
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Kok Yong Chin | + 1994 word(s) | 1994 | 2021-04-23 04:41:54 | | | |
| 2 | Lily Guo | Meta information modification | 1994 | 2021-04-25 03:10:06 | | |
Video Upload Options
Osteoporosis results from excessive bone resorption and reduced bone formation, triggered by sex hormone deficiency, oxidative stress and inflammation. Tanshinones are a class of lipophilic phenanthrene compounds found in the roots of Salvia miltiorrhiza with antioxidant and anti-inflammatory activities, which contribute to its anti-osteoporosis effects.
1. Introduction
Osteoporosis is a condition that increases the fracture risk of patients due to decreased bone strength, which is a result of bone microstructure and declining bone mass [1][2]. Osteoporosis can occur in both sexes, but it is more common in postmenopausal women than their male counterparts. This sex distinction occurs because of lower peak bone mass in women and the rapid decline of bone mass due to sudden cessation of oestrogen production in the body. Oestrogen deficiency leads to increased bone turnover, subsequently bone loss and osteoporosis [3]. Osteoporosis frequently remains undiagnosed due to its asymptomatic nature until it presents as low-trauma hip, spine, proximal humerus, pelvis and/or wrist fractures [4][5]. In 2010, it was estimated that 158 million individuals globally, aged 50 years or older, were at high risk of osteoporotic fracture and this number is expected to double by 2040 [6]. The cost of fractures in the United States is estimated to reach $25 billion annually by 2025 corresponding to three million projected fractures [7].
Pharmacotherapeutics for osteoporosis could be divided into anti-resorptive (i.e., bisphosphonates, oestrogen receptors modulators, oestrogen replacement and denosumab) or anabolic (i.e., teriparatide) medications. Anti-resorptive osteoporotic drugs reduce the rate of bone resorption by inhibiting osteoclasts [8]. Although they manage osteoporosis effectively, bone resorption inhibition is often associated with reduced bone formation since both processes are coupled. Coupling is modulated by osteogenic variables produced by osteoblasts. This event will prevent the repair of bone micro-fractures and jeopardise skeletal microarchitecture [9][10]. Cathepsin K (CatK) inhibitors allow inhibition of bone resorption without disturbing bone formation [11], but most agents are still in development [12][13][14]. Odonacatib is the only CatK inhibitor that had entered phase III clinical trial but was terminated due to cardio-cerebrovascular adverse effects [15][16]. On the other hand, anabolic agents increase bone formation rate more than bone resorption [8], but they are offered to patients with high fracture risk and have failed other therapies [11]. Other preventive agents like calcium and vitamin D are available, but their effectiveness is inconsistent. Ensuring adequate dietary calcium and vitamin D is compulsory in stopping the progression of osteoporosis [17]. However, vitamin D and calcium supplementation alone might not be sufficient to stop osteoporosis from occurring [18].
Tanshinones are the lipid-soluble diterpenoid quinones isolated from Danshen, the dried roots of a well-known traditional medicine Salva miltiorrhiza. They are the major lipid-soluble pharmacological constituents of Danshen and give the root its reddish-brown colour [19]. The major tanshinones isolated from Danshen included 15,16-dihydrotanshinone (D-T), tanshinone I (T-I), cryptotanshinone (C-T) and tanshinone IIA (T-IIA) [20][21]. A previous study indicated that D-T could selectively block the collagenase activity of CatK without affecting protease activity and osteoclastogenesis [22]. In vitro studies have also reported that T-IIA and C-T possess anti-inflammatory effect by inhibiting the activation of nuclear factor kappa B (NF-κB) pathway [23][24][25][26]. These studies suggest the potential of tanshinones as an anti-osteoporotic agent. Therefore, this article aims to review the effects of tanshinones on bone based on evidence from in vitro and in vivo studies.
2. Selection of Articles
A total of 158 articles were retrieved from the literature search, of which 59 were from PubMed, 89 were from Scopus and 10 were Web of Science. After removing duplicates (n = 61), 97 articles were screened. Seventy-seven articles not meeting the selection criteria were eliminated (12 review articles, 1 editorial letter and 64 articles not relevant to the current review). Finally, 20 articles fulfilling all criteria mentioned were included in the review (Table S2). The selection process from identification, screening, eligibility to inclusion of articles is shown in Figure 1.
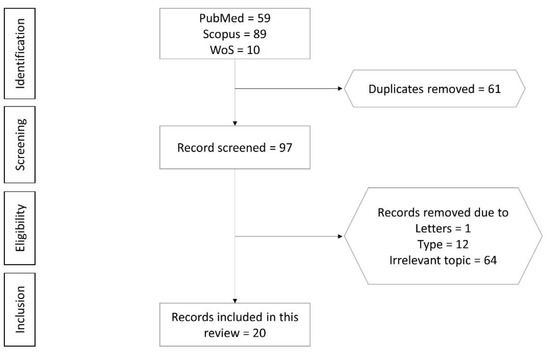
Figure 1. Flowchart of the article selection process.
3. The Skeletal Effects of Tanshinones
The current literature revealed that tanshinones exhibited anti-osteoporotic activity by suppressing osteoclastogenesis and improving osteoblastogenesis. Tanshinones exert anti-osteoclastogenic activity by blocking RANKL-induced activation of NF-κB, MAPK, Akt pathways and M-CSF/c-Src signalling. Tanshinones prevent osteoblast apoptosis and facilitate osteoblastogenesis by ameliorating oxidative stress and inflammation. Animal studies revealed that tanshinones prevented skeletal deterioration in osteoporosis models induced by oestrogen deficiency, diabetes and inflammation. They also prevent PE-induced osteolysis and improve fracture healing in animal models.
Osteoblasts are mesenchymal cells that produce and mineralise the bone matrix [27]. Osteoblast differentiation is regulated by Runx2 phosphorylation and transcription, which is mediated by the MAPK cascades. MAPK pathways and its components, JNK, ERK and p38, form the non-canonical BMP2 signal transduction pathways that regulate osteoblastogenesis [28][29][30][31]. T-IIA increases the activation of osteogenic genes which indicate its stimulatory effect on osteogenic differentiation [32][33][34]. Wang et al. pinpointed that the effects of T-IIA were mediated through JNK as inhibition of this pathway negated its effects on osteoblast differentiation and mineralisation [35].
Excessive ROS production could overwhelm intracellular antioxidant defence, causing oxidative stress and osteoporosis [36][37]. Apart from inhibiting osteoblast proliferation [38] and differentiation [39], oxidative stress also induces osteoblast apoptosis [40][41], thereby jeopardising bone formation [42]. Ameliorating oxidative stress could decrease osteoblast apoptosis and increase its differentiation [43]. Hydrogen peroxide, an end-product of Nox4, is one of the major ROS predominately present in mitochondria [44][45]. Blocking Nox4 activation may prevent osteoblast apoptosis. T-IIA was reported to inhibit Nox4 expression, which in turn decreased osteoblast apoptosis [46]. NF-κB activation negatively regulates bone formation by suppressing osteoblast differentiation [47]. T-IIA increased osteoblast differentiation via suppressing NF-κB activation and translation of its target genes (TNF-α, iNOS and COX2). This event is achieved by preventing IKK-β and IκBα degradation and p65 nuclear translocation. These effects translated to improved bone microstructure and biomechanical properties in animals treated with T-IIA [43].
Osteoclasts are derived from hematopoietic lineage cells and are capable of bone resorption [48]. It is necessary for normal bone homeostasis, but excessive resorption can induce pathological bone loss. A variety of hormones and cytokines regulate osteoclast differentiation and activation. Particularly, RANKL and M-CSF are the essential cytokines for osteoclastic differentiation [49]. M-CSF binds to colony-stimulating factor 1 receptor, and RANKL binds to RANK to promote osteoclast differentiation and survival, as well as bone resorptive activity [50][51]. RANK-RANKL binding leads to the recruitment of TRAF factors like TRAF 6 [52], resulting in the activation of NF-kB, Akt and MAPKs (ERK/p38/JNK) pathways. Besides, RANKL signalling activates c-Fos and subsequently NFATc1, a master switch for controlling osteoclast terminal differentiation [53][54][55]. All these pathways act in concert to initiate osteoclast differentiation and bone resorption by inducing transcription and expression of osteoclast-specific genes, such as TRAP, cathepsin K, matrix metalloproteinase 9 (MMP-9) and C-Src [56]. Exogenous factors like LPS can alter RANKL signalling and influence osteoclastogenesis. LPS induces production of proinflammatory cytokines of osteoblasts and precursor cells via COX-2, especially TNF-α, which subsequently augment RANKL signalling in osteoclasts [57][58]. Blocking of COX-2 is reported to inhibit osteoclastogenesis in vitro [59][60].
T-IIA treatment is reported to suppress RANKL and M-CSF-induced osteoclastogenesis from precursor cells and osteoclast function [61][62]. Similar effects were observed with T06, T-1, C-T and D-T treatment, indicating all tanshinones share similar properties [63][64][65]. T-IIA prevents RANKL-induced activation of TRAF 6, which in turn reduces activation of NF-κB, MAPK, Akt and c-Src pathways, and inhibits osteoclast formation and activity, marked by reduced TRAP and MMP9 expression [61][62]. T-IIA also inhibits the expression of RANKL-induced c-Fos and NFATc1, which suppress osteoclast differentiation [66]. Besides, T-IIA is reported to inhibit LPS-mediated COX-2 expression in bone marrow and calvarial osteoblast cells [67]. This action could reduce osteoclast formation and bone loss prevention in mice administered with LPS [67].
RANK-RANKL signalling also regulates CatK expression [68]. CatK represents a potential target of anti-osteoporosis therapy. CatK inhibition does not affect bone formation [69][70], suggesting that bone formation and resorption are uncoupled [16]. Furthermore, osteoclast formation and survival required for osteoblastic bone formation response during remodelling are not affected by CatK inhibition [71]. In contrast, increased bone formation was observed in CatK deficient mice [72]. The different forms of tanshinones (T-IIA and T06) exert distinct effects in CatK-associated bone remodelling. T-IIA suppressed RANKL-induced expression of CatK in RAW264.7 cells and BMMCs, but reduced the function and survival of osteoclasts [62]. This observation suggests that T-IIA may not be a selective inhibitor of CatK. On the other hand, T06 inhibited the activity of CatK but did not alter CatK-positive osteoclast number in mice with OVX-induced osteoporosis [64], which suggests that T06 may be a selective inhibitor of CatK. The selectivity ensures normal osteoblast-osteoclast crosstalk and bone remodelling are not interrupted. In comparison, bisphosphonates, an antiresorptive agent commonly used as the first-line treatment for osteoporosis, also inhibit bone formation [73].
The biological effects of tanshinones suggest their various potential clinical applications. Direct gingival mucosa injection of T-IIA reduced the recurrence distance and percentage of first molar tooth movement in Wistar rats by suppressing the osteoclast activity [74]. This evidence showed that T-IIA could prevent the loosening of teeth in gingival and periodontal diseases. Tanshinones enhanced skeletal health in healthy animals, by increasing BMD, femoral microstructures and strength, as well as lowering osteoclast activity [75]. Therefore, it could serve as an agent for the primary prevention of osteoporosis. Furthermore, various skeletal actions of tanshinones could be harnessed for secondary prevention of osteoporosis. T-IIA restored retinoic acid-induced decrease of cortical bone thickness and Tb.N by increasing serum oestradiol levels and preventing high bone remodelling in Wistar rats [76]. T-IIA also improved bone structural properties in mice with STZ-induced diabetic osteoporosis [77]. Additionally, T-IIA [62][78], T06 [64] and total tanshinones (T-IIA + C-T) [79] prevented OVX-induced bone loss in rats and mice by improving bone microstructures. T06 increased osteoblast number [64] while total tanshinones decreased osteoclast number [79] in vivo. Untreated osteoporosis could lead to fragility fracture. T-IIA could increase fracture healing in mice with femoral osteotomy to mimic fracture [35]. Osteolysis following joint replacement is mainly caused by the abrasive particles introduced by the prosthesis [80]. Recent studies showed that these abrasive particles could induce the release of cytokines associated with osteolysis, such as IL-6, IL-1, TNF-α and PGE2, worsening the inflammatory response [81]. PE particles have been confirmed to induce osteolysis around artificial joints [82]. T-IIA was shown to prevent calvarial bone resorption in PE particle-induced osteolysis [80]. Hence, T-IIA could be embedded with arthroplasty materials to avoid triggering inflammation and bone resorption.
Limited studies examined the safety of tanshinones. T-IIA at high concentration (≥6 μM) caused severe growth inhibition, development malformation and cardiotoxicity in zebrafish [83]. Similarly, T-11A at a high concentration (25 μM) was toxic to human endothelial EAhy926 cells as these cells were killed after a 24 h treatment [84]. There is limited data on the pharmacokinetic properties of tanshinones. Zhang et al. reported that tanshinones have limited bioavailability when administered orally [85]. After oral administration at 100 mg/kg, the systemic bioavailability of C-T was 2.05%, suggesting poor absorption or significant metabolism in the gut or/and liver. After intraperitoneal administration at 100 mg/kg, the systemic bioavailability of C-T was 10.60%, suggesting hepatic metabolism or low solubility of C-T [86]. There is a paucity of pharmacokinetics, pharmacodynamics and safety data of tanshinones in humans. A search through https://clinicaltrials.gov/ (accessed on 30 March 2021) using the term “tashinones” revealed four registered trials on left ventricular remodelling secondary to acute myocardial infarction (identifier: NCT02524964), pulmonary hypertension (identifier: NCT01637675), polycystic ovary syndrome (identifier: NCT01452477) and childhood acute promyeloid leukemia (identifier: NCT02200978). The last trial was recruiting subjects, while the status of the other three trials was unknown. No human clinical trial on the effects of tanshinones on skeletal diseases has been attempted, probably due to poor intestinal absorption and bioavailability [86][87]. Various methods have been developed to address the problem of low bioavailability, including designing water-soluble tanshinone derivatives, loading of tanshinones into discoidal and spherical high-density lipoproteins, liposomes, nanoparticles, microemulsions, cyclodextrin and solid dispersions [88][89][90][91][92]. However, due to the complicated manufacturing process, little progress has been made in the clinical application of these formulations [93]. Therefore, more comprehensive studies in this regard will help to establish tanshinones as one of the clinical therapeutic options for various bone conditions.
The present review did not exclude studies based on quality and assumed that articles published by journals indexed in three main and reputable databases are of sufficient quality to be included. We did not consider articles published in non-indexed journals, unpublished articles, thesis and non-primary research articles, potentially excluding some relevant studies.
References
- Black, D.M.; Rosen, C.J. Postmenopausal Osteoporosis. N. Engl. J. Med. 2016, 374, 254–262.
- Eastell, R.; O’Neill, T.W.; Hofbauer, L.C.; Langdahl, B.; Reid, I.R.; Gold, D.T.; Cummings, S.R. Postmenopausal osteoporosis. Nat. Rev. Dis. Prim. 2016, 2, 16069.
- Deeks, E.D. Author Correction to: Denosumab: A Review in Postmenopausal Osteoporosis. Drugs Aging 2018, 35, 261.
- Cosman, F.; De Beur, S.J.; LeBoff, M.S.; Lewiecki, E.M.; Tanner, B.; Randall, S.; Lindsay, R. Clinician’s Guide to Prevention and Treatment of Osteoporosis. Osteoporos. Int. 2014, 25, 2359–2381.
- Jeremiah, M.P.; Unwin, B.K.; Greenawald, M.H.; Casiano, V.E. Diagnosis and Management of Osteoporosis. Am. Fam. Physician 2015, 92, 261–268.
- Odén, A.; McCloskey, E.V.; Kanis, J.A.; Harvey, N.C.; Johansson, H. Burden of high fracture probability worldwide: Secular increases 2010–2040. Osteoporos. Int. 2015, 26, 2243–2248.
- Burge, R.; Dawson-Hughes, B.; Solomon, D.H.; Wong, J.B.; King, A.; Tosteson, A. Incidence and Economic Burden of Osteoporosis-Related Fractures in the United States, 2005-2025. J. Bone Miner. Res. 2006, 22, 465–475.
- Camacho, P.M.; Petak, S.M.; Binkley, N.; Clarke, B.L.; Harris, S.T.; Hurley, D.L.; Kleerekoper, M.; Lewiecki, E.M.; Miller, P.D.; Narula, H.S.; et al. American Association of Clinical Endocrinologists and American College of Endocrinology Clinical Practice Guidelines for the Diagnosis and Treatment of Postmenopausal Osteoporosis—2016. Endocr. Pr. 2016, 22, 1–42.
- Chapurlat, R.D.; Arlot, M.; Burt-Pichat, B.; Chavassieux, P.; Roux, J.P.; Portero-Muzy, N.; Delmas, P.D. Microcrack Frequency and Bone Remodeling in Postmenopausal Osteoporotic Women on Long-Term Bisphosphonates: A Bone Biopsy Study. J. Bone Miner. Res. 2007, 22, 1502–1509.
- Stepan, J.J.; Burr, D.B.; Pavo, I.; Sipos, A.; Michalska, D.; Li, J.; Fahrleitner-Pammer, A.; Petto, H.; Westmore, M.; Michalsky, D.; et al. Low bone mineral density is associated with bone microdamage accumulation in postmenopausal women with osteoporosis. Bone 2007, 41, 378–385.
- Chan, C.K.Y.; Mason, A.; Cooper, C.; Dennison, E. Novel advances in the treatment of osteoporosis. Br. Med Bull. 2016, 119, 129–142.
- Peroni, A.; Zini, A.; Braga, V.; Colato, C.; Adami, S.; Girolomoni, G. Drug-induced morphea: Report of a case induced by balicatib and review of the literature. J. Am. Acad. Dermatol. 2008, 59, 125–129.
- Rünger, T.M.; Quintanilla-Dieck, M.J.; Bhawan, J. Role of Cathepsin K in the Turnover of the Dermal Extracellular Matrix during Scar Formation. J. Investig. Dermatol. 2007, 127, 293–297.
- Tanaka, M.; Yamada, H.; Nishikawa, S.; Mori, H.; Ochi, Y.; Horai, N.; Li, M.; Amizuka, N. Joint Degradation in a Monkey Model of Collagen-Induced Arthritis: Role of Cathepsin K Based on Biochemical Markers and Histological Evaluation. Int. J. Rheumatol. 2016, 2016, 1–10.
- McClung, M.R.; O’Donoghue, M.L.; Papapoulos, S.E.; Bone, H.; Langdahl, B.; Saag, K.G.; Reid, I.R.; Kiel, D.P.; Cavallari, I.; Bonaca, M.P.; et al. Odanacatib for the treatment of postmenopausal osteoporosis: Results of the LOFT multicentre, randomised, double-blind, placebo-controlled trial and LOFT Extension study. Lancet Diabetes Endocrinol. 2019, 7, 899–911.
- Rongchen, D.; Wu, Z.; Chu, H.Y.; Lu, J.; Lyu, A.; Liu, J.; Zhang, G. Cathepsin K: The Action in and Beyond Bone. Front. Cell Dev. Biol. 2020, 8, 433.
- Tang, B.M.P.; Eslick, G.D.; Nowson, C.; Smith, C.; Bensoussan, A. Use of calcium or calcium in combination with vitamin D supplementation to prevent fractures and bone loss in people aged 50 years and older: A meta-analysis. Lancet 2007, 370, 657–666.
- The DIPART (Vitamin D Individual Patient Analysis of Randomized Trials) Group. Patient level pooled analysis of 68 500 patients from seven major vitamin D fracture trials in US and Europe. BMJ 2010, 340, b5463.
- Dong, Y.; Morris-Natschke, S.L.; Lee, K.-H. Biosynthesis, total syntheses, and antitumor activity of tanshinones and their analogs as potential therapeutic agents. Nat. Prod. Rep. 2011, 28, 529–542.
- Chen, X.; Guo, J.; Bao, J.; Lu, J.; Wang, Y. The Anticancer Properties of Salvia Miltiorrhiza Bunge (Danshen): A Systematic Review. Med. Res. Rev. 2013, 34, 768–794.
- Xing, L.; Tan, Z.-R.; Cheng, J.-L.; Huang, W.-H.; Zhang, W.; Deng, W.; Yuan, C.-S.; Zhou, H.-H. Bioavailability and pharmacokinetic comparison of tanshinones between two formulations of Salvia miltiorrhiza in healthy volunteers. Sci. Rep. 2017, 7, 4709.
- Panwar, P.; Søe, K.; Guido, R.V.C.; Bueno, R.V.C.; Delaisse, J.-M.; Brömme, D. A novel approach to inhibit bone resorption: Exosite inhibitors against cathepsin K. Br. J. Pharmacol. 2015, 173, 396–410.
- Ren, Z.H.; Tong, Y.H.; Xu, W.; Ma, J.; Chen, Y. Tanshinone II A attenuates inflammatory responses of rats with myocardial infarction by reducing MCP-1 expression. Phytomedicine 2010, 17, 212–218.
- Li, X.; Lian, L.-H.; Bai, T.; Wu, Y.-L.; Wan, Y.; Xie, W.-X.; Jin, X.; Nan, J.-X. Cryptotanshinone inhibits LPS-induced proinflammatory mediators via TLR4 and TAK1 signaling pathway. Int. Immunopharmacol. 2011, 11, 1871–1876.
- Li, X.-X.; Zheng, X.; Liu, Z.; Xu, Q.; Tang, H.; Feng, J.; Yang, S.; Vong, C.T.; Gao, H.; Wang, Y. Cryptotanshinone from Salvia miltiorrhiza Bunge (Danshen) inhibited inflammatory responses via TLR4/MyD88 signaling pathway. Chin. Med. 2020, 15, 1–13.
- Jang, S.I.; Kim, H.J.; Kim, Y.-J.; Jeong, S.-I.; You, Y.-O. Tanshinone IIA inhibits LPS-induced NF-κB activation in RAW 264.7 cells: Possible involvement of the NIK–IKK, ERK1/2, p38 and JNK pathways. Eur. J. Pharmacol. 2006, 542, 1–7.
- Dirckx, N.; Moorer, M.C.; Clemens, T.L.; Riddle, R.C. The role of osteoblasts in energy homeostasis. Nat. Rev. Endocrinol. 2019, 15, 651–665.
- Xiao, G.; Gopalakrishnan, R.; Jiang, D.; Reith, E.; Benson, M.D.; Franceschi, R.T. Bone Morphogenetic Proteins, Extracellular Matrix, and Mitogen-Activated Protein Kinase Signaling Pathways Are Required for Osteoblast-Specific Gene Expression and Differentiation in MC3T3-E1 Cells. J. Bone Miner. Res. 2002, 17, 101–110.
- Nohe, A.; Hassel, S.; Ehrlich, M.; Neubauer, F.; Sebald, W.; Henis, Y.I.; Knaus, P. The Mode of Bone Morphogenetic Protein (BMP) Receptor Oligomerization Determines Different BMP-2 Signaling Pathways. J. Biol. Chem. 2002, 277, 5330–5338.
- Massagué, J.; Blain, S.W.; Lo, R.S. TGFβ Signaling in Growth Control, Cancer, and Heritable Disorders. Cell 2000, 103, 295–309.
- Guo, X.; Wang, X.-F. Signaling cross-talk between TGF-β/BMP and other pathways. Cell Res. 2009, 19, 71–88.
- Liu, X.; Niu, Y.; Xie, W.; Wei, D.; Du, Q. Tanshinone IIA promotes osteogenic differentiation of human periodontal ligament stem cells via ERK1/2-dependent Runx2 induction. Am. J. Trans. Res. 2019, 11, 340–350.
- Qian, K.; Xu, H.; Dai, T.; Shi, K. Effects of Tanshinone IIA on osteogenic differentiation of mouse bone marrow mesenchymal stem cells. Naunyn-Schmiedeberg’s Arch. Pharmacol. 2015, 388, 1201–1209.
- Kim, H.J.; Kim, S.H. Tanshinone IIA enhances BMP-2-stimulated commitment of C2C12 cells into osteoblasts via p38 activation. Amino Acids 2010, 39, 1217–1226.
- Wang, Y.; Chen, H.; Zhang, H. Tanshinone IIA exerts beneficial effects on fracture healing in vitro and in vivo. Chem. Interactions 2019, 310, 108748.
- Baek, K.H.; Oh, K.W.; Lee, W.Y.; Lee, S.S.; Kim, M.K.; Kwon, H.S.; Rhee, E.J.; Han, J.H.; Song, K.H.; Cha, B.Y.; et al. Association of Oxidative Stress with Postmenopausal Osteoporosis and the Effects of Hydrogen Peroxide on Osteoclast Formation in Human Bone Marrow Cell Cultures. Calcif. Tissue Int. 2010, 87, 226–235.
- Yin, H.; Shi, Z.-G.; Yu, Y.-S.; Hu, J.; Wang, R.; Luan, Z.-P.; Guo, D.-H. Protection against osteoporosis by statins is linked to a reduction of oxidative stress and restoration of nitric oxide formation in aged and ovariectomized rats. Eur. J. Pharmacol. 2012, 674, 200–206.
- Li, M.; Zhao, L.; Liu, J.; Liu, A.-L.; Zeng, W.-S.; Luo, S.-Q.; Bai, X.-C. Hydrogen Peroxide Induces G2Cell Cycle Arrest and Inhibits Cell Proliferation in Osteoblasts. Anat. Rec. Adv. Integr. Anat. Evol. Biol. 2009, 292, 1107–1113.
- Zhong, Z.-M.; Bai, L.; Chen, J.-T. Advanced Oxidation Protein Products Inhibit Proliferation and Differentiation of Rat Osteoblast-like Cells via NF-κB Pathway. Cell. Physiol. Biochem. 2009, 24, 105–114.
- Almeida, M.; Han, L.; Ambrogini, E.; Bartell, S.M.; Manolagas, S.C. Oxidative Stress Stimulates Apoptosis and Activates NF-κB in Osteoblastic Cells via a PKCβ/p66shc Signaling Cascade: Counter Regulation by Estrogens or Androgens. Mol. Endocrinol. 2010, 24, 2030–2037.
- Wu, Y.; Wang, D.; Wang, X.; Wang, Y.; Ren, F.; Chang, D.; Chang, Z.; Jia, B. Caspase 3 is Activated through Caspase 8 instead of Caspase 9 during H2O2-induced Apoptosis in HeLa Cells. Cell. Physiol. Biochem. 2011, 27, 539–546.
- Moriishi, T.; Kawai, Y.; Komori, H.; Rokutanda, S.; Eguchi, Y.; Tsujimoto, Y.; Asahina, I.; Komori, T. Bcl2 Deficiency Activates FoxO through Akt Inactivation and Accelerates Osteoblast Differentiation. PLoS ONE 2014, 9, e86629.
- Zhu, S.; Wei, W.; Liu, Z.; Yang, Y.; Jia, H. Tanshinone-IIA attenuates the deleterious effects of oxidative stress in osteoporosis through the NF-κB signaling pathway. Mol. Med. Rep. 2018, 17, 6969–6976.
- Schroeder, K.; Zhang, M.; Benkhoff, S.; Mieth, A.; Pliquett, R.; Kosowski, J.; Kruse, C.; Luedike, P.; Michaelis, U.R.; Weissmann, N.; et al. Nox4 Is a Protective Reactive Oxygen Species Generating Vascular NADPH Oxidase. Circ. Res. 2012, 110, 1217–1225.
- Cabiscol, E.; Tamarit, J.; Ros, J. Oxidative stress in bacteria and protein damage by reactive oxygen species. Int. Microbiol. 2000, 3, 3–8.
- Li, J.; He, C.; Tong, W.; Zou, Y.; Li, D.; Zhang, C.; Xu, W. Tanshinone IIA blocks dexamethasone-induced apoptosis in osteoblasts through inhibiting Nox4-derived ROS production. Int. J. Clin. Exp. Pathol. 2015, 8, 13695–13706.
- Yao, Z.; Li, Y.; Yin, X.; Dong, Y.; Xing, L.; Boyce, B.F. NF-κB RelB Negatively Regulates Osteoblast Differentiation and Bone Formation. J. Bone Miner. Res. 2014, 29, 866–877.
- Gallois, A.; Lachuer, J.; Yvert, G.; Wierinckx, A.; Brunet, F.; Rabourdin-Combe, C.; Delprat, C.; Jurdic, P.; Mazzorana, M. Genome-wide expression analyses establish dendritic cells as a new osteoclast precursor able to generate bone-resorbing cells more efficiently than monocytes. J. Bone Miner. Res. 2010, 25, 661–672.
- De Vries, T.J.; Schoenmaker, T.; Aerts, D.; Grevers, L.C.; Souza, P.P.; Nazmi, K.; Van De Wiel, M.A.; Ylstra, B.; Van Lent, P.L.V.; Leenen, P.J.M.; et al. M-CSF Priming of Osteoclast Precursors Can Cause Osteoclastogenesis-Insensitivity, Which Can be Prevented and Overcome on Bone. J. Cell. Physiol. 2015, 230, 210–225.
- Mun, S.H.; Park, P.S.U.; Park-Min, K.-H. The M-CSF receptor in osteoclasts and beyond. Exp. Mol. Med. 2020, 52, 1239–1254.
- Suda, T.; Takahashi, N.; Udagawa, N.; Jimi, E.; Gillespie, M.T.; Martin, T.J. Modulation of Osteoclast Differentiation and Function by the New Members of the Tumor Necrosis Factor Receptor and Ligand Families. Endocr. Rev. 1999, 20, 345–357.
- Bharti, A.C.; Takada, Y.; Shishodia, S.; Aggarwal, B.B. Evidence That Receptor Activator of Nuclear Factor (NF)-κB Ligand Can Suppress Cell Proliferation and Induce Apoptosis through Activation of a NF-κB-independent and TRAF6-dependent Mechanism. J. Biol. Chem. 2004, 279, 6065–6076.
- Takayanagi, H.; Kim, S.; Koga, T.; Nishina, H.; Isshiki, M.; Yoshida, H.; Saiura, A.; Isobe, M.; Yokochi, T.; Inoue, J.-I.; et al. Induction and Activation of the Transcription Factor NFATc1 (NFAT2) Integrate RANKL Signaling in Terminal Differentiation of Osteoclasts. Dev. Cell 2002, 3, 889–901.
- Johnson, R.S.; Spiegelman, B.M.; Papaioannou, V. Pleiotropic effects of a null mutation in the c-fos proto-oncogene. Cell 1992, 71, 577–586.
- Ishida, N.; Hayashi, K.; Hoshijima, M.; Ogawa, T.; Koga, S.; Miyatake, Y.; Kumegawa, M.; Kimura, T.; Takeya, T. Large Scale Gene Expression Analysis of Osteoclastogenesisin Vitro and Elucidation of NFAT2 as a Key Regulator. J. Biol. Chem. 2002, 277, 41147–41156.
- Nakashima, T.; Hayashi, M.; Fukunaga, T.; Kurata, K.; Oh-Hora, M.; Feng, J.Q.; Bonewald, L.F.; Kodama, T.; Wutz, A.; Wagner, E.F.; et al. Evidence for osteocyte regulation of bone homeostasis through RANKL expression. Nat. Med. 2011, 17, 1231–1234.
- Li, L.; Pettit, A.R.; Gregory, L.S.; Forwood, M.R. Regulation of bone biology by prostaglandin endoperoxide H synthases (PGHS): A rose by any other name…. Cytokine Growth Factor Rev. 2006, 17, 203–216.
- Ono, K.; Akatsu, T.; Murakami, T.; Kitamura, R.; Yamamoto, M.; Shinomiya, N.; Rokutanda, M.; Sasaki, T.; Amizuka, N.; Ozawa, H.; et al. Involvement of Cyclo-Oxygenase-2 in Osteoclast Formation and Bone Destruction in Bone Metastasis of Mammary Carcinoma Cell Lines. J. Bone Miner. Res. 2002, 17, 774–781.
- Ono, K.; Akatsu, T.; Kugai, N.; Pilbeam, C.C.; Raisz, L.G. The effect of deletion of cyclooxygenase-2, prostaglandin receptor EP2, or EP4 in bone marrow cells on osteoclasts induced by mouse mammary cancer cell lines. Bone 2003, 33, 798–804.
- Kellinsalmi, M.; Parikka, V.; Risteli, J.; Hentunen, T.; Leskelä, H.-V.; Lehtonen, S.; Selander, K.; Väänänen, K.; Lehenkari, P. Inhibition of cyclooxygenase-2 down-regulates osteoclast and osteoblast differentiation and favours adipocyte formation in vitro. Eur. J. Pharmacol. 2007, 572, 102–110.
- Kim, H.-H.; Kim, J.H.; Kwak, H.B.; Huang, H.; Han, S.-H.; Ha, H.; Lee, S.W.; Woo, E.-R.; Lee, Z.H. Inhibition of osteoclast differentiation and bone resorption by tanshinone IIA isolated from Salvia miltiorrhiza Bunge. Biochem. Pharmacol. 2004, 67, 1647–1656.
- Cheng, L.; Zhou, S.; Zhao, Y.; Sun, Y.; Xu, Z.; Yuan, B.; Chen, X. Tanshinone IIA attenuates osteoclastogenesis in ovariectomized mice by inactivating NF-kB and Akt signaling pathways. Am. J. Transl. Res. 2018, 10, 1457–1468.
- Lee, S.-Y.; Choi, D.-Y.; Woo, E.-R. Inhibition of osteoclast differentiation by tanshinones from the root ofSalvia miltiorrhiza Bunge. Arch. Pharmacal Res. 2005, 28, 909–913.
- Panwar, P.; Xue, L.; Søe, K.; Srivastava, K.; Law, S.; Delaisse, J.-M.; Brömme, D. An Ectosteric Inhibitor of Cathepsin K Inhibits Bone Resorption in Ovariectomized Mice. J. Bone Miner. Res. 2017, 32, 2415–2430.
- Kim, H.-K.; Woo, E.-R.; Lee, H.-W.; Park, H.-R.; Kim, H.-N.; Jung, Y.-K.; Choi, J.-Y.; Chae, S.-W.; Kim, H.-R.; Chae, H.-J. The Correlation ofSalvia miltiorrhizaExtract–Induced Regulation of Osteoclastogenesis with the Amount of Components Tanshinone I, Tanshinone IIA, Cryptotanshinone, and Dihydrotanshinone. Immunopharmacol. Immunotoxicol. 2008, 30, 347–364.
- Kwak, H.B.; Yang, D.; Ha, H.; Lee, J.-H.; Kim, H.-N.; Woo, E.-R.; Lee, S.; Kim, H.-H.; Lee, Z.H. Tanshinone IIA inhibits osteoclast differentiation through down-regulation of c-Fos and NFATc1. Exp. Mol. Med. 2006, 38, 256–264.
- Kwak, H.B.; Sun, H.-M.; Ha, H.; Kim, H.-N.; Lee, J.-H.; Kim, H.-H.; Shin, H.-I.; Lee, Z.H. Tanshinone IIA suppresses inflammatory bone loss by inhibiting the synthesis of prostaglandin E2 in osteoblasts. Eur. J. Pharmacol. 2008, 601, 30–37.
- Troen, B.R. The Regulation of Cathepsin K Gene Expression. Ann. N. Y. Acad. Sci. 2006, 1068, 165–172.
- Brömme, D.; Panwar, P.; Turan, S. Cathepsin K osteoporosis trials, pycnodysostosis and mouse deficiency models: Commonalities and differences. Expert Opin. Drug Discov. 2016, 11, 457–472.
- Drake, M.T.; Clarke, B.L.; Oursler, M.J.; Khosla, S. Cathepsin K Inhibitors for Osteoporosis: Biology, Potential Clinical Utility, and Lessons Learned. Endocr. Rev. 2017, 38, 325–350.
- Martin, T.J.; Sims, N.A. Osteoclast-derived activity in the coupling of bone formation to resorption. Trends Mol. Med. 2005, 11, 76–81.
- Li, C.Y.; Jepsen, K.J.; Majeska, R.J.; Zhang, J.; Ni, R.; Gelb, B.D.; Schaffler, M.B. Mice Lacking Cathepsin K Maintain Bone Remodeling but Develop Bone Fragility Despite High Bone Mass. J. Bone Miner. Res. 2006, 21, 865–875.
- George, E.L.; Lin, Y.-L.; Saunders, M.M. Bisphosphonate-related osteonecrosis of the jaw: A mechanobiology perspective. Bone Rep. 2018, 8, 104–109.
- Zhang, S.Y.; Liu, J.G.; Zhao, G. Tanshinone type IIA inhibits osteoprotegerin and osteoclast differentiation factor expression at relapse stage after orthodontic tooth movement. Chinese J. Tissue Engineering Res. 2014, 18, 1730–1736.
- Yang, F.-F.; Gao, Y.-H.; Xi, H.-R.; Li, W.-Y.; Ma, H.-P.; Chen, K.-M. Effect of Compound Medicine of Tanshinone 2A and Resveratrol on Peak Bone Mass in Growing Rats. Zhongguo Yi Xue Ke Xue Yuan Xue Bao 2018, 40, 456–462.
- Zhou, Y.; Liu, Y.; Gao, Y. Effect of tanshitone on prevention and treatment of retinoic acid induced osteoporosis in mice. China J. Chin. Mater. Medica 2010, 35, 2923–2926.
- Zhang, J.; Cai, Z.; Yang, M.; Tong, L.; Zhang, Y. Inhibition of tanshinone IIA on renin activity protected against osteoporosis in diabetic mice. Pharm. Biol. 2020, 58, 219–224.
- Wang, L.; Cheng, L.; Zhang, B.; Wang, N.; Wang, F. Tanshinone prevents alveolar bone loss in ovariectomized osteoporosis rats by up-regulating phosphoglycerate dehydrogenase. Toxicol. Appl. Pharmacol. 2019, 376, 9–16.
- Cui, L.; Wu, T.; Liu, Y.-Y.; Deng, Y.-F.; Ai, C.-M.; Chen, H.-Q. Tanshinone prevents cancellous bone loss induced by ovariectomy in rats. Acta Pharmacol. Sin. 2004, 25, 678–684.
- Yao, J.; Ma, S.; Feng, W.; Wei, Y.; Lu, H.; Zhong, G.; Wu, Z.; Wang, H.; Su, W.; Li, J. Tanshinone IIA protects against polyethylene particle-induced osteolysis response in a mouse calvarial model. International Journal of Clinical and Experimental Pathology 2018, 11, 4461–4471.
- Noordin, S.; Masri, B. Periprosthetic osteolysis: Genetics, mechanisms and potential therapeutic interventions. Can. J. Surg. 2012, 55, 408–417.
- Neuerburg, C.; Loer, T.; Mittlmeier, L.; Polan, C.; Farkas, Z.; Holdt, L.M.; Utzschneider, S.; Schwiesau, J.; Grupp, T.M.; Böcker, W.; et al. Impact of vitamin E-blended UHMWPE wear particles on the osseous microenvironment in polyethylene particle-induced osteolysis. Int. J. Mol. Med. 2016, 38, 1652–1660.
- Wang, T.; Wang, C.; Wu, Q.; Zheng, K.; Chen, J.; Lan, Y.; Qin, Y.; Mei, W.; Wang, B. Evaluation of Tanshinone IIA Developmental Toxicity in Zebrafish Embryos. Molecules 2017, 22, 660.
- Yang, L.-J.; Jeng, C.-J.; Kung, H.-N.; Chang, C.-C.; Wang, A.-G.; Chau, G.-Y.; Don, M.-J.; Chau, Y.-P. Tanshinone IIA isolated from Salvia miltiorrhiza elicits the cell death of human endothelial cells. J. Biomed. Sci. 2005, 12, 347–361.
- Zhang, Y.; Jiang, P.; Ye, M.; Kim, S.-H.; Jiang, C.; Lü, J. Tanshinones: Sources, Pharmacokinetics and Anti-Cancer Activities. Int. J. Mol. Sci. 2012, 13, 13621–13666.
- Zhang, J.; Huang, M.; Guan, S.; Bi, H.-C.; Pan, Y.; Duan, W.; Chan, S.Y.; Chen, X.; Hong, Y.-H.; Bian, J.-S.; et al. A Mechanistic Study of the Intestinal Absorption of Cryptotanshinone, the Major Active Constituent ofSalvia miltiorrhiza. J. Pharmacol. Exp. Ther. 2006, 317, 1285–1294.
- Yu, X.-Y.; Lin, S.-G.; Zhou, Z.-W.; Chen, X.; Liang, J.; Liu, P.-Q.; Duan, W.; Chowbay, B.; Wen, J.-Y.; Li, C.-G.; et al. Role of P-Glycoprotein in the Intestinal Absorption of Tanshinone IIA, a Major Active Ingredient in the Root of Salvia miltiorrhiza Bunge. Curr. Drug Metab. 2007, 8, 325–340.
- Xu, S.; Liu, P. Tanshinone II-A: New perspectives for old remedies. Expert Opin. Ther. Pat. 2012, 23, 149–153.
- Wang, L.; Lai, Y.; Li, C.; Jiang, X. Study on the intestinal absorption profiles of tanshinone IIA and its inclusion complex with cyclodextrin in rats. PDA J. Pharm. Sci. Technol. 2010, 63, 390–400.
- Liu, X.; An, C.; Jin, P.; Liu, X.; Wang, L. Protective effects of cationic bovine serum albumin-conjugated PEGylated tanshinone IIA nanoparticles on cerebral ischemia. Biomater. 2013, 34, 817–830.
- Ma, H.; Fan, Q.; Yu, J.; Xin, J.; Zhang, C. Anticancer activities of tanshinone microemulsion against hepatocellular carcinoma in vitro and in vivo. Mol. Med. Rep. 2012, 7, 59–64.
- Jia, X.-B.; Yan, H.-M.; Zhang, Z.-H.; Jiang, Y.-R.; Ding, D.-M.; Sun, E. An attempt to stabilize tanshinone IIA solid dispersion by the use of ternary systems with nano-CaCO3and poloxamer 188. Pharmacogn. Mag. 2014, 10, 311–S317.
- Chen, M.; Cai, Y.; Zhang, W.; Chen, Z.; Shi, Z.; He, C. Recent insights into the biological activities and drug delivery systems of tanshinones. Int. J. Nanomed. 2016, 11, 121–130.




