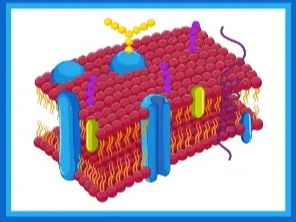
Tight junctions (TJ) are named according to their classical function to seal the cleft between epithelial and endothelial cells against unwanted passage of solutes and water. The main protein families of the TJ are claudins, TJ-associated MARVEL proteins (TAMP, including occludin and tricellulin), junctional adhesion molecules (JAM), and angulins, most of which are connected to the cytoskeleton via adapters such as zonula occludens (ZO) proteins. TJ proteins do not only form barriers but, in contrast, some constitute paracellular ion or water channels. The first molecular structures of claudins and models of TJ channel pores are published. This entry collection aims to provide further insight into the complex machinery of the development and control of tissue formation and cell differentiation.
- 1.6K
- 20 Jul 2021
- 1.3K
- 13 Jul 2021
- 1.2K
- 18 Jun 2021
- 1.2K
- 01 Jun 2021
- 1.5K
- 27 Apr 2021
- 1.4K
- 24 Mar 2021
- 1.8K
- 05 Nov 2020
- 1.4K
- 30 Oct 2020