Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Fabio Del Bello | + 4101 word(s) | 4101 | 2021-07-14 10:45:35 | | | |
| 2 | Vivi Li | Meta information modification | 4101 | 2021-09-01 11:35:19 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Del Bello, F.; Giorgioni, G.; Quaglia, W. Levodopa/Receptor Ligands in Parkinson’s Disease. Encyclopedia. Available online: https://encyclopedia.pub/entry/13783 (accessed on 08 February 2026).
Del Bello F, Giorgioni G, Quaglia W. Levodopa/Receptor Ligands in Parkinson’s Disease. Encyclopedia. Available at: https://encyclopedia.pub/entry/13783. Accessed February 08, 2026.
Del Bello, Fabio, Gianfabio Giorgioni, Wilma Quaglia. "Levodopa/Receptor Ligands in Parkinson’s Disease" Encyclopedia, https://encyclopedia.pub/entry/13783 (accessed February 08, 2026).
Del Bello, F., Giorgioni, G., & Quaglia, W. (2021, September 01). Levodopa/Receptor Ligands in Parkinson’s Disease. In Encyclopedia. https://encyclopedia.pub/entry/13783
Del Bello, Fabio, et al. "Levodopa/Receptor Ligands in Parkinson’s Disease." Encyclopedia. Web. 01 September, 2021.
Copy Citation
Levodopa (LD) is the most effective drug in the treatment of Parkinson’s disease (PD). However, although it represents the “gold standard” of PD therapy, LD can cause side effects, including gastrointestinal and cardiovascular symptoms as well as transient elevated liver enzyme levels. Moreover, LD therapy leads to LD-induced dyskinesia (LID), a disabling motor complication that represents a major challenge for the clinical neurologist. Due to the many limitations associated with LD therapeutic use, other dopaminergic and non-dopaminergic receptor drugs, including serotoninergic, gluamatergic and noradrenergic receptor ligands, are being developed to optimize the treatment response.
Parkinson’s disease
levodopa therapy
levodopa-induced side effects
dopaminergic drugs
non-dopaminergic receptor ligands
1. Introduction
Parkinson’s disease (PD), also known as idiopathic paralysis agitans, is one of the most frequent chronic neurodegenerative diseases worldwide. Although its etiology has not been determined so far, the main pathological characteristic is the decrease of the dopamine (DA) level due to the degeneration of the dopaminergic neurons in the substantia nigra pars compacta [1][2]. This leads to motor (i.e., postural instability, dyskinesias, tremor, and rigidity) and non-motor (i.e., depression, cognitive impairment, pain, hallucinations) symptoms [3][4][5][6][7][8][9][10][11][12][13]. Another pathologically severe aspect is the abnormal formation of protein aggregates inside nerve cells (Lewy bodies), whose primary structural component is the presynaptic neuronal protein α-synuclein. For this reason, PD is classified as synucleopathy. Unfortunately, effective inhibition of progression or the cure for PD is not yet available, while all the available therapies only provide relief for symptoms.
Dopaminergic medications are currently the most effective treatment for both motor and non-motor symptoms, though they are not devoid of limitations and frequently produce undesired side effects. The standard treatment of PD patients consists in the administration of DA) in the form of levodopa (LD), a catecholamine produced by the intraneuronal tyrosine hydroxylation [14][15][16][17][18][19]. Its combination with a peripheral DOPA decarboxylase inhibitor (i.e., carbidopa) increases LD availability in the central nervous system (CNS) and ameliorates the therapeutic profile of LD, prolonging its efficacy [20][21][22]. An increase in the efficacy of dopaminergic therapy is also obtained by the simultaneous blockade of the DA metabolism with monoaminooxidase B (MAO-B) and/or catechol-O-methyl transferase (COMT) inhibitors [23][24]. Although LD represents the “gold standard” of PD therapy [25], unfortunately, orally administered LD can cause side effects, including gastrointestinal and cardiovascular symptoms as well as transient elevated liver enzyme levels. Moreover, LD therapy leads to LD-induced dyskinesia (LID) [26], a disabling motor complication that represents a major challenge for the clinical neurologist [27]. Indeed, LID negatively affects the quality of life [28][29][30] and constitutes a serious obstacle to the management of PD imposing a limit and a reduction of LD dosage, thus restricting treatment efficacy [27].
Numerous therapies are currently being developed to treat the motor and non-motor complications of PD and LID [31].
Mostly a customized combination of DA agonists and LD formulations is performed. The striatal D1 and D2 receptors are the common binding sites of DA ligands for PD treatment, but lately D3 and D4 subtypes have also become potential targets.
At the best of our knowledge, ten DA agonists are so far available for this disease. They can be listed in ergot DA agonists, including Bromocriptine, Cabergoline, Dihydroergocriptine, Lisuride, and Pergolide and non-ergot DA agonists, including Piribedil, Pramipexole, Ropinirole, Apomorphine, and Rotigotine [32] (Figure 1).
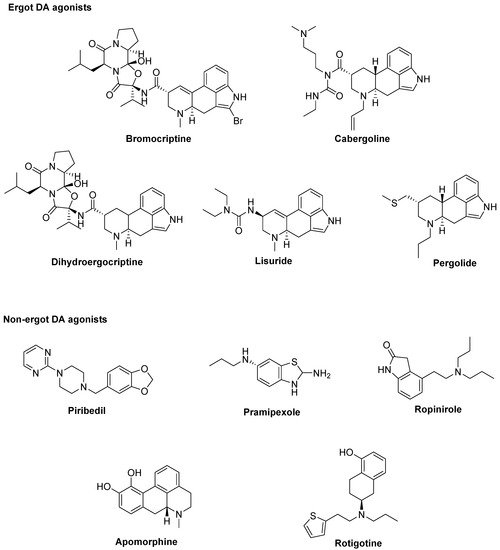
Figure 1. Dopamine (DA) agonists available for Parkinson’s disease (PD) treatment.
Unluckily, DA agonists are not devoid of significant side effects such as hallucinations, hypotension, nausea, vomiting, pathological gambling, compulsive shopping and hypersexuality [32][33]. As a therapeutic example, symptoms of early stage PD may be controlled by the treatment with Pramipexole [34], but after a while a combination with LD is needed to optimize the management of PD symptoms [35]. Thus, DA agonists are typically used either to reduce the dosage of LD or to delay its use (LD sparing) [36], although it has been discussed that dyskinesia evolvement is due to disease persistence rather than protracted LD use [37]. Recently, research on dopaminergic targets has produced some new interesting candidates (Figure 2).
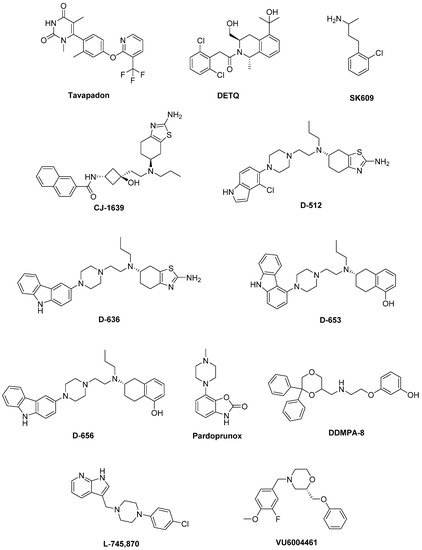
Figure 2. Emerging dopaminergic ligands as new levodopa (LD) adjuvant candidates.
Among these, Tavapadon (or PF-06649751) is a novel, highly selective D1/D5 agonist. A recent paper, reporting about Phase I PD studies, candidates Tavapadon as a novel therapeutic agent for PD with an initial safety, tolerability, and pharmacokinetic profile as well as potential for efficacy. The same report asserts that Phase II clinical trials have been initiated to deeper investigate the potential safety and efficacy of Tavapadon with the aim to determine the dose that can produce relief of symptoms while reducing dependence on LD and, in the meanwhile, avoiding the problems associated with long-term LD administration [38].
Preclinical and clinical studies have indicated the potential utility of D1 agonists for the treatment of neuropsychiatric disorders. However, these agents are not devoid of limitations. For instance, it has been demonstrated that LID results from increased D1 receptor-mediated transmission at the level of the direct pathway. Moreover, unlike positive allosteric modulators (PAMs), orthosteric D1 receptor agonists produce receptor desensitization and an inverted U-shaped dose-response curve [39]. The development of the D1 PAM DETQ has been reported as a different approach to D1 receptor activation [40]. Being able to amplify the effects of released endogenous DA in situ, DETQ gives a more physiological response. Its CNS pharmacology strictly reminds that of D1 agonists, but also shows remarkable differences (i.e., it does not induce stereotypy or desensitization) [40]. The reported behavioral and neurochemical test results suggest a therapeutic utility in neuropsychiatric disorders such as PD [41][42].
It has also been hypothesized that DA receptors in the striatum can form heteromeric complexes. Such an heteromerization leads to changes in the functional and pharmacological properties of receptors compared to their monomeric subtypes [43][44]. It has been observed a correlation between the expression of D1–D3 receptor heteromers and the development of LID [45]. Furthermore, D3 receptor stimulation can potentiate the D1 receptor signaling pathway [45][46]. Thus, future D3 antagonists or partial agonists able to selectively modulate the activity of striatal D1–D3 receptor heteromers could be very promising in LID control [47]. Treatment with LD also induces an ectopic expression of D3 receptors in the DA depleted dorsal striatum, which is associated with dyskinesia [39][45][48]. D3 receptor involvement in dyskinesia has further been proved by PET studies in humans showing an elevated D3 receptor binding in patients with dyskinesia [49]. It has been reported that D3 receptor agonists may produce neuroprotective effects by directly scavenging free radicals, improving the activity of free radical scavenging enzymes, stabilizing the mitochondrial membrane, directly inhibiting neuronal apoptosis. Moreover, being D3 receptors primarily localized in the midbrain limbic system, which is unrelated to motor function, selective D3 receptor agonists may have suitable anti-PD activity without significant extrapyramidal side effects [50][51][52][53][54].
The D3 receptor subtype has also been shown to exhibit biased signaling and desensitization pattern in response to certain agonists, DA included. Such an evidence could significantly contribute to the development of motor and hyperkinetic symptoms in PD and LID, respectively. On the contrary, the closely related D2 receptors have not demonstrated these D3 characteristics [39][55]. Thus, it has been demonstrated that the selective D3 agonist SK609, which does not induce desensitization of D3 receptors in vivo [56][57], was able to decrease locomotor activity [58][59]. Moreover, it has also been observed a dose dependent efficacy of SK609 in improving motor deficits in PD and ameliorating abnormal involuntary movements (AIMs) in LID using the hemiparkinsonian unilateral lesioned rodent PD model. A combination of SK609 and a low dose of LD induced a motor symptomatic relief without producing AIMs [60].
CJ-1639 is actually one of the most potent and selective D3 full agonist reported to date that may become one of the newer anti-PD drugs [61][62].
The novel ‘multifunctional’ D2/D3 high-affinity compound D-512, endowed with receptor agonist activity together with antioxidant and other neuroprotective features has recently been developed [63][64]. Compared with Ropinirole, it showed greater peak-dose efficacy and a longer lasting action, thus deserving consideration for clinical investigation.
The novel carbazole-based multifunctional D2/D3 receptor ligands D-636, D-653, and D-656, endowed with high binding affinity and full agonist activity at both receptors [65], have been proved to be highly efficacious in a PD rat model indicating their potential in relieving motor dysfunction in PD. They also exhibited neuroprotective property in an in vitro cellular model of PD. Furthermore, D-636 and D-653 demonstrated potent modulator effect on aggregation and toxicity of α-synuclein protein in vitro. Thus, it has been postulated that multifunctional drugs like D-636, D-653, and D-656 have the potential to alleviate motor dysfunction in PD patients, as well as to modify the disease progression.
Pardoprunox (SLV-308), a D2/D3 receptor partial agonist and 5-HT1A receptor full agonist, reached Phase III clinical trials for the treatment of PD. Compared with other dopaminergic agents, it displayed lower propensity to elicit side effects like dyskinesia [66].
Since ligands endowed with such a multitarget profile might be effective in PD pharmacotherapy, novel multitarget compounds based on the N-((6,6-diphenyl-1,4-dioxan-2-yl)methyl)-2-phenoxyethan-1-amine (DDMPA) scaffold were studied. Interestingly, the 3-hydroxy derivative, here named for the first time DDMPA-8, behaved as a partial agonist at D2 and as a potent full agonist at D3 and D4 subtypes. In addition to its potent 5-HT1A receptor agonism, that might be helpful in reducing dyskinetic side effects associated with the dopaminergic stimulation, such a dopaminergic profile makes DDMPA-8 a potential multitarget compound for the treatment of PD. In perspective, its evaluation in PD animal models would shed light on its therapeutic potential [67].
D4 receptors are present within the basal ganglia that represent a key area involved in parkinsonism and, in particular, in dyskinesia [68][69]. During the last years, a renewed interest has emerged around D4 receptors as potential therapeutic target for the treatment of PD, in which D4 antagonists can attenuate LID [70][71][72][73]. It has been observed that associating the potent D4 antagonist L-745,870 to LD significantly ameliorates the dyskinesia scenario in LID models. Such a result was quite remarkable since this compound has also demonstrated to be well tolerated in clinical trials. Thus, it could have a rapid development as a new tool for LID treatment. Unfortunately, disappointing results were obtained in the rotarod performance test when co-administered with LD. In fact, L-745,870 reduced the overall LD antiparkinsonian benefit in this model opening only a narrow therapeutic window to its use for the treatment of LIDs [74][75].
The effect of the novel selective D4 antagonist, VU6004461 [76], endowed with high blood–brain barrier penetrability has also been investigated. The clear antidyskinetic effect of both L-745,870 and VU6004461 points to the D4 as a possible future target for the treatment of LID [77]. At present more work is needed, but the use of D4 antagonists for the treatment of LIDs in PD remains a very promising area of research and the development of more highly optimized ligands is still an acceptable challenge [72].
All the results obtained so far are not enough and the rising of the aged population imposes new strategies in PD that may help to manage known limitations of current therapies. Some of the alternative strategies investigated as potential treatment of LID in PD involve non-dopaminergic receptors. To help researchers in such a challenge, this review focuses on recent investigations about non-dopaminergic CNS receptor ligands that have been identified to have therapeutic potential for the treatment of motor and non-motor symptoms of PD. Such agents in different way may contribute to extend LD response and/or ameliorate LD-induced side effects.
2. Serotonin Receptors
The serotonin (5-HT) system has been demonstrated to play a crucial role in the pathogenesis of LID in animal models of PD [78]. Indeed, after advanced dopaminergic cell loss, remaining serotonin neurons can convert exogenous LD to DA and mediate its vesicular storage and release [37][79]. The non-physiological DA release from these neurons might cause DA receptor overstimulation, leading to generation of dyskinesia [80]. Consequently, modulation of 5-HT system has emerged as a promising strategy for LID management. Several studies have shown a reduction of LID induced by targeting different 5-HT receptor (5-HTR) subtypes. 5-HT1AR (dorsal raphe nucleus and striatum), 5-HT1BR (striatopallidal pathways), and 5-HT2AR (substantia nigra pars reticulata and internal segment of the globus pallidus) can modulate DA, GABA, and glutamate release within the basal ganglia to improve motor symptoms of PD and to reduce dyskinesia [81]. 5-HT1AR and 5-HT1BR agonists, as well as 5-HT2AR and 5-HT3R antagonists have demonstrated a potential as antidyskinetic agents, while 5-HT4 agonists can increase LD-stimulated DA release in CNS.
2.1. 5-HT1ARs
5-HT1AR is the most studied of the 5-HT family. Indeed, several preclinical and clinical studies demonstrated that 5-HT1AR stimulation (auto- and heteroreceptors) [48][82][83] may reduce dyskinesia through the decrease of DA release [78]. Moreover, 5-HT1AR activation may also weaken glutamatergic transmission ameliorating motor symptoms [82].
In a preclinical study, the highly selective 5-HT1A full agonist 8-OH-DPAT and its (R)-(+) eutomer reduced LID, but also worsened motor function in a 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-lesioned primate model [84] (Figure 3).
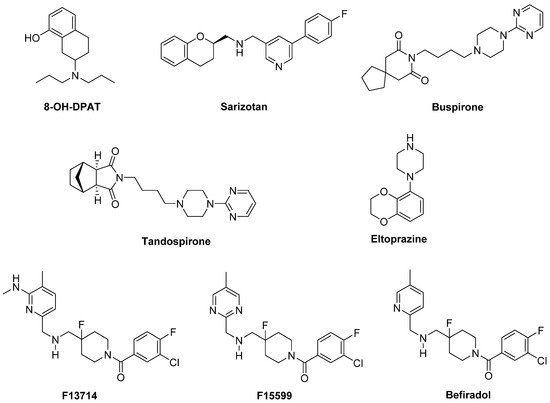
Figure 3. 5-HT1AR agonists.
Sarizotan, another 5-HT1AR full agonist, also endowed with partial D2-like agonist/antagonist profile [85], showed better results as an antidyskinetic agent in a 6-hydroxydopamine (6-OHDA)-lesioned rat model of PD [86]. When evaluated in a Phase II clinical study, at low dose it ameliorated some PD symptoms [87]. However, it failed in attenuating LID compared with placebo in two Phase III studies [88], limiting its therapeutic potential.
The partial 5-HT1AR agonists Buspirone and Tandospirone have been shown to possess antidyskinetic properties in humans, but also negatively impacted on parkinsonian symptoms [89][90]. Currently, a Phase III clinical trial is investigating the antidyskinetic potential of Buspirone, which also behaves as a D2-like receptor antagonist [91], on LID (NCT02617017), while a Phase I clinical trial is exploring its potential in combination with the non-selective NMDA antagonist Amantadine (NCT02589340).
Another 5-HT1AR partial agonist able to reduce LID in combination with LD in preclinical studies is Eltoprazine [92]. Unlike Buspirone and Tandospirone, this compound also behaves as a 5-HT1BR agonist and a 5-HT2CR antagonist [93]. In both rodent and monkey models, it abolished LD-mediated motor improvements, suggesting that it may have a narrow therapeutic window [92]. However, the loss of LD efficacy proved to be mitigated by co-administration with 5-hydroxy-tryptophan [94]. When tested in a clinical Phase I/IIa study, Eltoprazine attenuated LID without affecting the antiparkinsonian action of LD [95]. To further validate its efficacy, another Phase II trial is currently ongoing to assess the duration of Eltoprazine’s efficacy in LID management and its effects on motor function (NCT02439125). Preclinical studies have also highlighted the potential efficacy of combining eltoprazine with other compounds able to attenuate LID, such as Amantadine and the selective adenosine A2A receptor antagonist Preladenant [92][96][97].
The 5-HT1A agonists so far evaluated in clinical trials have shown off-target effects and only partial agonist efficacy at 5-HT1AR. In this contest, the new highly selective 5-HT1AR biased agonists F13714, F15599, and Befiradol (also known as F13640 or NLX112) were recently demonstrated to exhibit exceptionally potent antidyskinetic activity in animal models of PD, while minimally interfering with LD antiparkinsonian effects [98][99][100]. Biased 5-HT1A agonists are selective ligands that act in specific brain regions and preferentially target different 5-HT1AR subpopulations [101]. While F13714 and Befiradol preferentially bind presynaptic 5-HT1A autoreceptors, F15599 activates postsynaptic 5-HT1ARs [99][102][103]. Befiradol has recently been shown to possess a distinctive in vitro G-protein activation profile in rat brain cell membranes which differs from those of F13714 or F15599 [104]. In particular, it preferentially activate Gαo proteins over other G-protein subtypes. This compound is currently undergoing clinical development as an antidyskinetic agent (www.parkinsons.org.uk/news/investing-new-treatment-dyskinesia).
3. Glutamate Receptors
In rodent models of LID, high extracellular levels of glutamate were observed in the striatum and substantia nigra pars reticulata. Molecular imaging studies suggested that similar neurochemical changes of this system are evident in PD patients [105]. Therefore, glutamate receptors represent attractive targets for the treatment of LID. While the first efforts were addressed to antagonize the ionotropic glutamate receptors (iGluRs) N-methyl-D-aspartate (NMDA) and α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) subtypes [106], more recently, metabotropic glutamate receptors (mGluRs) have also been considered as potential targets for PD and LID treatment [107][108].
3.1. iGluRs
Several studies performed in animal models of LID and in post-mortem basal ganglia tissues from dyskinetic PD patients have revealed modifications in the expression and state of phosphorylation of iGluRs, in particular NMDA and AMPA receptors [105]. Therefore, these receptor systems are considered of major importance to the pathophysiology of LID.
3.1.1. NMDA Receptors
Alterations in NMDA receptor trafficking and distribution in the postsynaptic neurons appear to be associated with the extent of DA denervation as well as with the development of LID. However, the exact mechanisms regulating NMDA receptor subcellular trafficking and function in PD and LID are not fully elucidated yet [109][110]. Among the subunits forming the NMDA receptor, GluN2B subunit has attracted considerable interest. Indeed, from radioligand binding studies, performed both in NHP models of LID and dyskinetic PD patients, increased binding densities at GluN2B-containing NMDA receptors in the putamen were observed [111][112]. Furthermore, increased levels of GluN2B phosphorylation have been found in 6-OHDA-lesioned rats after chronic LD treatment [113].
The GluN2B-selective antagonists Ifenprodil and Traxoprodil (CP-101606) were reported to ameliorate parkinsonian symptoms and to reduce LID in rat and NHP models [114][115][116][117][118][119] (Figure 5). However, their use has been discouraged in NHP owing to the development of severe side effects, including amnesia and dissociation [114][116][120][121].
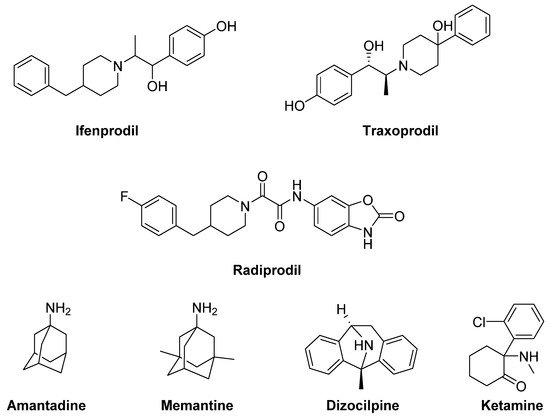
Figure 5. N-methyl-D-aspartate (NMDA) receptor ligands.
In general, divergent results have been obtained following treatment with GluN2B-selective antagonists in animal models of LID, ranging from improvement to no effect, and even to a worsening of AIMs [105].
Radiprodil, another GluN2B-selective antagonist, in combination with the selective A2A receptor antagonist Tozadenant, significantly improved motor activity both in 6-OHDA-lesioned rats and MPTP-lesioned NHP models, suggesting that the use of such a combination could lead to motor improvement to PD patients, without inducing the motor complications induced by LD therapy [122][123].
Promising results for the treatment of LID were also obtained with the weak non-competitive NMDA receptor antagonists Amantadine and Memantine. Amantadine, historically used as an antiviral agent, showed moderate but significant antidyskinetic efficacy in various clinical trials performed in the last two decades [124][125][126]. For this reason, it is the only drug with established antidyskinetic activity available in the market [127]. Amantadine treatment proved to reduce the duration of LID and to improve motor disability in PD [128] without major complications [125]. However, there are contrasting results concerning its long-term efficacy [129][130]. A Phase II clinical trial is currently ongoing to study the impact of Amantadine in preventing LID in early PD (NCT01538329). Other Phase II clinical trials are currently underway to evaluate the efficacy of Amantadine, in combination with other classes of drugs (e.g., Buspirone or Eltoprazine, see the section “Serotonin receptors”), in reducing LID in preclinical or clinical trials. Moreover, a recent study has revealed that the combination of a sub-effective dose of Amantadine and the nitric oxide synthase inhibitor 7-Nitroindazole potentiated the effect of reducing LD-induced AIMs in 6-OHDA-lesioned rats when compared to the effect of the drugs alone. This strategy may provide therapeutic benefits to PD patients at lower and thus more tolerable doses [131]. Memantine has also been investigated for its antidyskinetic potential in PD patients, but the results were conflicting. Although Memantine treatment was associated with lower LID scores and reduced daytime duration of dyskinesia, no significant effects on dyskinesia severity were found [132][133][134].
Other non-competitive NMDA receptor antagonists, including Neu-120 (structure not disclosed), Dizocilpine (MK-810) and Ketamine, displayed potential antidyskinetic effects.
Neu-120 is produced by Neurim Pharmaceuticals for the treatment of drug-induced dyskinesias. This compound, that also inhibits MAO-B and GSK-3β, has been subjected to a Phase I/II clinical trial to determine its safety, tolerability, pharmacokinetic and pharmacodynamic profiles in reducing LID in patients with advanced-phase idiopathic PD (NCT00607451). The study has been completed, but the results are not available yet.
Dizocilpine also reduced LD-induced AIMs in a rat model of LID, but only at concentrations that worsen parkinsonism [135]. However, when this compound was co-administered with the opioid glycopeptide Lactomorphin (see Figure 17), its pro-parkinsonian activity was suppressed, while a strong antidyskinetic effect remained [136].
Finally, the dissociative anesthetic Ketamine, administered at low sub-anesthetic doses, displayed a long-term effect in reducing LID in a preclinical 6-OHDA-lesioned rat model [137]. This result was confirmed by a clinical trial, in which intravenous infusion of low doses of Ketamine induced a long-lasting therapeutic benefit to reduce LID and depression in PD patients [138].
3.1.2. AMPA Receptors
Analogously to NMDA receptors, synaptic localization and phosphorylation of AMPA receptors proved to be altered in animal models of LID and in PD patients [139][140][141][142]. Moreover, in MPTP-lesioned monkeys and 6-OHDA-lesioned rats, the pharmacological blockade of AMPA receptors decreased LIDs and enhanced the antiparkinsonian effect of LD [143][144][145]. Conversely, AMPA receptor agonists triggered dyskinesias [145]. In the light of these findings, treatments with selective AMPA receptor antagonists alone or in combination with selective NMDA receptor antagonists showed beneficial effect in reducing dyskinesia [143].
The anticonvulsants Topiramate and Perampanel are the only AMPA receptor antagonists which have reached clinical trials (Figure 6). Topiramate is a negative modulator of AMPA receptors [146] and a PAM of GABAA receptors [147]. It has been reported to improve LID in MPTP-lesioned NHPs [148]. Moreover, in combination with the non-competitive NMDA receptor antagonist Amantadine, Topiramate elicited a synergistic antidyskinetic effect in both rodent and marmoset models of LID at low doses [149]. Despite these positive preclinical experiences, clinical trials have provided conflicting results. In a double-blind trial involving patients with idiopathic PD, Topiramate worsened dyskinesia and was poorly tolerated [150]. No results are so far available for other two Phase II clinical trials evaluating the efficacy of the combination of Amantadine and Topiramate versus Amantadine alone in PD patients with or without dyskinesia (NCT00794313, NCT01789047). Conflicting results were also found in clinical trials with the non-competitive antagonist Perampanel [151][152][153].
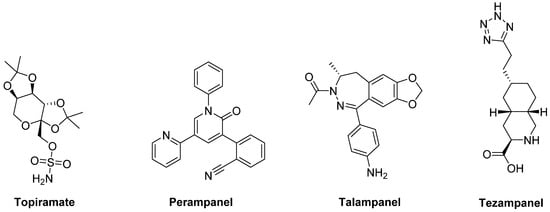
Figure 6. amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor ligands.
In preclinical studies, Talampanel (LY-300164, GYKI 537773), another non-competitive AMPA receptor antagonist, increased the anti-parkinsonian benefits of LD in MPTP-treated monkeys [145], while the competitive AMPA antagonist Tezampanel (LY-293558) was able to reduce wearing-off of LD-induced motor responses in 6-OHDA-lesioned rats [154].
4. Noradrenergic Receptors
The noradrenergic system plays an important role in the pathophysiology of PD. Noradrenergic neurons in the locus coeruleus [155] undergo degeneration in PD and may even anticipate the death of DA neurons [156][157][158]. They appear to play a protective role by establishing the extent of nigral degeneration induced by both neurotoxic damage and pathological events underlying PD [157][159][160]. Therefore, the indirect activation of adrenergic pathways by blocking presynaptic α2 adrenergic autoreceptors should prevent the nigrostriatal DA degeneration and subsequent motor deficits in PD.
Moreover, being the noradrenergic system implicated in autonomic function, targeting α2 or β adrenergic receptors (α2-Ars or β-Ars, respectively) appears to have potential to improve symptomatic orthostatic hypertension in PD.
4.1. α2-Ars
Stimulation of α2-Ars overexpressed in striatal GABAergic neurons activates direct basal ganglia pathway and is involved in the generation of LID, justifying the investigation of α2-AR antagonists as antidyskinetic agents [161].
The non-selective α2-AR antagonist Idazoxan was effective in alleviating the expression of AIMs in 6-OHDA-lesioned rats [162] (Figure 10). In a randomized, placebo-controlled pilot study, Idazoxan improved the severity of LIDs without affecting the antiparkinsonian effect of LD [163], but increasing the frequency of cardiovascular side effects.
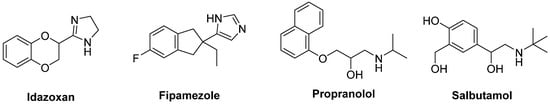
Figure 10. Noradrenergic receptor ligands.
Fipamezole, a more recently developed α2-AR antagonist, has also been shown to extend both the duration and quality of LD action in MPTP-lesioned NHP [164]. A clinical trial with ten PD patients has demonstrated good tolerability and sound antidyskinetic effect [165]. In a Phase II double-blind, placebo-controlled study in US and Indian PD patients Fipamezole did not show any significant antidyskinetic effect. However, the analysis of US subjects revealed that it reduced LIDs in a dose-dependent manner with an acceptable profile of adverse effects [166]. Other clinical trials with Fipamezole have been performed but the results have not been published yet (NCT01149811, NCT01140841, NCT00040209).
4.2. β-ARs
Pharmacological and neuroanatomical evidences support a role for β-ARs as potential therapeutic targets against LID. Indeed, both β1- and β2-ARs are expressed in the striatum [167] and are integral in PD patients [168].
The β2-AR antagonist Propranolol has been reported to reduce LID without affecting LD’s efficacy in several experimental and clinical studies (Figure 10). However, it failed to reduce dyskinesia produced by the D1 receptor agonist SKF81297 or the D2 receptor agonist Quinpirole. Antidyskinetic properties of Propranolol appear to be mediated via attenuation of LD-induced extra-physiological efflux of DA [169]. β blockers might be preferred first-line agents in PD patients who has co-morbid hypertension. Moreover, they are associated with a lower risk of constipation, which is one of the most frequent non-motor symptoms of PD [170]. However, in patients with asthma or chronic obstructive pulmonary disease, β blockers should not be used owing to the risk of bronchospasm [171].
Evidences also support the use of β2-AR agonists in PD therapy. Indeed, from molecular and immunological studies adrenergic stimulation has been suggested to decrease both α-synuclein deposition and release of neurotoxic molecules. In small clinical trials the β2-AR agonist Salbutamol in combination with LD improved parkinsonian symptoms in patients with fluctuating PD. Nevertheless, large randomized controlled trials are lacking [172].
References
- Apostolova, I.; Taleb, D.S.; Lipp, A.; Galazky, I.; Kupitz, D.; Lange, C.; Makowski, M.R.; Brenner, W.; Amthauer, H.; Plotkin, M.; et al. Utility of Follow-up Dopamine Transporter Spect with 123i-Fp-Cit in the Diagnostic Workup of Patients with Clinically Uncertain Parkinsonian Syndrome. Clin. Nucl. Med. 2017, 42, 589–594.
- Nido, G.S.; Dolle, C.; Flones, I.; Tuppen, H.A.; Alves, G.; Tysnes, O.B.; Haugarvoll, K.; Tzoulis, C. Ultradeep Mapping of Neuronal Mitochondrial Deletions in Parkinson’s Disease. Neurobiol. Aging 2018, 63, 120–127.
- Agosti, V.; Vitale, C.; Avella, D.; Rucco, R.; Santangelo, G.; Sorrentino, P.; Varriale, P.; Sorrentino, G. Effects of Global Postural Reeducation on Gait Kinematics in Parkinsonian Patients: A Pilot Randomized Three-Dimensional Motion Analysis Study. Neurol. Sci. 2016, 37, 515–522.
- Falaki, A.; Huang, X.; Lewis, M.M.; Latash, M.L. Dopaminergic Modulation of Multi-Muscle Synergies in Postural Tasks Performed by Patients with Parkinson’s Disease. J. Electromyogr. Kinesiol. 2017, 33, 20–26.
- Kataoka, H.; Okada, Y.; Kiriyama, T.; Kita, Y.; Nakamura, J.; Morioka, S.; Shomoto, K.; Ueno, S. Can Postural Instability Respond to Galvanic Vestibular Stimulation in Patients with Parkinson’s Disease? J. Mov. Disord. 2016, 9, 40–43.
- Ozinga, S.J.; Koop, M.M.; Linder, S.M.; Machado, A.G.; Dey, T.; Alberts, J.L. Three-Dimensional Evaluation of Postural Stability in Parkinson’s Disease with Mobile Technology. NeuroRehabilitation 2017, 41, 211–218.
- Picconi, B.; Hernandez, L.F.; Obeso, J.A.; Calabresi, P. Motor Complications in Parkinson’s Disease: Striatal Molecular and Electrophysiological Mechanisms of Dyskinesias. Mov. Disord. 2018, 33, 867–876.
- Silva, K.G.; De Freitas, T.B.; Dona, F.; Gananca, F.F.; Ferraz, H.B.; Torriani-Pasin, C.; Pompeu, J.E. Effects of Virtual Rehabilitation Versus Conventional Physical Therapy on Postural Control, Gait, and Cognition of Patients with Parkinson’s Disease: Study Protocol for a Randomized Controlled Feasibility Trial. Pilot Feasibility Stud. 2017, 3, 68.
- Wilczyński, J.; Habik, N. The Effect of L-Dopa on Postural Stability in Parkinson’s Disease Patients. Appl. Sci. 2019, 9, 409.
- Steib, S.; Klamroth, S.; Gassner, H.; Pasluosta, C.; Eskofier, B.; Winkler, J.; Klucken, J.; Pfeifer, K. Perturbation During Treadmill Training Improves Dynamic Balance and Gait in Parkinson’s Disease: A Single-Blind Randomized Controlled Pilot Trial. Neurorehabil. Neural Repair 2017, 31, 758–768.
- Wilczynski, J.; Pedrycz, A.; Mucha, D.; Ambrozy, T.; Mucha, D. Body Posture, Postural Stability, and Metabolic Age in Patients with Parkinson’s Disease. BioMed Res. Int. 2017, 2017, 3975417.
- Bryant, M.S.; Hou, J.G.; Collins, R.L.; Protas, E.J. Contribution of Axial Motor Impairment to Physical Inactivity in Parkinson Disease. Am. J. Phys. Med. Rehabil. 2016, 95, 348–354.
- Caetano, M.J.D.; Lord, S.R.; Allen, N.E.; Brodie, M.A.; Song, J.; Paul, S.S.; Canning, C.G.; Menant, J.C. Stepping Reaction Time and Gait Adaptability Are Significantly Impaired in People with Parkinson’s Disease: Implications for Fall Risk. Parkinsonism Relat. Disord. 2018, 47, 32–38.
- Beuter, A.; Hernandez, R.; Rigal, R.; Modolo, J.; Blanchet, P.J. Postural Sway and Effect of Levodopa in Early Parkinson’s Disease. Can. J. Neurol. Sci. 2008, 35, 65–68.
- Bonnet, C.T.; Delval, A.; Szaffarczyk, S.; Defebvre, L. Levodopa Has Primarily Negative Influences on Postural Control in Patients with Parkinson’s Disease. Behav. Brain Res. 2017, 331, 67–75.
- Mercuri, N.B.; Bernardi, G. The ‘Magic’ of L-Dopa: Why Is It the Gold Standard Parkinson’s Disease Therapy? Trends Pharmacol. Sci. 2005, 26, 341–344.
- Olanow, C.W.; Agid, Y.; Mizuno, Y.; Albanese, A.; Bonucelli, U.; Damier, P.; De Yebenes, J.; Gershanik, O.; Guttman, M.; Grandas, F.; et al. Levodopa in the Treatment of Parkinson’s Disease: Current Controversies. Mov. Disord. 2004, 19, 997–1005.
- Poewe, W.; Antonini, A.; Zijlmans, J.C.; Burkhard, P.R.; Vingerhoets, F. Levodopa in the Treatment of Parkinson’s Disease: An Old Drug Still Going Strong. Clin. Interv. Aging 2010, 5, 229–238.
- Smith, E.S.; Hardy, G.A.; Schallert, T.; Lee, H.J. The Impact of L-Dopa on Attentional Impairments in a Rat Model of Parkinson’s Disease. Neuroscience 2016, 337, 295–305.
- Cossu, G.; Ricchi, V.; Pilleri, M.; Mancini, F.; Murgia, D.; Ricchieri, G.; Mereu, A.; Melis, M.; Antonini, A. Levodopa-Carbidopa Intrajejunal Gel in Advanced Parkinson Disease with “on” Freezing of Gait. Neurol. Sci. 2015, 36, 1683–1686.
- Standaert, D.G.; Rodriguez, R.L.; Slevin, J.T.; Lobatz, M.; Eaton, S.; Chatamra, K.; Facheris, M.F.; Hall, C.; Sail, K.; Jalundhwala, Y.J.; et al. Effect of Levodopa-Carbidopa Intestinal Gel on Non-Motor Symptoms in Patients with Advanced Parkinson’s Disease. Mov. Disord. Clin. Pract. 2017, 4, 829–837.
- Zibetti, M.; Merola, A.; Artusi, C.A.; Rizzi, L.; Angrisano, S.; Reggio, D.; De Angelis, C.; Rizzone, M.; Lopiano, L. Levodopa/Carbidopa Intestinal Gel Infusion in Advanced Parkinson’s Disease: A 7-Year Experience. Eur. J. Neurol. 2014, 21, 312–318.
- Kocer, B.; Guven, H.; Comoglu, S.S. Homocysteine Levels in Parkinson’s Disease: Is Entacapone Effective? BioMed Res. Int. 2016, 2016, 7563705.
- Scott, L.J. Opicapone: A Review in Parkinson’s Disease. Drugs 2016, 76, 1293–1300.
- Ferreira, J.J.; Katzenschlager, R.; Bloem, B.R.; Bonuccelli, U.; Burn, D.; Deuschl, G.; Dietrichs, E.; Fabbrini, G.; Friedman, A.; Kanovsky, P.; et al. Summary of the Recommendations of the EFNS/MDS-ES Review on Therapeutic Management of Parkinson’s Disease. Eur. J. Neurol. 2013, 20, 5–15.
- Cenci, M.A. Molecular Mechanisms of L-Dopa-Induced Dyskinesia. In Handbook of Behavioral Neuroscience; Steiner, H., Tseng, K.Y., Eds.; Elsevier: Amsterdam, The Netherlands, 2016; Vol. 24, pp. 857–871.
- Cerri, S.; Siani, F.; Blandini, F. Investigational Drugs in Phase I and Phase II for Levodopa-Induced Dyskinesias. Expert Opin. Investig. Drugs 2017, 26, 777–791.
- Curtze, C.; Nutt, J.G.; Carlson-Kuhta, P.; Mancini, M.; Horak, F.B. Levodopa Is a Double-Edged Sword for Balance and Gait in People with Parkinson’s Disease. Mov. Disord. 2015, 30, 1361–1370.
- Hechtner, M.C.; Vogt, T.; Zöllner, Y.; Schröder, S.; Sauer, J.B.; Binder, H.; Singer, S.; Mikolajczyk, R. Quality of Life in Parkinson’s Disease Patients with Motor Fluctuations and Dyskinesias in Five European Countries. Parkinsonism Relat. Disord. 2014, 20, 969–974.
- Perez-Lloret, S.; Negre-Pages, L.; Damier, P.; Delval, A.; Derkinderen, P.; Destee, A.; Meissner, W.G.; Tison, F.; Rascol, O. L-DOPA-Induced Dyskinesias, Motor Fluctuations and Health-Related Quality of Life: The Copark Survey. Eur. J. Neurol. 2017, 24, 1532–1538.
- Dragasevic-Miskovic, N.; Petrovic, I.; Stankovic, I.; Kostic, V.S. Chemical Management of Levodopa-Induced Dyskinesia in Parkinson’s Disease Patients. Expert Opin. Pharmacother. 2019, 20, 219–230.
- Oertel, W.; Schulz, J.B. Current and Experimental Treatments of Parkinson Disease: A Guide for Neuroscientists. J. Neurochem. 2016, 139 (Suppl. 1), 325–337.
- Dong, J.; Cui, Y.; Li, S.; Le, W. Current Pharmaceutical Treatments and Alternative Therapies of Parkinson’s Disease. Curr. Neuropharmacol. 2016, 14, 339–355.
- Moore, T.J.; Glenmullen, J.; Mattison, D.R. Reports of Pathological Gambling, Hypersexuality, and Compulsive Shopping Associated with Dopamine Receptor Agonist Drugsimpulse Control Disorders and Dopamine Agonistsimpulse Control Disorders and Dopamine Agonists. JAMA Intern. Med. 2014, 174, 1930–1933.
- Connolly, B.S.; Lang, A.E. Pharmacological Treatment of Parkinson Disease: A Review. JAMA 2014, 311, 1670–1683.
- Noyes, K.; Dick, A.W.; Holloway, R.G. Pramipexole and Levodopa in Early Parkinson’s Disease. Pharmacoeconomics 2005, 23, 1257–1270.
- Thanvi, B.; Lo, N.; Robinson, T. Levodopa-Induced Dyskinesia in Parkinson’s Disease: Clinical Features, Pathogenesis, Prevention and Treatment. Postgrad. Med. J. 2007, 83, 384–388.
- Espay, A.J.; Morgante, F.; Merola, A.; Fasano, A.; Marsili, L.; Fox, S.H.; Bezard, E.; Picconi, B.; Calabresi, P.; Lang, A.E. Levodopa-Induced Dyskinesia in Parkinson Disease: Current and Evolving Concepts. Ann. Neurol. 2018, 84, 797–811.
- Sohur, U.S.; Gray, D.L.; Duvvuri, S.; Zhang, Y.; Thayer, K.; Feng, G. Phase 1 Parkinson’s Disease Studies Show the Dopamine D1/D5 Agonist PF-06649751 Is Safe and Well Tolerated. Neurol. Ther. 2018, 7, 307–319.
- Guigoni, C.; Aubert, I.; Li, Q.; Gurevich, V.V.; Benovic, J.L.; Ferry, S.; Mach, U.; Stark, H.; Leriche, L.; Håkansson, K.; et al. Pathogenesis of Levodopa-Induced Dyskinesia: Focus on D1 and D3 Dopamine Receptors. Parkinsonism Relat. Disord. 2005, 11, S25–S29.
- Svensson, K.A.; Heinz, B.A.; Schaus, J.M.; Beck, J.P.; Hao, J.; Krushinski, J.H.; Reinhard, M.R.; Cohen, M.P.; Hellman, S.L.; Getman, B.G.; et al. An Allosteric Potentiator of the Dopamine D1 Receptor Increases Locomotor Activity in Human D1 Knock-in Mice without Causing Stereotypy or Tachyphylaxis. J. Pharmacol. Exp. Ther. 2017, 360, 117–128.
- Bruns, R.F.; Mitchell, S.N.; Wafford, K.A.; Harper, A.J.; Shanks, E.A.; Carter, G.; O’Neill, M.J.; Murray, T.K.; Eastwood, B.J.; Schaus, J.M.; et al. Preclinical Profile of a Dopamine D1 Potentiator Suggests Therapeutic Utility in Neurological and Psychiatric Disorders. Neuropharmacology 2018, 128, 351–365.
- Meltzer, H.Y.; Rajagopal, L.; Matrisciano, F.; Hao, J.; Svensson, K.A.; Huang, M. The Allosteric Dopamine D1 Receptor Potentiator, Detq, Ameliorates Subchronic Phencyclidine-Induced Object Recognition Memory Deficits and Enhances Cortical Acetylcholine Efflux in Male Humanized D1 Receptor Knock-in Mice. Behav. Brain Res. 2019, 361, 139–150.
- Fiorentini, C.; Busi, C.; Gorruso, E.; Gotti, C.; Spano, P.; Missale, C. Reciprocal Regulation of Dopamine D1 and D3 Receptor Function and Trafficking by Heterodimerization. Mol. Pharmacol. 2008, 74, 59–69.
- Marcellino, D.; Ferré, S.; Casadó, V.; Cortés, A.; Le Foll, B.; Mazzola, C.; Drago, F.; Saur, O.; Stark, H.; Soriano, A.; et al. Identification of Dopamine D1–D3 Receptor Heteromers. Indications for a Role of Synergistic D1-D3 Receptor Interactions in the Striatum. J. Biol. Chem. 2008, 283, 26016–26025.
- Solis, O.; Garcia-Montes, J.R.; Gonzalez-Granillo, A.; Xu, M.; Moratalla, R. Dopamine D3 Receptor Modulates L-Dopa-Induced Dyskinesia by Targeting D1 Receptor-Mediated Striatal Signaling. Cereb. Cortex 2017, 27, 435–446.
- Fiorentini, C.; Savoia, P.; Bono, F.; Tallarico, P.; Missale, C. The D3 Dopamine Receptor: From Structural Interactions to Function. Eur. Neuropsychopharmacol. 2015, 25, 1462–1469.
- Solis, O.; Moratalla, R. Dopamine Receptors: Homomeric and Heteromeric Complexes in L-DOPA-Induced Dyskinesia. J. Neural Transm. 2018, 125, 1187–1194.
- Bézard, E.; Ferry, S.; Mach, U.; Stark, H.; Leriche, L.; Boraud, T.; Gross, C.; Sokoloff, P. Attenuation of Levodopa-Induced Dyskinesia by Normalizing Dopamine D3 Receptor Function. Nat. Med. 2003, 9, 762–767.
- Payer, D.E.; Guttman, M.; Kish, S.J.; Tong, J.; Adams, J.R.; Rusjan, P.; Houle, S.; Furukawa, Y.; Wilson, A.A.; Boileau, I. D3 Dopamine Receptor-Preferring [11C]PHNO PET Imaging in Parkinson Patients with Dyskinesia. Neurology 2016, 86, 224–230.
- Ghosh, B.; Antonio, T.; Zhen, J.; Kharkar, P.; Reith, M.E.A.; Dutta, A.K. Development of (S)-N6-(2-(4-(Isoquinolin-1-yl)Piperazin-1-yl)Ethyl)-N6-Propyl-4,5,6,7-Tetrahydrobenzo[d]-Thiazole-2,6-Diamine and Its Analogue as a D3 Receptor Preferring Agonist: Potent in Vivo Activity in Parkinson’s Disease Animal Models. J. Med. Chem. 2010, 53, 1023–1037.
- Hiller, C.; Kling, R.C.; Heinemann, F.W.; Meyer, K.; Hübner, H.; Gmeiner, P. Functionally Selective Dopamine D2/D3 Receptor Agonists Comprising an Enyne Moiety. J. Med. Chem. 2013, 56, 5130–5141.
- Tschammer, N.; Elsner, J.; Goetz, A.; Ehrlich, K.; Schuster, S.; Ruberg, M.; Kühhorn, J.; Thompson, D.; Whistler, J.; Hübner, H.; et al. Highly Potent 5-Aminotetrahydropyrazolopyridines: Enantioselective Dopamine D3 Receptor Binding, Functional Selectivity, and Analysis of Receptor−Ligand Interactions. J. Med. Chem. 2011, 54, 2477–2491.
- Zhang, H.; Tong, R.; Bai, L.; Shi, J.; Ouyang, L. Emerging Targets and New Small Molecule Therapies in Parkinson’s Disease Treatment. Bioorg. Med. Chem. 2016, 24, 1419–1430.
- Zhao, Y.; Lu, X.; Yang, C.-y.; Huang, Z.; Fu, W.; Hou, T.; Zhang, J. Computational Modeling toward Understanding Agonist Binding on Dopamine 3. J. Chem. Inf. Model. 2010, 50, 1633–1643.
- Gil-Mast, S.; Kortagere, S.; Kota, K.; Kuzhikandathil, E.V. An Amino Acid Residue in the Second Extracellular Loop Determines the Agonist-Dependent Tolerance Property of the Human D3 Dopamine Receptor. ACS Chem. Neurosci. 2013, 4, 940–951.
- Kortagere, S.; Kuzhikandahil, E.V. Novel D3 Dopamine Receptor Agonists to Treat Dyskinesia in Parkinson’s Disease. U.S. Patent WO2012021629 e, 16 February 2012.
- Westrich, L.; Gil-Mast, S.; Kortagere, S.; Kuzhikandathil, E.V. Development of Tolerance in D3 Dopamine Receptor Signaling Is Accompanied by Distinct Changes in Receptor Conformation. Biochem. Pharmacol. 2010, 79, 897–907.
- Cote, S.R.; Kuzhikandathil, E.V. In vitro and In vivo Characterization of the Agonist-Dependent D3 Dopamine Receptor Tolerance Property. Neuropharmacology 2014, 79, 359–367.
- Xu, W.; Wang, X.; Tocker, A.M.; Huang, P.; Reith, M.E.; Liu-Chen, L.Y.; Smith, A.B., 3rd; Kortagere, S. Functional Characterization of a Novel Series of Biased Signaling Dopamine D3 Receptor Agonists. ACS Chem. Neurosci. 2017, 8, 486–500.
- Simms, S.L.; Huettner, D.P.; Kortagere, S. In Vivo Characterization of a Novel Dopamine D3 Receptor Agonist to Treat Motor Symptoms of Parkinson’s Disease. Neuropharmacology 2016, 100, 106–115.
- Chen, J.; Collins, G.T.; Levant, B.; Woods, J.; Deschamps, J.R.; Wang, S. Cj-1639: A Potent and Highly Selective Dopamine D3 Receptor Full Agonist. ACS Med. Chem. Lett. 2011, 2, 620–625.
- Das, B.; Modi, G.; Dutta, A. Dopamine D3 Agonists in the Treatment of Parkinson’s Disease. Curr. Top. Med. Chem. 2015, 15, 908–926.
- Lindenbach, D.; Das, B.; Conti, M.M.; Meadows, S.M.; Dutta, A.K.; Bishop, C. D-512, a Novel Dopamine D2/3 Receptor Agonist, Demonstrates Greater Anti-Parkinsonian Efficacy Than Ropinirole in Parkinsonian Rats. Br. J. Pharmacol. 2017, 174, 3058–3071.
- Santra, S.; Xu, L.; Shah, M.; Johnson, M.; Dutta, A. D-512 and D-440 as Novel Multifunctional Dopamine Agonists: Characterization of Neuroprotection Properties and Evaluation of in Vivo Efficacy in a Parkinson’s Disease Animal Model. ACS Chem. Neurosci. 2013, 4, 1382–1392.
- Elmabruk, A.; Das, B.; Yedlapudi, D.; Xu, L.; Antonio, T.; Reith, M.E.A.; Dutta, A.K. Design, Synthesis, and Pharmacological Characterization of Carbazole Based Dopamine Agonists as Potential Symptomatic and Neuroprotective Therapeutic Agents for Parkinson’s Disease. ACS Chem. Neurosci. 2019, 10, 396–411.
- Glennon, J.C.; Van Scharrenburg, G.; Ronken, E.; Hesselink, M.B.; Reinders, J.H.; Van Der Neut, M.; Long, S.K.; Feenstra, R.W.; McCreary, A.C. In Vitro Characterization of SLV308 (7-[4-Methyl-1-Piperazinyl]-2(3h)-Benzoxazolone, Monohydrochloride): A Novel Partial Dopamine D2 and D3 Receptor Agonist and Serotonin 5-HT1A Receptor Agonist. Synapse 2006, 60, 599–608.
- Del Bello, F.; Ambrosini, D.; Bonifazi, A.; Newman, A.H.; Keck, T.M.; Giannella, M.; Giorgioni, G.; Piergentili, A.; Cappellacci, L.; Cilia, A.; et al. Multitarget 1,4-Dioxane Compounds Combining Favorable D2-Like and 5-HT1A Receptor Interactions with Potential for the Treatment of Parkinson’s Disease or Schizophrenia. ACS Chem. Neurosci. 2019.
- DeLong, M.R. Primate Models of Movement Disorders of Basal Ganglia Origin. Trends Neurosci. 1990, 13, 281–285.
- Huot, P.; Johnston, T.H.; Koprich, J.B.; Fox, S.H.; Brotchie, J.M. The Pharmacology of L-DOPA-Induced Dyskinesia in Parkinson’s Disease. Pharmacol. Rev. 2013, 65, 171–222.
- Del Bello, F.; Bonifazi, A.; Giorgioni, G.; Cifani, C.; Micioni Di Bonaventura, M.V.; Petrelli, R.; Piergentili, A.; Fontana, S.; Mammoli, V.; Yano, H.; et al. 1-[3-(4-Butylpiperidin-1-yl)Propyl]-1,2,3,4-Tetrahydroquinolin-2-One (77-LH-28-1) as a Model for the Rational Design of a Novel Class of Brain Penetrant Ligands with High Affinity and Selectivity for Dopamine D4 Receptor. J. Med. Chem. 2018, 61, 3712–3725.
- DeLong, M.R.; Wichmann, T. Circuits and Circuit Disorders of the Basal Ganglia. Arch. Neurol. 2007, 64, 20–24.
- Lindsley, C.W.; Hopkins, C.R. Return of D4 Dopamine Receptor Antagonists in Drug Discovery. J. Med. Chem. 2017, 60, 7233–7243.
- Wichmann, T.; DeLong, M.R. Functional Neuroanatomy of the Basal Ganglia in Parkinson’s Disease. Adv. Neurol. 2003, 91, 9–18.
- Huot, P.; Johnston, T.H.; Koprich, J.B.; Aman, A.; Fox, S.H.; Brotchie, J.M. L-745,870 Reduces L-DOPA-Induced Dyskinesia in the 1-Methyl-4-Phenyl-1,2,3,6-Tetrahydropyridine-Lesioned Macaque Model of Parkinson’s Disease. J. Pharmacol. Exp. Ther. 2012, 342, 576–585.
- Huot, P.; Johnston, T.H.; Koprich, J.B.; Espinosa, M.C.; Reyes, M.G.; Fox, S.H.; Brotchie, J.M. L-745,870 Reduces the Expression of Abnormal Involuntary Movements in the 6-OHDA-Lesioned Rat. Behav. Pharmacol. 2015, 26, 101–108.
- Witt, J.O.; McCollum, A.L.; Hurtado, M.A.; Huseman, E.D.; Jeffries, D.E.; Temple, K.J.; Plumley, H.C.; Blobaum, A.L.; Lindsley, C.W.; Hopkins, C.R. Synthesis and Characterization of a Series of Chiral Alkoxymethyl Morpholine Analogs as Dopamine Receptor 4 (D4R) Antagonists. Bioorg. Med. Chem. Lett. 2016, 26, 2481–2488.
- Sebastianutto, I.; Maslava, N.; Hopkins, C.R.; Cenci, M.A. Validation of an Improved Scale for Rating L-Dopa-Induced Dyskinesia in the Mouse and Effects of Specific Dopamine Receptor Antagonists. Neurobiol. Dis. 2016, 96, 156–170.
- Lanza, K.; Bishop, C. Serotonergic Targets for the Treatment of L-DOPA-Induced Dyskinesia. J. Neural Transm. 2018, 125, 1203–1216.
- Carta, M.; Tronci, E. Serotonin System Implication in L-Dopa-Induced Dyskinesia: From Animal Models to Clinical Investigations. Front. Neurol. 2014, 5, 78.
- Carta, M.; Carlsson, T.; Kirik, D.; Bjorklund, A. Dopamine Released from 5-HT Terminals Is the Cause of L-DOPA-Induced Dyskinesia in Parkinsonian Rats. Brain 2007, 130, 1819–1833.
- Nicholson, S.L.; Brotchie, J.M. 5-Hydroxytryptamine (5-HT, Serotonin) and Parkinson’s Disease—Opportunities for Novel Therapeutics to Reduce the Problems of Levodopa Therapy. Eur. J. Neurol. 2002, 9 (Suppl. 3), 1–6.
- Dupre, K.B.; Ostock, C.Y.; Eskow Jaunarajs, K.L.; Button, T.; Savage, L.M.; Wolf, W.; Bishop, C. Local Modulation of Striatal Glutamate Efflux by Serotonin 1A Receptor Stimulation in Dyskinetic, Hemiparkinsonian Rats. Exp. Neurol. 2011, 229, 288–299.
- Dupre, K.B.; Ostock, C.Y.; George, J.A.; Eskow Jaunarajs, K.L.; Hueston, C.M.; Bishop, C. Effects of 5-HT1A Receptor Stimulation on D1 Receptor Agonist-Induced Striatonigral Activity and Dyskinesia in Hemiparkinsonian Rats. ACS Chem. Neurosci. 2013, 4, 747–760.
- Iravani, M.M.; Tayarani-Binazir, K.; Chu, W.B.; Jackson, M.J.; Jenner, P. In 1-Methyl-4-Phenyl-1,2,3,6-Tetrahydropyridine-Treated Primates, the Selective 5-Hydroxytryptamine 1a Agonist (R)-(+)-8-Ohdpat Inhibits Levodopa-Induced Dyskinesia but Only with\ Increased Motor Disability. J. Pharmacol. Exp. Ther. 2006, 319, 1225–1234.
- Bartoszyk, G.D.; Van Amsterdam, C.; Greiner, H.E.; Rautenberg, W.; Russ, H.; Seyfried, C.A. Sarizotan, a Serotonin 5-HT1A Receptor Agonist and Dopamine Receptor Ligand. 1. Neurochemical Profile. J. Neural Transm. 2004, 111, 113–126.
- Bibbiani, F.; Oh, J.D.; Chase, T.N. Serotonin 5-HT1A Agonist Improves Motor Complications in Rodent and Primate Parkinsonian Models. Neurology 2001, 57, 1829–1834.
- Goetz, C.G.; Damier, P.; Hicking, C.; Laska, E.; Muller, T.; Olanow, C.W.; Rascol, O.; Russ, H. Sarizotan as a Treatment for Dyskinesias in Parkinson’s Disease: A Double-Blind Placebo-Controlled Trial. Mov. Disord. 2007, 22, 179–186.
- Goetz, C.G.; Laska, E.; Hicking, C.; Damier, P.; Müller, T.; Nutt, J.; Warren Olanow, C.; Rascol, O.; Russ, H. Placebo Influences on Dyskinesia in Parkinson’s Disease. Mov. Disord. 2008, 23, 700–707.
- Kannari, K.; Kurahashi, K.; Tomiyama, M.; Maeda, T.; Arai, A.; Baba, M.; Suda, T.; Matsunaga, M. Tandospirone Citrate, a Selective 5-HT1A Agonist, Alleviates L-DOPA-Induced Dyskinesia in Patients with Parkinson’s Disease. No to shinkei = Brain and nerve 2002, 54, 133–137.
- Ludwig, C.L.; Weinberger, D.R.; Bruno, G.; Gillespie, M.; Bakker, K.; LeWitt, P.A.; Chase, T.N. Buspirone, Parkinson’s Disease, and the Locus Ceruleus. Clin. Neuropharmacol. 1986, 9, 373–378.
- Politis, M.; Wu, K.; Loane, C.; Brooks, D.J.; Kiferle, L.; Turkheimer, F.E.; Bain, P.; Molloy, S.; Piccini, P. Serotonergic Mechanisms Responsible for Levodopa-Induced Dyskinesias in Parkinson’s Disease Patients. J. Clin. Invest. 2014, 124, 1340–1349.
- Bezard, E.; Tronci, E.; Pioli, E.Y.; Li, Q.; Porras, G.; Bjorklund, A.; Carta, M. Study of the Antidyskinetic Effect of Eltoprazine in Animal Models of Levodopa-Induced Dyskinesia. Mov. Disord. 2013, 28, 1088–1096.
- Schipper, J.; Tulp, M.T.M.; Sijbesma, H. Neurochemical Profile of Eltoprazine. Drug Metabol. Drug Interact. 1990, 8, 85–114.
- Tronci, E.; Fidalgo, C.; Stancampiano, R.; Carta, M. Effect of Selective and Non-Selective Serotonin Receptor Activation on L-DOPA-Induced Therapeutic Efficacy and Dyskinesia in Parkinsonian Rats. Behav. Brain Res. 2015, 292, 300–304.
- Svenningsson, P.; Rosenblad, C.; Af Edholm Arvidsson, K.; Wictorin, K.; Keywood, C.; Shankar, B.; Lowe, D.A.; Bjorklund, A.; Widner, H. Eltoprazine Counteracts L-Dopa-Induced Dyskinesias in Parkinson’s Disease: A Dose-Finding Study. Brain 2015, 138, 963–973.
- Ko, W.K.D.; Li, Q.; Cheng, L.Y.; Morelli, M.; Carta, M.; Bezard, E. A Preclinical Study on the Combined Effects of Repeated Eltoprazine and Preladenant Treatment for Alleviating L-DOPA-Induced Dyskinesia in Parkinson’s Disease. Eur. J. Pharmacol. 2017, 813, 10–16.
- Pinna, A.; Ko, W.K.; Costa, G.; Tronci, E.; Fidalgo, C.; Simola, N.; Li, Q.; Tabrizi, M.A.; Bezard, E.; Carta, M.; et al. Antidyskinetic Effect of A2A and 5HT1A/1B Receptor Ligands in Two Animal Models of Parkinson’s Disease. Mov. Disord. 2016, 31, 501–511.
- Huot, P.; Johnston, T.H.; Fox, S.H.; Newman-Tancredi, A.; Brotchie, J.M. The Highly-Selective 5-HT(1A) Agonist F15599 Reduces L-DOPA-Induced Dyskinesia without Compromising Anti-Parkinsonian Benefits in the MPTP-Lesioned Macaque. Neuropharmacology 2015, 97, 306–311.
- Iderberg, H.; McCreary, A.C.; Varney, M.A.; Cenci, M.A.; Newman-Tancredi, A. Activity of Serotonin 5-HT(1A) Receptor ’Biased Agonists’ in Rat Models of Parkinson’s Disease and L-DOPA-Induced Dyskinesia. Neuropharmacology 2015, 93, 52–67.
- Iderberg, H.; McCreary, A.C.; Varney, M.A.; Kleven, M.S.; Koek, W.; Bardin, L.; Depoortere, R.; Cenci, M.A.; Newman-Tancredi, A. NLX-112, a Novel 5-HT1A Receptor Agonist for the Treatment of L-DOPA-Induced Dyskinesia: Behavioral and Neurochemical Profile in Rat. Exp. Neurol. 2015, 271, 335–350.
- Chilmonczyk, Z.; Bojarski, A.J.; Pilc, A.; Sylte, I. Functional Selectivity and Antidepressant Activity of Serotonin 1A Receptor Ligands. Int. J. Mol. Sci. 2015, 16, 18474–18506.
- Llado-Pelfort, L.; Assie, M.B.; Newman-Tancredi, A.; Artigas, F.; Celada, P. Preferential in Vivo Action of F15599, a Novel 5-HT(1A) Receptor Agonist, at Postsynaptic 5-HT(1A) Receptors. Br. J. Pharmacol. 2010, 160, 1929–1940.
- Newman-Tancredi, A.; Martel, J.C.; Assie, M.B.; Buritova, J.; Lauressergues, E.; Cosi, C.; Heusler, P.; Bruins Slot, L.; Colpaert, F.C.; Vacher, B.; et al. Signal Transduction and Functional Selectivity of F15599, a Preferential Post-Synaptic 5-HT1A Receptor Agonist. Br. J. Pharmacol. 2009, 156, 338–353.
- Newman-Tancredi, A.; Varney, M.A.; McCreary, A.C. Effects of the Serotonin 5-HT1A Receptor Biased Agonists, F13714 and F15599, on Striatal Neurotransmitter Levels Following L-DOPA Administration in Hemi-Parkinsonian Rats. Neurochem. Res. 2018, 43, 1035–1046.
- Sgambato-Faure, V.; Cenci, M.A. Glutamatergic Mechanisms in the Dyskinesias Induced by Pharmacological Dopamine Replacement and Deep Brain Stimulation for the Treatment of Parkinson’s Disease. Prog. Neurobiol. 2012, 96, 69–86.
- Chase, T.N.; Oh, J.D.; Konitsiotis, S. Antiparkinsonian and Antidyskinetic Activity of Drugs Targeting Central Glutamatergic Mechanisms. J. Neurol. 2000, 247 (Suppl. 2), II36–42.
- Cenci, M.A.; Ohlin, K.E.; Odin, P. Current Options and Future Possibilities for the Treatment of Dyskinesia and Motor Fluctuations in Parkinson’s Disease. CNS Neurol. Disord. Drug Targets 2011, 10, 670–684.
- Rascol, O.; Fox, S.; Gasparini, F.; Kenney, C.; Di Paolo, T.; Gomez-Mancilla, B. Use of Metabotropic Glutamate 5-Receptor Antagonists for Treatment of Levodopa-Induced Dyskinesias. Parkinsonism Relat. Disord. 2014, 20, 947–956.
- Mellone, M.; Stanic, J.; Hernandez, L.F.; Iglesias, E.; Zianni, E.; Longhi, A.; Prigent, A.; Picconi, B.; Calabresi, P.; Hirsch, E.C.; et al. NMDA Receptor Glun2a/Glun2b Subunit Ratio as Synaptic Trait of Levodopa-Induced Dyskinesias: From Experimental Models to Patients. Front. Cell. Neurosci. 2015, 9, 245.
- Paille, V.; Picconi, B.; Bagetta, V.; Ghiglieri, V.; Sgobio, C.; Di Filippo, M.; Viscomi, M.T.; Giampa, C.; Fusco, F.R.; Gardoni, F.; et al. Distinct Levels of Dopamine Denervation Differentially Alter Striatal Synaptic Plasticity and NMDA Receptor Subunit Composition. J. Neurosci. 2010, 30, 14182–14193.
- Calon, F.; Morissette, M.; Ghribi, O.; Goulet, M.; Grondin, R.; Blanchet, P.J.; Bedard, P.J.; Di Paolo, T. Alteration of Glutamate Receptors in the Striatum of Dyskinetic 1-Methyl-4-Phenyl-1,2,3,6-Tetrahydropyridine-Treated Monkeys Following Dopamine Agonist Treatment. Prog. Neuropsychopharmacol. Biol. Psychiatry 2002, 26, 127–138.
- Calon, F.; Rajput, A.H.; Hornykiewicz, O.; Bédard, P.J.; Di Paolo, T. Levodopa-Induced Motor Complications Are Associated with Alterations of Glutamate Receptors in Parkinson’s Disease. Neurobiol. Dis. 2003, 14, 404–416.
- Chase, T.N.; Oh, J.D. Striatal Dopamine- and Glutamate-Mediated Dysregulation in Experimental Parkinsonism. Trends Neurosci. 2000, 23, S86–S91.
- Hadj Tahar, A.; Gregoire, L.; Darre, A.; Belanger, N.; Meltzer, L.; Bedard, P.J. Effect of a Selective Glutamate Antagonist on L-Dopa-Induced Dyskinesias in Drug-Naive Parkinsonian Monkeys. Neurobiol. Dis. 2004, 15, 171–176.
- Morissette, M.; Dridi, M.; Calon, F.; Tahar, A.H.; Meltzer, L.T.; Bédard, P.J.; Di Paolo, T. Prevention of Dyskinesia by an NMDA Receptor Antagonist in MPTP Monkeys: Effect on Adenosine A2A Receptors. Synapse 2006, 60, 239–250.
- Nash, J.E.; Fox, S.H.; Henry, B.; Hill, M.P.; Peggs, D.; McGuire, S.; Maneuf, Y.; Hille, C.; Brotchie, J.M.; Crossman, A.R. Antiparkinsonian Actions of Ifenprodil in the MPTP-Lesioned Marmoset Model of Parkinson’s Disease. Exp. Neurol. 2000, 165, 136–142.
- Nash, J.E.; Ravenscroft, P.; McGuire, S.; Crossman, A.R.; Menniti, F.S.; Brotchie, J.M. The NR2B-Selective NMDA Receptor Antagonist CP-101,606 Exacerbates L-DOPA-Induced Dyskinesia and Provides Mild Potentiation of Anti-Parkinsonian Effects of L-DOPA in the MPTP-Lesioned Marmoset Model of Parkinson’s Disease. Exp. Neurol. 2004, 188, 471–479.
- Nutt, J.G.; Gunzler, S.A.; Kirchhoff, T.; Hogarth, P.; Weaver, J.L.; Krams, M.; Jamerson, B.; Menniti, F.S.; Landen, J.W. Effects of a NR2B Selective NMDA Glutamate Antagonist, CP-101,606, on Dyskinesia and Parkinsonism. Mov. Disord. 2008, 23, 1860–1866.
- Igarashi, M.; Habata, T.; Akita, H.; Noda, K.; Ogata, M.; Saji, M. The NR2B Antagonist, Ifenprodil, Corrects the L-Dopa-Induced Deficit of Bilateral Movement and Reduces C-Fos Expression in the Subthalamic Nucleus of Hemiparkinsonian Rats. Neurosci. Res. 2015, 96, 45–53.
- Rylander, D.; Recchia, A.; Mela, F.; Dekundy, A.; Danysz, W.; Cenci, M.A. Pharmacological Modulation of Glutamate Transmission in a Rat Model of L-DOPA-Induced Dyskinesia: Effects on Motor Behavior and Striatal Nuclear Signaling. J. Pharmacol. Exp. Ther. 2009, 330, 227–235.
- Wessell, R.H.; Ahmed, S.M.; Menniti, F.S.; Dunbar, G.L.; Chase, T.N.; Oh, J.D. NR2B Selective NMDA Receptor Antagonist CP-101,606 Prevents Levodopa-Induced Motor Response Alterations in Hemi-Parkinsonian Rats. Neuropharmacology 2004, 47, 184–194.
- Michel, A.; Downey, P.; Van Damme, X.; De Wolf, C.; Schwarting, R.; Scheller, D. Behavioural Assessment of the A2a/NR2B Combination in the Unilateral 6-OHDA-Lesioned Rat Model: A New Method to Examine the Therapeutic Potential of Non-Dopaminergic Drugs. PLoS ONE 2015, 10, e0135949.
- Michel, A.; Nicolas, J.-M.; Rose, S.; Jackson, M.; Colman, P.; Briône, W.; Sciberras, D.; Muglia, P.; Scheller, D.K.; Citron, M.; et al. Antiparkinsonian Effects of the "Radiprodil and Tozadenant" Combination in MPTP-Treated Marmosets. PLoS ONE 2017, 12, e0182887.
- Snow, B.J.; Macdonald, L.; McAuley, D.; Wallis, W. The Effect of Amantadine on Levodopa-Induced Dyskinesias in Parkinson’s Disease: A Double-Blind, Placebo-Controlled Study. Clin. Neuropharmacol. 2000, 23, 82–85.
- Wolf, E.; Seppi, K.; Katzenschlager, R.; Hochschorner, G.; Ransmayr, G.; Schwingenschuh, P.; Ott, E.; Kloiber, I.; Haubenberger, D.; Auff, E.; et al. Long-Term Antidyskinetic Efficacy of Amantadine in Parkinson’s Disease. Mov. Disord. 2010, 25, 1357–1363.
- Sawada, H.; Oeda, T.; Kuno, S.; Nomoto, M.; Yamamoto, K.; Yamamoto, M.; Hisanaga, K.; Kawamura, T. Amantadine for Dyskinesias in Parkinson’s Disease: A Randomized Controlled Trial. PLoS ONE 2010, 5, e15298.
- Perez-Lloret, S.; Rascol, O. Efficacy and Safety of Amantadine for the Treatment of L-DOPA-Induced Dyskinesia. J. Neural Transm. 2018, 125, 1237–1250.
- Da Silva-Junior, F.P.; Braga-Neto, P.; Sueli Monte, F.; de Bruin, V.M. Amantadine Reduces the Duration of Levodopa-Induced Dyskinesia: A Randomized, Double-Blind, Placebo-Controlled Study. Parkinsonism Relat. Disord. 2005, 11, 449–452.
- Ory-Magne, F.; Corvol, J.C.; Azulay, J.P.; Bonnet, A.M.; Brefel-Courbon, C.; Damier, P.; Dellapina, E.; Destee, A.; Durif, F.; Galitzky, M.; et al. Withdrawing Amantadine in Dyskinetic Patients with Parkinson Disease: The Amandysk Trial. Neurology 2014, 82, 300–307.
- Thomas, A.; Iacono, D.; Luciano, A.L.; Armellino, K.; Di Iorio, A.; Onofrj, M. Duration of Amantadine Benefit on Dyskinesia of Severe Parkinson’s Disease. J. Neurol. Neurosurg. Psychiatry 2004, 75, 141–143.
- Bortolanza, M.; Bariotto-Dos-Santos, K.D.; Dos-Santos-Pereira, M.; da-Silva, C.A.; Del-Bel, E. Antidyskinetic Effect of 7-Nitroindazole and Sodium Nitroprusside Associated with Amantadine in a Rat Model of Parkinson’s Disease. Neurotox. Res. 2016, 30, 88–100.
- Merello, M.; Nouzeilles, M.I.; Cammarota, A.; Leiguarda, R. Effect of Memantine (NMDA Antagonist) on Parkinson’s Disease: A Double-Blind Crossover Randomized Study. Clin. Neuropharmacol. 1999, 22, 273–276.
- Moreau, C.; Delval, A.; Tiffreau, V.; Defebvre, L.; Dujardin, K.; Duhamel, A.; Petyt, G.; Hossein-Foucher, C.; Blum, D.; Sablonniere, B.; et al. Memantine for Axial Signs in Parkinson’s Disease: A Randomised, Double-Blind, Placebo-Controlled Pilot Study. J. Neurol. Neurosurg. Psychiatry 2013, 84, 552–555.
- Wictorin, K.; Widner, H. Memantine and Reduced Time with Dyskinesia in Parkinson’s Disease. Acta Neurol. Scand. 2016, 133, 355–360.
- Paquette, M.A.; Anderson, A.M.; Lewis, J.R.; Meshul, C.K.; Johnson, S.W.; Paul Berger, S. MK-801 Inhibits L-DOPA-Induced Abnormal Involuntary Movements Only at Doses That Worsen Parkinsonism. Neuropharmacology 2010, 58, 1002–1008.
- Flores, A.J.; Bartlett, M.J.; Root, B.K.; Parent, K.L.; Heien, M.L.; Porreca, F.; Polt, R.; Sherman, S.J.; Falk, T. The Combination of the Opioid Glycopeptide MMP-2200 and a NMDA Receptor Antagonist Reduced L-Dopa-Induced Dyskinesia and MMP-2200 by Itself Reduced Dopamine Receptor 2-Like Agonist-Induced Dyskinesia. Neuropharmacology 2018, 141, 260–271.
- Bartlett, M.J.; Joseph, R.M.; LePoidevin, L.M.; Parent, K.L.; Laude, N.D.; Lazarus, L.B.; Heien, M.L.; Estevez, M.; Sherman, S.J.; Falk, T. Long-Term Effect of Sub-Anesthetic Ketamine in Reducing L-DOPA-Induced Dyskinesias in a Preclinical Model. Neurosci. Lett. 2016, 612, 121–125.
- Sherman, S.J.; Estevez, M.; Magill, A.B.; Falk, T. Case Reports Showing a Long-Term Effect of Subanesthetic Ketamine Infusion in Reducing L-Dopa-Induced Dyskinesias. Case Rep. Neurol. 2016, 8, 53–58.
- Santini, E.; Sgambato-Faure, V.; Li, Q.; Savasta, M.; Dovero, S.; Fisone, G.; Bezard, E. Distinct Changes in cAMP and Extracellular Signal-Regulated Protein Kinase Signalling in L-DOPA-Induced Dyskinesia. PLoS ONE 2010, 5, e12322.
- Santini, E.; Valjent, E.; Usiello, A.; Carta, M.; Borgkvist, A.; Girault, J.A.; Herve, D.; Greengard, P.; Fisone, G. Critical Involvement of cAMP/DARPP-32 and Extracellular Signal-Regulated Protein Kinase Signaling in L-DOPA-Induced Dyskinesia. J. Neurosci. 2007, 27, 6995–7005.
- Ba, M.; Kong, M.; Yang, H.; Ma, G.; Lu, G.; Chen, S.; Liu, Z. Changes in Subcellular Distribution and Phosphorylation of GluR1 in Lesioned Striatum of 6-Hydroxydopamine-Lesioned and L-Dopa-Treated Rats. Neurochem. Res. 2006, 31, 1337–1347.
- Errico, F.; Bonito-Oliva, A.; Bagetta, V.; Vitucci, D.; Romano, R.; Zianni, E.; Napolitano, F.; Marinucci, S.; Di Luca, M.; Calabresi, P.; et al. Higher Free D-Aspartate and N-Methyl-D-Aspartate Levels Prevent Striatal Depotentiation and Anticipate L-DOPA-Induced Dyskinesia. Exp. Neurol. 2011, 232, 240–250.
- Bibbiani, F.; Oh, J.D.; Kielaite, A.; Collins, M.A.; Smith, C.; Chase, T.N. Combined Blockade of AMPA and NMDA Glutamate Receptors Reduces Levodopa-Induced Motor Complications in Animal Models of PD. Exp. Neurol. 2005, 196, 422–429.
- Kobylecki, C.; Cenci, M.A.; Crossman, A.R.; Ravenscroft, P. Calcium-Permeable AMPA Receptors Are Involved in the Induction and Expression of L-Dopa-Induced Dyskinesia in Parkinson’s Disease. J. Neurochem. 2010, 114, 499–511.
- Konitsiotis, S.; Blanchet, P.J.; Verhagen, L.; Lamers, E.; Chase, T.N. AMPA Receptor Blockade Improves Levodopa-Induced Dyskinesia in MPTP Monkeys. Neurology 2000, 54, 1589–1595.
- Vijayakumar, D.; Jankovic, J. Drug-Induced Dyskinesia, Part 1: Treatment of Levodopa-Induced Dyskinesia. Drugs 2016, 76, 759–777.
- White, H.S.; Brown, S.D.; Woodhead, J.H.; Skeen, G.A.; Wolf, H.H. Topiramate Modulates GABA-Evoked Currents in Murine Cortical Neurons by a Nonbenzodiazepine Mechanism. Epilepsia 2000, 41 (Suppl. 1), S17–20.
- Silverdale, M.A.; Nicholson, S.L.; Crossman, A.R.; Brotchie, J.M. Topiramate Reduces Levodopa-Induced Dyskinesia in the MPTP-Lesioned Marmoset Model of Parkinson’s Disease. Mov. Disord. 2005, 20, 403–409.
- Kobylecki, C.; Hill, M.P.; Crossman, A.R.; Ravenscroft, P. Synergistic Antidyskinetic Effects of Topiramate and Amantadine in Animal Models of Parkinson’s Disease. Mov. Disord. 2011, 26, 2354–2363.
- Kobylecki, C.; Burn, D.J.; Kass-Iliyya, L.; Kellett, M.W.; Crossman, A.R.; Silverdale, M.A. Randomized Clinical Trial of Topiramate for Levodopa-Induced Dyskinesia in Parkinson’s Disease. Parkinsonism Relat. Disord. 2014, 20, 452–455.
- Eggert, K.; Squillacote, D.; Barone, P.; Dodel, R.; Katzenschlager, R.; Emre, M.; Lees, A.J.; Rascol, O.; Poewe, W.; Tolosa, E.; et al. Safety and Efficacy of Perampanel in Advanced Parkinson’s Disease: A Randomized, Placebo-Controlled Study. Mov. Disord. 2010, 25, 896–905.
- Lees, A.; Fahn, S.; Eggert, K.M.; Jankovic, J.; Lang, A.; Micheli, F.; Maral Mouradian, M.; Oertel, W.H.; Olanow, C.W.; Poewe, W.; et al. Perampanel, an AMPA Antagonist, Found to Have No Benefit in Reducing “Off” Time in Parkinson’s Disease. Mov. Disord. 2012, 27, 284–288.
- Rascol, O.; Barone, P.; Behari, M.; Emre, M.; Giladi, N.; Olanow, C.W.; Ruzicka, E.; Bibbiani, F.; Squillacote, D.; Patten, A.; et al. Perampanel in Parkinson Disease Fluctuations: A Double-Blind Randomized Trial with Placebo and Entacapone. Clin. Neuropharmacol. 2012, 35, 15–20.
- Marin, C.; Jimenez, A.; Bonastre, M.; Vila, M.; Agid, Y.; Hirsch, E.C.; Tolosa, E. Ly293558, an AMPA Glutamate Receptor Antagonist, Prevents and Reverses Levodopa-Induced Motor Alterations in Parkinsonian Rats. Synapse 2001, 42, 40–47.
- Foote, S.L.; Bloom, F.E.; Aston-Jones, G. Nucleus Locus Ceruleus: New Evidence of Anatomical and Physiological Specificity. Physiol. Rev. 1983, 63, 844–914.
- Zarow, C.; Lyness, S.A.; Mortimer, J.A.; Chui, H.C. Neuronal Loss Is Greater in the Locus Coeruleus Than Nucleus Basalis and Substantia Nigra in Alzheimer and Parkinson Diseases. Arch. Neurol. 2003, 60, 337–341.
- Fornai, F.; di Poggio, A.B.; Pellegrini, A.; Ruggieri, S.; Paparelli, A. Noradrenaline in Parkinson’s Disease: From Disease Progression to Current Therapeutics. Curr. Med. Chem. 2007, 14, 2330–2334.
- McMillan, P.J.; White, S.S.; Franklin, A.; Greenup, J.L.; Leverenz, J.B.; Raskind, M.A.; Szot, P. Differential Response of the Central Noradrenergic Nervous System to the Loss of Locus Coeruleus Neurons in Parkinson’s Disease and Alzheimer’s Disease. Brain Res. 2011, 1373, 240–252.
- Mavridis, M.; Degryse, A.D.; Lategan, A.J.; Marien, M.R.; Colpaert, F.C. Effects of Locus Coeruleus Lesions on Parkinsonian Signs, Striatal Dopamine and Substantia Nigra Cell Loss after 1-Methyl-4-Phenyl-1,2,3,6-Tetrahydropyridine in Monkeys: A Possible Role for the Locus Coeruleus in the Progression of Parkinson’s Disease. Neuroscience 1991, 41, 507–523.
- Rommelfanger, K.S.; Edwards, G.L.; Freeman, K.G.; Liles, L.C.; Miller, G.W.; Weinshenker, D. Norepinephrine Loss Produces More Profound Motor Deficits Than MPTP Treatment in Mice. Proc. Natl. Acad. Sci. USA 2007, 104, 13804–13809.
- Savola, J.M.; Hill, M.; Engstrom, M.; Merivuori, H.; Wurster, S.; McGuire, S.G.; Fox, S.H.; Crossman, A.R.; Brotchie, J.M. Fipamezole (JP-1730) Is a Potent Alpha2 Adrenergic Receptor Antagonist That Reduces Levodopa-Induced Dyskinesia in the MPTP-Lesioned Primate Model of Parkinson’s Disease. Mov. Disord. 2003, 18, 872–883.
- Barnum, C.J.; Bhide, N.; Lindenbach, D.; Surrena, M.A.; Goldenberg, A.A.; Tignor, S.; Klioueva, A.; Walters, H.; Bishop, C. Effects of Noradrenergic Denervation on L-DOPA-Induced Dyskinesia and Its Treatment by A- and B-Adrenergic Receptor Antagonists in Hemiparkinsonian Rats. Pharmacol. Biochem. Behav. 2012, 100, 607–615.
- Rascol, O.; Arnulf, I.; Peyro-Saint Paul, H.; Brefel-Courbon, C.; Vidailhet, M.; Thalamas, C.; Bonnet, A.M.; Descombes, S.; Bejjani, B.; Fabre, N.; et al. Idazoxan, an Alpha-2 Antagonist, and L-DOPA-Induced Dyskinesias in Patients with Parkinson’s Disease. Mov. Disord. 2001, 16, 708–713.
- Johnston, T.H.; Fox, S.H.; Piggott, M.J.; Savola, J.M.; Brotchie, J.M. The Alpha(2) Adrenergic Antagonist Fipamezole Improves Quality of Levodopa Action in Parkinsonian Primates. Mov. Disord. 2010, 25, 2084–2093.
- Dimitrova, T.; Bara-Jimenez, W.; Savola, J.; Encarnacion, E.; Mouradian, M.; Chase, T. Alpha-2 Adrenergic Antagonist Effects in Parkinson’s Disease; Neurology, 2011; Lippincott Williams & Wilkins 530 Walnut St: Philadelphia, PA, USA; p. A540.
- Lewitt, P.A.; Hauser, R.A.; Lu, M.; Nicholas, A.P.; Weiner, W.; Coppard, N.; Leinonen, M.; Savola, J.M. Randomized Clinical Trial of Fipamezole for Dyskinesia in Parkinson Disease (Fjord Study). Neurology 2012, 79, 163–169.
- Rainbow, T.C.; Parsons, B.; Wolfe, B.B. Quantitative Autoradiography of Beta 1- and Beta 2-Adrenergic Receptors in Rat Brain. Proc. Natl. Acad. Sci. USA 1984, 81, 1585–1589.
- Waeber, C.; Rigo, M.; Chinaglia, G.; Probst, A.; Palacios, J.M. Beta-Adrenergic Receptor Subtypes in the Basal Ganglia of Patients with Huntington’s Chorea and Parkinson’s Disease. Synapse 1991, 8, 270–280.
- Bhide, N.; Lindenbach, D.; Barnum, C.J.; George, J.A.; Surrena, M.A.; Bishop, C. Effects of the Beta-Adrenergic Receptor Antagonist Propranolol on Dyskinesia and L-DOPA-Induced Striatal Da Efflux in the Hemi-Parkinsonian Rat. J. Neurochem. 2015, 134, 222–232.
- Pagano, G.; Tan, E.E.; Haider, J.M.; Bautista, A.; Tagliati, M. Constipation Is Reduced by Beta-Blockers and Increased by Dopaminergic Medications in Parkinson’s Disease. Parkinsonism Relat. Disord. 2015, 21, 120–125.
- Julius, A.; Longfellow, K. Movement Disorders: A Brief Guide in Medication Management. Med. Clin. N. Am. 2016, 100, 733–761.
- Magistrelli, L.; Comi, C. Beta2-Adrenoceptor Agonists in Parkinson’s Disease and Other Synucleinopathies. J. Neuroimmune Pharmacol. 2019.
More
Information
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
801
Revisions:
2 times
(View History)
Update Date:
01 Sep 2021
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




