Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Benedetta Bussolati | + 2593 word(s) | 2593 | 2021-05-26 06:22:04 | | | |
| 2 | Dean Liu | -10 word(s) | 2583 | 2021-05-26 08:30:47 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Bussolati, B. Angiogenic Properties of Placenta-Derived EVs. Encyclopedia. Available online: https://encyclopedia.pub/entry/10089 (accessed on 08 February 2026).
Bussolati B. Angiogenic Properties of Placenta-Derived EVs. Encyclopedia. Available at: https://encyclopedia.pub/entry/10089. Accessed February 08, 2026.
Bussolati, Benedetta. "Angiogenic Properties of Placenta-Derived EVs" Encyclopedia, https://encyclopedia.pub/entry/10089 (accessed February 08, 2026).
Bussolati, B. (2021, May 26). Angiogenic Properties of Placenta-Derived EVs. In Encyclopedia. https://encyclopedia.pub/entry/10089
Bussolati, Benedetta. "Angiogenic Properties of Placenta-Derived EVs." Encyclopedia. Web. 26 May, 2021.
Copy Citation
Angiogenesis is one of the main processes that coordinate the biological events leading to a successful pregnancy, and its imbalance characterizes several pregnancy-related diseases, including preeclampsia. Intracellular interactions via extracellular vesicles (EVs) contribute to pregnancy’s physiology and pathophysiology, and to the fetal–maternal interaction.
extracellular vesicles
preeclampsia
angiogenesis
1. Introduction
Extracellular vesicles (EVs) have been established as a means of cellular communication and are involved in physiological and pathophysiological processes through the transfer of bioactive molecules such as proteins, RNAs and lipids [1]. EVs are released by all cell types and can be found in all body fluids. The subtype and composition of EVs are dependent on the route of EV generation and parental origin, respectively [2]. The content of EVs can be packaged based on signals received from other cells or environmental factors such as oxygen, glucose concentration and sheath stress. In pregnant women, trophoblast-derived EVs are found in the blood [3], amniotic fluid [4], and urine [5]. These EVs have placenta-specific markers such as HLA-G [6], syncytin-1 [7] and placental-type alkaline phosphatase (PLAP-1) [8]. Due to their small size, EVs can cross the placental barrier, thereby enabling feto–maternal communication throughout the pregnancy [9] (Figure 1). Given that EVs are involved in a wide range of processes, it is no surprise that they play an important role in pregnancy. EVs regulate various normal physiological processes during pregnancy, including implantation of the embryo by regulation of the endometrium, trophoblast invasion, immune regulation of maternal responses and spiral artery remodeling [10]. Changes in the total number, content, and bioactivity of EVs have been reported in pregnancy complications such as preeclampsia (PE) [11].
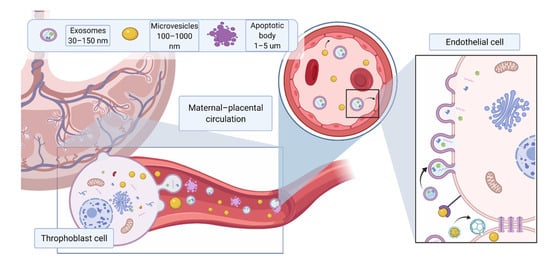
Figure 1. Different EV subtypes released from the placenta during pregnancy. The main subtypes of extracellular vesicles reported include exosomes (30–150 nm) formed from intracellular endosomal compartments and characterized by expression of tetraspanins (CD63, CD81, CD9); microvesicles (100 nm–1 μm), which originate from cell plasma membrane, characterized by CD 40; apoptotic bodies (>1 μm), which are released by apoptotic cells, express phosphatidylserine on their surface and caspase 3 and 7 internally. Due to their small size, EVs can cross the placental membrane and contribute to feto–maternal signaling. Placental EVs have been previously found in maternal circulation and shown to directly affect maternal endothelium. Created with BioRender.com (accessed on 18 May 2021).
Angiogenesis, the process by which blood vessels form for the delivery of nutrients to the body, is necessary both prior to and during pregnancy. A balance between pro and anti-angiogenic factors during pregnancy is key to a successful pregnancy. Imbalance of angiogenic factors, and subsequently, widespread endothelial dysfunction is considered the hallmark of pregnancy-related diseases such as preeclampsia (PE) [12]. The clinical manifestation of PE includes the development of hypertension after 20 weeks of gestation [13] and the coexistence of either proteinuria or other maternal organ dysfunction such as renal insufficiency, liver dysfunction, neurological features including headache or visual disturbances, hemolysis or thrombocytopenia, pulmonary edema [13][14][15]. Moreover, PE increases the risk of maternal and perinatal mortality and morbidity, and is associated with future cardiovascular disease risk [16]. Preeclampsia is classified as a new onset hypertensive pregnancy disorder. Depending on the time of delivery, early-onset preeclampsia manifests before the 34th week of gestation and is described as a fetal disorder that is associated with placental dysfunction and adverse fetal outcomes. Late-onset preeclampsia requires delivery at or after the 34th week of gestation and is considered as a maternal disorder associated with endothelial dysfunction and end organ damage [13].
Despite great scientific advances, PE is still defined as a “disease of theories”. Insufficient placenta development including abnormal spiral artery remodeling, placental hypoxia, oxidative stress, impaired angiogenesis and insufficient placental perfusion contribute to the development of preeclampsia [17][18][19]. Over the last two decades, increasing evidence suggests that angiogenic factors imbalance plays a pivotal role in PE pathogenesis [20][21]. Soluble fms-like tyrosine kinase 1 (sFlt-1), a soluble form of vascular endothelial growth factor receptor 1 (VEGFR-1) extracellular ligand-binding domain, is the key anti-angiogenic factor released by placenta during pregnancy. This soluble form of VEGFR-1 can bind to all isoforms of VEGF [22][23], as well as to the PlGF. Indeed, sFlt- 1 may act as a decoy receptor and hinder VEGF signaling through binding to its cognate receptors, thus inhibiting VEGF-mediated pro-angiogenic effects [24]. During normal pregnancy, the levels of sFlt-1 increase throughout gestation, providing a limiting and protective barrier for potentially unhealthy VEGF-dependent over signaling [25][26]. However, maternal circulating sFlt-1 levels are significantly increased in PE compared to normal pregnancy prior to the onset of the disease [27]. Furthermore, in vivo studies have showed that exogenous administration of sFlt-1 led to typical PE-like symptoms such as hypertension and glomerular endotheliosis in pregnant rats [20], whereas reduced circulating levels of free sFlt-1 below critical threshold rescued the damaging effects of sFlt-1 [21][28][29][30]. Another anti-angiogenic factor released by placenta is soluble endoglin (sEng), a soluble form of the coreceptor of transforming growth factor-β (TGF-β), which acts as a decoy receptor of TGF-β leading to a decrease in angiogenesis [31]. Not surprisingly, harmful molecules released from the placenta may reach the fetal circulation, causing endothelial dysfunction in the fetus. Indeed, many reports [32][33] have described fetoplacental endothelial dysfunction associated with preeclamptic pregnancies (Figure 1). A vicious cycle is therefore created, which is to the detriment of the mother and the fetus.
2. Pro-Angiogenic Functions of EVs in Healthy Pregnancy
The influence of EVs on the angiogenic process has been reported in various in vitro and in vivo studies [12]. EVs are considered to modulate the angiogenic process through the transfer of several molecules including small RNA species and proteins. In particular, small RNA species, such as microRNA, are transferred by EVs and are considered pivotal for the reprogramming of target cells [34]. Lombardo et al. reported that miRNA-126 and p-STAT5 in endothelial-derived EVs are responsible for IL-3-mediated paracrine pro-angiogenic signals [35]. Similarly, endothelial-derived exosomes require miRNA-214 to simulate angiogenesis in recipient cells [36]. In vivo, injection of EPC-derived EVs containing the angiogenic miRNAs miRNA-126 and miRNA-296 in a mouse hind limb ligation model significantly increased capillary density and blood perfusion [37]. Several other microRNAs present in the EV cargo have been reported to be involved in the induction of angiogenesis, including miRNA-125a [38], miR31 [39] and miRNA-150 [40]. In parallel, several proteins released by EVs have also been found to be involved in the modulation of angiogenesis, including VEGF [41][42], FGF-2 [43], PDGF [42][44][45], c-kit [46], sphingosine-1-phosphate [47], regulated on activation of normal T cell expression and secretion [47], CD40L [48], C-reactive protein [49][50][51], metalloproteases [48][52], stem cell factor [53], and urokinase-type plasminogen activator. Furthermore, EVs can promote angiogenesis through the transfer of key lipids and proteins involved in activation of PI3K [54], extracellular signal-regulated kinase 1 and 2 [55][56][57], Wnt4/βcatenin [58], and nuclear factor-κB [59][60] pathways.
In pregnancy, a large number of studies focus on the activity of EVs released by maternal and fetal cells, including endothelial cells, immune cells, trophoblast and stem cells with the latter being present in the umbilical cord, placenta, amniotic fluid and amniotic membranes (Figure 1). These EVs are capable of inducing tissue regeneration and angiogenesis and can be found in maternal circulation starting from 7 weeks of gestation [61], in amniotic fluid [4], and urine [5]. The heterogeneity of EVs produced in this environment results in a plethora of pro-angiogenic factors being delivered to support the physiological development of normal pregnancy and the maintenance of endothelial homeostasis (Table 1). The following paragraphs will discuss the role of healthy pregnancy-related EVs in angiogenesis, according to their different tissue types of origin.
Table 1. Angiogenic factors associated with EVs and their role in pregnancy.
| Source | Bio-Factor/Functional Assay | Platform | Reference |
|---|---|---|---|
| Umbilical cord blood | miRNA-15, miRNA-150 | In vitro | Luo et al., 2018 [44] |
| Umbilical cord | VEGF, VEGFR-2, MPC-1, angiogenin, tie-2/TEK and IGF | In vitro | (Xiong et al., 2018) [62] |
| Umbilical cord | Activation of Wnt/β-catenin pathway | In vitro | (Zhang et al., 2015) [58] |
| Placental explant EVs | Angiogenesis and migration | In vitro and in vivo | (Salomon et al., 2013) [63] |
| Trophoblast-EVs | EMMPRIN | In vitro and in vivo | (Balbi et al., 2019) [64] |
| Maternal–blood EVs | Shh | In vivo | (Martínez et al., 2006) [65] |
| Maternal–blood EVs | enhances endothelial cell proliferation, migration, and tube formation | In vitro | (Jia et al., 2018) [66] |
| Throphoblast-EVs | eNOS | In vitro | (Motta-Mejia et al., 2017) [67] |
| Placental explants | Flt/endoglin | In vitro | (D. Tannetta et al., 2014) [61] |
3. Anti-Angiogenic Actions of EVs in Preeclampsia
As discussed above, placental-derived EVs play an important physiological role in mother and fetus communication through the delivery of a range of proteins, lipids, and nucleic acids [68]. On the other hand, alterations in the concentration and content of placenta-derived EVs are associated with pregnancy-related diseases, such as PE [69][70][71][72][73]. Angiogenic imbalance is considered to be the main contributor of endothelial dysfunction, in PE [74]. Flt-1 and Eng have been detected on the surface of placental-derived EVs [3][69][75]. These Flt-1 and Eng expressing EVs are capable of binding to pro-angiogenic factors, VEGF, PlGF and TGF-β [69]. Interestingly, the capacity of Eng expressing placental-EVs to bind TGF-β was much higher in comparison to the affinity for VEGF and PlGF to Flt-1 expressing EVs [70].
The anti-angiogenic effect of circulating EVs in PE appears to be, at least in part, mediated by the presence of Flt-1 or Eng in the form of membrane receptors on the EV surface, as these can act as decoy receptors by sequestering angiogenic soluble factors, similarly to the presence of the soluble forms. Tannetta et al. [76] showed that EVs isolated from preeclamptic placenta expressed higher level of Flt-1 in comparison to EVs isolated from normal placenta. Application of EVs containing sFlt-1 to HUVEC cells led to a reduction in tube formation, cell invasion and an increase in cellular permeability [76]. EVs isolated from first trimester placental explants treated with sera from either normal pregnant women or preeclamptic women showed no significant differences in their size or concentration. However, EVs isolated from preeclamptic sera-treated placental explants were able to cause endothelial cell activation due to up-regulation of High Mobility Group Box 1 (HMGB1) in EVs, a potent danger-associated molecular pattern/danger signal that can lead to sterile inflammation [77]. Furthermore, administration of platelet or endothelial cell-derived EVs to pregnant mice induced PE-like symptoms and decreased embryonic vascularization [78]. Han et al. showed that infusion of EVs derived from injured placenta rather than normal placenta led to the development of hypertension and proteinuria in pregnant mice. These EVs released from injured placenta caused disruption of endothelial integrity and enhanced vasoconstriction [79]. These studies highlighted a possible pathogenic role of circulating EVs in PE. Studies in vivo have also confirmed the role of EVs in affecting angiogenesis and inducing PE-like syndromes by administering EVs derived from pre-eclamptic placentas in mice. The injection of those EVs resulted in damage to the vasculature and poor fetal nutrition [75].
The shedding of EVs into the maternal blood in PE has also been shown to correlate with systolic blood pressure [80]. Neprilysin (NEP), a membrane-bound metalloproteinase that is involved in vasodilator degradation, has been directly correlated with hypertension (REF). Interestingly, NEP has been found on the surface of trophoblast-EVs. Moreover, Gill et al. [81] showed that the level of NEP in the EVs derived from placenta and syncytiotrophoblast cells were both augmented in preeclamptic women compared to normal pregnant women, indicating that increased levels of NEP-expressing EVs in the maternal circulation may play a role in causing PE-related symptoms including hypertension, heart failure [81]. Furthermore, placental trophoblast-EVs in PE contain reduced levels of endothelial nitric oxide synthase (eNOS), and thus reduced production of nitric oxide production, a potent vasodilator (59), suggesting that PE-associated EVs may contribute to decreased NO bioavailability, resulting in endothelial dysfunction. Additionally, EVs may also inhibit angiogenesis by low-density lipoprotein receptor-mediated endocytosis [82], and by CD36-dependent uptake of EVs and induction of oxidative stress [83][84].
Not surprisingly, the majority of studies that have investigated EV in the development of PE have focused on the effect of placental EVs on the endothelium. Vascular smooth muscle cells residing in vessels are also an important part of the processes that lead to placentation and vascular remodeling. EVs from extravillous trophoblasts were reported to promote vascular smooth muscle cell migration, thus suggesting their role in the remodeling of spiral arteries [85]. However, the possible contribution of EVs on vascular smooth muscle cells in the pathophysiology of preeclampsia have not yet been researched.
Beside membrane-bound proteins, EVs derived from gestational tissues during complicated pregnancies contain multiple miRNAs, which may play an anti-angiogenic role under these conditions, particularly in PE [33]. Cronqvist et al. [86] demonstrated that syncytiotrophoblast-derived EVs directly transferred functional placental miRNA that directly targeted Flt-1 mRNA to primary human endothelial cells and subsequently regulated the expression of Flt-1, suggesting that miRNA enclosed in placental EVs may directly affect the maternal and fetal endothelial function through regulating angiogenic factors [86]. The miRNAs most commonly involved in angiogenic processes are outlined below (Table 2) [11]. For example, miRNA-210, which has an anti-angiogenesis property is actively secreted in placental-EVs. It has been found in the circulation of pregnant women and the level of miRNA-210 was elevated in women with PE and hypoxia [87]. In addition, EVs derived from trophoblast and endothelial cells contained miRNA-210 and its action may be mediated through directly targeting ERK [42]. miRNA-520c-3p, another miRNA found in trophoblast-EVs, can reduce invasiveness in cancerous cells [88][89]. Interestingly, Takahashi et al. [89] showed that MiRNA-520c-3p was present in first-trimester trophoblast cells and trophoblast cell lines and that overexpression of MiRNA-520c-3p in EVs significantly inhibited cell invasion by targeting CD44. The results showed that EVs produced by cells with miRNA-520c-3p overexpression significantly reduced invasiveness via repression of CD44. Moreover, several miRNAs which have been previously associated with hypertension have been found to be differentially expressed in preeclamptic EVs, including miRN26b-5p, miRNA-7-5p and miR181a-5p [90]. In addition, placental 19 miRNA cluster (C19MC), a cluster almost exclusively expressed on the placenta [91], has been reported to be altered in PE [88].
Table 2. Angiogenic factors associated with EVs and their role in pregnancy.
| Source of EVs | Bio-Factor/Functional Assay | Platform | Reference |
|---|---|---|---|
| Placental explants/trophoblast cell culture/maternal blood | s-Eng | in vitro and in vivo | (Chang et al., 2018) [92] |
| (Schuster et al., 2020) [74] | |||
| (D. S. Tannetta et al., 2013) [70] | |||
| (Salomon et al., 2014) [3] | |||
| Placental explants/trophoblast cell culture/maternal blood | s-Flt | in vitro and in vivo | (Chang et al., 2018) [75] |
| (Schuster et al., 2020) [74] | |||
| (D. S. Tannetta et al., 2013) [69] | |||
| (Salomon et al., 2014) [3] | |||
| Trophoblast EVs | NEP | In vitro | (Gill et al., 2019) [81] |
| Placental explants | VEGFR1/Endoglin | in vivo | (Tannetta et al. 2013) [76] |
| Placental explants | HMGB1 | In vitro | (Xiao et al.,2017) [77] |
| Placental explant | miRNA-210 | In vitro | (Anton et al., 2013) [87] |
| Placental explant | miRN26b-5p, miRNA-7-5p and miR181a-5p | In vitro | (Zhang et al., 2020) [90] |
| Placental explant | C19MC associated miRNA | In vitro | (Morelli et al., 2012) [88] |
| Maternal circulation | miRNA-486-1-5p, miRNA-486-2-5p | In vitro | (Salomon et al., 2013) [63] |
| Trophoblast EVs | miRNA-520c-3p | In vitro | (Takahashi et al., 2017) [89] |
| Serum derived EVs | Syncitin-2 | X | (Vargas et al., 2014) [7] |
Altogether, the studies described above suggest that EVs derived from preeclamptic placentas play a direct role in endothelial dysfunction and contribute to PE development through their membrane-bound proteins and the release of internal molecules such as anti-angiogenic proteins and miRNAs. However, recent studies have challenged these theories. It has been shown that EVs isolated using the common methods may cause contamination of soluble bioactive factors that may affect their resultant bioactivities [93]. O’Brien et al. [94] showed that placental explant-derived EVs had no significant effect on angiogenesis in vitro when EVs were administered alone, in contrast with the effect of EVs administered with conditioned medium. These data may suggest that the endothelial dysfunction associated with PE is linked with the action of soluble factors rather than EVs. To fully elucidate this point, future research on EVs bioactivity requires more stringent design and planning. Moreover, EVs from different sources must be researched on different platforms (in vitro, in vivo, organ on a chip) and on different functional assays (invasion, angiogenesis, apoptosis, etc.).
References
- Valadi, H.; Ekström, K.; Bossios, A.; Sjöstrand, M.; Lee, J.J.; Lötvall, J.O. Exosome-mediated transfer of mRNAs and microRNAs is a novel mechanism of genetic exchange between cells. Nat. Cell Biol. 2007, 9, 654–659.
- Börger, V.; Weiss, D.J.; Anderson, J.D.; Borràs, F.E.; Bussolati, B.; Carter, D.R.F.; Dominici, M.; Falcón-Pérez, J.M.; Gimona, M.; Hill, A.F.; et al. International Society for Extracellular Vesicles and International Society for Cell and Gene Therapy statement on extracellular vesicles from mesenchymal stromal cells and other cells: Considerations for potential therapeutic agents to suppress coronaviru. Cytotherapy 2020, 22, 482–485.
- Salomon, C.; Torres, M.J.; Kobayashi, M.; Scholz-Romero, K.; Sobrevia, L.; Dobierzewska, A.; Illanes, S.E.; Mitchell, M.D.; Rice, G.E. A gestational profile of placental exosomes in maternal plasma and their effects on endothelial cell migration. PLoS ONE 2014, 9, e98667.
- Ebert, B.; Rai, A.J. Isolation and characterization of amniotic fluid-derived extracellular vesicles for biomarker discovery. Methods Mol. Biol. 2019, 1885, 287–294.
- Hu, C.C.; Katerelos, M.; Choy, S.W.; Crossthwaite, A.; Walker, S.P.; Pell, G.; Lee, M.; Cook, N.; Mount, P.F.; Paizis, K.; et al. Pre-eclampsia is associated with altered expression of the renal sodium transporters NKCC2, NCC and ENaC in urinary extracellular vesicles. PLoS ONE 2018, 13, e0204514.
- Orozco, A.F.; Jorgez, C.J.; Ramos-Perez, W.D.; Popek, E.J.; Yu, X.; Kozinetz, C.A.; Bischoff, F.Z.; Lewis, D.E. Placental Release of Distinct DNA-associated Micro-particles into Maternal Circulation: Reflective of Gestation Time and Preeclampsia. Placenta 2009, 30, 891–897.
- Vargas, A.; Zhou, S.; Éthier-Chiasson, M.; Flipo, D.; Lafond, J.; Gilbert, C.; Barbeau, B. Syncytin proteins incorporated in placenta exosomes are important for cell uptake and show variation in abundance in serum exosomes from patients with preeclampsia. FASEB J. 2014, 28, 3703–3719.
- Germain, S.J.; Sacks, G.P.; Soorana, S.R.; Sargent, I.L.; Redman, C.W. Systemic Inflammatory Priming in Normal Pregnancy and Preeclampsia: The Role of Circulating Syncytiotrophoblast Microparticles. J. Immunol. 2007, 178, 5949–5956.
- Buca, D.; Bologna, G.; D’amico, A.; Cugini, S.; Musca, F.; Febbo, M.; D’arcangelo, D.; Buca, D.; Simeone, P.; Liberati, M.; et al. Extracellular vesicles in feto–maternal crosstalk and pregnancy disorders. Int. J. Mol. Sci. 2020, 21, 2120.
- Miranda, J.; Paules, C.; Nair, S.; Lai, A.; Palma, C.; Scholz-Romero, K.; Rice, G.E.; Gratacos, E.; Crispi, F.; Salomon, C. Placental exosomes profile in maternal and fetal circulation in intrauterine growth restriction-liquid biopsies to monitoring fetal growth. Placenta 2018, 64, 34–43.
- Mitchell, M.D.; Peiris, H.N.; Kobayashi, M.; Koh, Y.Q.; Duncombe, G.; Illanes, S.E.; Rice, G.E.; Salomon, C. Placental exosomes in normal and complicated pregnancy. Am. J. Obstet. Gynecol. 2015, 213, S173–S181.
- Todorova, D.; Simoncini, S.; Lacroix, R.; Sabatier, F.; Dignat-George, F. Extracellular vesicles in angiogenesis. Circ. Res. 2017, 120, 1658–1673.
- Brown, M.A.; Magee, L.A.; Kenny, L.C.; Karumanchi, S.A.; McCarthy, F.P.; Saito, S.; Hall, D.R.; Warren, C.E.; Adoyi, G.; Ishaku, S. Hypertensive disorders of pregnancy: ISSHP classification, diagnosis, and management recommendations for international practice. Hypertension 2018, 72, 24–43.
- Trogstad, L.; Magnus, P.; Stoltenberg, C. Pre-eclampsia: Risk factors and causal models. Best Pract. Res. Clin. Obstet. Gynaecol. 2011, 25, 329–342.
- Fatmeh, J.; Farahnaz, C. Seasonal variation in the prevalence of preeclampsia. J. Fam. Med. 2018, 6, 766–769.
- Scott, G.; Gillon, T.E.; Pels, A.; von Dadelszen, P.; Magee, L.A. Guidelines—Similarities and dissimilarities: A systematic review of international clinical practice guidelines for pregnancy hypertension. Am. J. Obstet. Gynecol. 2020.
- Ahmed, A.; Ramma, W. Unravelling the theories of pre-eclampsia: Are the protective pathways the new paradigm? Br. J. Pharmacol. 2015, 172, 1574–1586.
- Young, B.C.; Levine, R.J.; Karumanchi, S.A. Pathogenesis of preeclampsia. Annu. Rev. Pathol. Mech. Dis. 2010, 5, 173–192.
- Ramma, W.; Ahmed, A. Is inflammation the cause of pre-eclampsia. In Biochemical Society Transactions; Portland Press: Portland, ME, USA, 2011; Volume 39, pp. 1619–1627.
- Maynard, S.E.; Min, J.; Merchan, J.; Lim, K.-H.; Li, J.; Mondal, S.; Libermann, T.A.; Morgon, J.P.; Sellke, F.W.; Stillman, I.E.; et al. Excess placental soluble fms-like tyrosine kinase 1 (sFlt1) may contribute to endothelial dysfunction hypertension, and proteinuria in preeclampsia. J. Clin. Investig. 2003, 111, 649–658.
- Bergmann, A.; Ahmad, S.; Cudmore, M.; Gruber, A.D.; Wittschen, P.; Lindenmaier, W.; Christofori, G.; Gross, V.; Gonzalves, A.C.D.C.; Gröne, H.-J.; et al. Reduction of circulating soluble Flt-1 alleviates preeclampsia-like symptoms in a mouse model. J. Cell. Mol. Med. 2010, 14, 1857–1867.
- Kendall, R.L.; Thomas, K.A. Inhibition of vascular endothelial cell growth factor activity by an endogenously encoded soluble receptor. Proc. Natl. Acad. Sci. USA 1993, 90, 10705–10709.
- He, Y.; Smith, S.K.; Day, K.A.; Clark, D.E.; Licence, D.R.; Charnock-Jones, D.S. Alternative Splicing of Vascular Endothelial Growth Factor (VEGF)-R1 (FLT-1) pre-mRNA Is Important for the Regulation of VEGF Activity. Mol. Endocrinol. 1999, 13, 537–545.
- Mutter, W.P.; Karumanchi, S.A. Molecular mechanisms of preeclampsia. Microvasc. Res. 2008, 75, 1–8.
- Chen, D.; Wang, H.; Huang, H.; Dong, M. Vascular endothelial growth factor attenuates Nω-Nitro-L-arginine methyl ester-induced preeclampsia-like manifestations in rats. Clin. Exp. Hypertens. 2008, 30, 606–615.
- Sela, S.; Itin, A.; Natanson-Yaron, S.; Greenfield, C.; Goldman-Wohl, D.; Yagel, S.; Keshet, E. A novel human-specific soluble vascular endothelial growth factor receptor 1: Cell type-specific splicing and implications to vascular endothelial growth factor homeostasis and preeclampsia. Circ. Res. 2008, 102, 1566–1574.
- Levine, R.J.; Maynard, S.E.; Qian, C.; Lim, K.-H.; England, L.J.; Yu, K.F.; Schisterman, E.F.; Thadhani, R.; Sachs, B.P.; Epstein, F.H.; et al. Circulating Angiogenic Factors and the Risk of Preeclampsia. N. Engl. J. Med. 2004, 12, 672–683.
- Ahmed, A.; Rahman, M.; Zhang, X.; Acevedo, C.H.; Nijjar, S.; Rushton, I.; Bussolati, B.; St John, J. Induction of placental heme oxygenase-1 is protective against TNFalpha-induced cytotoxicity and promotes vessel relaxation. Mol. Med. 2000, 6, 391–409.
- Ahmad, S.; Ahmed, A. Elevated Placental Soluble Vascular Endothelial Growth Factor Receptor-1 Inhibits Angiogenesis in Preeclampsia. Circ. Res. 2004, 95, 884–891.
- Eddy, A.C.; Bidwell Iii, G.L.; George, E.M. Pro-angiogenic therapeutics for preeclampsia. Biol. Sex Differ. 2018, 9, 1–11.
- Lawera, A.; Tong, Z.; Thorikay, M.; Redgrave, R.E.; Cai, J.; Van Dinther, M.; Morrell, N.W.; Afink, G.B.; Charnock-Jones, D.S.; Arthur, H.M.; et al. Role of soluble endoglin in BMP9 signaling. Proc. Natl. Acad. Sci. USA 2019, 116, 17800–17808.
- Wadsack, C.; Desoye, G.; Hiden, U. The feto-placental endothelium in pregnancy pathologies. Wien. Med. Wochenschr. 2012, 162, 220–224.
- Escudero, C.A.; Herlitz, K.; Troncoso, F.; Acurio, J.; Aguayo, C.; Roberts, J.M.; Truong, G.; Duncombe, G.; Rice, G.; Salomon, C. Role of extracellular vesicles and microRNAs on dysfunctional angiogenesis during preeclamptic pregnancies. Front. Physiol. 2016, 7, 98.
- Deregibus, M.C.; Cantaluppi, V.; Calogero, R.; Lo Iacono, M.; Tetta, C.; Biancone, L.; Bruno, S.; Bussolati, B.; Camussi, G. Endothelial progenitor cell—Derived microvesicles activate an angiogenic program in endothelial cells by a horizontal transfer of mRNA. Blood 2007, 110, 2440–2448.
- Lombardo, G.; Dentelli, P.; Togliatto, G.; Rosso, A.; Gili, M.; Gallo, S.; Deregibus, M.C.; Camussi, G.; Brizzi, M.F. Activated Stat5 trafficking Via Endothelial Cell-derived Extracellular Vesicles Controls IL-3 Pro-angiogenic Paracrine Action. Sci. Rep. 2016, 6, 25689.
- Van Balkom, B.W.M.; De Jong, O.G.; Smits, M.; Brummelman, J.; Ouden, K.D.; De Bree, P.M.; Van Eijndhoven, M.A.J.; Pegtel, D.M.; Stoorvogel, W.; Würdinger, T.; et al. Endothelial cells require miR-214 to secrete exosomes that suppress senescence and induce angiogenesis in human and mouse endothelial cells. Blood 2013, 121, 3997–4006.
- Ranghino, A.; Cantaluppi, V.; Grange, C.; Vitillo, L.; Fop, F.; Biancone, L.; Deregibus, M.C.; Tetta, C.; Segoloni, G.P.; Camussi, G. TETTA Endothelial Progenitor Cell-Derived Microvesicles Improve Neovascularization In A Murine Model Of Hindlimb Ischemia. Int. J. Immunopathol. Pharmacol. 2012, 25, 75–85.
- Liang, X.; Zhang, L.; Wang, S.; Han, Q.; Zhao, R.C. Exosomes secreted by mesenchymal stem cells promote endothelial cell angiogenesis by transferring miR-125a. J. Cell Sci. 2016, 129, 2182–2189.
- Kang, T.; Jones, T.M.; Naddell, C.; Bacanamwo, M.; Calvert, J.W.; Thompson, W.E.; Bond, V.C.; Chen, Y.E.; Liu, D. Adipose-Derived Stem Cells Induce Angiogenesis via Microvesicle Transport of miRNA-31. Stem Cells Transl. Med. 2016, 5, 440–450.
- Liu, Y.; Zhao, L.; Li, D.; Yin, Y.; Zhang, C.Y.; Li, J.; Zhang, Y. Microvesicle-delivery miR-150 promotes tumorigenesis by up-regulating VEGF, and the neutralization of miR-150 attenuate tumor development. Protein Cell 2013, 4, 932–941.
- Zou, L.; Chen, Q.; Quanbeck, Z.; Bechtold, J.E.; Kaufman, D.S. Angiogenic activity mediates bone repair from human pluripotent stem cell-derived osteogenic cells. Sci. Rep. 2016, 6, 22868.
- Brill, A.; Dashevsky, O.; Rivo, J.; Gozal, Y.; Varon, D. Platelet-derived microparticles induce angiogenesis and stimulate post-ischemic revascularization. Cardiovasc. Res. 2005, 67, 30–38.
- Ahmed, A. Heparin-binding angiogenic growth factors in pregnancy. Placenta 1997, 18, 215–258.
- Luo, J.; Fan, Y.; Shen, L.; Niu, L.; Zhao, Y.; Jiang, D.; Zhu, L.; Jiang, A.; Tang, Q.; Ma, J.; et al. The pro-angiogenesis of exosomes derived from umbilical cord blood of intrauterine growth restriction pigs was repressed associated with MiRNAs. Int. J. Biol. Sci. 2018, 14, 1426–1436.
- Mamer, S.B.; Chen, S.; Weddell, J.C.; Palasz, A.; Wittenkeller, A.; Kumar, M.; Imoukhuede, P.I. Discovery of High-Affinity PDGF-VEGFR Interactions: Redefining RTK Dynamics. Sci. Rep. 2017, 7, 16439.
- Lopatina, T.; Bruno, S.; Tetta, C.; Kalinina, N.; Porta, M.; Camussi, G. Platelet-Derived Growth Factor Regulates the Secretion of Extracellular Vesicles by Adipose Mesenchymal Stem Cells and Enhances Their Angiogenic Potential; Springer: Berlin/Heidelberg, Germany, 2014.
- Ohtsuka, M.; Sasaki, K.-I.; Ueno, T.; Seki, R.; Nakayoshi, T.; Koiwaya, H.; Toyama, Y.; Yokoyama, S.; Mitsutake, Y.; Chibana, H.; et al. Platelet-derived microparticles augment the adhesion and neovascularization capacities of circulating angiogenic cells obtained from atherosclerotic patients. Atherosclerosis 2013, 227, 275–282.
- Leroyer, A.S.; Rautou, P.E.; Silvestre, J.S.; Castier, Y.; Lesèche, G.; Devue, C.; Duriez, M.; Brandes, R.P.; Lutgens, E.; Tedgui, A.; et al. CD40 Ligand+ Microparticles From Human Atherosclerotic Plaques Stimulate Endothelial Proliferation and Angiogenesis. A Potential Mechanism for Intraplaque Neovascularization. J. Am. Coll. Cardiol. 2008, 52, 1302–1311.
- Braig, D.; Nero, T.L.; Koch, H.G.; Kaiser, B.; Wang, X.; Thiele, J.R.; Morton, C.J.; Zeller, J.; Kiefer, J.; Potempa, L.A.; et al. Transitional changes in the CRP structure lead to the exposure of proinflammatory binding sites. Nat. Commun. 2017, 8, 14188.
- Turu, M.M.; Slevin, M.; Matou, S.; West, D.; Rodríguez, C.; Luque, A.; Grau-Olivares, M.; Badimon, L.; Martinez-Gonzalez, J.; Krupinski, J. C-reactive protein exerts angiogenic effects on vascular endothelial cells and modulates associated signalling pathways and gene expression. BMC Cell Biol. 2008, 9, 47.
- Habersberger, J.; Strang, F.; Scheichl, A.; Htun, N.; Bassler, N.; Merivirta, R.-M.; Diehl, P.; Krippner, G.; Meikle, P.; Eisenhardt, S.U.; et al. Circulating microparticles generate and transport monomeric C-reactive protein in patients with myocardial infarction. Cardiovasc. Res. 2012, 96, 64–72.
- Taraboletti, G.; D’Ascenzo, S.; Borsotti, P.; Giavazzi, R.; Pavan, A.; Dolo, V. Shedding of the matrix metalloproteinases MMP-2, MMP-9, and MT1-MMP as membrane vesicle-associated components by endothelial cells. Am. J. Pathol. 2002, 160, 673–680.
- Lacroix, M.; Caramel, J.; Goguet-Rubio, P.; Linares, L.; Estrach, S. Transcription factor E4F1 is essential for epidermal stem cell maintenance and skin homeostasis. Proc. Natl. Acad. Sci. USA 2010, 107, 21076–21081.
- Kim, S.Y.; Ryu, H.M.; Yang, J.H.; Kim, M.Y.; Ahn, H.K.; Lim, H.J.; Shin, J.S.; Woo, H.J.; Park, S.Y.; Kim, Y.M.; et al. Maternal Levels of Soluble Adhesion Molecules in Preeclampsia. J. Korean Med. Sci. 2004, 19, 688–692.
- Arderiu, G.; Espinosa, S.; Peña, E.; Aledo, R.; Badimon, L. PAR2–SMAD3 in microvascular endothelial cells is indispensable for vascular stability via tissue factor signaling. J. Mol. Cell Biol. 2016, 8, 255–270.
- Zhang, W.; Zhou, X.; Zhang, H.; Yao, Q.; Liu, Y.; Dong, Z. Extracellular vesicles in diagnosis and therapy of kidney diseases. Am. J. Physiol. Ren. Physiol. 2016, 311, F844–F851.
- Li, L.; Zhao, G.D.; Shi, Z.; Qi, L.L.; Zhou, L.Y.; Fu, Z.X. The Ras/Raf/MEK/ERK signaling pathway and its role in the occurrence and development of HCC. Oncol. Lett. 2016, 12, 3045–3050.
- Zhang, B.; Wu, X.; Zhang, X.; Sun, Y.; Yan, Y.; Shi, H.; Zhu, Y.; Wu, L.; Pan, Z.; Zhu, W.; et al. Human Umbilical Cord Mesenchymal Stem Cell Exosomes Enhance Angiogenesis Through the Wnt4/β-Catenin Pathway. Stem Cells Transl. Med. 2015, 4, 513–522.
- Anderson, J.D.; Johansson, H.J.; Graham, C.S.; Vesterlund, M.; Pham, M.T.; Bramlett, C.S.; Montgomery, E.N.; Mellema, M.S.; Bardini, R.L.; Contreras, Z.; et al. Comprehensive proteomic analysis of mesenchymal stem cell exosomes reveals modulation of angiogenesis via nuclear factor-kappaB signaling. Stem Cells 2016, 34, 601–613.
- Shabbir, A.; Cox, A.; Rodriguez-Menocal, L.; Salgado, M.; Van Badiavas, E. Mesenchymal Stem Cell Exosomes Induce Proliferation and Migration of Normal and Chronic Wound Fibroblasts, and Enhance Angiogenesis in Vitro. Stem Cells Dev. 2015, 24, 1635–1647.
- Tannetta, D.; Dragovic, R.; Alyahyaei, Z.; Southcombe, J. Extracellular vesicles and reproduction-promotion of successful pregnancy. Cell. Mol. Immunol. 2014, 11, 548–563.
- Xiong, Z.H.; Wei, J.; Lu, M.Q.; Jin, M.Y.; Geng, H.L. Protective effect of human umbilical cord mesenchymal stem cell exosomes on preserving the morphology and angiogenesis of placenta in rats with preeclampsia. Biomed. Pharm. 2018, 105, 1240–1247.
- Salomon, C.; Kobayashi, M.; Ashman, K.; Sobrevia, L.; Mitchell, M.D.; Rice, G.E. Hypoxia-induced changes in the bioactivity of cytotrophoblast-derived exosomes. PLoS ONE 2013, 8, e79636.
- Balbi, C.; Lodder, K.; Costa, A.; Moimas, S.; Moccia, F.; van Herwaarden, T.; Rosti, V.; Campagnoli, F.; Palmeri, A.; De Biasio, P.; et al. Reactivating endogenous mechanisms of cardiac regeneration via paracrine boosting using the human amniotic fluid stem cell secretome. Int. J. Cardiol. 2019, 287, 87–95.
- Martínez, M.C.; Larbret, F.; Zobairi, F.; Coulombe, J.; Debili, N.; Vainchenker, W.; Ruat, M.; Freyssinet, J.M. Transfer of differentiation signal by membrane microvesicles harboring hedgehog morphogens. Blood 2006, 108, 3012–3020.
- Jia, L.; Zhou, X.; Huang, X.; Xu, X.; Jia, Y.; Wu, Y.; Yao, J.; Wu, Y.; Wang, K. Maternal and umbilical cord serum-derived exosomes enhance endothelial cell proliferation and migration. FASEB J. 2018, 32, 4534–4543.
- Motta-mejia, C.; Kandzija, N.; Zhang, W.; Mhlomi, V.; Cerdeira, A.S.; Burdujan, A.; Tannetta, D.; Dragovic, R.; Sargent, I.L.; Redman, C.W.; et al. Preeclampsia Placental Vesicles Carry Active Endothelial Nitric Oxide Synthase and Their Activity is Reduced in Preeclampsia. Hypertension 2017, 70, 372–381.
- Tong, M.; Chamley, L.W. Isolation and characterization of extracellular vesicles from ex vivo cultured human placental explants. In Methods in Molecular Biology; Humana Press Inc.: Totowa, NJ, USA, 2018; Volume 1710, pp. 117–129.
- Attwood, H.D.; Park, W.W. Embolism to The Lungs By Trophoblast. BJOG Int. J. Obstet. Gynaecol. 1961, 68, 611–617.
- Chua, S.; Wilkins, T.; Sargent, I.; Redman, C. Trophoblast deportation in pre-eclamptic pregnancy. BJOG Int. J. Obstet. Gynaecol. 1991, 98, 973–979.
- Buurma, A.J.; Penning, M.E.; Prins, F.; Schutte, J.M.; Bruijn, J.A.; Wilhelmus, S.; Rajakumar, A.; Bloemenkamp, K.W.M.; Karumanchi, S.A.; Baelde, H.J. Preeclampsia is associated with the presence of transcriptionally active placental fragments in the maternal lung. Hypertension 2013, 62, 608–613.
- Goswamia, D.; Tannetta, D.S.; Magee, L.A.; Fuchisawa, A.; Redman, C.W.G.; Sargent, I.L.; von Dadelszen, P. Excess syncytiotrophoblast microparticle shedding is a feature of early-onset pre-eclampsia, but not normotensive intrauterine growth restriction. Placenta 2006, 27, 56–61.
- Chen, K.; Nishi, H.; Travers, R.; Tsuboi, N.; Martinod, K.; Wagner, D.D.; Stan, R.; Croce, K.; Mayadas, T.N. Endocytosis of soluble immune complexes leads to their clearance by FcγRIIIB but induces neutrophil extracellular traps via FcγRIIA in vivo. Blood 2012, 120, 4421–4431.
- Schuster, J.; Cheng, S.; Padbury, J.; Sharma, S. Placental extracellular vesicles and pre-eclampsia. Am. J. Reprod. Immunol. 2021, 85, e13297.
- Chang, C.C.; Sung, W.W.; Hsu, H.T.; Yeh, C.M.; Lee, C.H.; Chen, Y.L.; Liu, T.C.; Yeh, K.T. Validation of EGFL6 expression as a prognostic marker in patients with lung adenocarcinoma in Taiwan: A retrospective study. BMJ Open 2018, 8, e021385.
- Tannetta, D.S.; Dragovic, R.A.; Gardiner, C.; Redman, C.W.; Sargent, I.L. Characterisation of Syncytiotrophoblast Vesicles in Normal Pregnancy and Pre-Eclampsia: Expression of Flt-1 and Endoglin. PLoS ONE 2013, 8, e56754.
- Xiao, X.; Xiao, F.; Zhao, M.; Tong, M.; Wise, M.R.; Stone, P.R.; Chamley, L.W.; Chen, Q. Treating normal early gestation placentae with preeclamptic sera produces extracellular micro and nano vesicles that activate endothelial cells. J. Reprod. Immunol. 2017, 120, 34–41.
- Kohli, S.; Ranjan, S.; Hoffmann, J.; Kashif, M.; Daniel, E.A.; Al-Dabet, M.M.; Bock, F.; Nazir, S.; Huebner, H.; Mertens, P.R.; et al. Maternal extracellular vesicles and platelets promote preeclampsia via inflammasome activation in trophoblasts. Blood 2016, 128, 2153–2164.
- Han, C.; Wang, C.; Chen, Y.; Wang, J.; Xu, X.; Hilton, T.; Cai, W.; Zhao, Z.; Wu, Y.; Li, K.; et al. Placenta-derived extracellular vesicles induce preeclampsia in mouse models. Haematologica 2020, 105, 1686–1694.
- Lok, C.A.R.; Van Der Post, J.A.M.; Sargent, I.L.; Hau, C.M.; Sturk, A.; Boer, K.; Nieuwland, R. Changes in microparticle numbers and cellular origin during pregnancy and preeclampsia. Hypertens. Pregnancy 2008, 27, 344–360.
- Gill, M.; Motta-Mejia, C.; Kandzija, N.; Cooke, W.; Zhang, W.; Cerdeira, A.S.; Bastie, C.; Redman, C.; Vatish, M. Placental syncytiotrophoblast-derived extracellular vesicles carry active NEP (Neprilysin) and are increased in preeclampsia. Hypertension 2019, 73, 1112–1119.
- Pan, G.; Chen, D.; Xu, L.; Dong, X.; You, L.; Zhu, Z.; Zhang, H.; Hu, Y. Cardiac dysfunction in women with severe preeclampsia detected by tissue Doppler and speckle-tracking echocardiography. Int. J. Clin. Exp. Med. 2019, 12, 9245–9250.
- Ramakrishnan, P.; Maclean, M.; MacGregor, S.J.; Anderson, J.G.; Grant, M.H. Cytotoxic responses to 405 nm light exposure in mammalian and bacterial cells: Involvement of reactive oxygen species. Toxicol. In Vitro 2016, 33, 54–62.
- Yang, G.; Wu, L.; Jiang, B.; Yang, W.; Qi, J.; Cao, K.; Meng, Q.; Mustafa, A.K.; Mu, W.; Zhang, S.; et al. H2S as a Physiologic Vasorelaxant: Hypertension in Mice with Deletion of Cystathionine γ-Lyase. Science 2008, 322, 587–590.
- Salomon, C.; Sarah, Y.; Scholz-Romero, K.; Kobayashi, M.; Vaswani, K.; Kvaskoff, D.; Illanes, S.E.; Mitchell, M.D.; Rice, G.E. Extravillous trophoblast cells-derived exosomes promote vascular smooth muscle cell migration. Front. Pharmacol. 2014, 5, 175.
- Cronqvist, T.; Tannetta, D.; Mörgelin, M.; Belting, M.; Sargent, I.; Familari, M.; Hansson, S.R. Syncytiotrophoblast derived extracellular vesicles transfer functional placental miRNAs to primary human endothelial cells. Sci. Rep. 2017, 7, 4558.
- Anton, L.; Olarerin-George, A.O.; Schwartz, N.; Srinivas, S.; Bastek, J.; Hogenesch, J.B.; Elovitz, M.A. MiR-210 inhibits trophoblast invasion and is a serum biomarker for preeclampsia. Am. J. Pathol. 2013, 183, 1437–1445.
- Donker, R.B.; Mouillet, J.F.; Chu, T.; Hubel, C.A.; Stolz, D.B.; Morelli, A.E.; Sadovsky, Y. The expression profile of C19MC microRNAs in primary human trophoblast cells and exosomes. Mol. Hum. Reprod. 2012, 18, 417–424.
- Takahashi, H.; Ohkuchi, A.; Kuwata, T.; Usui, R.; Baba, Y.; Suzuki, H.; Chaw Kyi, T.T.; Matsubara, S.; Saito, S.; Takizawa, T. Endogenous and exogenous miR-520c-3p modulates CD44-mediated extravillous trophoblast invasion. Placenta 2017, 50, 25–31.
- Srinivasan, S.; Treacy, R.; Herrero, T.; Olsen, R.; Leonardo, T.R.; Zhang, X.; DeHoff, P.; To, C.; Poling, L.G.; Fernando, A.; et al. Discovery and Verification of Extracellular miRNA Biomarkers for Non-invasive Prediction of Pre-eclampsia in Asymptomatic Women. Cell Rep. Med. 2020, 1, 100013.
- Morales-Prieto, D.M.; Chaiwangyen, W.; Ospina-Prieto, S.; Schneider, U.; Herrmann, J.; Gruhn, B.; Markert, U.R. MicroRNA expression profiles of trophoblastic cells. Placenta 2012, 33, 725–734.
- Chang, X.; Yao, J.; He, Q.; Liu, M.; Duan, T.; Wang, K. Exosomes from women with preeclampsia induced vascular dysfunction by delivering sFLT (soluble fms-like tyrosine kinase)-1 and SENG (soluble endoglin) to endothelial cells. Hypertension 2018, 72, 1381–1390.
- Whittaker, T.E.; Nagelkerke, A.; Nele, V.; Kauscher, U.; Stevens, M.M. Experimental artefacts can lead to misattribution of bioactivity from soluble mesenchymal stem cell paracrine factors to extracellular vesicles. J. Extracell. Vesicles 2020, 9, 1807674.
- O’Brien, M.; Baczyk, D.; Kingdom, J.C. Endothelial Dysfunction in Severe Preeclampsia is Mediated by Soluble Factors, Rather than Extracellular Vesicles. Sci. Rep. 2017, 7, 5887.
More
Information
Subjects:
Cell Biology
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
734
Revisions:
2 times
(View History)
Update Date:
26 May 2021
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




