Prostate cancer is a heterogeneous disease, the second deadliest malignancy in men and the most commonly diagnosed cancer among men. Traditional plants have been applied to handle various diseases and to develop new drugs. Medicinal plants are potential sources of natural bioactive compounds that include alkaloids, phenolic compounds, terpenes, and steroids.
- prostate cancer
- medicinal plants
- phytotherapy
- secondary metabolites
- plant formulas
1. Introduction
1.1. A Brief Overview on Prostate Cancer
1.2. Prostate Cancer: Main Risk Factors
1.2.1. Non-Modified Risk Factors
Risk Group | Relative Risk of Prostate Cancer | ||||
|---|---|---|---|---|---|
Father and brother had prostate cancer | 9 | ||||
[ | |||||
] | |||||
-, no effect observed; +, positive effect.
4. Evidence from Clinical Studies
Phytochemicals/Formulae | Bioactive Effect | Reference | ||||||
|---|---|---|---|---|---|---|---|---|
≥2 first degree relatives having prostate cancer | 4.39 | |||||||
Brothers having prostate cancer | 3.14 | |||||||
First degree relative with prostate cancer at the age of<65 | 2.87 | |||||||
Second degree relative with prostate cancer | 2.52 | |||||||
One first degree relative with prostate cancer | 2.48 | |||||||
Father having prostate cancer | 2.35 | |||||||
First degree relative with prostate cancer at the age of ≥65 | 1.92 |
1.2.2. Modified Risk Factors
2. Therapeutic Strategies: A Brief Summary
Risk Group | Clinical Stage | PSA (ng/mL) | Gleason Score | Biopsy Criteria | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Low | ||||||||||||||||||
Danshen (Salvia miltiorrhiza) | T1a or T1c | Protective effects; Improved survival (5–10%)<10 | 2–6 |
[Unilateral or <50% of core involved | ||||||||||||||
] |
[266] |
Intermediate | T1b, T1c, or T2a | <10 | 3 + 4 = 7 | Bilateral | ||||||||||||
High | T1b, T1c, T2b, or T3 | 10–20 | 4 + 3 = 7 | >50% of core involved or perineural invasion or ductal differentiation | ||||||||||||||
Very high | T4 | >20 | 8–10 | Lymphovascular invasion or neuroendocrine differentiation |
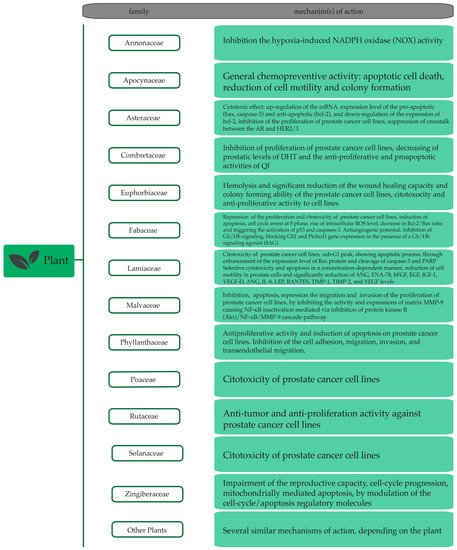
3. Plant Extracts and Plant-Derived Bioactives in Prostate Cancer
3.1. Plant Extracts with Anti-Prostate Cancer Potential
Plant Species | Family | In Vitro | In Vivo |
|---|
3.2. Plant-Derived Bioactives with Anti-Prostate Cancer Potential
Bioactive Compounds | In Vitro | In Vivo | References | References | |||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
Acacia catechu | Fabaceae | + | - |
[110] |
|||||||||||||||||||||||
Achillea santolinoides | Asteraceae | ||||||||||||||||||||||||||
(−)-Anonaine | + | ||||||||||||||||||||||||||
TCM formulae (Chai-Hu-Jia-Long-Gu-Mu-Li-Tang) | + | Improved survival | - | - |
[ |
[257] |
[267] | 176] |
[182] [111] |
||||||||||||||||||
Achillea teretifolia | Asteraceae | ||||||||||||||||||||||||||
(−)-Caaverine | + | + | - | - |
[176] |
[112] |
|||||||||||||||||||||
[ | ] |
Allium wallichii | |||||||||||||||||||||||||
(−)-Nuciferine | Amaryllidaceae | + | - |
[ |
+ | - |
[176] |
[182] 113] |
|||||||||||||||||||
Aloe perryi | Xanthorrhoeaceae | + | - |
[114] |
|||||||||||||||||||||||
6-Hydroxycrinamine | + | - |
[177] |
[183] |
Anaxagorea brevipes | ||||||||||||||||||||||
7-Hydroxydehydronuciferine | Annonaceae | + | + | - | - |
[176] |
[182 [115] |
||||||||||||||||||||
] | Angelica gigas | Apiaceae | - | ||||||||||||||||||||||||
Capsaicin | + | - | + |
[178] |
[184] | ||||||||||||||||||||||
Annona muricata | Annonaceae | ||||||||||||||||||||||||||
Crinamine | + | + | - | - |
[177] |
[183] [118] |
|||||||||||||||||||||
Anogeissus latifolia | Combretaceae | ||||||||||||||||||||||||||
Emetine | + | + | - | + |
[110] |
||||||||||||||||||||||
Apocynum venetum | |||||||||||||||||||||||||||
Liriodenine | Apocynaceae | + | + | - | - |
[176] |
[ [119] |
||||||||||||||||||||
] | Arachis hypogaea | ||||||||||||||||||||||||||
Lycorine | Fabaceae | + | + | - | + |
[120] |
|||||||||||||||||||||
Baliospermum montanum | Euphorbiaceae | + | |||||||||||||||||||||||||
Matrine | + | - | + |
[182] |
[121] |
||||||||||||||||||||||
[ | 188] |
Berberis libanotica | Berberidaceae | ||||||||||||||||||||||||
Oxymatrine | + | - | + |
[ |
- |
122] |
|||||||||||||||||||||
[ | ] |
[188] |
Byrsonima crassifolia | Malpighiaceae | + | ||||||||||||||||||||||
Oxysophocarpine | + | - | - |
[182] |
[123] |
||||||||||||||||||||||
[ | ] | Calliandra portoricensis | Fabaceae | + | - | ||||||||||||||||||||||
Schisanspheninal A | [124] |
||||||||||||||||||||||||||
+ | - |
[183] |
[189] |
Capsicum chinense | Solanaceae | + | - |
[123] |
|||||||||||||||||||
Sophocarpine | + | - |
[182] |
[188] |
Carica papaya | Caricaceae | |||||||||||||||||||||
Tetrandrine | + | + | - | - |
[184] |
[190] |
[125] |
||||||||||||||||||||
Cascabela peruviana | Apocynaceae | + | - |
[126] |
|||||||||||||||||||||||
Chenopodium hybridum | Amaranthaceae | + | - |
[127] |
|||||||||||||||||||||||
Cnidoscolus chayamansa | Euphorbiaceae | + | - |
[123] |
|||||||||||||||||||||||
Cornus mas | Cornaceae | + | - |
[128] |
|||||||||||||||||||||||
Costus pulverulentus | Costaceae | + | - |
[129] |
|||||||||||||||||||||||
Crataegus Pinnatifida | Rosaceae | + | - |
[130] |
|||||||||||||||||||||||
Crocus sativus | Iridaceae | + | + | ||||||||||||||||||||||||
Curcuma longa | Zingiberaceae | + | - |
[131 | |||||||||||||||||||||||
10-Gingerol | + | - |
[175] |
||||||||||||||||||||||||
6-Gingerol | + | ||||||||||||||||||||||||||
Phyllanthaceae | |||||||||||||||||||||||||||
+ | |||||||||||||||||||||||||||
- | |||||||||||||||||||||||||||
[ | |||||||||||||||||||||||||||
] | |||||||||||||||||||||||||||
Plumbago zeylanica | Plumbaginaceae | + | |||||||||||||||||||||||||
Carotenoids | |||||||||||||||||||||||||||
Crocetin | + | - |
[133] |
||||||||||||||||||||||||
Crocin | + | - |
[132] |
||||||||||||||||||||||||
Fatty acid | ][134] | ||||||||||||||||||||||||||
Cymbopogon citratus | Poaceae | + | - |
[135] |
|||||||||||||||||||||||
Cymbopogon giganteus | Poaceae | + | - |
[135] |
|||||||||||||||||||||||
Euphorbia microsciadia | Euphorbiaceae | + | - |
[111] |
|||||||||||||||||||||||
Euphorbia szovitsii | Euphorbiaceae | + | - |
[111] |
|||||||||||||||||||||||
Eurycoma longifolia | Simaroubaceae | + | - | + |
[175] [136] |
||||||||||||||||||||||
Fagara zanthoxyloides | Rutaceae | ||||||||||||||||||||||||||
6-Prenylnaringenin | + | + | - | - |
[188] |
[194] [137] |
|||||||||||||||||||||
Fagopyrum esculentum | Polygonaceae | ||||||||||||||||||||||||||
6-Shogoal | + | + | - | - |
[175] [138] |
||||||||||||||||||||||
Fagopyrum tataricum | Polygonaceae | + | - |
[138] |
|||||||||||||||||||||||
Ficus deltoidea var. angustifolia | Moraceae | + | - |
[139] |
|||||||||||||||||||||||
Ficus deltoidea var. deltoidea | Moraceae | + | - | - |
[155] |
||||||||||||||||||||||
Polygonatum sp | Asparagaceae | + | - |
[156] |
|||||||||||||||||||||||
Pseudocedrela kotchyi | Meliaceae | + | - |
[137] |
|||||||||||||||||||||||
Psidium guajava | Myrtaceae | + | + |
[138]] | |||||||||||||||||||||||
(E)-ethyl 8-methylnon-6-enoate | + | - |
[123] |
||||||||||||||||||||||||
Phenolic compounds | |||||||||||||||||||||||||||
α-Mangostin | + | + |
[185] |
[191]. |
|||||||||||||||||||||||
γ-Tocopherol | + | - |
[186] |
[192] |
|||||||||||||||||||||||
δ-Tocotrienol | + | - |
[186] |
[192] |
|||||||||||||||||||||||
(-)-5,7-Difluoroepicatechin-3-O-gallate | + | - |
[187] |
[193] |
|||||||||||||||||||||||
(-)-Epicatechin-3-O-gallate | + | - |
[187] |
[193] | |||||||||||||||||||||||
7-o-Galloyl catechin | + | - |
[189] |
[195] |
|||||||||||||||||||||||
8-Gingerol | + | - |
[175] |
||||||||||||||||||||||||
8-Prenylnaringenin | + |
[139] |
|||||||||||||||||||||||||
- |
[188] |
[194] |
Formosa lambsquarters | ||||||||||||||||||||||||
Afzelin | Amaranthaceae | + | - | + |
[138] |
||||||||||||||||||||||
- |
[190] |
[196] |
Glycine max | Fabaceae | + | - |
[140] |
||||||||||||||||||||
Altholactone | + | - |
[191] |
[197] |
Glycyrrhiza uralensis | Fabaceae | + | ||||||||||||||||||||
Apigenin | + | - |
[192] |
[198] [141] |
|||||||||||||||||||||||
Haplophyllum perforatum | |||||||||||||||||||||||||||
Camptothin B | Rutaceae | + | + | - | - |
[141] [111] |
|||||||||||||||||||||
Helicteres hirsuta | |||||||||||||||||||||||||||
Catechin | Malvaceae | + | + | - | - |
[189] |
[ [142] |
||||||||||||||||||||
] | Hertia angustifolia | Asteraceae | + | - |
[111] |
||||||||||||||||||||||
Catechin-3-o-gallate | + | - |
[189] |
[195] |
Hibiscus sabdariffa | Malvaceae | + | + | |||||||||||||||||||
Chlorogenic acid | + | - |
[130] [143] |
||||||||||||||||||||||||
Leucaena leucocephala | Fabaceae | + | |||||||||||||||||||||||||
Chrysin | + | - | - | ||||||||||||||||||||||||
] | [199] |
Lysimachia ciliata | Primulaceae | ||||||||||||||||||||||||
Cinnamaldehyde | + | + | - | - |
[194] |
[200] [144] |
|||||||||||||||||||||
Malmea depressa | Annonaceae | ||||||||||||||||||||||||||
Cornusiin A | + | + | - | - |
[141] [123] |
||||||||||||||||||||||
Maytenus royleana | |||||||||||||||||||||||||||
Cornusiin H | Celastraceae | + | + | - | + |
[145] |
|||||||||||||||||||||
[ | ] |
Medicago sativa | |||||||||||||||||||||||||
Curcumin | Fabaceae | + | + | - | + |
[111] |
|||||||||||||||||||||
Melissa officinalis | Lamiaceae | + | - |
[146] | |||||||||||||||||||||||
Decursin | + | [ |
- |
[117] | 147] | ||||||||||||||||||||||
Mentha arvensis | Lamiaceae | + | ] |
||||||||||||||||||||||||
Decursinol angelate | + | - | - |
[ |
|||||||||||||||||||||||
Mentha spicata | Lamiaceae | ||||||||||||||||||||||||||
Dehydrozingerone | + | + | - | - |
[199] |
[205] [148] |
|||||||||||||||||||||
Mentha viridis | Lamiaceae | ||||||||||||||||||||||||||
Delphinidin | + | + | - | + |
[148] |
||||||||||||||||||||||
Moringa oleifera | |||||||||||||||||||||||||||
Ellagic acid | Moringaceae | + | + | + | - |
[110] |
|||||||||||||||||||||
Nepeta cataria | Lamiaceae | + | - | ||||||||||||||||||||||||
Eugenol | + | - |
[194] |
[200] [149] |
|||||||||||||||||||||||
Nigella sativa | Ranunculaceae | + | |||||||||||||||||||||||||
Fisetin | + | - | + | [ |
[204] |
[210] | |||||||||||||||||||||
Oryza sativa | Poaceae | ||||||||||||||||||||||||||
Flavokawain A | + | + | + | - |
[205] |
[151] |
|||||||||||||||||||||
[ | ] |
Paeonia lactiflora | |||||||||||||||||||||||||
Flavopiridol | Paeoniaceae | + | - | + | + |
[206] |
[152]. |
||||||||||||||||||||
[ | ] |
Paramignya trimera | Rutaceae | + | |||||||||||||||||||||||
Garcinol | + | - | + |
[153] |
|||||||||||||||||||||||
Phyllanthus amarus | |||||||||||||||||||||||||||
Ginkgetin | Phyllanthaceae | + | + | + | - |
[209] |
[215] [154] |
||||||||||||||||||||
Phyllanthus niruri | Phyllanthaceae | + | - | ||||||||||||||||||||||||
Hesperetin | [154] |
||||||||||||||||||||||||||
+ | - |
[210] |
[216] |
Phyllanthus urinaria | Phyllanthaceae | ||||||||||||||||||||||
Hirsutenone | + | + | - | - |
[211] |
[217] [154] |
|||||||||||||||||||||
Phyllanthus watsonii | |||||||||||||||||||||||||||
HLBT-100 or HLBT-001 (5,3′-dihydroxy- 6,7,8,4′-tetramethoxyflavanone) | + | - |
[212] |
[218] |
|||||||||||||||||||||||
Honokiol | + | - |
[213] |
[219] |
|||||||||||||||||||||||
Icarisid II | + | - |
[214] |
[220] |
|||||||||||||||||||||||
Isoangustone A | + | - | |||||||||||||||||||||||||
Isovitexin | + | - |
[139] |
Punica granatum | |||||||||||||||||||||||
Juglone | Lythraceae | + | + | - | + |
[217] |
[223] | ||||||||||||||||||||
Quisqualis indica | Combretaceae | ||||||||||||||||||||||||||
Licoricidin | + | + | - | + |
[162] |
||||||||||||||||||||||
[ | , | 222] |
Remotiflori radix | Campanulaceae | |||||||||||||||||||||||
Magnolol | + | + | + |
[ |
- |
163] |
|||||||||||||||||||||
[ | ] |
[224] |
Salvia multicaulis Vahl | Lamiaceae | + | ||||||||||||||||||||||
Mangiferin | - | + |
[111] |
||||||||||||||||||||||||
+ | Salvia trilobal | Lamiaceae | + | - |
[ | ||||||||||||||||||||||
Maysin | + |
164] |
|||||||||||||||||||||||||
- |
[221] |
[227] |
Sigesbeckia orientalis | Asteraceae | |||||||||||||||||||||||
Methyl gallate | + | + | - | - |
[189] |
[ | + | + |
[224] |
[230] |
|||||||||||||||||
Peperotetraphin | + | - |
[225] |
[231] |
|||||||||||||||||||||||
Physangulatins I | + | - |
[226] |
[ | |||||||||||||||||||||||
Pomegranate juice | Extension of PSA doubling time, with no adverse effects | ||||||||||||||||||||||||||
[ | ][260] | 195] [165] |
|||||||||||||||||||||||||
Sophora alopecuroides | |||||||||||||||||||||||||||
Osthol | Fabaceae | + | + | - | - |
[111] |
|||||||||||||||||||||
] | Sutherlandia frutescens | Fabaceae | + | + |
[166] |
||||||||||||||||||||||
Terminalia bellerica | |||||||||||||||||||||||||||
Oxyfadichalcones A | + | - |
[223] |
[229] |
Combretaceae | ||||||||||||||||||||||
Oxyfadichalcones B | + | + | - | - |
[223] |
[229] [110] |
|||||||||||||||||||||
Terminalia catappa | Combretaceae | ||||||||||||||||||||||||||
Oxyfadichalcones C | + | + | - | - |
[223] |
[229] [123] |
|||||||||||||||||||||
Urtica dioica | |||||||||||||||||||||||||||
Oxyfadichalcones D | Urticaceae | + | + | - | - | Plumbagin | + | + | |||||||||||||||||||
Punicalagin | + | - |
[228] |
[234] |
|||||||||||||||||||||||
Quercetin | + | + | |||||||||||||||||||||||||
Resveratrol | + | + | |||||||||||||||||||||||||
Pomegranate, green tea, broccoli, turmeric | Decreased PSA levels |
[261] |
[271] |
||||||||||||||||||||||||
Resveratrol | Decreased the circulating levels of androgen precursors |
[262] |
[223] |
[229] | |||||||||||||||||||||||
Vitis rotundifolia | |||||||||||||||||||||||||||
Oxyfadichalcones E | Vitaceae | + | + | - | - |
[223] |
[229] [168] |
||||||||||||||||||||
Wedelia chinensis | Asteraceae | - | + | ||||||||||||||||||||||||
Alkaloids | |||||||||||||||||||||||||||
Oxyfadichalcones F | |||||||||||||||||||||||||||
+ | |||||||||||||||||||||||||||
- | |||||||||||||||||||||||||||
[ | |||||||||||||||||||||||||||
] | |||||||||||||||||||||||||||
[ | |||||||||||||||||||||||||||
] | |||||||||||||||||||||||||||
] | |||||||||||||||||||||||||||
[ | |||||||||||||||||||||||||||
] | |||||||||||||||||||||||||||
[ | |||||||||||||||||||||||||||
Withania coagulans | |||||||||||||||||||||||||||
Oxyfadichalcones G | |||||||||||||||||||||||||||
Solanaceae | |||||||||||||||||||||||||||
+ | |||||||||||||||||||||||||||
- | |||||||||||||||||||||||||||
- | |||||||||||||||||||||||||||
+ | |||||||||||||||||||||||||||
[ | |||||||||||||||||||||||||||
] | |||||||||||||||||||||||||||
[ | |||||||||||||||||||||||||||
[ | |||||||||||||||||||||||||||
] | |||||||||||||||||||||||||||
] | |||||||||||||||||||||||||||
Xylopia aethiopica | Annonaceae | + | - |
[172] |
|||||||||||||||||||||||
Paeonol | Zanthoxyli fructus | Rutaceae | + | + |
[173] |
||||||||||||||||||||||
Zingiber officinale | Zingiberaceae | + | + |
[131] | |||||||||||||||||||||||
] | |||||||||||||||||||||||||||
[ | Rutin | + | - |
[235] |
[241] |
||||||||||||||||||||||
Tannic acid | + | - |
[236] |
[242] |
|||||||||||||||||||||||
Tricin | + | - |
[237] |
[243] |
|||||||||||||||||||||||
Xanthohumol | + | - | |||||||||||||||||||||||||
Protein | |||||||||||||||||||||||||||
[ | 273] |
] | [175] | Agglutinin | + | + |
[239] |
[245] |
|||||||||||||||||||
Diffusa cyclotide 1 | + | - |
[240] |
[246] |
|||||||||||||||||||||||
Diffusa cyclotide 2 | + | - |
[240] |
[246] |
|||||||||||||||||||||||
Diffusa cyclotide 3 | + | + |
[240] |
[246] |
|||||||||||||||||||||||
Lectin ConBr | + | - |
[241] |
[247] |
|||||||||||||||||||||||
Lectin ConM | + | - |
[241] |
[247] |
|||||||||||||||||||||||
Lectin DLasiL | + | - |
[241] |
[247] |
|||||||||||||||||||||||
Lectin DSclerL | + | - |
[241] |
[247] |
|||||||||||||||||||||||
Terpenoids | |||||||||||||||||||||||||||
α-Santalol | + | + | |||||||||||||||||||||||||
+ | |||||||||||||||||||||||||||
+ |
[246] |
[252] |
|||||||||||||||||||||||||
Citral | + | - |
[135] |
||||||||||||||||||||||||
Diosgenin | + | - |
[247] |
[253]. |
|||||||||||||||||||||||
Euphol | + | - |
[248] |
[254] |
|||||||||||||||||||||||
Isocuparenal | + | - |
[183] |
[189] |
|||||||||||||||||||||||
Jungermannenone A | + | - |
[249] |
[255] |
|||||||||||||||||||||||
Jungermannenone B | |||||||||||||||||||||||||||
Extension of PSA doubling time, with no adverse effects |
[263] |
[274] |
+: Showed in vitro or in vivo antiproliferative effect; -: Not found.
+ | ||||||||||
- | ||||||||||
[ | ||||||||||
] | ||||||||||
[ | ||||||||||
] | ||||||||||
Muricins M | ||||||||||
+ | ||||||||||
- | ||||||||||
[ | ||||||||||
] | ||||||||||
[ | ||||||||||
] | ||||||||||
Muricins N | ||||||||||
+ | ||||||||||
- | ||||||||||
PC-SPEC | Decreased PSA levels |
[264] |
[275] |
|||||||
[ | ||||||||||
] | ||||||||||
[ | ||||||||||
] | ||||||||||
4 | ||||||||||
S | ||||||||||
,5 | ||||||||||
R | ||||||||||
,9 | ||||||||||
S | ||||||||||
,10 | ||||||||||
R | ||||||||||
-Labdatrien-6,19-olide | ||||||||||
+ | ||||||||||
- | ||||||||||
[ | ||||||||||
] | ||||||||||
[ | ||||||||||
] | ||||||||||
(20R)-Dammarane-3β,12β,20,25-tetrol (25-OH-PPD) | + | + |
[244] |
[250] |
||||||
Andrographolide | + | + |
[245] |
[251] |
||||||
Celastrol | ||||||||||
[ | ||||||||||
] | ||||||||||
[ | ] |
|||||||||
Nummularic acid | + | - |
[251] |
[257] |
||||||
Oenotheralanosterol B | + | - |
[252] |
[258] |
||||||
Plectranthoic acid | + | - |
[253] |
[259] |
||||||
Sutherlandioside D | + | - |
[166]. |
|||||||
Widdaranal A | - |
[183] |
[189] |
|||||||
Widdaranal B | + | - |
[183] |
[189] |
||||||
Widdarol peroxide | + | - |
[183] |
[189] |
||||||
Withaferin A | + | - |
[254] |
