1.1. Context and Background
The global population of older adults is projected to surpass 2.1 billion by 2050, accompanied by an increase in mental health challenges such as depression, anxiety, and cognitive decline
[1][2]. While smart home technologies (SHTs) have garnered attention for their potential in fall detection and chronic disease management, fewer studies explore their ability to detect and intervene in mental health issues at early stages
[3]. Addressing this gap, the present review synthesizes research on SHT usability and accessibility—factors critical to older adults’ sustained engagement—while focusing on mental health monitoring and interventions. Unlike prior reviews that emphasize physical health or general technology adoption, this work highlights mental and emotional well-being
[4][5][6]. By emphasizing user-centered design principles, this review aims to propose a roadmap for optimizing older adults’ mental health outcomes through SHTs.
1.2. Significance
Early detection of depression, anxiety, and cognitive decline through in-home monitoring can significantly reduce healthcare burdens and improve quality of life
[6]. Despite these benefits, widespread adoption of SHTs remains slow due to usability challenges, limited personalization, high costs, and privacy concerns
[3][7][8]. This review seeks to bridge the gap between the promise of SHTs and their practical implementation by identifying barriers, synthesizing user-driven solutions, and proposing strategies to better align these technologies with older adults’ mental health needs.
1.3. Smart Home Technologies (SHTs) as a Solution, and Adoption Barriers
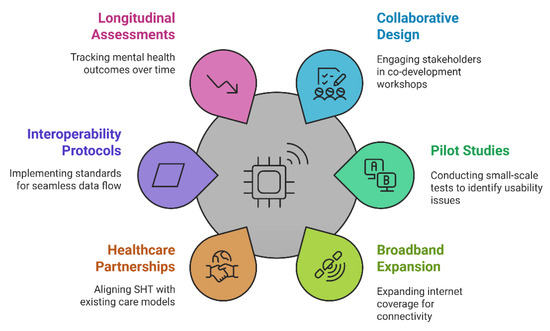
Smart home technologies (SHTs), as illustrated in
Figure 1, utilize interconnected devices, including motion sensors, ambient monitors, AI-driven analytics, and telehealth interfaces, to provide real-time support for older adults
[7][8]. Leveraging IoT architectures, these systems monitor daily tasks, track vital signs, and detect behavioral changes, such as reduced physical activity, which may signal mental health concerns like depression
[4][9]. However, adoption is hindered by usability challenges, including complex interfaces, small text sizes, and overwhelming data presentations, which discourage consistent use
[10]. Technology-related anxiety, such as fears of device malfunction or data breaches, further inhibits engagement, especially among less tech-savvy users
[3][11]. Accessibility barriers, including physical impairments (e.g., reduced motor skills, sensory deficits) and limited internet access in rural areas, exacerbate these challenges
[12][13][14]. Privacy concerns regarding continuous data collection raise issues of surveillance, autonomy, and data ownership
[15][16]. Distrust in “always-on” sensors, particularly when data usage policies lack transparency or when mental health monitoring carries stigma, compounds these concerns
[17]. Ethical considerations, such as ensuring user consent and agency, are critical in addressing these privacy issues. Economic constraints, including device costs, subscription fees, and home modifications, pose additional barriers, especially for older adults on fixed incomes
[18][19]. Despite these challenges, well-designed SHTs grounded in ethical principles—such as autonomy and beneficence—can reduce psychological stressors related to isolation and chronic conditions
[20]. Research underscores the potential of ambient-assisted living systems, AI-enabled reminders, and remote counseling to complement human support when usability, accessibility, and ethical concerns are addressed holistically
[21].
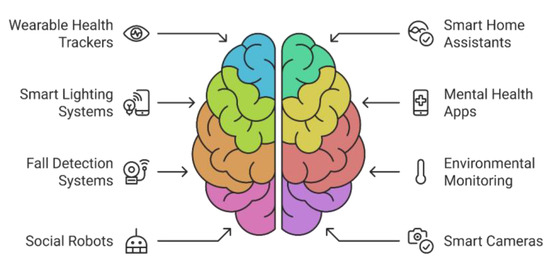
Figure 1. Enhancing mental health in seniors with technology.
1.4. Early Detection and Intervention Through SHTs: Features and Interventions
Smart home technologies (SHTs) offer robust solutions for mental health monitoring and support through integrated features and intervention methods. Behavioral monitoring systems enable continuous tracking of movement, sleep patterns, and daily routines, allowing for early detection of potential mental health challenges
[22][23]. Cognitive assessment tools evaluate memory recall and problem-solving capabilities through interactive tasks seamlessly integrated into daily living
[6][10][24]. Advanced AI-driven emotional analysis detects markers of psychological distress through vocal patterns, facial expressions, and text inputs, offering a stigma-free, home-based evaluation process
[25][26]. Intervention capabilities include automated medication management systems to maintain proper dosage schedules for mental health medications
[27][28], as well as crisis alert features that notify caregivers and healthcare providers during acute mental health events
[27][29][30]. Social engagement tools further combat isolation through video-calling platforms, online group activities, and virtual companionship features, fostering meaningful interactions
[22][31][32]. When implemented with careful attention to usability and accessibility, these technologies can proactively address mental health risks, reducing the impact of undetected depression, anxiety, and early-stage cognitive decline
[31][32].
1.5. Purpose and Scope
This narrative review evaluates the usability and accessibility of SHTs for older adults facing mental health challenges. It examines key barriers such as interface complexity, cognitive overload, and accessibility issues arising from physical impairments or economic constraints
[33][34]. By analyzing SHT features—such as behavioral monitoring, cognitive assessments, and AI-driven emotional analysis—and their potential for interventions like medication reminders and crisis alerts, this study proposes an integrative framework that combines technical innovation with user-centered design principles. The proposed framework addresses gaps such as limited personalization, siloed data streams, and ethical concerns, aiming to optimize SHTs for enhancing older adults’ well-being and independence
[25][30].
2. Materials and Methods
2.1. Research Design and Review Protocol
This study employs a narrative review design to explore the current literature on smart home technologies (SHTs) and their impact on older adults’ mental health. While not a systematic review, this approach allows for a thematic exploration of qualitative and quantitative findings across diverse contexts. To enhance transparency, we adhered to a checklist adapted from the PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) in our search and selection processes (see
Figure A1 in
Appendix A for the PRISMA-style flow chart).
In addition to peer-reviewed studies, key reports and guidelines from reputable organizations (e.g., WHO, ISO) were referenced to provide contextual insights. These resources were not included in systematic review tables or the PRISMA flow chart but are cited in the text and reference list for transparency.
2.2. Search Strategy
Comprehensive searches were conducted on PubMed, IEEE Xplore, and Google Scholar, covering the period from January 2010 to early 2024. The primary search terms included the following: “Smart Home Technology”, “Older Adults”, “Mental Health”, “Usability”, “Accessibility”, “Early Detection”, and “Intervention”. Boolean operators (AND/OR) were employed to combine these terms. The search was restricted to English-language studies to ensure the feasibility of quality assessment.
2.3. Inclusion and Exclusion Criteria
Inclusion: (1) Studies focusing on older adults (≥60 years) using or evaluating smart home systems; (2) articles that addressed mental health aspects (e.g., depression, anxiety, cognitive decline); (3) studies that explicitly discussed HCD principles like usability or accessibility; and (4) empirical or theoretical works published in peer-reviewed journals or as full conference papers.
Exclusion: (1) Studies centered exclusively on physical health metrics (e.g., fall detection) without mentioning mental health outcomes; (2) non-English studies; (3) abstract-only publications; and (4) pediatric or non-geriatric populations.
2.4. Screening and Selection Process
Two authors (M.M.F. and A.H.) independently screened titles and abstracts for relevance. Discrepancies were resolved through discussion or by consulting a third reviewer (A.M.G.). The initial search yielded 248 potentially relevant articles, of which 52 underwent full-text review. Ultimately, 27 studies met the inclusion criteria.
2.5. Quality Assessment
Each included study was subjected to a comprehensive quality assessment using the Mixed Methods Appraisal Tool (MMAT). This tool evaluates methodological rigor across qualitative, quantitative, and mixed-methods research designs. The MMAT-based appraisal results, including categorizations and overall quality ratings, are summarized in Table A1. Studies with low relevance or unclear methodologies were excluded or flagged for limited interpretability, ensuring robust review findings.
2.6. Data Extraction and Synthesis
Study details, including author(s), year of publication, study design (qualitative, quantitative, or mixed), population characteristics, interventions, and key findings related to SHT usability, accessibility, and mental health impact, were extracted. A thematic analysis was conducted to synthesize recurring barriers, facilitators, and proposed solutions.
This review also adapted a protocol developed by Lyon et al.
[20] o guide the development of a framework for smart home technologies. The protocol emphasizes human-centered design principles and iterative refinement through continuous user feedback, making it particularly relevant for addressing usability and accessibility barriers faced by older adults in mental health monitoring.
3. Results
3.1. Summary of Included Studies
Table A2 presents an overview of the 27 included studies, detailing their methodologies, participant characteristics, and key mental health-related outcomes. Among the studies, 15 employed quantitative designs, such as surveys or intervention trials; 7 utilized qualitative methods, including interviews or focus groups; and 5 adopted mixed-methods approaches that integrated qualitative and quantitative data (refer to
Appendix B for
Table A2).
3.2. Usability and Accessibility Challenges in SHTs
A total of 18 studies (67%) highlighted interface complexity as a chief barrier, noting that multi-step menus, small fonts, and cluttered displays induced cognitive overload
[10][12]. Twelve studies (44%) emphasized physical or sensory impairments—notably reduced vision and dexterity—as major obstacles to sustained system use
[13][14]. Additionally, five studies (19%) reported that technology anxiety and fear of data breaches deterred participants from fully engaging with SHTs
[3][15].
3.3. Economic and Infrastructure Barriers
Nine studies (33%) indicated that high device and subscription costs limited adoption among fixed-income older adults, particularly in rural areas where broadband coverage was unreliable
[18][19]. Three studies (11%) suggested that government subsidies or insurance reimbursement schemes could significantly boost SHT uptake, though current policies remain underdeveloped
[20].
3.4. Mental Health Monitoring and Early Interventions
Twelve studies (44%) reported that AI-driven monitoring—including voice analysis, behavioral tracking, and cognitive quizzes—enabled early detection of depressive symptoms or cognitive decline
[22][24]. Among these, four studies (15%) successfully integrated social engagement features, which reduced loneliness and provided timely alerts to caregivers
[31][32]. However, seven studies (26%) noted persistent data silo issues, preventing a holistic view of users’ mental well-being across different apps and devices
[13][31].
4. Discussion
This narrative review underscores the transformative potential of smart home technologies (SHTs) in supporting early detection and intervention of mental health challenges among older adults. By leveraging real-time monitoring of daily activities, mood fluctuations, and cognitive markers, SHTs can address critical gaps in traditional healthcare delivery, ultimately empowering older adults to age in place with dignity and autonomy
[22][24].
4.1. Comparison with Existing Literature
Our findings are consistent with prior research that identifies usability, accessibility, and privacy concerns as pivotal barriers to SHT adoption among older adults
[10][13]. While much of the existing literature predominantly addresses SHT applications for physical health metrics, such as fall detection or chronic disease management
[7][9], this review uniquely emphasizes the role of SHTs in mental health monitoring and interventions. The results highlight the significant potential of adaptive interfaces and culturally tailored designs in mitigating technology-related anxiety and enhancing user acceptance
[19][25]. These insights align with the growing evidence that participatory co-design and iterative feedback loops during development are crucial for ensuring technology acceptance and efficacy among older populations.
4.2. Analysis of Findings
The findings from this narrative review highlight the substantial potential of smart home technologies (SHTs) to enhance older adults’ mental health through early detection, continuous monitoring, and timely interventions
[22][24][30]. By integrating behavioral tracking, cognitive assessments, and social engagement features, SHTs address the critical challenges of isolation, cognitive decline, and emotional distress, which are common in aging populations
[7][9][31]. Despite these promising capabilities, the review also identifies persistent barriers—spanning usability, accessibility, privacy concerns, and economic and infrastructural challenges—which hinder the widespread adoption and consistent utilization of SHTs among older adults
[12][15].
Usability Challenges: Usability remains a significant obstacle to SHT adoption, with issues such as interface complexity, small fonts, and multi-step menus contributing to cognitive overload for users
[10][12]. Poor interoperability across devices exacerbates frustration, while cryptic error messages and constant updates contribute to technology anxiety and undermine user trust
[3][11][15]. To address these challenges, developers advocate for simplified interfaces with larger text, reduced menu complexity, and adaptive systems that respond to individual user needs. Participatory co-design approaches, involving older adults in the development process, have shown promise in enhancing usability and engagement
[10][13]. Additionally, standardized communication protocols, consistent design principles, intuitive troubleshooting tools, and transparent privacy policies can foster confidence and acceptance among users
[16][17][25].
Accessibility Barriers: Economic constraints, physical and sensory limitations, and cultural and linguistic diversity present additional barriers to SHT accessibility. High costs and limited funding options restrict access for many older adults, particularly in underserved or rural areas where infrastructure upgrades (e.g., reliable broadband connectivity) may also be required
[18][20]. Physical impairments, such as reduced vision, motor control, and hearing, make interactions with touchscreens or precise controls difficult, especially when adaptive features are inconsistently implemented
[12][13]. Cultural and linguistic barriers further hinder inclusivity, as many SHTs lack localized interfaces or multi-language support
[14]. Tailored solutions—such as culturally aligned designs, customizable features, and adaptive interfaces—can mitigate these challenges, ensuring that SHTs are more accessible and beneficial for diverse populations of older adults
[25].
Privacy and Ethical Concerns: Data privacy concerns represent a significant barrier, especially in the context of continuous monitoring for emotional or behavioral cues. Many older adults express distrust of “always-on” sensors, citing fears over data misuse, surveillance, and unclear ownership of personal information
[16][17]. Ethical concerns regarding autonomy and informed consent further complicate the adoption of SHTs, particularly when these technologies monitor sensitive mental health data. Transparent privacy policies, ethical frameworks prioritizing user agency, and secure data management systems are essential for addressing these anxieties and fostering user trust
[15][25].
Economic and Infrastructural Challenges: Economic disparities and infrastructural limitations, particularly in underserved regions, exacerbate SHT adoption barriers. High upfront costs, ongoing subscription fees, and necessary home modifications can strain fixed incomes, while inadequate broadband connectivity limits the functionality of internet-dependent features
[19][20]. Addressing these issues through government subsidies, insurance coverage, and targeted infrastructure investments could significantly enhance access and adoption rates
[20][21].
Holistically addressing these multifaceted barriers (
Figure 2) is essential for transitioning SHTs from experimental applications to robust, scalable solutions that can effectively support older adults’ mental health and well-being
[25][31].
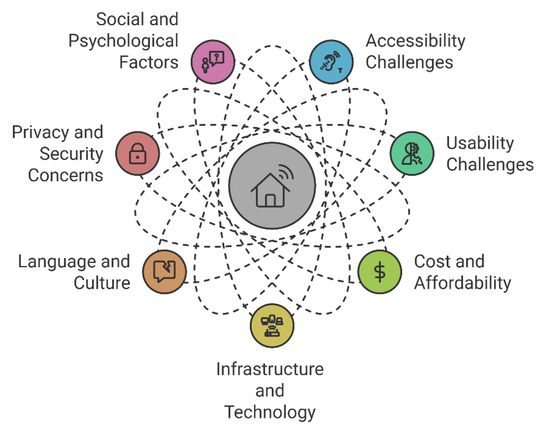
Figure 2. Comprehensive overview of SHT barriers for older adults.
4.3. Identified Gaps
Smart home technologies (SHTs) often prioritize physical health metrics like fall detection and mobility tracking, neglecting critical mental health indicators such as mood changes, social interaction, and cognitive performance
[4][7][9][21][22]. Even when included, mental health data are often secondary, limiting early detection of issues like depression or cognitive decline
[6][8]. A lack of personalization also hinders adoption. Standardized interfaces fail to accommodate diverse cognitive, sensory, and cultural needs, leading to frustration and abandonment
[12][18][25]. Co-design processes involving older adults remain inconsistent, preventing usability improvements and adaptation to user needs
[20][26][30]. Privacy concerns and fragmented data systems exacerbate these issues. Continuous monitoring raises fears about surveillance and misuse, while unclear data-sharing policies erode trust
[15][16][17]. Fragmented platforms further restrict holistic assessments, missing critical correlations, such as between sleep patterns and social engagement
[13][31]. Addressing these gaps requires balancing physical and mental health metrics, enhancing personalization through user-centered design, and ensuring robust privacy protections and data integration
[25][31].
4.4. Proposed Solutions: Design Strategies and Co-Creation
Addressing the identified barriers and gaps requires a multi-level strategy: Financial Assistance and Subsidies: Government- or insurer-provided incentives can offset device costs, particularly for low-income older adults
[19]. Infrastructure Improvements: Upgrading broadband coverage and user-friendly networking solutions help close the digital divide, especially in rural regions
[20]. Universal Design Principles: As recommended by recognized usability standards, developers should incorporate large text, multimodal feedback, and adaptive interfaces
[12][18]. Consistent design patterns across vendors also ease cognitive load, allowing skill transfer
[13]. Localization and Cultural Responsiveness: Multi-language support and culturally sensitive interface options can reduce mistrust and promote sustained engagement
[14]. Customizing terminology or alert functions to align with local norms may help older users feel more comfortable
[25].
These interventions (
Figure 3) can make SHTs more inclusive, accessible, and effective for older adults’ mental health needs, addressing both usability and accessibility gaps
[31].

Figure 3. Strategies for bridging gaps.
4.5. Conceptual Framework for Integrative Smart Home Solutions
This framework (Figure 4) integrates technical innovation (e.g., smart sensors, AI analytics) with human-centered design principles (e.g., usability, trust, personalization) to support early detection and intervention for older adults’ mental health challenges.
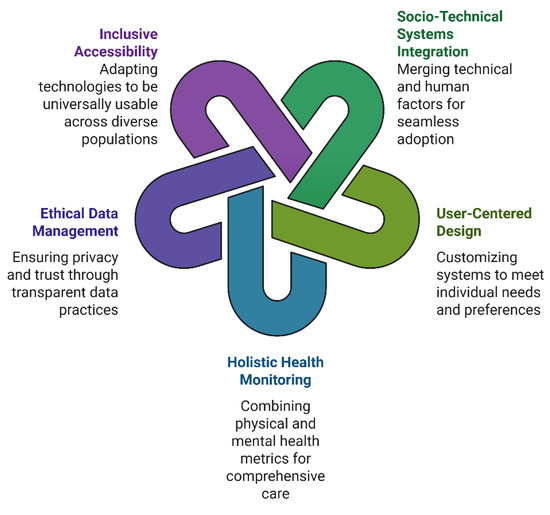
Figure 4. Integrating SHT design solutions for older adults.
4.5.1. Core Principles of the Framework
- ○
-
Integration of Socio-Technical Systems: effective adoption relies on merging technical capabilities with social, cultural, and behavioral factors, building trust through reliability and relevance
[12][15][16][17].
- ○
-
User-Centered Design and Personalization: co-design processes and iterative feedback enable systems to adapt to cognitive, physical, and linguistic needs, improving satisfaction and sustained use
[18][19][25][26].
- ○
-
Holistic Health Monitoring: equal emphasis on mental health (e.g., mood, cognitive performance) and physical metrics creates a comprehensive well-being profile, integrating behavioral, cognitive, and emotional sensing
[7][9][22][24][30][31].
- ○
-
Ethical Data Management and Transparency: clear communication of data practices, robust security measures (e.g., encryption), and customizable consent tools address privacy concerns and build trust
[14][15][16][17][19].
- ○
-
Inclusive Accessibility: universal design principles adapt to sensory and motor impairments, while cultural and linguistic responsiveness broadens usability across diverse populations
[12][13][14][25].
4.5.2. Framework Components and Dynamics
The proposed framework integrates four interacting components, as illustrated in Figure 5:
- ○
-
Adaptive User Interface Layer: 1. Personalized Layouts: large buttons, high-contrast visuals, voice/gesture input for users with varying dexterity or vision
[12][18]. 2. Cultural/Language Localization: multi-language support, culturally relevant prompts, and flexible navigation to accommodate diverse backgrounds
[14][25]. 3. Real-Time Feedback: simple, reassuring messages or icons confirming user actions, minimizing technology anxiety
[3][11].
- ○
-
Multimodal Sensing and Data Fusion: 1. Behavioral/Physiological Monitoring: sleep patterns, physical activity, and vital signs integrated with mental health indicators (mood, memory tasks)
[22][24]. 2. AI-Driven Analysis: emotional state inference via speech/text analysis or facial recognition, delivering discreet alerts for significant mental health risks
[25][30]. 3. Interoperability: standardized protocols that unify disparate sensors and systems, offering a holistic view of user well-being
[12][31].
- ○
-
Secure Cloud and Data Governance: 1. Privacy Safeguards: encryption, anonymization, and user-controlled permissions to mitigate surveillance fears and align with ethical guidelines
[15][16]. 2. Synchronized Platforms: a unified database ensures consistent updates across devices (smart speakers, tablets, wearables), avoiding siloed data
[13][31]. 3. Analytics for Caregivers/Providers: seamless sharing of relevant metrics with trusted parties, enabling timely intervention for mental health concerns
[29][32].
- ○
-
Support and Engagement Mechanisms: 1. Medication/Crisis Alerts: automated reminders and emergency notifications that incorporate both mental and physical health triggers
[27][30]. 2. Social Connectivity: in-home video conferencing, online communities, and interactive programs to reduce isolation
[31][32]. 3. Iterative Co-Design: continuous user feedback sessions to refine both interface and features, ensuring SHTs stay aligned with older adults’ evolving needs
[20][26].
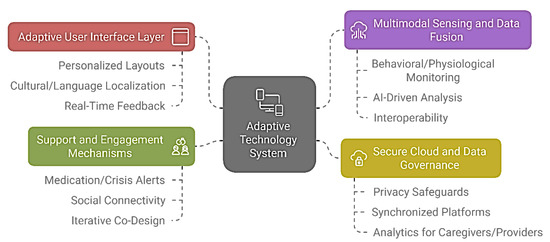
Figure 5. Adaptive SHT system for older adults.
These components function within a dynamic feedback loop (Figure 6a) that collects user data, applies AI-driven analysis, adjusts system settings, and delivers insights to users, caregivers, or healthcare professionals. Iterative co-design further enhances system usability and effectiveness (Figure 6b) [25][30].
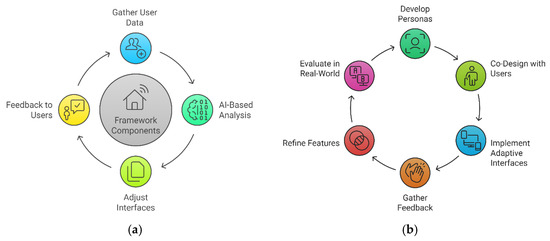 Figure 6. (a) Dynamic feedback loop for mental health support. (b) Iterative design process of SHT for older adults.
Figure 6. (a) Dynamic feedback loop for mental health support. (b) Iterative design process of SHT for older adults.
4.5.3. Implementation Pathway
The successful operation of this integrative framework relies on three sequential phases:
-
Phase 1: Collaborative Design and Piloting: 1. Involve older adults, caregivers, designers, and healthcare providers in co-development workshops to ensure the system reflects user needs and expectations
[26][29]. 2. Conduct small-scale pilot studies to identify usability pain points and refine the system before wide deployment
[20][30].
-
Phase 2: Scalable Deployment and Infrastructure Integration: 1. Expand broadband coverage and ensure robust connectivity to support real-time data exchange
[20]. 2. Collaborate with healthcare institutions and insurers to integrate SHT solutions into existing care models, allowing for potential subsidies or insurance reimbursement
[19][21]. 3. Implement standardized interoperability protocols, facilitating seamless data flow and reducing user confusion
[12][13].
-
Phase 3: Continuous Evaluation and Policy Support: 1. Establish longitudinal assessment of mental health outcomes, tracking indicators like depression severity, anxiety episodes, and cognitive functioning
[31][32]. 2. Develop policy frameworks and ethical guidelines mandating transparent data usage, anonymization protocols, and user consent mechanisms
[15][16]. 3. Encourage iterative updates through user feedback, refining the SHT ecosystem to maintain relevance as older adults’ capabilities and preferences evolve
[26][30].
By following this implementation pathway (
Figure 7), smart home systems can transition from fragmented technologies to cohesive, user-centered platforms that actively enhance older adults’ mental health. This strategy directly addresses the barriers identified in earlier sections, including over-reliance on physical health metrics, lack of personalization, privacy concerns, and data silos. Ultimately, it optimizes SHTs for the complex realities of aging in place
[14][25][31].
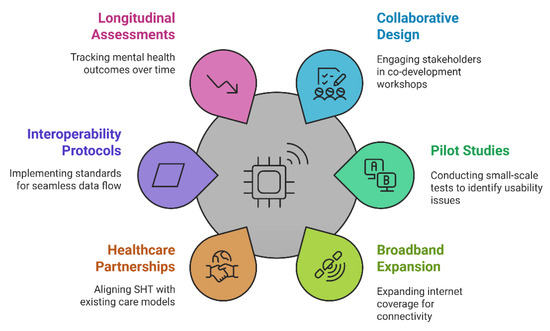
Figure 7. SHT integration implementation path for older adults.
4.6. Opportunities for Collaboration
The development and deployment of smart home technologies (SHTs) require a multi-stakeholder collaborative approach to address their inherent complexities. Designers and engineers can drive advancements in usability and privacy through co-design workshops, user testing, and iterative refinements
[12][26]. Healthcare professionals play a critical role in ensuring that mental health tools are clinically relevant and responsibly integrated into existing care systems
[22][27]. Policymakers and insurers can facilitate broader adoption by creating supportive infrastructure, such as subsidies and reimbursement models for validated interventions
[19][21]. Engaging older adults and caregivers as active participants ensures the development of user-centered designs that foster trust, usability, and sustained engagement
[25][30]. Collaborative efforts can also establish interoperability standards, conduct scalable pilot studies, and promote evidence-based policies
[12][31]. Such partnerships enhance the practicality, accessibility, and impact of SHTs, paving the way for meaningful mental health improvements and widespread adoption among aging populations
[20][25].
4.7. Limitations
This review has several limitations. First, restricting the analysis to English-language studies may have excluded relevant findings published in other languages. Second, the use of a narrative review design, rather than a strict systematic approach, limits the ability to conduct quantitative syntheses such as meta-analyses. Third, while the quality assessment utilized the Mixed Methods Appraisal Tool (MMAT), the evaluation was primarily descriptive due to the heterogeneity of included study designs. Finally, this review did not delve deeply into cost-effectiveness data, which is an important area for future exploration.
4.8. Future Research Directions
Although SHTs hold immense promise, critical research gaps persist. Longitudinal studies are essential for evaluating the long-term effectiveness, user retention, and potential unintended consequences of SHTs, such as over-reliance on technology or privacy fatigue
[30][32]. These studies would clarify whether the early benefits of SHT interventions endure or evolve over time
[22][24].
Advancements in AI integration and personalization remain a priority. AI-driven systems must be refined to address cultural nuances, language variations, and ethical considerations
[14][15]. Real-time system adaptations to changes in user stress levels or motor abilities require further exploration, supported by co-design research. Collaboration between AI experts and mental health professionals could enable predictive models that anticipate crises before they escalate
[25][31].
Policy and ethical frameworks are also crucial for promoting widespread SHT adoption. Regulatory guidelines, insurance reimbursement structures, and international standards must be developed to support equitable access to SHTs
[19][21]. Lessons from telehealth adoption can inform the creation of transparent data-handling protocols and user consent models that promote trust and equity
[15][31]. Addressing these challenges through interdisciplinary efforts will ensure that SHTs not only enable aging in place but also foster mental and emotional well-being among diverse older populations
[20][30].
5. Conclusions
Smart home technologies (SHTs) hold significant promise for supporting older adults by enabling early detection and intervention for mental health challenges. This review highlights the importance of prioritizing usability, accessibility, and user-driven co-design to ensure successful adoption. Personalized interfaces, robust privacy protections, and collaborative efforts among policymakers, developers, and healthcare providers are essential for making these technologies inclusive, affordable, and ethically governed. By addressing these priorities, SHTs can enhance autonomy, reduce social isolation, and improve the overall well-being of aging populations.

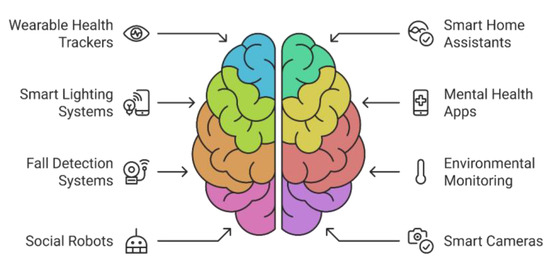
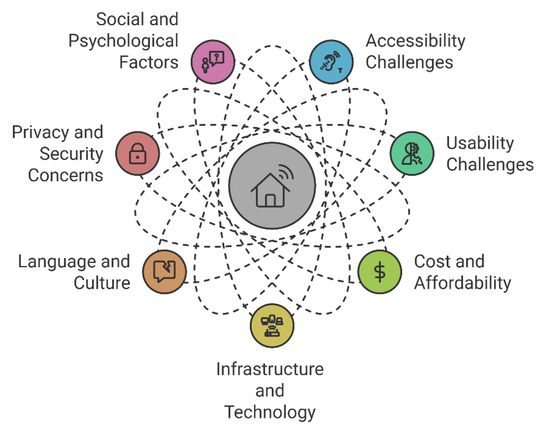

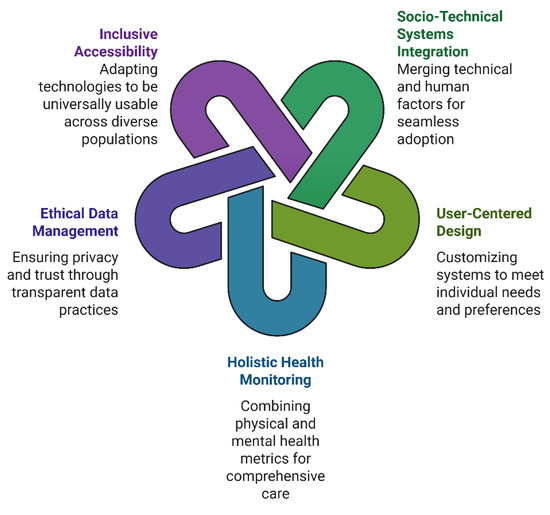
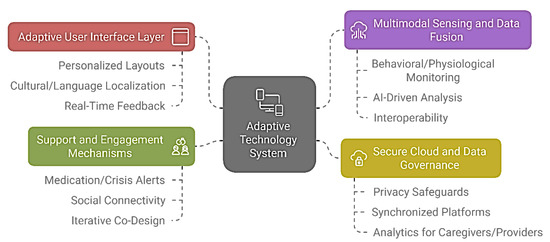
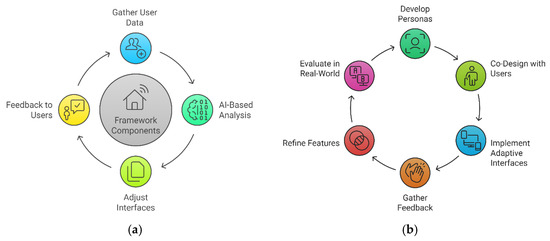 Figure 6. (a) Dynamic feedback loop for mental health support. (b) Iterative design process of SHT for older adults.
Figure 6. (a) Dynamic feedback loop for mental health support. (b) Iterative design process of SHT for older adults.