. |
|
Paramignya trimera |
Rutaceae |
+ |
- |
[153] |
|
Phyllanthus amarus |
Phyllanthaceae |
+ |
- |
[154] |
|
Phyllanthus niruri |
Phyllanthaceae |
+ |
- |
[154] |
|
Phyllanthus urinaria |
Phyllanthaceae |
+ |
- |
[154] |
|
Phyllanthus watsonii |
Phyllanthaceae |
+ |
- |
[154] |
|
Plumbago zeylanica |
Plumbaginaceae |
+ |
- |
[155] |
|
Polygonatum sp |
Asparagaceae |
+ |
- |
[156] |
|
Pseudocedrela kotchyi |
Meliaceae |
+ |
- |
[137] |
|
Psidium guajava |
Myrtaceae |
+ |
+ |
|
|
Punica granatum |
Lythraceae |
+ |
+ |
|
|
Quisqualis indica |
Combretaceae |
+ |
+ |
[162] |
|
Remotiflori radix |
Campanulaceae |
+ |
+ |
[163] |
|
Salvia multicaulis Vahl |
Lamiaceae |
+ |
- |
[111] |
|
Salvia trilobal |
Lamiaceae |
+ |
- |
[164] |
|
Sigesbeckia orientalis |
Asteraceae |
+ |
- |
[165] |
|
Sophora alopecuroides |
Fabaceae |
+ |
- |
[111] |
|
Sutherlandia frutescens |
Fabaceae |
+ |
+ |
[166] |
|
Terminalia bellerica |
Combretaceae |
+ |
- |
[110] |
|
Terminalia catappa |
Combretaceae |
+ |
- |
[123] |
|
Urtica dioica |
Urticaceae |
+ |
- |
|
|
Vitis rotundifolia |
Vitaceae |
+ |
- |
[168] |
|
Wedelia chinensis |
Asteraceae |
- |
+ |
|
|
Withania coagulans |
Solanaceae |
- |
+ |
[171] |
|
Xylopia aethiopica |
Annonaceae |
+ |
- |
[172] |
|
Zanthoxyli fructus |
Rutaceae |
+ |
+ |
[173] |
|
Zingiber officinale |
Zingiberaceae |
+ |
+ |
+: Showed in vitro or in vivo antiproliferative effect; -: Not found.
3.2. Plant-Derived Bioactives with Anti-Prostate Cancer Potential
|
Bioactive Compounds |
In Vitro |
In Vivo |
References |
|---|---|---|---|
|
Alkaloids |
|||
|
(−)-Anonaine |
+ |
- |
[176] |
|
(−)-Caaverine |
+ |
- |
[176] |
|
(−)-Nuciferine |
+ |
- |
[176] |
|
6-Hydroxycrinamine |
+ |
- |
[177] |
|
7-Hydroxydehydronuciferine |
+ |
- |
[176] |
|
Capsaicin |
+ |
- |
[178] |
|
Crinamine |
+ |
- |
[177] |
|
Emetine |
+ |
+ |
|
|
Liriodenine |
+ |
- |
[176] |
|
Lycorine |
+ |
+ |
|
|
Matrine |
+ |
- |
[182] |
|
Oxymatrine |
+ |
- |
[182] |
|
Oxysophocarpine |
+ |
- |
[182] |
|
Schisanspheninal A |
+ |
- |
[183] |
|
Sophocarpine |
+ |
- |
[182] |
|
Tetrandrine |
+ |
- |
[184] |
|
Carotenoids |
|||
|
Crocetin |
+ |
- |
[133] |
|
Crocin |
+ |
- |
[132] |
|
Fatty acid |
|||
|
(E)-ethyl 8-methylnon-6-enoate |
+ |
- |
[123] |
|
Phenolic compounds |
|||
|
α-Mangostin |
+ |
+ |
[185]. |
|
γ-Tocopherol |
+ |
- |
[186] |
|
δ-Tocotrienol |
+ |
- |
[186] |
|
(-)-5,7-Difluoroepicatechin-3-O-gallate |
+ |
- |
[187] |
|
(-)-Epicatechin-3-O-gallate |
+ |
- |
[187] |
|
10-Gingerol |
+ |
- |
[175] |
|
6-Gingerol |
+ |
- |
[175] |
|
6-Prenylnaringenin |
+ |
- |
[188] |
|
6-Shogoal |
+ |
- |
[175] |
|
7-o-Galloyl catechin |
+ |
- |
[189] |
|
8-Gingerol |
+ |
- |
[175] |
|
8-Prenylnaringenin |
+ |
- |
[188] |
|
Afzelin |
+ |
- |
[190] |
|
Altholactone |
+ |
- |
[191] |
|
Apigenin |
+ |
[192] |
|
|
Camptothin B |
+ |
- |
[141] |
|
Catechin |
+ |
- |
[189] |
|
Catechin-3-o-gallate |
+ |
- |
[189] |
|
Chlorogenic acid |
+ |
- |
[130] |
|
Chrysin |
+ |
- |
[193] |
|
Cinnamaldehyde |
+ |
- |
[194] |
|
Cornusiin A |
+ |
- |
[141] |
|
Cornusiin H |
+ |
- |
[141] |
|
Curcumin |
+ |
+ |
|
|
Decursin |
+ |
- |
[117] |
|
Decursinol angelate |
+ |
- |
[117] |
|
Dehydrozingerone |
+ |
- |
[199] |
|
Delphinidin |
+ |
+ |
|
|
Ellagic acid |
+ |
+ |
|
|
Eugenol |
+ |
- |
[194] |
|
Fisetin |
+ |
+ |
[204] |
|
Flavokawain A |
+ |
+ |
[205] |
|
Flavopiridol |
+ |
+ |
[206] |
|
Garcinol |
+ |
+ |
|
|
Ginkgetin |
+ |
+ |
[209] |
|
Hesperetin |
+ |
- |
[210] |
|
Hirsutenone |
+ |
- |
[211] |
|
HLBT-100 or HLBT-001 (5,3′-dihydroxy- 6,7,8,4′-tetramethoxyflavanone) |
+ |
- |
[212] |
|
Honokiol |
+ |
- |
[213] |
|
Icarisid II |
+ |
- |
[214] |
|
Isoangustone A |
+ |
- |
|
|
Isovitexin |
+ |
- |
[139] |
|
Juglone |
+ |
- |
[217] |
|
Licoricidin |
+ |
- |
|
|
Magnolol |
+ |
- |
[218] |
|
Mangiferin |
+ |
+ |
|
|
Maysin |
+ |
- |
[221] |
|
Methyl gallate |
+ |
- |
[189] |
|
Osthol |
+ |
- |
|
|
Oxyfadichalcones A |
+ |
- |
[223] |
|
Oxyfadichalcones B |
+ |
- |
[223] |
|
Oxyfadichalcones C |
+ |
- |
[223] |
|
Oxyfadichalcones D |
+ |
- |
[223] |
|
Oxyfadichalcones E |
+ |
- |
[223] |
|
Oxyfadichalcones F |
+ |
- |
[223] |
|
Oxyfadichalcones G |
+ |
- |
[223] |
|
Paeonol |
+ |
+ |
[224] |
|
Peperotetraphin |
+ |
- |
[225] |
|
Physangulatins I |
+ |
- |
[226] |
|
Plumbagin |
+ |
+ |
|
|
Punicalagin |
+ |
- |
[228] |
|
Quercetin |
+ |
+ |
|
|
Resveratrol |
+ |
+ |
|
|
Rutin |
+ |
- |
[235] |
|
Tannic acid |
+ |
- |
[236] |
|
Tricin |
+ |
- |
[237] |
|
Xanthohumol |
+ |
- |
|
|
Protein |
|||
|
Agglutinin |
+ |
+ |
[239] |
|
Diffusa cyclotide 1 |
+ |
- |
[240] |
|
Diffusa cyclotide 2 |
+ |
- |
[240] |
|
Diffusa cyclotide 3 |
+ |
+ |
[240] |
|
Lectin ConBr |
+ |
- |
[241] |
|
Lectin ConM |
+ |
- |
[241] |
|
Lectin DLasiL |
+ |
- |
[241] |
|
Lectin DSclerL |
+ |
- |
[241] |
|
Terpenoids |
|||
|
α-Santalol |
+ |
+ |
[242] |
|
4S,5R,9S,10R-Labdatrien-6,19-olide |
+ |
- |
[243] |
|
(20R)-Dammarane-3β,12β,20,25-tetrol (25-OH-PPD) |
+ |
+ |
[244] |
|
Andrographolide |
+ |
+ |
[245] |
|
Celastrol |
+ |
+ |
[246] |
|
Citral |
+ |
- |
[135] |
|
Diosgenin |
+ |
- |
[247]. |
|
Euphol |
+ |
- |
[248] |
|
Isocuparenal |
+ |
- |
[183] |
|
Jungermannenone A |
+ |
- |
[249] |
|
Jungermannenone B |
+ |
- |
[249] |
|
Muricins M |
+ |
- |
[250] |
|
Muricins N |
+ |
- |
[250] |
|
Nummularic acid |
+ |
- |
[251] |
|
Oenotheralanosterol B |
+ |
- |
[252] |
|
Plectranthoic acid |
+ |
- |
[253] |
|
Sutherlandioside D |
+ |
- |
[166]. |
|
Widdaranal A |
- |
[183] |
|
|
Widdaranal B |
+ |
- |
[183] |
|
Widdarol peroxide |
+ |
- |
[183] |
|
Withaferin A |
+ |
- |
[254] |
-, no effect observed; +, positive effect.
4. Evidence from Clinical Studies
|
Phytochemicals/Formulae |
Bioactive Effect |
Reference |
|---|---|---|
|
Danshen (Salvia miltiorrhiza) |
Protective effects; Improved survival (5–10%) |
[256] |
|
TCM formulae (Chai-Hu-Jia-Long-Gu-Mu-Li-Tang) |
Improved survival |
[257] |
|
Pomegranate juice |
Extension of PSA doubling time, with no adverse effects |
|
|
Pomegranate, green tea, broccoli, turmeric |
Decreased PSA levels |
[261] |
|
Resveratrol |
Decreased the circulating levels of androgen precursors |
[262] |
|
Extension of PSA doubling time, with no adverse effects |
[263] |
|
|
PC-SPEC |
Decreased PSA levels |
[264] |
References
- Etemadi, A.; Sadjadi, A.; Semnani, S.; Nouraie, S.M.; Khademi, H.; Bahadori, M. Cancer registry in Iran: A brief overview. Arch. Iran. Med. 2008, 11, 577–580.
- Casey, S.C.; Amedei, A.; Aquilano, K.; Azmi, A.S.; Benencia, F.; Bhakta, D.; Bilsland, A.E.; Boosani, C.S.; Chen, S.; Ciriolo, M.R.; et al. Cancer prevention and therapy through the modulation of the tumor microenvironment. Semin. Cancer Biol. 2015, 35, S199–S223.
- Siegel, R.L.; Fedewa, S.A.; Miller, K.D.; Goding-Sauer, A.; Pinheiro, P.S.; Martinez-Tyson, D.; Jemal, A. Cancer statistics for hispanics/latinos, 2015. CA Cancer J. Clin. 2015, 65, 457–480.
- Shokoohinia, Y.; Jafari, F.; Mohammadi, Z.; Bazvandi, L.; Hosseinzadeh, L.; Chow, N.; Bhattacharyya, P.; Farzaei, M.H.; Farooqi, A.A.; Nabavi, S.M.; et al. Potential anticancer properties of osthol: A comprehensive mechanistic review. Nutrients 2018, 10, 36.
- Sharma, P.; McClees, S.F.; Afaq, F. Pomegranate for prevention and treatment of cancer: An update. Molecules 2017, 22, 177.
- Novio, S.; Cartea, M.E.; Soengas, P.; Freire-Garabal, M.; Nunez-Iglesias, M.J. Effects of Brassicaceae isothiocyanates on prostate cancer. Molecules 2016, 21, 626.
- Torre, L.A.; Siegel, R.L.; Ward, E.M.; Jemal, A. Global cancer incidence and mortality rates and trends—An update. Cancer Epidemiol. Prev. Biomark. 2015, 25, 16–27.
- Giovannucci, E.; Harlan, D.M.; Archer, M.C.; Bergenstal, R.M.; Gapstur, S.M.; Habel, L.A.; Pollak, M.; Regensteiner, J.G.; Yee, D. Diabetes and cancer: A consensus report. CA Cancer J. Clin. 2010, 60, 207–221.
- Ferlay, J.; Soerjomataram, I.; Ervik, M.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.; Forman, D.; Bray, F. Globocan 2012 v1.0, Cancer Incidence and Mortality Worldwide: Iarc Cancerbase No. 11; International Agency for Research on Cancer: Lyon, France, 2015.
- Attard, G.; Parker, C.; Eeles, R.A.; Schroder, F.; Tomlins, S.A.; Tannock, I.; Drake, C.G.; de Bono, J.S. Prostate cancer. Lancet 2016, 387, 70–82.
- Klotz, L.; Vesprini, D.; Sethukavalan, P.; Jethava, V.; Zhang, L.; Jain, S.; Yamamoto, T.; Mamedov, A.; Loblaw, A. Long-term follow-up of a large active surveillance cohort of patients with prostate cancer. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2015, 33, 272–277.
- Abedi, A.-R.; Fallah-Karkan, M.; Allameh, F.; Ranjbar, A.; Shadmehr, A. Incidental prostate cancer: A 10-year review of a tertiary center, Tehran, Iran. Res. Rep. Urol. 2018, 10, 1–6.
- Daniyal, M.; Siddiqui, Z.A.; Akram, M.; Asif, H.; Sultana, S.; Khan, A. Epidemiology, etiology, diagnosis and treatment of prostate cancer. Asian Pac. J. Cancer Prev. 2014, 15, 9575–9578.
- Pernar, C.H.; Ebot, E.M.; Wilson, K.M.; Mucci, L.A. The epidemiology of prostate cancer. Cold Spring Harb. Perspect. Med. 2018, 3, a030361.
- Barve, A.; Khor, T.O.; Hao, X.; Keum, Y.S.; Yang, C.S.; Reddy, B.; Kong, A.N. Murine prostate cancer inhibition by dietary phytochemicals—Curcumin and phenyethylisothiocyanate. Pharm. Res. 2008, 25, 2181–2189.
- Dunn, M.W.; Kazer, M.W. Prostate cancer overview. Semin. Oncol. Nurs. 2011, 27, 241–250.
- Ferlay, J.; Soerjomataram, I.; Dikshit, R.; Eser, S.; Mathers, C.; Rebelo, M.; Parkin, D.M.; Forman, D.; Bray, F. Cancer incidence and mortality worldwide: Sources, methods and major patterns in globocan 2012. Int. J. Cancer 2015, 136, E359–E386.
- Bashir, M.N. Epidemiology of prostate cancer. Asian Pac. J. Cancer Prev. 2015, 16, 5137–5141.
- American Cancer Society. Key Statistics for Prostate Cancer; American Cancer Society: Atlanta, GA, USA, 2018.
- Packer, J.R.; Maitland, N.J. The molecular and cellular origin of human prostate cancer. Biochim. Biophys. Acta 2016, 1863, 1238–1260.
- Mills, P.K.; Beeson, W.L.; Phillips, R.L.; Fraser, G.E. Cohort study of diet, lifestyle, and prostate cancer in adventist men. Cancer 1989, 64, 598–604.
- Chan, J.M.; Stampfer, M.J.; Giovannucci, E.L. What causes prostate cancer? A brief summary of the epidemiology. Semin. Cancer Biol. 1998, 8, 263–273.
- Pandey, M.K.; Gupta, S.C.; Nabavizadeh, A.; Aggarwal, B.B. Regulation of cell signaling pathways by dietary agents for cancer prevention and treatment. Semin. Cancer Biol. 2017, 46, 158–181.
- Mantovani, A.; Allavena, P.; Sica, A.; Balkwill, F. Cancer-related inflammation. Nature 2008, 454, 436–444.
- Hamilton, W.; Sharp, D. Symptomatic diagnosis of prostate cancer in primary care: A structured review. Br. J. Gen. Pr. 2004, 54, 617–621.
- Young, S.-M.; Bansal, P.; Vella, E.T.; Finelli, A.; Levitt, C.; Loblaw, A. Systematic review of clinical features of suspected prostate cancer in primary care. Can. Fam. Physician 2015, 61, e26–e35.
- Quinlan, M.; O’Daly, B.; O’Brien, M.; Gardner, S.; Lennon, G.; Mulvin, D.; Quinlan, D. The value of appropriate assessment prior to specialist referral in men with prostatic symptoms. Ir. J. Med Sci. 2009, 178, 281–285.
- Nam, R.K.; Kattan, M.W.; Chin, J.L.; Trachtenberg, J.; Singal, R.; Rendon, R.; Klotz, L.H.; Sugar, L.; Sherman, C.; Izawa, J. Prospective multi-institutional study evaluating the performance of prostate cancer risk calculators. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2011, 29, 2959–2964.
- Brown, M.L.; Potosky, A.L.; Thompson, G.B.; Kessler, L.K. The knowledge and use of screening tests for colorectal and prostate cancer: Data from the 1987 national health interview survey. Prev. Med. 1990, 19, 562–574.
- Barry, M.J. Screening for Prostate Cancer—The Controversy That Refuses to Die; Massachusetts Medical Society: Waltham, MA, USA, 2009.
- Siegel, R.; Ma, J.; Zou, Z.; Jemal, A. Cancer statistics, 2014. CA Cancer J. Clin. 2014, 64, 9–29.
- Center, M.M.; Jemal, A.; Lortet-Tieulent, J.; Ward, E.; Ferlay, J.; Brawley, O.; Bray, F. International variation in prostate cancer incidence and mortality rates. Eur. Urol. 2012, 61, 1079–1092.
- Thompson, I.M.; Pauler, D.K.; Goodman, P.J.; Tangen, C.M.; Lucia, M.S.; Parnes, H.L.; Minasian, L.M.; Ford, L.G.; Lippman, S.M.; Crawford, E.D. Prevalence of prostate cancer among men with a prostate-specific antigen level ≤ 4.0 ng per milliliter. N. Engl. J. Med. 2004, 350, 2239–2246.
- Ghai, S.; Haider, M.A. Multiparametric-mri in diagnosis of prostate cancer. Indian J. Urol. Iju J. Urol. Soc. India 2015, 31, 194.
- Cook, G.J.; Azad, G.; Padhani, A.R. Bone imaging in prostate cancer: The evolving roles of nuclear medicine and radiology. Clin. Transl. Imaging 2016, 4, 439–447.
- Zheng, X.-Y.; Zhang, P.; Xie, L.-P.; You, Q.-H.; Cai, B.-S.; Qin, J. Prostate-specific antigen velocity (PSAV) and PSAV per initial volume (PSAVD) for early detection of prostate cancer in Chinese men. Asian Pac. J. Cancer Prev. 2012, 13, 5529–5533.
- Hayes, J.H.; Barry, M.J. Screening for prostate cancer with the prostate-specific antigen test: A review of current evidence. JAMA 2014, 311, 1143–1149.
- Eggener, S.E.; Cifu, A.S.; Nabhan, C. Prostate cancer screening. JAMA 2015, 314, 825–826.
- Prensner, J.R.; Rubin, M.A.; Wei, J.T.; Chinnaiyan, A.M. Beyond psa: The next generation of prostate cancer biomarkers. Sci. Transl. Med. 2012, 4, rv123–rv127.
- Cuzick, J.; Thorat, M.A.; Andriole, G.; Brawley, O.W.; Brown, P.H.; Culig, Z.; Eeles, R.A.; Ford, L.G.; Hamdy, F.C.; Holmberg, L. Prevention and early detection of prostate cancer. Lancet Oncol. 2014, 15, e484–e492.
- Jahn, J.L.; Giovannucci, E.L.; Stampfer, M.J. The high prevalence of undiagnosed prostate cancer at autopsy: Implications for epidemiology and treatment of prostate cancer in the prostate-specific antigen-era. Int. J. Cancer 2015, 137, 2795–2802.
- Chan, J.M.; Giovannucci, E.L. Vegetables, fruits, associated micronutrients, and risk of prostate cancer. Epidemiol. Rev. 2001, 23, 82–86.
- Bashir, M.N.; Ahmad, M.R.; Malik, A. Risk factors of prostate cancer: A case-control study in Faisalabad, Pakistan. Asian Pac. J. Cancer Prev. 2014, 15, 10237–10240.
- Howlader, N.; Noone, A.; Krapcho, M.; Miller, D.; Bishop, K.; Altekruse, S.; Kosary, C.; Yu, M.; Ruhl, J.; Tatalovich, Z. Seer Cancer Statistics Review. 1975–2013. National Cancer Institute: Bethesda, MD, USA. Available online: https://seer.cancer.gov/archive/csr/1975_2013/ (accessed on 10 September 2018).
- Goggins, W.B.; Wong, G. Cancer among asian indians/pakistanis living in the united states: Low incidence and generally above average survival. Cancer Causes Control. 2009, 20, 635–643.
- Hemminki, K.; Ankerst, D.P.; Sundquist, J.; Mousavi, S.M. Prostate cancer incidence and survival in immigrants to Sweden. World J. Urol. 2013, 31, 1483–1488.
- Kiciński, M.; Vangronsveld, J.; Nawrot, T.S. An epidemiological reappraisal of the familial aggregation of prostate cancer: A meta-analysis. PLoS ONE 2011, 6, e27130.
- Eeles, R.A.; Al Olama, A.A.; Benlloch, S.; Saunders, E.J.; Leongamornlert, D.A.; Tymrakiewicz, M.; Ghoussaini, M.; Luccarini, C.; Dennis, J.; Jugurnauth-Little, S. Identification of 23 new prostate cancer susceptibility loci using the icogs custom genotyping array. Nat. Genet. 2013, 45, 385.
- Hoffmann, T.J.; Van Den Eeden, S.K.; Sakoda, L.C.; Jorgenson, E.; Habel, L.A.; Graff, R.E.; Passarelli, M.N.; Cario, C.L.; Emami, N.C.; Chao, C.R. A large multi-ethnic genome-wide association study of prostate cancer identifies novel risk variants and substantial ethnic differences. Cancer Discov. 2015, 5, 878–891.
- Hemminki, K.; Czene, K. Attributable risks of familial cancer from the family-cancer database. Cancer Epidemiol. Prev. Biomark. 2002, 11, 1638–1644.
- Möller, E.; Wilson, K.M.; Batista, J.L.; Mucci, L.A.; Bälter, K.; Giovannucci, E. Body size across the life course and prostate cancer in the health professionals follow-up study. Int. J. Cancer 2016, 138, 853–865.
- Zuccolo, L.; Harris, R.; Gunnell, D.; Oliver, S.; Lane, J.A.; Davis, M.; Donovan, J.; Neal, D.; Hamdy, F.; Beynon, R. Height and prostate cancer risk: A large nested case-control study (protect) and meta-analysis. Cancer Epidemiol. Prev. Biomark. 2008, 17, 2325–2336.
- Anuurad, E.; Shiwaku, K.; Nogi, A.; Kitajima, K.; Enkhmaa, B.; Shimono, K.; Yamane, Y. The new bmi criteria for asians by the regional office for the western pacific region of who are suitable for screening of overweight to prevent metabolic syndrome in elder Japanese workers. J. Occup. Health 2003, 45, 335–343.
- Cao, Y.; Ma, J. Body-mass index, prostate cancer-specific mortality and biochemical recurrence: A systematic review and meta-analysis. Cancer Prev. Res. 2011, 4, 486–501.
- Ma, J.; Li, H.; Giovannucci, E.; Mucci, L.; Qiu, W.; Nguyen, P.L.; Gaziano, J.M.; Pollak, M.; Stampfer, M.J. Prediagnostic body-mass index, plasma c-peptide concentration, and prostate cancer-specific mortality in men with prostate cancer: A long-term survival analysis. Lancet Oncol. 2008, 9, 1039–1047.
- Joshu, C.E.; Mondul, A.M.; Menke, A.; Meinhold, C.L.; Han, M.; Humphreys, E.; Freedland, S.J.; Walsh, P.C.; Platz, E.A. Weight gain is associated with an increased risk of prostate cancer recurrence after prostatectomy in the PSA era. Cancer Prev. Res. 2011, 4, 544–551.
- World Health Organization. Global Status Report on Alcohol and Health; World Health Organization: Geneva, Switzerland, 2014.
- Kenfield, S.A.; Stampfer, M.J.; Chan, J.M.; Giovannucci, E. Smoking and prostate cancer survival and recurrence. JAMA 2011, 305, 2548–2555.
- Richman, E.L.; Kenfield, S.A.; Stampfer, M.J.; Paciorek, A.; Carroll, P.R.; Chan, J.M. Physical activity after diagnosis and risk of prostate cancer progression: Data from the cancer of the prostate strategic urologic research endeavor. Cancer Res. 2011, 71, 3889–3895.
- Loprinzi, P.D.; Kohli, M. Effect of Physical Activity and Sedentary Behavior on Serum Prostate-Specific Antigen Concentrations: Results from the National Health and Nutrition Examination Survey (NHANES), 2003–2006, Mayo Clinic Proceedings; Elsevier: Amsterdam, The Netherlands, 2013; pp. 11–21.
- Holt, S.K.; Kwon, E.M.; Koopmeiners, J.S.; Lin, D.W.; Feng, Z.; Ostrander, E.A.; Peters, U.; Stanford, J.L. Vitamin d pathway gene variants and prostate cancer prognosis. Prostate 2010, 70, 1448–1460.
- Kristal, A.R.; Arnold, K.B.; Neuhouser, M.L.; Goodman, P.; Platz, E.A.; Albanes, D.; Thompson, I.M. Diet, supplement use, and prostate cancer risk: Results from the prostate cancer prevention trial. Am. J. Epidemiol. 2010, 172, 566–577.
- Mahmood, S.; Qasmi, G.; Ahmed, A.; Kokab, F.; Zahid, M.F.; Afridi, M.I.; Razzaq, A. Lifestyle factors associated with the risk of prostate cancer among Pakistani men. J. Ayub Med. Coll. Abbottabad 2012, 24, 122–126.
- Butler, L.M.; Wong, A.S.; Koh, W.-P.; Wang, R.; Yuan, J.-M.; Mimi, C.Y. Calcium intake increases risk of prostate cancer among Singapore Chinese. Cancer Res. 2010, 70, 4941–4948.
- De Martel, C.; Ferlay, J.; Franceschi, S.; Vignat, J.; Bray, F.; Forman, D.; Plummer, M. Global burden of cancers attributable to infections in 2008: A review and synthetic analysis. Lancet Oncol. 2012, 13, 607–615.
- Sutcliffe, S.; Platz, E.A. Inflammation and prostate cancer: A focus on infections. Curr. Urol. Rep. 2008, 9, 243.
- Sutcliffe, S.; Neace, C.; Magnuson, N.S.; Reeves, R.; Alderete, J. Trichomonosis, a common curable sti, and prostate carcinogenesis—a proposed molecular mechanism. PLoS Pathog. 2012, 8, e1002801.
- Meyer, T.E.; Coker, A.L.; Sanderson, M.; Symanski, E. A case–control study of farming and prostate cancer in African-American and Caucasian men. Occup. Environ. Med. 2007, 64, 155–160.
- Nair-Shalliker, V.; Smith, D.P.; Egger, S.; Hughes, A.M.; Kaldor, J.M.; Clements, M.; Kricker, A.; Armstrong, B.K. Sun exposure may increase risk of prostate cancer in the high UV environment of new south wales, Australia: A case–control study. Int. J. Cancer 2012, 131, E726–E732.
- Myles, P.; Evans, S.; Lophatananon, A.; Dimitropoulou, P.; Easton, D.; Key, T.; Pocock, R.; Dearnaley, D.; Guy, M.; Edwards, S. Diagnostic radiation procedures and risk of prostate cancer. Br. J. Cancer 2008, 98, 1852.
- Zuccolo, L.; Lewis, S.J.; Donovan, J.L.; Hamdy, F.C.; Neal, D.E.; Smith, G.D. Alcohol consumption and PSA-detected prostate cancer risk—A case-control nested in the protect study. Int. J. Cancer 2013, 132, 2176–2185.
- McGregor, S.E.; Courneya, K.S.; Kopciuk, K.A.; Tosevski, C.; Friedenreich, C.M. Case–control study of lifetime alcohol intake and prostate cancer risk. Cancer Causes Control 2013, 24, 451–461.
- Endogenous Hormones and Prostate Cancer Collaborative Group; Roddam, A.W.; Allen, N.E.; Appleby, P.; Key, T.J. Endogenous sex hormones and prostate cancer: A collaborative analysis of 18 prospective studies. J. Natl. Cancer Inst. 2008, 100, 170–183.
- Nelles, J.L.; Hu, W.-Y.; Prins, G.S. Estrogen action and prostate cancer. Expert Rev. Endocrinol. Metab. 2011, 6, 437–451.
- Nelson, A.W.; Tilley, W.D.; Neal, D.E.; Carroll, J.S. Estrogen receptor beta in prostate cancer: Friend or foe? Endocr. Relat. Cancer 2014, 21, T219–T234.
- Roddam, A.W.; Allen, N.E.; Appleby, P.; Key, T.J.; Ferrucci, L.; Carter, H.B.; Metter, E.J.; Chen, C.; Weiss, N.S.; Fitzpatrick, A. Insulin-like growth factors, their binding proteins, and prostate cancer risk: Analysis of individual patient data from 12 prospective studies. Ann. Intern. Med. 2008, 149, 461–471.
- Uzoh, C.; Holly, J.; Biernacka, K.; Persad, R.; Bahl, A.; Gillatt, D.; Perks, C. Insulin-like growth factor-binding protein-2 promotes prostate cancer cell growth via igf-dependent or-independent mechanisms and reduces the efficacy of docetaxel. Br. J. Cancer 2011, 104, 1587.
- Robinson, D.; Van Allen, E.M.; Wu, Y.-M.; Schultz, N.; Lonigro, R.J.; Mosquera, J.-M.; Montgomery, B.; Taplin, M.-E.; Pritchard, C.C.; Attard, G. Integrative clinical genomics of advanced prostate cancer. Cell 2015, 161, 1215–1228.
- Klein, A.J.S.E.A. Epidemiology, etiology, and prevention of prostate cancer. In Campbell-Walsh Urology, 11th ed.; Wein, A.J., Ed.; Elsevier: Philadelphia, PA, USA, 2016; Volume 3, pp. 2543–2564.
- Sun, F.; Oyesanmi, O.; Fontanarosa, J.; Reston, J.; Guzzo, T.; Schoelles, K. Therapies for Clinically Localized Prostate Cancer: Update of a 2008 Systematic Review; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2014.
- Mottet, N.; Bellmunt, J.; Bolla, M.; Briers, E.; Cumberbatch, M.G.; De Santis, M.; Fossati, N.; Gross, T.; Henry, A.M.; Joniau, S. EAU-ESTRO-SIOG guidelines on prostate cancer. Part 1: Screening, diagnosis, and local treatment with curative intent. Eur. Urol. 2017, 71, 618–629.
- Cornford, P.; Bellmunt, J.; Bolla, M.; Briers, E.; De Santis, M.; Gross, T.; Henry, A.M.; Joniau, S.; Lam, T.B.; Mason, M.D. EAU-ESTRO-SIOG guidelines on prostate cancer. Part II: Treatment of relapsing, metastatic, and castration-resistant prostate cancer. Eur. Urol. 2017, 71, 630–642.
- Wang, G.; Hu, F.B.; Mistry, K.B.; Zhang, C.; Ren, F.; Huo, Y.; Paige, D.; Bartell, T.; Hong, X.; Caruso, D.; et al. Association between maternal prepregnancy body mass index and plasma folate concentrations with child metabolic health. JAMA Pediatrics 2016, 170, e160845.
- Peeling, P.; Binnie, M.J.; Goods, P.S.R.; Sim, M.; Burke, L.M. Evidence-based supplements for the enhancement of athletic performance. Int. J. Sport Nutr. Exerc. Metab. 2018, 28, 178–187.
- Young, H.H. The early diagnosis and radical cure of carcinoma of the prostate: Being a study of 40 cases and presentation of a radical operation which was carried out in four cases. Johns Hopkins Hosp. Bull. 1905, 16, 315–321.
- Ramsay, C.; Pickard, R.; Robertson, C.; Close, A.; Vale, L.; Armstrong, N.; Barocas, D.; Eden, C.; Fraser, C.; Gurung, T. Systematic review and economic modelling of the relative clinical benefit and cost-effectiveness of laparoscopic surgery and robotic surgery for removal of the prostate in men with localised prostate cancer. Health Technol. Assess. 2012, 16, 1.
- Keyes, M.; Crook, J.; Morton, G.; Vigneault, E.; Usmani, N.; Morris, W.J. Treatment options for localized prostate cancer. Can. Fam. Physician 2013, 59, 1269–1274.
- Litwin, M.S.; Tan, H.-J. The diagnosis and treatment of prostate cancer: A review. JAMA 2017, 317, 2532–2542.
- Bayoumi, A.M.; Brown, A.D.; Garber, A.M. Cost-effectiveness of androgen suppression therapies in advanced prostate cancer. J. Natl. Cancer Inst. 2000, 92, 1731–1739.
- Oefelein, M.G.; Feng, A.; Scolieri, M.J.; Ricchiutti, D.; Resnick, M.I. Reassessment of the definition of castrate levels of testosterone: Implications for clinical decision making. Urology 2000, 56, 1021–1024.
- Seidenfeld, J.; Samson, D.J.; Hasselblad, V.; Aronson, N.; Albertsen, P.C.; Bennett, C.L.; Wilt, T.J. Single-therapy androgen suppression in men with advanced prostate cancer: A systematic review and meta-analysis. Ann. Intern. Med. 2000, 132, 566–577.
- Crawford, E.D.; Shore, N.D.; Moul, J.W.; Tombal, B.; Schröder, F.H.; Miller, K.; Boccon-Gibod, L.; Malmberg, A.; Olesen, T.K.; Persson, B.-E. Long-term tolerability and efficacy of degarelix: 5-year results from a phase iii extension trial with a 1-arm crossover from leuprolide to degarelix. Urology 2014, 83, 1122–1128.
- Goenka, A.; Magsanoc, J.M.; Pei, X.; Schechter, M.; Kollmeier, M.; Cox, B.; Scardino, P.T.; Eastham, J.A.; Zelefsky, M.J. Long-term outcomes after high-dose postprostatectomy salvage radiation treatment. Int. J. Radiat. Oncol. Biol. Phys. 2012, 84, 112–118.
- Chen, C.P.; Weinberg, V.; Shinohara, K.; Roach, M., III; Nash, M.; Gottschalk, A.; Chang, A.J.; Hsu, I.-C. Salvage HDR brachytherapy for recurrent prostate cancer after previous definitive radiation therapy: 5-year outcomes. Int. J. Radiat. Oncol. Biol. Phys. 2013, 86, 324–329.
- Karnes, R.J.; Murphy, C.R.; Bergstralh, E.J.; DiMonte, G.; Cheville, J.C.; Lowe, V.J.; Mynderse, L.A.; Kwon, E.D. Salvage lymph node dissection for prostate cancer nodal recurrence detected by 11c-choline positron emission tomography/computerized tomography. J. Urol. 2015, 193, 111–116.
- Allameh, F.; Rahavian, A.H.; Ghiasy, S. Prevalence of castration success rate in Iranian metastatic prostate cancer patients: A referral center statistics. Int. J. Cancer Manag. 2018, 11, e83613.
- Beer, T.; Garzotto, M.; Henner, W.; Eilers, K.; Wersinger, E. Multiple cycles of intermittent chemotherapy in metastatic androgen-independent prostate cancer. Br. J. Cancer 2004, 91, 1425.
- Dy, S.M.; Asch, S.M.; Naeim, A.; Sanati, H.; Walling, A.; Lorenz, K.A. Evidence-based standards for cancer pain management. J. Clin. Oncol. 2008, 26, 3879–3885.
- Esper, P.; Pienta, K. Supportive Care in the Patient with Hormone Refractory Prostate Cancer. Semin. Urol. Oncol. 1997, 15, 56–64.
- Roehrborn, C.G.; Black, L.K. The economic burden of prostate cancer. BJU Int. 2011, 108, 806–813.
- National Cancer Institute. Online Summary of Trends in Us Cancer Control Measures. Available online: https://progressreport.cancer.gov/after/economic_burden (accessed on 12 September 2018).
- Moghadam, M.F.; Rangchian, M.; Ayati, M.; Pourmand, G.; Zeinali, L.; Rasekh, H. Economic burden of prostate cancer in Iran. Value Health 2016, 19, A147.
- Restelli, U.; Ceresoli, G.L.; Croce, D.; Evangelista, L.; Maffioli, L.S.; Gianoncelli, L.; Bombardieri, E. Economic burden of the management of metastatic castrate-resistant prostate cancer in Italy: A cost of illness study. Cancer Manag. Res. 2017, 9, 789.
- Savithramma, N.; Rao, M.L.; Suhrulatha, D. Screening of medicinal plants for secondary metabolites. Middle-East. J. Sci. Res. 2011, 8, 579–584.
- Petrovska, B.B. Historical review of medicinal plants’ usage. Pharmacogn. Rev. 2012, 6, 1–5.
- Ghasemzadeh, A.; Ghasemzadeh, N. Flavonoids and phenolic acids: Role and biochemical activity in plants and human. J. Med. Plants Res. 2011, 5, 6697–6703.
- Cragg, G.M.; Newman, D.J. Natural product drug discovery in the next millennium. Pharm. Biol. 2001, 39 (Suppl. 1), 8–17.
- Bodeker, G. Traditional health system: Valuing biodiversity for human health and wellbeing. In Cultural and Spiritual Values in Biodiversity; Posey, D.A., Ed.; Intermediate Technology Publications: London, UK, 2000; pp. 261–284.
- Choi, Y.J.; Choi, Y.K.; Lee, K.M.; Cho, S.G.; Kang, S.Y.; Ko, S.G. Sh003 induces apoptosis of du145 prostate cancer cells by inhibiting ERK-involved pathway. BMC Complement. Altern. Med. 2016, 16, 507.
- Diab, K.A.; Guru, S.K.; Bhushan, S.; Saxena, A.K. In vitro anticancer activities of Anogeissus latifolia, Terminalia bellerica, Acacia catechu and Moringa oleiferna Indian plants. Asian Pac. J. Cancer Prev. 2015, 16, 6423–6428.
- Asadi-Samani, M.; Rafieian-Kopaei, M.; Lorigooini, Z.; Shirzad, H. A screening of growth inhibitory activity of iranian medicinal plants on prostate cancer cell lines. BioMedicine 2018, 8, 8.
- Bali, E.B.; Acik, L.; Elci, P.; Sarper, M.; Avcu, F.; Vural, M. In vitro anti-oxidant, cytotoxic and pro-apoptotic effects of Achillea teretifolia willd extracts on human prostate cancer cell lines. Pharmacogn. Mag. 2015, 11, S308–S315.
- Bhandari, J.; Muhammad, B.; Thapa, P.; Shrestha, B.G. Study of phytochemical, anti-microbial, anti-oxidant, and anti-cancer properties of Allium wallichii. BMC Complement. Altern. Med. 2017, 17, 102.
- Al-Oqail, M.M.; El-Shaibany, A.; Al-Jassas, E.; Al-Sheddi, E.S.; Al-Massarani, S.M.; Farshori, N.N. In vitro anti-proliferative activities of aloe perryi flowers extract on human liver, colon, breast, lung, prostate and epithelial cancer cell lines. Pak. J. Pharm. Sci. 2016, 29, 723–729.
- de Alencar, D.C.; Pinheiro, M.L.; Pereira, J.L.; de Carvalho, J.E.; Campos, F.R.; Serain, A.F.; Tirico, R.B.; Hernandez-Tasco, A.J.; Costa, E.V.; Salvador, M.J. Chemical composition of the essential oil from the leaves of Anaxagorea brevipes (Annonaceae) and evaluation of its bioactivity. Nat. Prod. Res. 2016, 30, 1088–1092.
- Zhang, J.; Wang, L.; Zhang, Y.; Li, L.; Tang, S.; Xing, C.; Kim, S.H.; Jiang, C.; Lu, J. Chemopreventive effect of Korean angelica root extract on tramp carcinogenesis and integrative “omic” profiling of affected neuroendocrine carcinomas. Mol. Carcinog. 2015, 54, 1567–1583.
- Tang, S.-N.; Zhang, J.; Wu, W.; Jiang, P.; Puppala, M.; Zhang, Y.; Xing, C.; Kim, S.-H.; Jiang, C.; Lü, J. Chemopreventive effects of Korean angelica vs. Its major pyranocoumarins on two lineages of transgenic adenocarcinoma of mouse prostate carcinogenesis. Cancer Prev. Res. 2015, 8, 835–844.
- Deep, G.; Kumar, R.; Jain, A.K.; Dhar, D.; Panigrahi, G.K.; Hussain, A.; Agarwal, C.; El-Elimat, T.; Sica, V.P.; Oberlies, N.H.; et al. Graviola inhibits hypoxia-induced NADPH oxidase activity in prostate cancer cells reducing their proliferation and clonogenicity. Sci. Rep. 2016, 6, 23135.
- Huang, S.P.; Ho, T.M.; Yang, C.W.; Chang, Y.J.; Chen, J.F.; Shaw, N.S.; Horng, J.C.; Hsu, S.L.; Liao, M.Y.; Wu, L.C.; et al. Chemopreventive potential of ethanolic extracts of luobuma leaves (Apocynum venetum L.) in androgen insensitive prostate cancer. Nutrients 2017, 9, 948.
- Chen, L.; Yan, F.; Chen, W.; Zhao, L.; Zhang, J.; Lu, Q.; Liu, R. Procyanidin from peanut skin induces antiproliferative effect in human prostate carcinoma cells du145. Chem. Biol. Interact. 2018, 288, 12–23.
- Cherian, A.M.; Snima, K.S.; Kamath, C.R.; Nair, S.V.; Lakshmanan, V.K. Effect of Baliospermum montanum nanomedicine apoptosis induction and anti-migration of prostate cancer cells. Biomed. Pharmacother. Biomed. Pharmacother. 2015, 71, 201–209.
- El-Merahbi, R.; Liu, Y.N.; Eid, A.; Daoud, G.; Hosry, L.; Monzer, A.; Mouhieddine, T.H.; Hamade, A.; Najjar, F.; Abou-Kheir, W. Berberis libanotica ehrenb extract shows anti-neoplastic effects on prostate cancer stem/progenitor cells. PLoS ONE 2014, 9, e112453.
- Fort, R.; Trinidad Barnech, J.; Dourron, J.; Colazzo, M.; Aguirre-Crespo, F.; Duhagon, M.; Álvarez, G. Isolation and structural characterization of bioactive molecules on prostate cancer from Mayan traditional medicinal plants. Pharmaceuticals 2018, 11, 78.
- Adaramoye, O.; Erguen, B.; Oyebode, O.; Nitzsche, B.; Hopfner, M.; Jung, K.; Rabien, A. Antioxidant, antiangiogenic and antiproliferative activities of root methanol extract of Calliandra portoricensis in human prostate cancer cells. J. Integr. Med. 2015, 13, 185–193.
- Pandey, S.; Walpole, C.; Cabot, P.J.; Shaw, P.N.; Batra, J.; Hewavitharana, A.K. Selective anti-proliferative activities of carica papaya leaf juice extracts against prostate cancer. Biomed. Pharmacother. Biomed. Pharmacother. 2017, 89, 515–523.
- Ramos-Silva, A.; Tavares-Carreon, F.; Figueroa, M.; De la Torre-Zavala, S.; Gastelum-Arellanez, A.; Rodriguez-Garcia, A.; Galan-Wong, L.J.; Aviles-Arnaut, H. Anticancer potential of Thevetia peruviana fruit methanolic extract. BMC Complement. Altern. Med. 2017, 17, 241.
- Podolak, I.; Olech, M.; Galanty, A.; Zaluski, D.; Grabowska, K.; Sobolewska, D.; Michalik, M.; Nowak, R. Flavonoid and phenolic acid profile by lc-ms/ms and biological activity of crude extracts from Chenopodium hybridum aerial parts. Nat. Prod. Res. 2016, 30, 1766–1770.
- Yousefi, B.; Abasi, M.; Abbasi, M.M.; Jahanban-Esfahlan, R. Anti-proliferative properties of cornus mass fruit in different human cancer cells. Asian Pac. J. Cancer Prev. 2015, 16, 5727–5731.
- Alonso-Castro, A.J.; Zapata-Morales, J.R.; Gonzalez-Chavez, M.M.; Carranza-Alvarez, C.; Hernandez-Benavides, D.M.; Hernandez-Morales, A. Pharmacological effects and toxicity of Costus pulverulentus c. Presl (Costaceae). J. Ethnopharmacol. 2016, 180, 124–130.
- Lee, M.S.; Lee, S.O.; Kim, K.R.; Lee, H.J. Sphingosine kinase-1 involves the inhibitory action of hif-1alpha by Chlorogenic acid in hypoxic du145 cells. Int. J. Mol. Sci. 2017, 18, 325.
- Zheng, J.; Zhou, Y.; Li, Y.; Xu, D.P.; Li, S.; Li, H.B. Spices for prevention and treatment of cancers. Nutrients 2016, 8, 495.
- D’Alessandro, A.M.; Mancini, A.; Lizzi, A.R.; De Simone, A.; Marroccella, C.E.; Gravina, G.L.; Tatone, C.; Festuccia, C. Crocus sativus stigma extract and its major constituent crocin possess significant antiproliferative properties against human prostate cancer. Nutr. Cancer 2013, 65, 930–942.
- Festuccia, C.; Mancini, A.; Gravina, G.L.; Scarsella, L.; Llorens, S.; Alonso, G.L.; Tatone, C.; Di Cesare, E.; Jannini, E.A.; Lenzi, A.; et al. Antitumor effects of saffron-derived carotenoids in prostate cancer cell models. Biomed Res. Int. 2014, 2014, 135048.
- Irshad, S.; Ashfaq, A.; Muazzam, A.; Yasmeen, A. Antimicrobial and anti-prostate cancer activity of turmeric (Curcuma longa L.) and black pepper (Piper nigrum L.) used in typical pakistani cuisine. Pak. J. Zool. 2017, 49, 1665–1669.
- Bayala, B.; Bassole, I.H.N.; Maqdasy, S.; Baron, S.; Simpore, J.; Lobaccaro, J.A. Cymbopogon citratus and Cymbopogon giganteus essential oils have cytotoxic effects on tumor cell cultures. Identification of citral as a new putative anti-proliferative molecule. Biochimie 2018, 153, 162–170.
- Tong, K.L.; Chan, K.L.; AbuBakar, S.; Low, B.S.; Ma, H.Q.; Wong, P.F. The in vitro and in vivo anti-cancer activities of a standardized quassinoids composition from Eurycoma longifolia on lncap human prostate cancer cells. PLoS ONE 2015, 10, e0121752.
- Kassim, O.O.; Copeland, R.L.; Kenguele, H.M.; Nekhai, S.; Ako-Nai, K.A.; Kanaan, Y.M. Antiproliferative activities of Fagara xanthoxyloides and Pseudocedrela kotschyi against prostate cancer cell lines. Anticancer Res. 2015, 35, 1453–1458.
- Lin, H.C.; Lin, J.Y. Immune cell-conditioned media suppress prostate cancer pc-3 cell growth correlating with decreased proinflammatory/anti-inflammatory cytokine ratios in the media using 5 selected crude polysaccharides. Integr. Cancer Ther. 2016, 15, Np13–Np25.
- Hanafi, M.M.M.; Afzan, A.; Yaakob, H.; Aziz, R.; Sarmidi, M.R.; Wolfender, J.L.; Prieto, J.M. In vitro pro-apoptotic and anti-migratory effects of Ficus deltoidea L. Plant extracts on the human prostate cancer cell lines pc3. Front. Pharmacol. 2017, 8, 895.
- Rayaprolu, S.J.; Hettiarachchy, N.S.; Horax, R.; Phillips, G.K.; Mahendran, M.; Chen, P. Soybean peptide fractions inhibit human blood, breast and prostate cancer cell proliferation. J. Food Sci. Technol. 2017, 54, 38–44.
- Park, S.Y.; Kwon, S.J.; Lim, S.S.; Kim, J.K.; Lee, K.W.; Park, J.H. Licoricidin, an active compound in the hexane/ethanol extract of Glycyrrhiza uralensis, inhibits lung metastasis of 4t1 murine mammary carcinoma cells. Int. J. Mol. Sci. 2016, 17, 934.
- Pham, H.N.T.; Sakoff, J.A.; Bond, D.R.; Vuong, Q.V.; Bowyer, M.C.; Scarlett, C.J. In vitro antibacterial and anticancer properties of Helicteres hirsuta lour. Leaf and stem extracts and their fractions. Mol. Biol. Rep. 2018, 45, 2125–2133.
- Chiu, C.T.; Chen, J.H.; Chou, F.P.; Lin, H.H. Hibiscus sabdariffa leaf extract inhibits human prostate cancer cell invasion via down-regulation of akt/nf-kb/mmp-9 pathway. Nutrients 2015, 7, 5065–5087.
- Koczurkiewicz, P.; Kowolik, E.; Podolak, I.; Wnuk, D.; Piska, K.; Labedz-Maslowska, A.; Wojcik-Pszczola, K.; Pekala, E.; Czyz, J.; Michalik, M. Synergistic cytotoxic and anti-invasive effects of mitoxantrone and triterpene saponins from Lysimachia ciliata on human prostate cancer cells. Planta Med. 2016, 82, 1546–1552.
- Shabbir, M.; Syed, D.N.; Lall, R.K.; Khan, M.R.; Mukhtar, H. Potent anti-proliferative, pro-apoptotic activity of the maytenus royleanus extract against prostate cancer cells: Evidence in in-vitro and in-vivo models. PLoS ONE 2015, 10, e0119859.
- Jahanban-Esfahlan, R.; Seidi, K.; Monfaredan, A.; Shafie-Irannejad, V.; Abbasi, M.M.; Karimian, A.; Yousefi, B. The herbal medicine melissa officinalis extract effects on gene expression of p53, bcl-2, her2, vegf-a and htert in human lung, breast and prostate cancer cell lines. Gene 2017, 613, 14–19.
- Jahanban-Esfahlan, A.; Modaeinama, S.; Abasi, M.; Abbasi, M.M.; Jahanban-Esfahlan, R. Anti proliferative properties of Melissa officinalis in different human cancer cells. Asian Pac. J. Cancer Prev. 2015, 16, 5703–5707.
- Sharma, V.; Hussain, S.; Gupta, M.; Saxena, A.K. In vitro anticancer activity of extracts of Mentha spp. Against human cancer cells. Indian J. Biochem. Biophys. 2014, 51, 416–419.
- Emami, S.A.; Asili, J.; Hossein Nia, S.; Yazdian-Robati, R.; Sahranavard, M.; Tayarani-Najaran, Z. Growth inhibition and apoptosis induction of essential oils and extracts of Nepeta cataria L. On human prostatic and breast cancer cell lines. Asian Pac. J. Cancer Prev. 2016, 17, 125–130.
- Mollazadeh, H.; Afshari, A.R.; Hosseinzadeh, H. Review on the potential therapeutic roles of nigella sativa in the treatment of patients with cancer: Involvement of apoptosis: Black cumin and cancer. J. Pharmacopunct. 2017, 20, 158–172.
- Uttama, S.; Itharat, A.; Rattarom, R.; Makchuchit, S.; Panthong, S.; Sakpakdeejaroen, I. Biological activities and chemical content of sung yod rice bran oil extracted by expression and soxhlet extraction methods. J. Med Assoc. Thail. Chotmaihet Thangphaet 2014, 97 (Suppl. 8), S125–S132.
- Zhang, Z.H.; Xie, D.D.; Xu, S.; Xia, M.Z.; Zhang, Z.Q.; Geng, H.; Chen, L.; Wang, D.M.; Wei, W.; Yu, D.X.; et al. Total glucosides of paeony inhibits lipopolysaccharide-induced proliferation, migration and invasion in androgen insensitive prostate cancer cells. PLoS ONE 2017, 12, e0182584.
- Nguyen, V.T.; Sakoff, J.A.; Scarlett, C.J. Physicochemical properties, antioxidant and anti-proliferative capacities of dried leaf and its extract from xao tam phan (Paramignya trimera). Chem. Biodivers. 2017, 14, e1600498.
- Tang, Y.Q.; Jaganath, I.B.; Manikam, R.; Sekaran, S.D. Phyllanthus spp. Exerts anti-angiogenic and anti-metastatic effects through inhibition on matrix metalloproteinase enzymes. Nutr. Cancer 2015, 67, 783–795.
- Nair, H.A.; Snima, K.S.; Kamath, R.C.; Nair, S.V.; Lakshmanan, V.K. Plumbagin nanoparticles induce dose and PH dependent toxicity on prostate cancer cells. Curr. Drug Deliv. 2015, 12, 709–716.
- Han, S.Y.; Hu, M.H.; Qi, G.Y.; Ma, C.X.; Wang, Y.Y.; Ma, F.L.; Tao, N.; Qin, Z.H. Polysaccharides from polygonatum inhibit the proliferation of prostate cancer-associated fibroblasts. Asian Pac. J. Cancer Prev. 2016, 17, 3829–3833.
- Peng, C.-C.; Peng, C.-H.; Chen, K.-C.; Hsieh, C.-L.; Peng, R.Y. The aqueous soluble polyphenolic fraction of Psidium guajava leaves exhibits potent anti-angiogenesis and anti-migration actions on du145 cells. Evid. Based Complement. Altern. Med. 2011, 2011, 219069.
- Chen, K.C.; Peng, C.C.; Chiu, W.T.; Cheng, Y.T.; Huang, G.T.; Hsieh, C.L.; Peng, R.Y. Action mechanism and signal pathways of Psidium guajava L. Aqueous extract in killing prostate cancer lncap cells. Nutr. Cancer 2010, 62, 260–270.
- Albrecht, M.; Jiang, W.; Kumi-Diaka, J.; Lansky, E.P.; Gommersall, L.M.; Patel, A.; Mansel, R.E.; Neeman, I.; Geldof, A.A.; Campbell, M.J. Pomegranate extracts potently suppress proliferation, xenograft growth, and invasion of human prostate cancer cells. J. Med. Food 2004, 7, 274–283.
- Pantuck, A.J.; Pettaway, C.A.; Dreicer, R.; Corman, J.; Katz, A.; Ho, A.; Aronson, W.; Clark, W.; Simmons, G.; Heber, D. A randomized, double-blind, placebo-controlled study of the effects of pomegranate extract on rising psa levels in men following primary therapy for prostate cancer. Prostate Cancer Prostatic Dis. 2015, 18, 242–248.
- Seidi, K.; Jahanban-Esfahlan, R.; Abasi, M.; Abbasi, M.M. Anti tumoral properties of Punica granatum (Pomegranate) seed extract in different human cancer cells. Asian Pac. J. Cancer Prev. 2016, 17, 1119–1122.
- Ub Wijerathne, C.; Park, H.S.; Jeong, H.Y.; Song, J.W.; Moon, O.S.; Seo, Y.W.; Won, Y.S.; Son, H.Y.; Lim, J.H.; Yeon, S.H.; et al. Quisqualis indica improves benign prostatic hyperplasia by regulating prostate cell proliferation and apoptosis. Biol. Pharm. Bull. 2017, 40, 2125–2133.
- Kim, A.; Im, M.; Ma, J.Y. Ethanol extract of remotiflori radix induces endoplasmic reticulum stress-mediated cell death through ampk/mtor signaling in human prostate cancer cells. Sci. Rep. 2015, 5, 8394.
- Atmaca, H.; Bozkurt, E. Apoptotic and anti-angiogenic effects of Salvia triloba extract in prostate cancer cell lines. Tumour Biol. J. Int. Soc. Oncodev. Biol. Med. 2016, 37, 3639–3646.
- Chang, C.C.; Hsu, H.F.; Huang, K.H.; Wu, J.M.; Kuo, S.M.; Ling, X.H.; Houng, J.Y. Anti-proliferative effects of Siegesbeckia orientalis ethanol extract on human endometrial rl-95 cancer cells. Molecules 2014, 19, 19980–19994.
- Lin, H.; Jackson, G.A.; Lu, Y.; Drenkhahn, S.K.; Brownstein, K.J.; Starkey, N.J.; Lamberson, W.R.; Fritsche, K.L.; Mossine, V.V.; Besch-Williford, C.L.; et al. Inhibition of gli/hedgehog signaling in prostate cancer cells by “cancer bush” Sutherlandia frutescens extract. Cell Biol. Int. 2016, 40, 131–142.
- Mohammadi, A.; Mansoori, B.; Aghapour, M.; Baradaran, B. Urtica dioica dichloromethane extract induce apoptosis from intrinsic pathway on human prostate cancer cells (pc3). Cell. Mol. Biol. 2016, 62, 78–83.
- Burton, L.J.; Rivera, M.; Hawsawi, O.; Zou, J.; Hudson, T.; Wang, G.; Zhang, Q.; Cubano, L.; Boukli, N.; Odero-Marah, V. Muscadine grape skin extract induces an unfolded protein response-mediated autophagy in prostate cancer cells: A tmt-based quantitative proteomic analysis. PLoS ONE 2016, 11, e0164115.
- Tsai, C.H.; Tzeng, S.F.; Hsieh, S.C.; Tsai, C.J.; Yang, Y.C.; Tsai, M.H.; Hsiao, P.W. A standardized Wedelia chinensis extract overcomes the feedback activation of her2/3 signaling upon androgen-ablation in prostate cancer. Front. Pharmacol. 2017, 8, 721.
- Tsai, C.H.; Tzeng, S.F.; Hsieh, S.C.; Lin, C.Y.; Tsai, C.J.; Chen, Y.R.; Yang, Y.C.; Chou, Y.W.; Lee, M.T.; Hsiao, P.W. Development of a standardized and effect-optimized herbal extract of Wedelia chinensis for prostate cancer. Phytomed. Int. J. Phytother. Phytopharm. 2015, 22, 406–414.
- Sarbishegi, M.; Khani, M.; Salimi, S.; Valizadeh, M.; Sargolzaei Aval, F. Antiproliferative and antioxidant effects of Withania coagulans extract on benign prostatic hyperplasia in rats. Nephro-Urol. Mon. 2016, 8, e33180.
- Adaramoye, O.; Erguen, B.; Nitzsche, B.; Hopfner, M.; Jung, K.; Rabien, A. Antioxidant and antiproliferative potentials of methanol extract of Xylopia aethiopica (dunal) a. Rich in pc-3 and lncap cells. J. Basic Clin. Physiol. Pharmacol. 2017, 28, 403–412.
- Yang, Y.; Ikezoe, T.; Takeuchi, T.; Adachi, Y.; Ohtsuki, Y.; Koeffler, H.P.; Taguchi, H. Zanthoxyli fructus induces growth arrest and apoptosis of lncap human prostate cancer cells in vitro and in vivo in association with blockade of the akt and ar signal pathways. Oncol. Rep. 2006, 15, 1581–1590.
- Karna, P.; Chagani, S.; Gundala, S.R.; Rida, P.C.G.; Asif, G.; Sharma, V.; Gupta, M.V.; Aneja, R. Benefits of whole ginger extract in prostate cancer. Br. J. Nutr. 2012, 107, 473–484.
- Brahmbhatt, M.; Gundala, S.R.; Asif, G.; Shamsi, S.A.; Aneja, R. Ginger phytochemicals exhibit synergy to inhibit prostate cancer cell proliferation. Nutr. Cancer 2013, 65, 263–272.
- Liu, C.M.; Kao, C.L.; Wu, H.M.; Li, W.J.; Huang, C.T.; Li, H.T.; Chen, C.Y. Antioxidant and anticancer aporphine alkaloids from the leaves of Nelumbo nucifera gaertn. Cv. Rosa-plena. Molecules 2014, 19, 17829–17838.
- Arai, M.A.; Akamine, R.; Sadhu, S.K.; Ahmed, F.; Ishibashi, M. Hedgehog/gli-mediated transcriptional activity inhibitors from Crinum asiaticum. J. Nat. Med. 2015, 69, 538–542.
- Ramos-Torres, A.; Bort, A.; Morell, C.; Rodriguez-Henche, N.; Diaz-Laviada, I. The pepper’s natural ingredient capsaicin induces autophagy blockage in prostate cancer cells. Oncotarget 2016, 7, 1569–1583.
- Bamji, Z.D.; Washington, K.N.; Akinboye, E.; Bakare, O.; Kanaan, Y.M.; Copeland, R.L., Jr. Apoptotic effects of novel dithiocarbamate analogs of emetine in prostate cancer cell lines. Anticancer Res. 2015, 35, 4723–4732.
- Akinboye, E.S.; Rosen, M.D.; Bakare, O.; Denmeade, S.R. Anticancer activities of emetine prodrugs that are proteolytically activated by the prostate specific antigen (PSA) and evaluation of in vivo toxicity of emetine derivatives. Bioorg. Med. Chem. 2017, 25, 6707–6717.
- Hu, M.; Peng, S.; He, Y.; Qin, M.; Cong, X.; Xing, Y.; Liu, M.; Yi, Z. Lycorine is a novel inhibitor of the growth and metastasis of hormone-refractory prostate cancer. Oncotarget 2015, 6, 15348–15361.
- Wang, Q.; Xu, J.; Li, X.; Zhang, D.; Han, Y.; Zhang, X. Comprehensive two-dimensional pc-3 prostate cancer cell membrane chromatography for screening anti-tumor components from radix Sophorae flavescentis. J. Sep. Sci. 2017, 40, 2688–2693.
- Poornima, B.; Siva, B.; Shankaraiah, G.; Venkanna, A.; Nayak, V.L.; Ramakrishna, S.; Venkat Rao, C.; Babu, K.S. Novel sesquiterpenes from Schisandra grandiflora: Isolation, cytotoxic activity and synthesis of their triazole derivatives using “click” reaction. Eur. J. Med. Chem. 2015, 92, 449–458.
- Lan, J.; Huang, L.; Lou, H.; Chen, C.; Liu, T.; Hu, S.; Yao, Y.; Song, J.; Luo, J.; Liu, Y.; et al. Design and synthesis of novel c14-urea-tetrandrine derivatives with potent anti-cancer activity. Eur. J. Med. Chem. 2018, 143, 1968–1980.
- Li, G.; Petiwala, S.M.; Nonn, L.; Johnson, J.J. Inhibition of chop accentuates the apoptotic effect of alpha-mangostin from the Mangosteen fruit (Garcinia mangostana) in 22rv1 prostate cancer cells. Biochem. Biophys. Res. Commun. 2014, 453, 75–80.
- Sato, C.; Kaneko, S.; Sato, A.; Virgona, N.; Namiki, K.; Yano, T. Combination effect of delta-tocotrienol and gamma-tocopherol on prostate cancer cell growth. J. Nutr. Sci. Vitaminol. 2017, 63, 349–354.
- Stadlbauer, S.; Steinborn, C.; Klemd, A.; Hattori, F.; Ohmori, K.; Suzuki, K.; Huber, R.; Wolf, P.; Grundemann, C. Impact of green tea catechin ecg and its synthesized fluorinated analogue on prostate cancer cells and stimulated immunocompetent cells. Planta Med. 2018, 84, 813–819.
- Busch, C.; Noor, S.; Leischner, C.; Burkard, M.; Lauer, U.M.; Venturelli, S. Anti-proliferative activity of hop-derived prenylflavonoids against human cancer cell lines. Wien. Med. Wochenschr. 2015, 165, 258–261.
- Afsar, T.; Trembley, J.H.; Salomon, C.E.; Razak, S.; Khan, M.R.; Ahmed, K. Growth inhibition and apoptosis in cancer cells induced by polyphenolic compounds of Acacia hydaspica: Involvement of multiple signal transduction pathways. Sci. Rep. 2016, 6, 23077.
- Zhu, K.C.; Sun, J.M.; Shen, J.G.; Jin, J.Z.; Liu, F.; Xu, X.L.; Chen, L.; Liu, L.T.; Lv, J.J. Afzelin exhibits anti-cancer activity against androgen-sensitive lncap and androgen-independent pc-3 prostate cancer cells through the inhibition of lim domain kinase 1. Oncol. Lett. 2015, 10, 2359–2365.
- Jiang, C.; Masood, M.; Rasul, A.; Wei, W.; Wang, Y.; Ali, M.; Mustaqeem, M.; Li, J.; Li, X. Altholactone inhibits nf-kappab and stat3 activation and induces reactive oxygen species-mediated apoptosis in prostate cancer du145 cells. Molecules 2017, 22, 240.
- Shukla, S.; Shankar, E.; Fu, P.; MacLennan, G.T.; Gupta, S. Suppression of nf-kappab and nf-kappab-regulated gene expression by apigenin through ikappabalpha and ikk pathway in tramp mice. PLoS ONE 2015, 10, e0138710.
- Ryu, S.; Lim, W.; Bazer, F.W.; Song, G. Chrysin induces death of prostate cancer cells by inducing ros and er stress. J. Cell. Physiol. 2017, 232, 3786–3797.
- Sharma, U.K.; Sharma, A.K.; Gupta, A.; Kumar, R.; Pandey, A.; Pandey, A.K. Pharmacological activities of cinnamaldehyde and eugenol: Antioxidant, cytotoxic and anti-leishmanial studies. Cell. Mol. Biol. 2017, 63, 73–78.
- Adahoun, M.A.; Al-Akhras, M.H.; Jaafar, M.S.; Bououdina, M. Enhanced anti-cancer and antimicrobial activities of curcumin nanoparticles. Artif. CellsNanomed. Biotechnol. 2017, 45, 98–107.
- Chen, Q.H. Curcumin-based anti-prostate cancer agents. Anti-Cancer Agents Med. Chem. 2015, 15, 138–156.
- Dorai, T.; Cao, Y.C.; Dorai, B.; Buttyan, R.; Katz, A.E. Therapeutic potential of curcumin in human prostate cancer. III. Curcumin inhibits proliferation, induces apoptosis, and inhibits angiogenesis of lncap prostate cancer cells in vivo. Prostate 2001, 47, 293–303.
- Perrone, D.; Ardito, F.; Giannatempo, G.; Dioguardi, M.; Troiano, G.; Lo Russo, L.; A, D.E.L.; Laino, L.; Lo Muzio, L. Biological and therapeutic activities, and anticancer properties of curcumin. Exp. Ther. Med. 2015, 10, 1615–1623.
- Kumar, C.; Rasool, R.U.; Iqra, Z.; Nalli, Y.; Dutt, P.; Satti, N.K.; Sharma, N.; Gandhi, S.G.; Goswami, A.; Ali, A. Alkyne-azide cycloaddition analogues of dehydrozingerone as potential anti-prostate cancer inhibitors via the pi3k/akt/nf-kb pathway. MedChemComm 2017, 8, 2115–2124.
- Jeong, M.H.; Ko, H.; Jeon, H.; Sung, G.J.; Park, S.Y.; Jun, W.J.; Lee, Y.H.; Lee, J.; Lee, S.W.; Yoon, H.G.; et al. Delphinidin induces apoptosis via cleaved hdac3-mediated p53 acetylation and oligomerization in prostate cancer cells. Oncotarget 2016, 7, 56767–56780.
- Hafeez, B.B.; Siddiqui, I.A.; Asim, M.; Malik, A.; Afaq, F.; Adhami, V.M.; Saleem, M.; Din, M.; Mukhtar, H. A dietary anthocyanidin delphinidin induces apoptosis of human prostate cancer pc3 cells in vitro and in vivo: Involvement of nuclear factor-κb signaling. Cancer Res. 2008, 68, 8564–8572.
- Naiki-Ito, A.; Chewonarin, T.; Tang, M.; Pitchakarn, P.; Kuno, T.; Ogawa, K.; Asamoto, M.; Shirai, T.; Takahashi, S. Ellagic acid, a component of pomegranate fruit juice, suppresses androgen-dependent prostate carcinogenesis via induction of apoptosis. Prostate 2015, 75, 151–160.
- Eskandari, E.; Heidarian, E.; Amini, S.A.; Saffari-Chaleshtori, J. Evaluating the effects of ellagic acid on pstat3, pakt, and perk1/2 signaling pathways in prostate cancer pc3 cells. J. Cancer Res. Ther. 2016, 12, 1266–1271.
- Lall, R.K.; Syed, D.N.; Khan, M.I.; Adhami, V.M.; Gong, Y.; Lucey, J.A.; Mukhtar, H. Dietary flavonoid fisetin increases abundance of high-molecular-mass hyaluronan conferring resistance to prostate oncogenesis. Carcinogenesis 2016, 37, 918–928.
- Li, X.; Yokoyama, N.N.; Zhang, S.; Ding, L.; Liu, H.M.; Lilly, M.B.; Mercola, D.; Zi, X. Flavokawain a induces deneddylation and skp2 degradation leading to inhibition of tumorigenesis and cancer progression in the tramp transgenic mouse model. Oncotarget 2015, 6, 41809–41824.
- Drees, M.; Dengler, W.A.; Roth, T.; Labonte, H.; Mayo, J.; Malspeis, L.; Grever, M.; Sausville, E.A.; Fiebig, H.H. Flavopiridol (l86–8275): Selective antitumor activity in vitro and activity in vivo for prostate carcinoma cells. Clin. Cancer Res. 1997, 3, 273.
- Wang, Y.; Tsai, M.-L.; Chiou, L.-Y.; Ho, C.-T.; Pan, M.-H. Antitumor activity of garcinol in human prostate cancer cells and xenograft mice. J. Agric. Food Chem. 2015, 63, 9047–9052.
- Behera, A.K.; Swamy, M.M.; Natesh, N.; Kundu, T.K. Garcinol and its role in chronic diseases. Adv. Exp. Med. Biol. 2016, 928, 435–452.
- Jeon, Y.J.; Jung, S.N.; Yun, J.; Lee, C.W.; Choi, J.; Lee, Y.J.; Han, D.C.; Kwon, B.M. Ginkgetin inhibits the growth of du-145 prostate cancer cells through inhibition of signal transducer and activator of transcription 3 activity. Cancer Sci. 2015, 106, 413–420.
- Shirzad, M.; Heidarian, E.; Beshkar, P.; Gholami-Arjenaki, M. Biological effects of hesperetin on interleukin-6/phosphorylated signal transducer and activator of transcription 3 pathway signaling in prostate cancer pc3 cells. Pharmacogn. Res. 2017, 9, 188–194.
- Kang, S.; Kim, J.E.; Li, Y.; Jung, S.K.; Song, N.R.; Thimmegowda, N.R.; Kim, B.Y.; Lee, H.J.; Bode, A.M.; Dong, Z.; et al. Hirsutenone in alnus extract inhibits akt activity and suppresses prostate cancer cell proliferation. Mol. Carcinog. 2015, 54, 1354–1362.
- Lowe, H.I.C.; Toyang, N.J.; Watson, C.T.; Ayeah, K.N.; Bryant, J. Hlbt-100: A highly potent anti-cancer flavanone from Tillandsia recurvata (L.). Cancer Cell Int. 2017, 17, 38.
- Hahm, E.-R.; Karlsson, A.I.; Bonner, M.Y.; Arbiser, J.L.; Singh, S.V. Honokiol inhibits androgen receptor activity in prostate cancer cells. Prostate 2014, 74, 408–420.
- Miura, Y.; Oyama, M.; Iguchi, K.; Ito, T.; Baba, M.; Shikama, Y.; Usui, S.; Hirano, K.; Iinuma, M.; Mikamo, H. Anti-androgenic activity of icarisid II from Epimedium herb in prostate cancer lncap cells. J. Nutr. Sci. Vitaminol. 2015, 61, 201–204.
- Park, S.Y.; Lim, S.S.; Kim, J.K.; Kang, I.J.; Kim, J.S.; Lee, C.; Kim, J.; Park, J.H. Hexane-ethanol extract of glycyrrhiza uralensis containing licoricidin inhibits the metastatic capacity of du145 human prostate cancer cells. Br. J. Nutr. 2010, 104, 1272–1282.
- Seon, M.R.; Park, S.Y.; Kwon, S.J.; Lim, S.S.; Choi, H.J.; Park, H.; Lim, D.Y.; Kim, J.S.; Lee, C.H.; Kim, J.; et al. Hexane/ethanol extract of glycyrrhiza uralensis and its active compound isoangustone a induce g1 cycle arrest in du145 human prostate and 4t1 murine mammary cancer cells. J. Nutr. Biochem. 2012, 23, 85–92.
- Fang, F.; Chen, S.; Ma, J.; Cui, J.; Li, Q.; Meng, G.; Wang, L. Juglone suppresses epithelial-mesenchymal transition in prostate cancer cells via the protein kinase b/glycogen synthase kinase-3beta/snail signaling pathway. Oncol. Lett. 2018, 16, 2579–2584.
- McKeown, B.T.; McDougall, L.; Catalli, A.; Hurta, R.A. Magnolol causes alterations in the cell cycle in androgen insensitive human prostate cancer cells in vitro by affecting expression of key cell cycle regulatory proteins. Nutr. Cancer 2014, 66, 1154–1164.
- Li, M.; Ma, H.; Yang, L.; Li, P. Mangiferin inhibition of proliferation and induction of apoptosis in human prostate cancer cells is correlated with downregulation of b-cell lymphoma-2 and upregulation of microrna-182. Oncol. Lett. 2016, 11, 817–822.
- Nunez Selles, A.J.; Daglia, M.; Rastrelli, L. The potential role of mangiferin in cancer treatment through its immunomodulatory, anti-angiogenic, apoptopic, and gene regulatory effects. Biofactors 2016, 42, 475–491.
- Lee, J.; Lee, S.; Kim, S.L.; Choi, J.W.; Seo, J.Y.; Choi, D.J.; Park, Y.I. Corn silk maysin induces apoptotic cell death in pc-3 prostate cancer cells via mitochondria-dependent pathway. Life Sci. 2014, 119, 47–55.
- Shokoohinia, Y.; Hosseinzadeh, L.; Alipour, M.; Mostafaie, A.; Mohammadi-Motlagh, H.-R. Comparative evaluation of cytotoxic and apoptogenic effects of several coumarins on human cancer cell lines: Osthole induces apoptosis in p53-deficient h1299 cells. Adv. Pharmacol. Sci. 2014, 2014, 8.
- Liu, Y.; Zhang, X.; Kelsang, N.; Tu, G.; Kong, D.; Lu, J.; Zhang, Y.; Liang, H.; Tu, P.; Zhang, Q. Structurally diverse cytotoxic dimeric chalcones from Oxytropis chiliophylla. J. Nat. Prod. 2018, 81, 307–315.
- Xu, Y.; Zhu, J.Y.; Lei, Z.M.; Wan, L.J.; Zhu, X.W.; Ye, F.; Tong, Y.Y. Anti-proliferative effects of paeonol on human prostate cancer cell lines du145 and pc-3. J. Physiol. Biochem. 2017, 73, 157–165.
- Tsai, C.C.; Chuang, T.W.; Chen, L.J.; Niu, H.S.; Chung, K.M.; Cheng, J.T.; Lin, K.C. Increase in apoptosis by combination of metformin with silibinin in human colorectal cancer cells. World J. Gastroenterol. 2015, 21, 4169–4177.
- Sun, C.P.; Qiu, C.Y.; Yuan, T.; Nie, X.F.; Sun, H.X.; Zhang, Q.; Li, H.X.; Ding, L.Q.; Zhao, F.; Chen, L.X.; et al. Antiproliferative and anti-inflammatory withanolides from Physalis angulata. J. Nat. Prod. 2016, 79, 1586–1597.
- Aziz, M.H.; Dreckschmidt, N.E.; Verma, A.K. Plumbagin, a medicinal plant-derived naphthoquinone, is a novel inhibitor of the growth and invasion of hormone refractory prostate cancer. Cancer Res. 2008, 68, 9024–9032.
- Adaramoye, O.; Erguen, B.; Nitzsche, B.; Hopfner, M.; Jung, K.; Rabien, A. Punicalagin, a polyphenol from pomegranate fruit, induces growth inhibition and apoptosis in human pc-3 and lncap cells. Chem. Biol. Interact. 2017, 274, 100–106.
- Al-Jabban, S.M.; Zhang, X.; Chen, G.; Mekuria, E.A.; Rakotondraibe, L.H.; Chen, Q.H. Synthesis and anti-proliferative effects of quercetin derivatives. Nat. Prod. Commun. 2015, 10, 2113–2118.
- Li, X.; Chen, G.; Zhang, X.; Zhang, Q.; Zheng, S.; Wang, G.; Chen, Q.H. A new class of flavonol-based anti-prostate cancer agents: Design, synthesis, and evaluation in cell models. Bioorg. Med. Chem. Lett. 2016, 26, 4241–4245.
- Yang, F.; Song, L.; Wang, H.; Wang, J.; Xu, Z.; Xing, N. Quercetin in prostate cancer: Chemotherapeutic and chemopreventive effects, mechanisms and clinical application potential (review). Oncol. Rep. 2015, 33, 2659–2668.
- Li, J.; Chong, T.; Wang, Z.; Chen, H.; Li, H.; Cao, J.; Zhang, P.; Li, H. A novel anticancer effect of resveratrol: Reversal of epithelialmesenchymal transition in prostate cancer cells. Mol. Med. Rep. 2014, 10, 1717–1724.
- Wang, T.T.Y.; Hudson, T.S.; Wang, T.-C.; Remsberg, C.M.; Davies, N.M.; Takahashi, Y.; Kim, Y.S.; Seifried, H.; Vinyard, B.T.; Perkins, S.N.; et al. Differential effects of resveratrol on androgen-responsive lncap human prostate cancer cells in vitro and in vivo. Carcinogenesis 2008, 29, 2001–2010.
- Berman, A.Y.; Motechin, R.A.; Wiesenfeld, M.Y.; Holz, M.K. The therapeutic potential of resveratrol: A review of clinical trials. NPJ Precis. Oncol. 2017, 1, 35.
- Lee, C.L.; Hwang, T.L.; Peng, C.Y.; Chen, C.J.; Kuo, C.L.; Chang, W.Y.; Wu, Y.C. Anti-inflammatory and cytotoxic compounds from solanum macaonense. Nat. Prod. Commun. 2015, 10, 345–348.
- Karakurt, S.; Adali, O. Tannic acid inhibits proliferation, migration, invasion of prostate cancer and modulates drug metabolizing and antioxidant enzymes. Anti-Cancer Agents Med. Chem. 2016, 16, 781–789.
- Ghasemi, S.; Lorigooini, Z.; Wibowo, J.; Amini-Khoei, H. Tricin isolated from allium atroviolaceum potentiated the effect of docetaxel on pc3 cell proliferation: Role of mir-21. Nat. Prod. Res. 2018, 33, 1828–1831.
- Klosek, M.; Mertas, A.; Krol, W.; Jaworska, D.; Szymszal, J.; Szliszka, E. Tumor necrosis factor-related apoptosis-inducing ligand-induced apoptosis in prostate cancer cells after treatment with xanthohumol-a natural compound present in Humulus lupulus L. Int. J. Mol. Sci. 2016, 17, 837.
- Ikemoto, K.; Shimizu, K.; Ohashi, K.; Takeuchi, Y.; Shimizu, M.; Oku, N. Bauhinia purprea agglutinin-modified liposomes for human prostate cancer treatment. Cancer Sci. 2016, 107, 53–59.
- Hu, E.; Wang, D.; Chen, J.; Tao, X. Novel cyclotides from Hedyotis diffusa induce apoptosis and inhibit proliferation and migration of prostate cancer cells. Int. J. Clin. Exp. Med. 2015, 8, 4059–4065.
- Gondim, A.C.S.; Romero-Canelon, I.; Sousa, E.H.S.; Blindauer, C.A.; Butler, J.S.; Romero, M.J.; Sanchez-Cano, C.; Sousa, B.L.; Chaves, R.P.; Nagano, C.S.; et al. The potent anti-cancer activity of Dioclea lasiocarpa lectin. J. Inorg. Biochem. 2017, 175, 179–189.
- Santha, S.; Dwivedi, C. Anticancer effects of sandalwood (Santalum album). Anticancer Res. 2015, 35, 3137–3145.
- Farimani, M.M.; Taleghani, A.; Aliabadi, A.; Aliahmadi, A.; Esmaeili, M.A.; Namazi Sarvestani, N.; Khavasi, H.R.; Smiesko, M.; Hamburger, M.; Nejad Ebrahimi, S. Labdane diterpenoids from Salvia leriifolia: Absolute configuration, antimicrobial and cytotoxic activities. Planta Med. 2016, 82, 1279–1285.
- Wang, W.; Rayburn, E.R.; Hao, M.; Zhao, Y.; Hill, D.L.; Zhang, R.; Wang, H. Experimental therapy of prostate cancer with novel natural product anti-cancer ginsenosides. Prostate 2008, 68, 809–819.
- Chun, J.Y.; Tummala, R.; Nadiminty, N.; Lou, W.; Liu, C.; Yang, J.; Evans, C.P.; Zhou, Q.; Gao, A.C. Andrographolide, an herbal medicine, inhibits interleukin-6 expression and suppresses prostate cancer cell growth. Genes Cancer 2010, 1, 868–876.
- Kuchta, K.; Xiang, Y.; Huang, S.; Tang, Y.; Peng, X.; Wang, X.; Zhu, Y.; Li, J.; Xu, J.; Lin, Z.; et al. Celastrol, an active constituent of the TCM plant Tripterygium wilfordii hook. F. inhibits prostate cancer bone metastasis. Prostate Cancer Prostatic Dis. 2017, 20, 156–164.
- Nie, C.; Zhou, J.; Qin, X.; Shi, X.; Zeng, Q.; Liu, J.; Yan, S.; Zhang, L. Diosgenininduced autophagy and apoptosis in a human prostate cancer cell line. Mol. Med. Rep. 2016, 14, 4349–4359.
- Silva, V.A.O.; Rosa, M.N.; Tansini, A.; Oliveira, R.J.S.; Martinho, O.; Lima, J.P.; Pianowski, L.F.; Reis, R.M. In vitro screening of cytotoxic activity of euphol from Euphorbia tirucalli on a large panel of human cancer-derived cell lines. Exp. Ther. Med. 2018, 16, 557–566.
- Guo, Y.X.; Lin, Z.M.; Wang, M.J.; Dong, Y.W.; Niu, H.M.; Young, C.Y.; Lou, H.X.; Yuan, H.Q. Jungermannenone a and b induce ros-and cell cycle-dependent apoptosis in prostate cancer cells in vitro. Acta Pharmacol. Sin. 2016, 37, 814–824.
- Sun, S.; Liu, J.; Zhou, N.; Zhu, W.; Dou, Q.P.; Zhou, K. Isolation of three new annonaceous acetogenins from graviola fruit (Annona muricata) and their anti-proliferation on human prostate cancer cell pc-3. Bioorg. Med. Chem. Lett. 2016, 26, 4382–4385.
- Younis, T.; Khan, M.I.; Khan, M.R.; Rasul, A.; Majid, M.; Adhami, V.M.; Mukhtar, H. Nummularic acid, a triterpenoid, from the medicinal plant Fraxinus xanthoxyloides, induces energy crisis to suppress growth of prostate cancer cells. Mol. Carcinog. 2018, 57, 1267–1277.
- Singh, S.; Dubey, V.; Singh, D.K.; Fatima, K.; Ahmad, A.; Luqman, S. Antiproliferative and antimicrobial efficacy of the compounds isolated from the roots of Oenothera biennis L. J. Pharm. Pharmacol. 2017, 69, 1230–1243.
- Akhtar, N.; Syed, D.N.; Khan, M.I.; Adhami, V.M.; Mirza, B.; Mukhtar, H. The pentacyclic triterpenoid, plectranthoic acid, a novel activator of ampk induces apoptotic death in prostate cancer cells. Oncotarget 2016, 7, 3819–3831.
- Piao, L.; Canguo, Z.; Wenjie, L.; Xiaoli, C.; Wenli, S.; Li, L. Lipopolysaccharides-stimulated macrophage products enhance withaferin a-induced apoptosis via activation of caspases and inhibition of nf-kappab pathway in human cancer cells. Mol. Immunol. 2017, 81, 92–101.
- Perabo, F.G.E.; von Löw, E.C.; Siener, R.; Ellinger, J.; Müller, S.C.; Bastian, P.J. [a critical assessment of phytotherapy for prostate cancer]. Urol. A 2009, 48, 270–271, 274–283.
- Wu, C.Y.; Yang, Y.H.; Lin, Y.Y.; Kuan, F.C.; Lin, Y.S.; Lin, W.Y.; Tsai, M.Y.; Yang, J.J.; Cheng, Y.C.; Shu, L.H.; et al. Anti-cancer effect of danshen and dihydroisotanshinone i on prostate cancer: Targeting the crosstalk between macrophages and cancer cells via inhibition of the stat3/ccl2 signaling pathway. Oncotarget 2017, 8, 40246–40263.
- Liu, J.-M.; Lin, P.-H.; Hsu, R.-J.; Chang, Y.-H.; Cheng, K.-C.; Pang, S.-T.; Lin, S.-K. Complementary traditional chinese medicine therapy improves survival in patients with metastatic prostate cancer. Medicine 2016, 95, e4475.
- Pantuck, A.J.; Leppert, J.T.; Zomorodian, N.; Aronson, W.; Hong, J.; Barnard, R.J.; Seeram, N.; Liker, H.; Wang, H.; Elashoff, R.; et al. Phase ii study of pomegranate juice for men with rising prostate-specific antigen following surgery or radiation for prostate cancer. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2006, 12, 4018–4026.
- Pantuck, A.J.; Leppert, J.T.; Zomorodian, N.; Seeram, N.; Seiler, D.; Liker, H.; Wang, H.-j.; Elashoff, R.; Heber, D.; Belldegrun, A.S. 831: Phase ii study of pomegranate juice for men with rising PSA following surgery or radiation for prostate cancer. J. Urol. 2005, 173, 225–226.
- Paller, C.J.; Ye, X.; Wozniak, P.J.; Gillespie, B.K.; Sieber, P.R.; Greengold, R.H.; Stockton, B.R.; Hertzman, B.L.; Efros, M.D.; Roper, R.P.; et al. A randomized phase ii study of pomegranate extract for men with rising psa following initial therapy for localized prostate cancer. Prostate Cancer Prostatic Dis. 2013, 16, 50–55.
- Thomas, R.; Williams, M.; Sharma, H.; Chaudry, A.; Bellamy, P. A double-blind, placebo-controlled randomised trial evaluating the effect of a polyphenol-rich whole food supplement on psa progression in men with prostate cancer—The UK NCRN pomi-t study. Prostate Cancer Prostatic Dis. 2014, 17, 180.
- Kjaer, T.N.; Ornstrup, M.J.; Poulsen, M.M.; Jorgensen, J.O.; Hougaard, D.M.; Cohen, A.S.; Neghabat, S.; Richelsen, B.; Pedersen, S.B. Resveratrol reduces the levels of circulating androgen precursors but has no effect on, testosterone, dihydrotestosterone, psa levels or prostate volume. A 4-month randomised trial in middle-aged men. Prostate 2015, 75, 1255–1263.
- Paller, C.J.; Rudek, M.A.; Zhou, X.C.; Wagner, W.D.; Hudson, T.S.; Anders, N.; Hammers, H.J.; Dowling, D.; King, S.; Antonarakis, E.S.; et al. A phase i study of muscadine grape skin extract in men with biochemically recurrent prostate cancer: Safety, tolerability, and dose determination. Prostate 2015, 75, 1518–1525.
- De La Taille, A.; Buttyan, R.; Hayek, O.; Bagiella, E.; Shabsigh, A.; Burchardt, M.; Burchardt, T.; Chopin, D.K.; Katz, A.E. Herbal therapy pc-spes: In vitro effects and evaluation of its efficacy in 69 patients with prostate cancer. J. Urol. 2000, 164, 1229–1234.




