
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Mirko Duradoni | + 3608 word(s) | 3608 | 2021-04-13 11:34:03 | | | |
| 2 | Vivi Li | Meta information modification | 3608 | 2021-04-14 06:19:49 | | | | |
| 3 | Vivi Li | Meta information modification | 3608 | 2021-04-14 06:20:43 | | |
Video Upload Options
Technological advancement is constantly evolving, and it is also developing in the mental health field. Various applications, often based on virtual reality, have been implemented to carry out psychological assessments and interventions, using innovative human–machine interaction systems. In this context, the LEAP Motion sensing technology has raised interest, since it allows for more natural interactions with digital contents, via an optical tracking of hand and finger movements.
1. Introduction
Growing attention has been given to technology-based tools, and researchers are increasingly analyzing their potential to contribute to mental health services [1]. Recently, different technologies have been included in mental healthcare delivery, and this has promoted a reflection on innovative care models that can reach people who might not have access to services [2]. Studies in this field also shed light on the recently developed LEAP Motion technology. The LEAP Motion controller is a highly compact and affordable USB motion capture device with two cameras and three infrared LEDs (Figure 1—left side). Thanks to the illumination of the surrounding space, the device captures hand gestures at a one-meter distance with a mean accuracy of 0.7 mm [3]. A tracking algorithm allows us to estimate the position and orientation of hands and fingers that are directly visible in a three-dimensional virtual representation [4]. In this way, data coming from the LEAP Motion controller allow users to interact within a virtual environment in a touchless way, by using natural hand gestures as input commands [4] (Figure 1—right side).
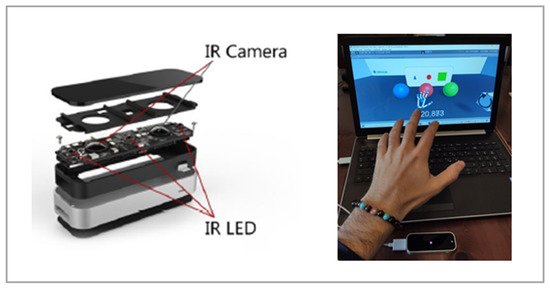
Figure 1. Exploded view of the LEAP Motion device. Reference taken from Wozniak et al., 2016 (left side) and an example of a LEAP-Motion-based virtual environment (right side).
The LEAP Motion Software Development Kit recognizes simple movements such as swipe, tapping, grabbing, and circular gestures, making it possible to manipulate virtual objects by grasping and placing them [4]. It must be noted that the tracking quality can be altered by too strong or poor illumination of the room and that occluded parts of the hand cannot be traced by the device, even if it can estimate conventional movements [4].
Touchless interaction with small hand gestures could offer opportunities for people with disabilities [5]. Indeed, this kind of user interface is broadly used in gaming but also in assistive technologies, as they are able to identify movements of the body, thus valuable for people with impairments that prevent them from using touch interfaces [6].
Moreover, research also shows the benefits of gesture interaction in populations with developmental disorders, thanks to the possibility to promote motor skills as well as cognitive and social ones in monitored virtual environments that can reproduce real settings [7].
For these reasons, motion capture systems, such as Microsoft’s Kinect, have already demonstrated their usefulness in supporting physical rehabilitation [8][9] and intervention in clinical populations with specific needs [10][11]. However, such systems typically do not allow for the development of low-cost custom applications. The LEAP technology can overcome this limitation, by enabling immediate communication with freeware graphics engines. This has led researchers worldwide to develop a whole series of activities ex novo [12][13][14][15][16].
This technology is easily accessible by populations with different levels of technological expertise and could be used for gamified activities, which are appreciated, for instance, by children [17].
In general, playing, recreational programs [18][19], and virtual reality (VR) activities are often used by hospitals to support people in reducing their fear, distress, and the intensity of perceived pain in various medical procedures [20][21][22]. However, virtual gamified activities can not only be useful for distraction but also can offer a means to assess some psychological dimensions of users [23]. For instance, the use of virtual reality has recently been proposed to battle social isolation in institutionalized elderly people in residential structures, with positive effects regarding the reduction in loneliness [24].
With specific regard to the LEAP Motion technology, researchers have used it to project and implement interventions for neurodevelopmental and neurocognitive disorders that are of interest in this paper.
Neurodevelopmental disorders are a group of disorders characterized by the disorder onset in the developmental period. Indeed, the disorders often manifest before entering grade school, and they are defined by developmental deficits that cause impairments of personal, occupational, social, and academic functioning. Instead, the neurocognitive disorders include disorders characterized by core clinical deficits in cognitive functions. They are not developmental deficits but acquired, indeed, the cognition impairment is not present from birth or very early life, it rather constitutes a decline from a previous level of functioning [25].
Among neurodevelopmental disorders there are autism spectrum disorder and attention-deficit/hyperactivity disorder. Autism spectrum disorder (ASD) is characterized by persistent deficits in social communication and interaction skills as well as repetitive and restricted behavior patterns, interests, and activities. Communication and interaction impairment are shown in different contexts including socio-emotional reciprocity, nonverbal communicative behaviors, and in developing, understanding, and maintaining relationships. Stereotypy can be found in motor movements, use of objects, and speech; inflexible adherence to routines and hyper- or hypo-reactivity to sensory input are other characteristics. The spectrum integrates four pervasive developmental disorders that were considered distinct diagnoses in the DSM-IV: Asperger’s disorder, autistic disorder, childhood disintegrative disorder, and pervasive developmental disorder are not otherwise specified. Prevalence in the U.S. and non-U.S. countries is around 1% of the population [25]. Attention-deficit/hyperactivity disorder (ADHD) is characterized by persistent symptoms of inattention, impulsivity, and/or hyperactivity that interfere with functioning. Inattention may manifest in having difficulty sustaining focus, straying from activities, and being disorganized, for example. Impulsivity is defined by precipitous actions realized without forethought and potentially hurting the person. It may display in deciding without considering consequences and having socially intrusive behaviors. Hyperactivity is shown with excessive and inappropriate motor activity, resulting in extreme restlessness or also talkativeness. In the general population, attention-deficit/hyperactivity disorder is more frequent in boys than in girls. ADHD seems to occur across cultures in about 5% of children and about 2.5% of adults [25].
Among neurocognitive disorders there are major and mild neurocognitive disorders. The major neurocognitive disorder is introduced in DSM-5 as an alternative term to dementia. It is characterized by a significant cognitive decline in one or more cognitive domains including complex attention, learning, language, memory, executive function, perceptual–motor, or social cognition. The cognitive deficits interfere with independence in everyday activities for which the person needs assistance, at least in complex instrumental ones. The maintenance of independent functioning distinguishes the mild and major neurocognitive disorders. Indeed, the mild neurocognitive disorder is characterized by a modest cognitive decline in the same cognitive domains, but cognitive impairment does not interfere with independent functioning in everyday activities [25]. Here, daily tasks become more laborious, and the person needs compensatory strategies [26]. Mild neurocognitive disorder represents a framework for the commonly used diagnosis of mild cognitive impairment (MCI) [26]. Estimates of prevalence for dementia—congruent with major neurocognitive disorder—are about 1–2% at 65 years and 30% by 85 years, while for mild cognitive impairment—congruent with mild neurocognitive disorder—are variable, from 2 to 10% at 65 years and 5 to 25% by 85 years [25].
2. Objectives of LEAP-Motion-Based Interventions
Psychological interventions performed so far with LEAP Motion have had different specific purposes, depending on the nature of the clinical condition considered. However, recurring objectives have typically included the evaluation and/or the enhancement of deficient areas.
Protocols for neurodevelopmental disorders have been aimed to promote, above all, psychomotor and psychosocial rehabilitation in contexts that stimulate learning. Concerning ADHD, interventions have targeted training of sustained and focalized attention, as well as hand–eye coordination [27][28]. This is because ADHD is characterized by an attention-deficit, often linked to fine motor impairments and visuo-spatial skills difficulties, which also have consequences on the learning process [27].
Similarly, ASD interventions have been focused on the improvement of fine motor skills and visual motor integration, fostering attention and motor control [14][29][30][31][32][33], as these functions have been found to be commonly problematic [29]. Learning difficulties have been supported too [34][35]. Additionally, socialization, communication, and independence have been encouraged by specific interventions [15][16][36], given the persistent deficits displayed.
Interventions for neurocognitive disorders typically have targeted cognitive screening, assessment of the impairment, and cognitive rehabilitation. In dementia, the core goals have concerned the evaluation of executive functions and the exercise of everyday activities associated with memory stimulation [37][38][39]. Likewise, in MCI, the cognitive performance has been assessed, and the action impairment has again been the focal point of intervention [23][40][41]. Indeed, declines in these domains are considered defining characteristics of this kind of disorder [42].
3. Protocols of LEAP-Motion-Based Interventions
Interactivity, immersivity, and multi-sensory stimulation are keywords in designing interventions for both neurodevelopmental and neurocognitive disorders. Indeed, LEAP Motion has been introduced in gamified virtual environments for engaging users to complete particular tasks, specifically implemented to assess or strengthen impaired functions. The following sections describe the protocols.
Protocols in neurodevelopmental disorders: ADHD and ASD.
Protocols in neurodevelopmental disorders have been based on the gamified manipulation of virtual objects and multisensory learning.
Hand–eye coordination and fine motor skills have been among the pivotal areas targeted in studies on ADHD. Garcia-Zapirain et al. [28] addressed them in a dual system for the rehabilitation of cognitive functions of children. Using an eye-tracker and LEAP Motion, participants could interact with an arithmetic gamified application and perform operations with numbers displayed on virtual flower’s petals. Users could introduce the correct solution using the eye gaze and the hands, by stretching the same number of fingers as the number of the result. The main outcomes showed that this hand–eye coordination exercise helped to improve users’ skills and attention, whereas the natural interaction devices proved to be engaging alternatives to handwriting or other kinds of interfaces. The underlying idea is that learning requires the interaction of different sensory modalities with activities that stimulate not only visual analysis and cognition, but also physical movements. This is also suggested by Capelo et al. [27] who used LEAP Motion in a multisensory virtual game, in which participants had to place different geometric figures (i.e., blocks, cubes, spheres) in color-matching containers. The authors found an increase in concentration and motivation levels, in a natural and entertaining interaction. Besides, the game promoted relaxation when children interacted with LEAP Motion because the device turned out to be easy to use.
Zhu et al. [30] implemented two similar LEAP-Motion-based games for children with ASD. In the first one, the task was to grasp and put some balls in boxes of the same color, while in the second one, users had to match fruits to some sticks. Despite the small sample size, the authors reported an improvement in fine motor skills and recognition, with the achievement of 100% accuracy in completing the task. Cai et al. [29] replicated the procedure and confirmed the aforementioned enhancements, underlining also a learning transfer of skills and rules. In particular, abilities such as looking at the hands and objects and moving the gaze with them were increased by the game. The author attributed this result to a probable combination of comprehension of the task rules together with the improvement of fine motor skills and recognition in interacting with LEAP Motion. As stated by the authors, this is one of the early attempts to investigate the effect of using gesture-based games for developing such skills in children with ASD.
Furthermore, even Tang et al. [31] considered LEAP Motion as a useful tool in order to train fine motor skills, especially because of its portability. In a first pilot study, they proposed a drawing game [31], whereas in a second study, they investigated an interaction with a domestic environment and in a zoo thanks to a word–image pairing task [31]. The results underlined high levels of sustained attention and showed that engagement with stimulating tasks, which was noticed with minimum training, made children practice specific movements, allowing them to develop motor control and learning towards more complex motor patterns. The authors also reported that parents and caregivers were involved, they noticed their child’s enduring attentiveness and commitment, and this could probably increase the possibility to extend the training at home, contributing to consolidating the learning.
Recently, Tang et al. [32] introduced LEAP Motion in a drum-playing game, observing that it can promote an entertaining learning approach. They also found that the acceptability of the application depended on the task being natural and that the children’s engagement was not influenced by the severity of the disorder.
Syahputra et al. [14] tried to train attention and focus relying on the abilities of children to move virtual objects, in particular collecting coins, while manipulating an item in four labyrinths of increasing difficulty. As a result, LEAP Motion was deemed able to exercise focusing in children.
Likewise, Rahmadiva et al. [33] addressed the focus of children with ASD and their social skills. They described multiple games, including a color-matching game with balls and boxes; a similar one, with fish and containers in a virtual underwater world; an activity of movement across virtual streets following signs and signals to meet virtual people; a game of item selection according to the gaze direction of a virtual character. The results indicated that participants were engaged and that LEAP Motion could be employed as a device in virtual settings for children with autism, even if its use as a means of rehabilitation requires practice.
To teach visual matching skills to students with ASD, Hu et al. [35] proposed an innovative LEAP-Motion-based computer-assisted instruction (CAI) approach. This was compared to a traditional teacher-implemented instruction (TII) approach in a task of daily item matching. Results showed that the innovative CAI was more effective in teaching the target skills to students with ASD, it showed to be more engaging, and some participants achieved a higher level of accuracy during the intervention with it. The authors concluded that it could promote their independence and learning. Hu and Han [34] investigated the same procedure and confirmed the aforementioned outcomes, underlining high task engagement and the maintenance of the acquired skills for three months. Nevertheless, Hu et al. [35] also observed some low accuracy issues because the hand-gesture recognition showed drops with young children’s small hands.
Other studies have been focused on social skills, developing collaborative virtual environments (CVE) with LEAP Motion for children with ASD. Zhao et al. [15][16] designed a series of collaborative games, aiming to foster socialization and communication. Specifically, they implemented a puzzle, a collection, and a delivery game, which required two users to spend an equal and coordinated effort, in order to match, move, and place virtual objects, usually across obstacles. To complete the task, they had to control a virtual tool with two handles, designed for a natural and more immersive experience. Results showed improvements in children’s engagement and motivation, as well as an increase in cooperation patterns and growing spontaneous communication.
Halabi et al. [36] included LEAP Motion and other devices in a virtual-reality-based system aiming to improve the social performance of children with ASD. They proposed a virtual school setting that involved the user in greetings and conversations with a teacher avatar. Usability studies showed that the system had a positive impact on communication skills.
4. Protocols in Neurocognitive Disorders: Dementia and MCI
Protocols in neurocognitive disorders have been based on the gamified simulation of basic behaviors and functional abilities, including personal living.
The pioneering use of LEAP Motion for dementia is described in a pilot study by Tarnanas, Schlee et al. [39]. They employed it together with other devices to collect information about the rate of change in users’ functional impairment in a task of fire evacuation of a virtual apartment, designed with different scenarios of growing difficulty. The authors aimed at improving the ecological validity of such measures as a screening tool for early dementia. The participants had to move on a treadmill to approximate the actual movements in front of a projection screen, and they could interact with the environment thanks to hand gestures (i.e., Leap Motion and Kinect), planning a strategy to evacuate safety. The results showed that virtual reality, motion tracking, and natural tasks could help in pre-dementia diagnosis, executive function assessment, and intervention.
Tarnanas, Mouzakidis et al. [41] examined the same system; in an activity of the daily living module, the psychomotor evaluation was conducted through performance measures in different tasks, to evaluate the users’ understanding and their abilities to perform specific physical tasks accurately. Here, LEAP Motion was used in a finger-tapping test. The outcomes of the study confirmed the possibility to also contribute to MCI diagnosis, by measuring functional abilities in virtual reality with such devices.
Similarly, Martono et al. [40] considered everyday action impairment in a pilot study. They designed a lunch box packing task with specific steps (e.g., taking bread and spreading jelly, wrapping a sandwich, taking cookies and juice) as daily activity in a virtual kitchen on a tablet. LEAP Motion recorded finger movements, and data were used to create clusters of participants; at the same time, the authors realized a performance-based assessment of each user, describing errors made during the exercise. Despite sample limitations, results from a comparison suggested that this approach could be relevant to cluster patients according to virtually assessed symptoms.
Unlike the aforementioned studies, Sacco et al. [38] identified some limitations of LEAP Motion. In a project of virtual training for visuo-spatial abilities in elderly with minor cognitive disorders, LEAP Motion was compared with other devices in a virtual shopping task. The user had to read the name of some products from a shopping list, to identify the correct lane of the market to find them, and finally, to select the right items on the shelves. LEAP Motion showed to be influenced by light and to have some lack of accuracy, due to the fact that the hand obstructs the tracking when it is perpendicular to the device.
Nevertheless, Chua et al. [23] used virtual reality and LEAP Motion to mimic everyday activities in three-dimensional games, from which to assess not only executive functions, but also memory, perceptual motor skills, and learning. Seven activities were proposed: users had to open a door by means of the right key and a code, to make a phone call typing a number, to identify famous people, groceries advertisement and numbers on a newspaper, to organize house objects in categories, to select an outfit according to a specific occurrence, to take cash from a teller machine, and to do shopping. Preliminary outcomes concluded that virtual reality and LEAP Motion could be used for the screening of cognitive functions in older people in primary care settings.
Vallejo et al. [37] implemented a table preparation task in a virtual kitchen setting, in which the aim was to place some kitchenware accurately and quickly, stimulating executive functions and response time. The author compared the usability of LEAP Motion to another interface (i.e., Razer Hydra) and found that participants preferred the first one, even if they were faster to finish the task using the last one. However, conclusions showed that LEAP Motion represented well the reality of movements such as taking and displacing, and it seemed promising for virtual rehabilitation.
5. Background for LEAP-Motion-Based Interventions
The reviewed studies have analyzed the use of LEAP-Motion-based gesture interaction systems in interventions for different clinical populations. Protocols were designed to target various psycho-motor functions and psycho-social skills, on the basis of evidence coming from studies in the field of virtual reality and motion-based gaming.
Those studies have shown that games can provide safe environments for practicing in various tasks, as many times as the user needs, and can also improve learning from mistakes owing to a motivating real-time feedback [29] and self-paced activities. Indeed, research indicates that children with ASD can learn how to behave in social settings when they constantly train in specific situations [43], whereas extended practice of everyday activities can enhance performance in people with neurocognitive disorders [40].
Moreover, evidence shows that games can promote improvements in hand–eye coordination and visuospatial skills [44], also encouraging decision making and cognitive strategies [27]. Motion-based gaming can foster learning, attention [45], and psycho-motor skills, due to the continuous need of motor actions [27]. This is relevant in designing game-based protocols given that these areas are particularly important for all the aforementioned clinical populations, especially in ADHD and in ASD.
Other evidence deals with engagement; for instance, the interaction of children with ASD with natural electronic devices show a high involvement with virtual reality [46][47][48][49], making them actively engaged [50][51] and avoiding being overburdened by stimuli as happens in human interactions [47]. This turns out to be useful for rehabilitation interventions and screening.
Furthermore, virtual reality can generate ecological validity [39], involving participants in the task with a minor focus on the testing procedure, contrary to traditional measures [52][53]. As shown in studies on neurocognitive disorders, gesture-based games can also allow for assessing executive functions and perceptual motor functions that often are only partially considered in paper-and-pencil screening tools [54].
In summary, whilst the reviewed studies were based on such previous evidence on the usefulness of virtual-reality-based procedures, they not only confirmed those preliminary findings, but especially showed the potential (as well as the current limitations) of the use of the LEAP Motion technology to that aim.
6. Technology Weaknesses and Future Challenges
Alongside positive impact outcomes, some technology weaknesses have been reported. Accuracy issues have been noted in LEAP Motion tacking ability; particularly, it has been found to be weaker when the hand is positioned perpendicularly to the device, and to be influenced by light [38]. Moreover, some studies reported negative feedback addressing LEAP Motion lacking sensitivity with younger children’s hands that were too small to be correctly detected [15][35]. This led to their exclusion from the study or to a sub-optimal fit to its usage.
Thence, future modifications would be needed to adjust its abilities in order to also fit with children’s characteristics, thus supporting not only a better game experience but also an improved validity in studies including it.
References
- Carpenter-Song, E. Promoting Meaningful Recovery with Digital Mental Health Care. Epidemiol. Psychiatr. Sci. 2020, 29.
- Lustgarten, S.D.; Elhai, J.D. Technology Use in Mental Health Practice and Research: Legal and Ethical Risks. Clin. Psychol. Sci. Pract. 2018, 25, e12234.
- Weichert, F.; Bachmann, D.; Rudak, B.; Fisseler, D. Analysis of the Accuracy and Robustness of the Leap Motion Controller. Sensors 2013, 13, 6380–6393.
- Wozniak, P.; Vauderwange, O.; Mandal, A.; Javahiraly, N.; Curticapean, D. Possible Applications of the LEAP Motion Controller for More Interactive Simulated Experiments in Augmented or Virtual Reality. In Proceedings of the Optics Education and Outreach IV, San Diego, CA, USA, 27 September 2016; International Society for Optics and Photonics: Bellingham, WA, USA, 2016; Volume 9946.
- Kurschl, W.; Augstein, M.; Burger, T.; Pointner, C. User Modeling for People with Special Needs. Int. J. Pervasive Comput. Commun. 2014, 10, 313–336.
- Braun, M.; Wölfel, M.; Renner, G.; Menschik, C. Accessibility of Different Natural User Interfaces for People with Intellectual Disabilities. In Proceedings of the 2020 International Conference on Cyberworlds (CW), Caen, France, 19 September–1 October 2020; pp. 211–218.
- Sharma, S.; Varkey, B.; Achary, K.; Hakulinen, J.; Turunen, M.; Heimonen, T.; Srivastava, S.; Rajput, N. Designing Gesture-Based Applications for Individuals with Developmental Disabilities: Guidelines from User Studies in India. ACM Trans. Access. Comput. 2018, 11, 1–27.
- Chang, Y.-J.; Chen, S.-F.; Huang, J.-D. A Kinect-Based System for Physical Rehabilitation: A Pilot Study for Young Adults with Motor Disabilities. Res. Dev. Disabil. 2011, 32, 2566–2570.
- Webster, D.; Celik, O. Systematic Review of Kinect Applications in Elderly Care and Stroke Rehabilitation. J. Neuroeng. Rehabil. 2014, 11, 108.
- Boutsika, E. Kinect in Education: A Proposal for Children with Autism. Procedia Comput. Sci. 2014, 27, 123–129.
- Retalis, S.; Korpa, T.; Skaloumpakas, C.; Boloudakis, M.; Kourakli, M.; Altanis, I.; Siameri, F.; Papadopoulou, P.; Lytra, F.; Pervanidou, P. Empowering Children With ADHD Learning Disabilities With the Kinems Kinect Learning Games. In Proceedings of the European Conference on Games Based Learning, Berlin, Germany, 9–10 October 2014; Volume 2, p. 469.
- Perhakaran, G.; Yusof, A.M.; Rusli, M.E.; Yusoff, M.Z.M.; Mahidin, E.M.M.; Mahalil, I.; Zainuddin, A.R.R. SnoezelenCAVE: Virtual Reality CAVE Snoezelen Framework for Autism Spectrum Disorders. In Advances in Visual Informatics; Badioze Zaman, H., Robinson, P., Smeaton, A.F., Shih, T.K., Velastin, S., Jaafar, A., Mohamad Ali, N., Eds.; Springer International Publishing: Cham, Switzerland, 2015; pp. 443–453.
- Schroeder, P.A.; Lohmann, J.; Butz, M.V.; Plewnia, C. Behavioral Bias for Food Reflected in Hand Movements: A Preliminary Study with Healthy Subjects. Cyberpsychol. Behav. Soc. Netw. 2015, 19, 120–126.
- Syahputra, M.F.; Sari, P.P.; Arisandi, D.; Abdullah, D.; Napitupulu, D.; Setiawan, M.I.; Albra, W.; Asnawi; Andayani, U. Implementation of Augmented Reality to Train Focus on Children with s Pecial Needs. J. Phys. Conf. Ser. 2018, 978, 012109.
- Zhao, H.; Swanson, A.; Weitlauf, A.; Warren, Z.; Sarkar, N. A Novel Collaborative Virtual Reality Game for Children with ASD to Foster Social Interaction. In Universal Access in Human-Computer Interaction. Users and Context Diversity; Antona, M., Stephanidis, C., Eds.; Springer International Publishing: Cham, Switzerland, 2016; pp. 276–288.
- Zhao, H.; Swanson, A.R.; Weitlauf, A.S.; Warren, Z.E.; Sarkar, N. Hand-in-Hand: A Communication-Enhancement Collaborative Virtual Reality System for Promoting Social Interaction in Children With Autism Spectrum Disorders. IEEE Trans. Hum. Mach. Syst. 2018, 48, 136–148.
- Ebner, M.; Spot, N. Game-Based Learning with the Leap Motion Controller. Handb. Res. Gaming Trends P-12 Educ. 2015, 555–565.
- Kuntz, N.; Adams, J.A.; Zahr, L.; Killen, R.; Cameron, K.; Wasson, H. Therapeutic Play and Bone Marrow Transplantation. J. Pediatr. Nurs. 1996, 11, 359–367.
- O’Connell, S.R. Recreation Therapy: Reducing the Effects of Isolation for the Patient in a Protected Environment. Child. Health Care 1984, 12, 118–121.
- Dumoulin, S.; Bouchard, S.; Ellis, J.; Lavoie, K.L.; Vézina, M.-P.; Charbonneau, P.; Tardif, J.; Hajjar, A. A Randomized Controlled Trial on the Use of Virtual Reality for Needle-Related Procedures in Children and Adolescents in the Emergency Department. Games Health J. 2019, 8, 285–293.
- Indovina, P.; Barone, D.; Gallo, L.; Chirico, A.; De Pietro, G.; Giordano, A. Virtual Reality as a Distraction Intervention to Relieve Pain and Distress During Medical Procedures. Clin. J. Pain 2018, 34, 858–877.
- Piskorz, J.; Czub, M. Effectiveness of a Virtual Reality Intervention to Minimize Pediatric Stress and Pain Intensity during Venipuncture. J. Spec. Pediatr. Nurs. 2018, 23, e12201.
- Chua, S.I.L.; Tan, N.C.; Wong, W.T.; Allen, J.C., Jr.; Quah, J.H.M.; Malhotra, R.; Østbye, T. Virtual Reality for Screening of Cognitive Function in Older Persons: Comparative Study. J. Med. Internet Res. 2019, 21, e14821.
- Harrison, K.E. Sharing a (Cyber)Space: Fostering Relationship Maintenance in Residential Care through Virtual Reality; UC Santa Barbara: California, CA, USA, 2019.
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: Dsm-5, 5th ed.; Amer Psychiatric Pub Inc.: Washington, DC, USA, 2013; ISBN 978-0-89042-555-8.
- Sachdev, P.S.; Blacker, D.; Blazer, D.G.; Ganguli, M.; Jeste, D.V.; Paulsen, J.S.; Petersen, R.C. Classifying Neurocognitive Disorders: The DSM-5 Approach. Nat. Rev. Neurol. 2014, 10, 634–642.
- Capelo, D.C.; Sánchez, M.E.; Hurtado, J.S.; Chicaiza, D.B. Multisensory Virtual Game with Use of the Device Leap Motion to Improve the Lack of Attention in Children of 7–12 Years with ADHD. In Proceedings of the International Conference on Information Technology & Systems (ICITS 2018); Rocha, Á., Guarda, T., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 897–906.
- Garcia-Zapirain, B.; de la Torre Díez, I.; López-Coronado, M. Dual System for Enhancing Cognitive Abilities of Children with ADHD Using Leap Motion and Eye-Tracking Technologies. J. Med. Syst. 2017, 41, 111.
- Cai, S.; Zhu, G.; Wu, Y.-T.; Liu, E.; Hu, X. A Case Study of Gesture-Based Games in Enhancing the Fine Motor Skills and Recognition of Children with Autism. Interact. Learn. Environ. 2018, 26, 1039–1052.
- Zhu, G.; Cai, S.; Ma, Y.; Liu, E. A Series of Leap Motion-Based Matching Games for Enhancing the Fine Motor Skills of Children with Autism. In Proceedings of the 2015 IEEE 15th International Conference on Advanced Learning Technologies, Hualien, Taiwan, 6–9 July 2015; pp. 430–431.
- Tang, T.Y.; Falzarano, M.; Morreale, P.A. Engaging Chinese Children with Autism to Interact with Portable Hand- and Finger-Gesture Based Applications: Experiment and Reflections. In Learning and Collaboration Technologies; Zaphiris, P., Ioannou, A., Eds.; Springer International Publishing: Cham, Switzerland, 2016; pp. 562–572.
- Tang, T.Y.; Falzarano, M.; Morreale, P.A. Assessment of the Utility of Gesture-Based Applications for the Engagement of Chinese Children with Autism. Univers. Access Inf. Soc. 2018, 17, 275–290.
- Rahmadiva, M.; Arifin, A.; Fatoni, M.H.; Baki, S.H.; Watanabe, T. A Design of Multipurpose Virtual Reality Game for Children with Autism Spectrum Disorder. In Proceedings of the 2019 International Biomedical Instrumentation and Technology Conference (IBITeC), Piscataway, NJ, USA, 23–24 October 2019; Volume 1, pp. 1–6.
- Hu, X.; Han, Z.R. Effects of Gesture-Based Match-to-Sample Instruction via Virtual Reality Technology for Chinese Students with Autism Spectrum Disorders. Int. J. Dev. Disabil. 2019, 65, 327–336.
- Hu, X.; Lee, G.T.; Tsai, Y.-T.; Yang, Y.; Cai, S. Comparing Computer-Assisted and Teacher-Implemented Visual Matching Instruction for Children with ASD and/or Other DD. J. Autism Dev. Disord. 2020, 50, 2540–2555.
- Halabi, O.; Elseoud, S.A.; Alja’am, J.M.; Alpona, H.; Al-Hemadi, M.; Al-Hassan, D. Immersive Virtual Reality in Improving Communication Skills in Children with Autism. Int. J. Interact. Mob. Technol. IJIM 2017, 11, 146–158.
- Vallejo, V.; Tarnanas, I.; Yamaguchi, T.; Tsukagoshi, T.; Yasuda, R.; Müri, R.M.; Mosimann, U.P.; Nef, T. Usability Assessment of Natural User Interfaces during Serious Games: Adjustments for Dementia Intervention. J. Pain Manag. 2015, 9, 333–339.
- Sacco, M.; Redaelli, C.; Zangiacomi, A.; Greci, L.; Di Santo, S.; Leone, A.; Vezzoli, A. GOJI an Advanced Virtual Environment Supporting Training of Physical and Cognitive Activities to Prevent Dementia Occurrence in Elderly with Minor Cognitive Disorders. In Ambient Assisted Living: Italian Forum 2014; Andò, B., Siciliano, P., Marletta, V., Monteriù, A., Eds.; Biosystems & Biorobotics; Springer International Publishing: Cham, Switzerland, 2015; pp. 429–437. ISBN 978-3-319-18374-9.
- Tarnanas, I.; Schlee, W.; Tsolaki, M.; Müri, R.; Mosimann, U.; Nef, T. Ecological Validity of Virtual Reality Daily Living Activities Screening for Early Dementia: Longitudinal Study. JMIR Serious Games 2013, 1, e2778.
- Martono, N.P.; Yamaguchi, T.; Ohwada, H. Utilizing Finger Movement Data to Cluster Patients with Everyday Action Impairment. In Proceedings of the 2016 IEEE 15th International Conference on Cognitive Informatics Cognitive Computing (ICCI*CC), Palo Alto, CA, USA, 22–23 August 2016; pp. 459–464.
- Tarnanas, I.; Mouzakidis, C.; Schlee, W. Functional Impairment in Virtual-Reality-Daily-Living-Activities as a Defining Feature of Amnestic MCI: Cognitive and Psychomotor Correlates. In Proceedings of the 2013 International Conference on Virtual Rehabilitation (ICVR), Piscataway, NJ, USA, 26–29 August 2013; pp. 27–34.
- Ganguli, M. Can the DSM-5 Framework Enhance the Diagnosis of MCI? Neurology 2013, 81, 2045–2050.
- Maglione, M.A.; Gans, D.; Das, L.; Timbie, J.; Kasari, C.; The Technical Expert Panel; HRSA Autism Intervention Research—Behavioral (AIR-B) Network. Nonmedical Interventions for Children With ASD: Recommended Guidelines and Further Research Needs. Pediatrics 2012, 130, S169–S178.
- Vinkler, M.; Sochor, J. Integrating Motion Tracking Sensors to Human-Computer Interaction with Respect to Specific User Needs. In Proceedings of the The 18th Central European Seminar on Computer Graphics, Smolenice, Slovakia, 25–27 May 2014; Volume 26, p. 2014.
- Bartoli, L.; Corradi, C.; Garzotto, F.; Valoriani, M. Exploring Motion-Based Touchless Games for Autistic Children’s Learning. In Proceedings of the 12th International Conference on Interaction Design and Children, New York, NY, USA, 24 June 2013; Association for Computing Machinery: New York, NY, USA, 2013; pp. 102–111.
- Pennington, R.C. Computer-Assisted Instruction for Teaching Academic Skills to Students With Autism Spectrum Disorders: A Review of Literature. Focus Autism Dev. Disabil. 2010, 25, 239–248.
- Salter, T.; Davey, N.; Michaud, F. Designing Developing QueBall, a Robotic Device for Autism Therapy. In Proceedings of the The 23rd IEEE International Symposium on Robot and Human Interactive Communication, Edinburgh, UK, 25–29 August 2014; pp. 574–579.
- Sansosti, F.J.; Doolan, M.L.; Remaklus, B.; Krupko, A.; Sansosti, J.M. Computer-Assisted Interventions for Students with Autism Spectrum Disorders within School-Based Contexts: A Quantitative Meta-Analysis of Single-Subject Research. Rev. J. Autism Dev. Disord. 2014, 2, 128–140.
- Shane, H.C.; Albert, P.D. Electronic Screen Media for Persons with Autism Spectrum Disorders: Results of a Survey. J. Autism Dev. Disord. 2008, 38, 1499–1508.
- Parsons, S.; Cobb, S. State-of-the-Art of Virtual Reality Technologies for Children on the Autism Spectrum. Eur. J. Spec. Needs Educ. 2011, 26, 355–366.
- Strickland, D. Virtual Reality for the Treatment of Autism. Stud. Health Technol. Inform. 1997, 44, 81–86.
- Cesa, G.L.; Manzoni, G.M.; Bacchetta, M.; Castelnuovo, G.; Conti, S.; Gaggioli, A.; Mantovani, F.; Molinari, E.; Cárdenas-López, G.; Riva, G. Virtual Reality for Enhancing the Cognitive Behavioral Treatment of Obesity With Binge Eating Disorder: Randomized Controlled Study With One-Year Follow-Up. J. Med. Internet Res. 2013, 15, e113.
- Rizzo, A.A.; Buckwalter, J.G. Virtual Reality and Cognitive Assessment and Rehabilitation: The State of the Art. Stud. Health Technol. Inform. 1997, 44, 123–145.
- Cullen, B.; O’Neill, B.; Evans, J.J.; Coen, R.F.; Lawlor, B.A. A Review of Screening Tests for Cognitive Impairment. J. Neurol. Neurosurg. Psychiatry 2007, 78, 790–799.




