
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Sathyanarayanan Doraiswamy | + 2488 word(s) | 2488 | 2021-03-11 07:40:05 | | | |
| 2 | Lily Guo | Meta information modification | 2488 | 2021-03-22 10:30:27 | | | | |
| 3 | Lily Guo | Meta information modification | 2488 | 2021-03-22 10:31:04 | | |
Video Upload Options
Globally, the COVID-19 pandemic has affected older people disproportionately. Prior to the pandemic, some studies reported that telehealth was an efficient and effective form of health care delivery, particularly for older people. There has been increased use of telehealth and publication of new literature on this topic during the pandemic, so we conducted a scoping review and evidence synthesis for telehealth use in geriatric care to summarize learning from these new data.
1. Introduction
Globally, the COVID-19 pandemic has affected older people disproportionately. One estimate identifies that older people over 65 years of age have a mortality risk 100 times greater than those in younger age groups [1]. The increased vulnerability of older people to respiratory epidemics, including COVID-19, is multifactorial, driven by biological, behavioral, demographic, health care accessibility, and social determinants [2]. Among these factors, the lack of access to health care for older people is an emerging and worrying trend. Some factors contributing to this during the current pandemic are (a) an overwhelmed health sector unable to prioritize health care needs of older people, (b) the restriction of movement and lockdowns imposed as prevention measures, and the consequent challenges faced by older people trying to access health care facilities, and (c) concern and fear among older people and their caregivers of contracting COVID-19 while seeking care from health facilities. Lack of timely access to healthcare services poses an additional risk of morbidity and mortality for older people [3].
Countries and health care institutions committed to providing care to the older population have used innovative methods to ensure availability and access to health care services for older people [4], notably the use of telehealth. Prior to the pandemic, some studies reported that telehealth was an efficient and effective form of health care delivery, particularly for older people [5]. However, despite the availability of telehealth services, uptake was limited due to skepticism from both patients and the service providers. Other factors hindering the scaling-up of telehealth services prior to the pandemic included concerns for patient safety, data confidentiality, absence of in-person physical examination by health providers, lack of access to technology, legal restrictions, and ambiguous health insurance coverage policies [6]. Questions were also raised about the technological literacy of older people and whether telehealth would meet the needs of older people with cognitive decline or those with auditory and/or visual impairments [7].
With the onset of the COVID-19 pandemic, a rapid scale-up of telehealth services was noted globally as countries began to relax legal restrictions regarding the use of telehealth for the provision of health care services. While insurance companies in some countries had included limited telehealth services in their coverage pre-COVID-19, the scale and scope of coverage for telehealth have rapidly increased during the pandemic [8][9]. There is now a growing optimism on the global use of telehealth services in several specialties, and the field of geriatrics is no exception. Various models for the provision of telehealth services to older people have emerged during the pandemic and their strengths/opportunities highlighted [10]. However, weaknesses and threats to telehealth readiness among older people have also emerged [11]. There is a growing call to learn from the pandemic experience and contribute to the emerging knowledge on telehealth use for older people during this period. This will also improve availability, accessibility, affordability, quality, and demand generation for telehealth among older people during the ongoing pandemic and beyond.
In this article, we use the term ‘geriatrics’ to describe the whole spectrum of health care services for older people, inclusive of preventative, curative, and rehabilitative components. The term ‘telehealth’ is not currently standardized. Currently, it can include a broader perspective using such terms as e-health and digital medicine, or it can have a more specific focus such as teleneurology and telestroke. We define telehealth as the provision of health care remotely (where the patient and the health care provider do not physically meet in person). This is explained in additional detail under the sub-section ‘terminologies’ within the Methods section. Both telehealth as a specialized field in information and communication technology and geriatrics as a specialty of medicine are predominantly available in high-income countries [12][13].
It should be noted that telehealth is still in evolution, and geriatrics is a nuanced specialty given that older adults and their caregivers have unique needs [14]. The provision of telehealth services for populations who live in residential care facilities, such as nursing homes and long-term care facilities, can also be cumbersome. The provision of telehealth services in these contexts needs to be understood further. In any other population, telehealth services would largely mean service provision at the patient’s home (with the exception of specialist care from higher-level health facilities) [15].
A scoping review is an ideal tool to understand the breadth and depth of published literature on topics that are unclear, whereas a systematic review is better to address more specific questions on well-researched topics [16]. Munn et al. (2018) provide guidance for authors on how to choose between a systematic review and a scoping review [17]. Since our intention was not to answer a single clinically relevant question but rather to identify specific concepts/characteristics relevant to telehealth use in geriatrics during the COVID-19 pandemic, a scoping review was the preferred methodology [17][18]. This approach resonates with Arksey and O’Malley’s recommendations regarding specific circumstances in which scoping reviews add value [19]. We believe that a scoping review of telehealth use in geriatrics will provide a baseline view of key concepts and characteristics in the intersection of telehealth and geriatrics, identify and analyze gaps in the knowledge base for geriatric telehealthcare during COVID-19, and serve as a stimulus for future systematic reviews. We designed our scoping review and evidence synthesis to answer the research question, “What can we learn from published literature about the availability, accessibility (including demand and utilization), affordability, and quality of telehealth services in geriatric care during the COVID-19 pandemic?”
2. Search Strategy
We systematically searched PubMed, Embase, and the WHO COVID-19 global research database for articles published between 1 January and 20 August 2020 with no geographic and language limitations, using a combination of keywords as well as a controlled vocabulary. The start date of the search strategy (1 January 2020) corresponded to the earliest date when literature in the COVID-19 context was likely to have been published (the first cluster of cases were reported in Wuhan, China, 31 December 2019) [20]. 20 August 2020 was the last day we conducted the search in all three databases.
Good practice in conducting a scoping review involves searching at least two online databases [21][22]. We included a third database to improve the comprehensiveness of our search. Notably, Pubmed and Embase are the preferred databases for searching primary studies as part of scoping and systematic reviews [23]. Pubmed, as a proxy to MEDLINE, provides extensive coverage to the point where some authors have suggested that doing a Pubmed search alone may be sufficient for reviews [24]. Embase serves as a good complement to Pubmed and is known to produce unique references along with coverage of second-tier European and Asian journals [23]. With the inclusion of several databases in one online database, the WHO’s COVID-19 global research database increases the prospects of newly published articles that may not have yet been indexed in Pubmed and Embase [25].
We built the search strategy step-by-step according to the JBI manual for scoping review [21][22]. Firstly, a limited search was conducted on Pubmed and Embase for relevant articles. The initial search was followed by an analysis of the text words contained in the title and abstract of retrieved articles and of the index terms used to describe the articles. This helped us develop the three concepts for our search strategy: (a) COVID-19, (b) telehealth/telemedicine, and (c) old age. These concepts and the final choice of our databases were discussed and agreed upon in consultation with a senior librarian. Thereafter, an initial set of key terms was developed for our search strategy through a systematic brainstorming process involving all authors, each of whom has significant experience publishing scoping and systematic reviews together. On the advice of the senior librarian, we further compared our key terms with the terms included in the search strategy compilations done by the Medical Library Association [26]. The final search strategy was validated by the librarian and the senior authors. We then carried out a second search using all identified keywords and index terms in the three databases. It is to note that Pubmed (MeSH) [27] and Embase (EMTREE) [28] use specific systems of classification of keywords. Our search included words borrowed from the respective systems of the classification used by these databases. However, the WHO global COVID-19 database permits the use of keywords only, and our search strategy for this database was drawn from our search strategy in Pubmed and Embase. Thirdly, the reference list of articles in the included full-texts was searched for additional articles. The detailed search strategy for each of the databases is available in File S2.
3. Selection of Articles
After duplicate removal, our search strategy identified 548 articles relevant to our review. Of these, 446 articles were excluded at the stage of title and abstract screening and another 30 articles during full-text screening. Among the 30 articles excluded after the full-text screening, twelve articles dealt with issues such as electronic health records, artificial intelligence, and computational analysis, which are not traditionally considered to be part of telehealth; twelve articles used information technology to conduct research; two articles discussed past pandemics; two were studies carried out before the onset of the COVID-19 pandemic; one article was a simulation study to assess adverse drug events; one article was a study protocol. Our supplementary search of the reference lists from the included articles yielded an additional seven articles relevant to our review. A total of 79 articles were finally included in our scoping review. The PRISMA flowchart representing the article selection process is included in Figure 1.
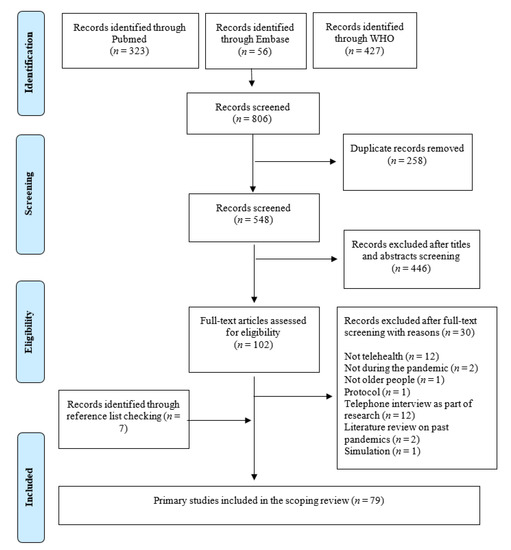
Figure 1. PRISMA 2009 flowchart of the scoping review’s inclusion.
4. Discussion
Our scoping review and evidence synthesis summarizes data and information from 79 articles pertaining to telehealth use for the provision of geriatric care. During the COVID-19 pandemic, physical distancing for older people has been recognized as a mechanism to mitigate spread in this high-risk category and thus been implemented in several countries worldwide. This has also allowed more flexibility for telehealth use in geriatric care.
4.1. Availability, Accessibility, Affordability, and Quality of Telehealth in Geriatric Care during the COVID-19 Pandemic
COVID-19 has demonstrated the value of telehealth in providing geriatric care during the pandemic. Relying on telehealth to provide continuity of geriatric care services and avoid the risk of contagion by reducing the need for visiting health care facilities has been shown to be feasible during the pandemic [29]. It is noteworthy that a majority of the articles in this review were written in the context of high-income countries, notably the United States of America (USA), and were published predominantly in geriatrics-related journals published in those countries. This is similar to other studies, which have found that the vast majority of published articles on telehealth were from studies carried out in high-income countries, and a vast majority of them were from the USA [9]. In high-income countries, access to and use of telehealth for older people has improved during the pandemic. This occurred due to the relaxation of legal restrictions for providing health care and the inclusion of telehealth as a reimbursable service by insurance companies in countries such as Australia [30]. The same cannot be said about low- and low-middle-income countries from which the telehealth literature is sparse.
A wide application of telehealth services has been seen during the pandemic in both home and long-term care settings in which older people live. In long-term care settings, telehealth has been used as an adjunct to provide collaborative support for getting advice from multiple specialists concurrently. The articles included in our review provide some evidence of the application of telehealth in providing a whole spectrum of health care services, including preventative, curative, and rehabilitative services but with a greater focus on curative services.
Among the curative services provided to older people during the pandemic, our review finds that there is more literature on telehealth application for neuropsychiatry services than other specialty services. This finding reflects the fact that frailty and dementia are the more common conditions managed by telehealth services. There seems to be a limited number of other medical specialties using telehealth to provide services to older people. Worldwide though, the use of telehealth in other specialties such as dermatology, pathology, and radiology has been well documented as part of non-geriatric health care [31]. There is much potential to expand various telehealth services to older people in the future.
Only a small proportion of the articles identified in our review were based on empirical research, so there is clearly a need for additional research to generate good quality evidence on telehealth use by older people. Nevertheless, the available evidence provides invaluable information. Prior to COVID-19, telehealth was not widely available to older people, citing a lack of capacity on their part to navigate the technology needed for its use [32]. However, a majority of the articles in our review report an increasing interest and uptake of telehealth by older people since the onset of the COVID-19 pandemic. When telehealth is provided in an age-friendly manner with active collaboration between older persons and their health care providers, we are likely to see an increased service uptake [32]. This is a significant finding.
4.2. Strengths, Weakness, Opportunities, and Threats for Telehealth Use in Geriatric Care during the COVID-19 Pandemic
In our SWOT analysis, strengths identified for telehealth use in geriatric care are the convenience and affordability for older people. The weaknesses identified showcase that telehealth as a field must evolve and adapt to meet the needs of older people, specifically those with physical and cognitive limitations. Also, the gap in telehealth knowledge and capacity for use by health care providers must be addressed. The threats focus on inequity and the lack of standardization in the provision of age-friendly telehealth services. The articles included in our review identify opportunities primarily in the technological advancements driven by simplicity and user-friendliness. All these identified areas offer broad scope for future exploration.
4.3. Implications for Practice and Research Gaps
Given global concerns on the quality of publications that emerged since the onset of the pandemic [33][34], our decision to exclude gray literature and restrict our search to peer-reviewed articles only can be seen as the most appropriate approach to synthesize available evidence. Our scoping review found that optimizing telehealth services for older people requires broader engagement with broader participation by older people, their caregivers, physicians, and other health care providers, as well as technology experts and health managers. Our scoping review found a limited number of articles that can answer questions on the safety, utility, scalability, cost-effectiveness, and demand for telehealth use in geriatrics. Therefore, there is a clear need for additional research in these areas during the pandemic and beyond. There is also a need to address the lack of standardization of telehealth terminologies used in the geriatric context [35].
References
- Ioannidis, J.P.; Axfors, C.; Contopoulos-Ioannidis, D.G. Population-level COVID-19 mortality risk for non-elderly individuals overall and for non-elderly individuals without underlying diseases in pandemic epicenters. Environ. Res. 2020, 188, 109890.
- Doraiswamy, S.; Mamtani, R.; Ameduri, M.; Abraham, A.; Cheema, S. Respiratory epidemics and older people. Age Ageing 2020, 49, 896–900.
- United Nations. Policy Brief: The Impact of COVID-19 on Older Persons; United Nations: New York, NY, USA, 2020.
- Vergara, J.; Parish, A.; Smallheer, B. Telehealth: Opportunities in geriatric patient care during COVID-19. Geriatr. Nurs. 2020, 41, 657–658.
- Merrell, R.C. Geriatric Telemedicine: Background and Evidence for Telemedicine as a Way to Address the Challenges of Geriatrics. Healthc. Inform. Res. 2015, 21, 223–229.
- Lustig, T.A. The Role of Telehealth in an Evolving Health Care Environment: Workshop Summary; National Academies Press: Washington, DC, USA, 2012.
- Foster, M.V.; Sethares, K.A. Facilitators and barriers to the adoption of telehealth in older adults: An integrative review. Comput. Inform. Nurs. 2014, 32, 523–533.
- Wosik, J.; Fudim, M.; Cameron, B.; Gellad, Z.F.; Cho, A.; Phinney, D.; Curtis, S.; Roman, M.; Poon, E.G.; Ferranti, J.; et al. Telehealth transformation: COVID-19 and the rise of virtual care. J. Am. Med. Inform. Assoc. 2020, 27, 957–962.
- Doraiswamy, S.; Abraham, A.; Mamtani, R.; Cheema, S. Use of Telehealth during the COVID-19 Pandemic: Scoping Review. J. Med. Internet Res. 2020, 22, e24087.
- Tan, L.F.; Teng, V.H.W.; Seetharaman, S.K.; Yip, A.W. Facilitating telehealth for older adults during the COVID-19 pandemic and beyond: Strategies from a Singapore geriatric center. Geriatr. Gerontol. Int. 2020, 20, 993–995.
- Lam, K.; Lu, A.D.; Shi, Y.; Covinsky, K.E. Assessing Telemedicine Unreadiness Among Older Adults in the United States during the COVID-19 Pandemic. JAMA Intern. Med. 2020, 180, 1389.
- Mangoni, A.A. Geriatric medicine in an aging society: Up for a challenge? Front. Med. 2014, 1, 10.
- Dotchin, C.L.; Akinyemi, R.O.; Gray, W.K.; Walker, R.W. Geriatric medicine: Services and training in Africa. Age Ageing 2012, 42, 124–128.
- Brubaker, J. (Ed.) The Birth of a New Specialty: Geriatrics. J. Lanc. Gen. Hosp. 2008, 3, 105–107.
- Cimperman, M.; Brenčič, M.M.; Trkman, P.; Stanonik Mde, L. Older adults’ perceptions of home telehealth services. Telemed. J. e-Health 2013, 19, 786–790.
- Peterson, J.; Pearce, P.F.; Ferguson, L.A.; Langford, C.A. Understanding scoping reviews: Definition, purpose, and process. J. Am. Assoc. Nurse Pract. 2017, 29, 12–16.
- Munn, Z.; Peters, M.D.J.; Stern, C.; Tufanaru, C.; McArthur, A.; Aromataris, E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med. Res. Methodol. 2018, 18, 1–7.
- Anderson, S.; Allen, P.; Peckham, S.; Goodwin, N. Asking the right questions: Scoping studies in the commissioning of research on the organisation and delivery of health services. Health Res. Policy Syst. 2008, 6, 7.
- Arksey, H.; O’Malley, L. Scoping studies: Towards a methodological framework. Int. J. Soc. Res. Methodol. 2005, 8, 19–32.
- WHO. Novel Coronavirus—China; WHO: Geneva, Switzerland, 2020.
- Peters, M.; Godfrey, C.; McInerney, P. Scoping Reviews, Joanna Briggs Institute Reviewer Manual [Internet]; The Joanna Briggs Institute: Adelaide, Australia, 2017; Chapter 11.
- Peters, M.D.; Godfrey, C.M.; Khalil, H.; McInerney, P.; Parker, D.; Soares, C.B. Guidance for conducting systematic scoping reviews. Int. J. Evid.-Based Healthc. 2015, 13, 141–146.
- Bain, P. Research Guides: Systematic Reviews and Meta Analysis: Databases and Sources; Harvard Library: Boston, MA, USA, 2021; Available online: (accessed on 7 January 2021).
- Halladay, C.W.; Trikalinos, T.A.; Schmid, I.T.; Schmid, C.H.; Dahabreh, I.J. Using data sources beyond PubMed has a modest impact on the results of systematic reviews of therapeutic interventions. J. Clin. Epidemiol. 2015, 68, 1076–1084.
- World Health Organization. COVID-19 Global Literature on Coronavirus Disease. 2021. Available online: (accessed on 20 August 2020).
- Association, M.L. MLA: COVID-19 Literature Searching. 2020. Available online: (accessed on 1 January 2021).
- Lipscomb, C.E. Medical Subject Headings (MeSH). Bull. Med. Libr. Assoc. 2000, 88, 265–266.
- Knight, S.R.; Pengel, L.H.M.; Morris, P.J. Evidence in Transplantation. In Kidney Transplantation—Principles and Practice, 7th ed.; Morris, P.J., Knechtle, S.J., Eds.; W.B. Saunders: Philadelphia, PA, USA, 2014; Chapter 42; pp. 729–736.
- Mann, D.M.; Chen, J.; Chunara, R.; Testa, P.A.; Nov, O. COVID-19 transforms health care through telemedicine: Evidence from the field. J. Am. Med. Inform. Assoc. 2020, 27, 1132–1135.
- Fisk, M.; Livingstone, A.; Pit, S.W. Telehealth in the Context of COVID-19: Changing Perspectives in Australia, the United Kingdom, and the United States. J. Med. Internet Res. 2020, 22, e19264.
- World Health Organization. Telemedicine: Opportunities and Developments in Member States; Report on the Second Global Survey on eHealth; World Health Organization: Geneva, Switzerland, 2010.
- Bujnowska-Fedak, M.; Grata-Borkowska, U. Use of telemedicine-based care for the aging and elderly: Promises and pitfalls. Smart Homecare Technol. TeleHealth 2015, 2015, 91–105.
- Horbach, S.P.J.M. Pandemic publishing: Medical journals strongly speed up their publication process for COVID-19. Quant. Sci. Stud. 2020, 1, 1056–1067.
- Palayew, A.; Norgaard, O.; Safreed-Harmon, K.; Andersen, T.H.; Rasmussen, L.N.; Lazarus, J.V. Pandemic publishing poses a new COVID-19 challenge. Nat. Hum. Behav. 2020, 4, 666–669.
- Fatehi, F.; Wootton, R. Telemedicine, telehealth or e-health? A bibliometric analysis of the trends in the use of these terms. J. Telemed. Telecare 2012, 18, 460–464.





