
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | 雪 王 | -- | 2532 | 2024-03-18 07:33:34 | | | |
| 2 | Sirius Huang | Meta information modification | 2532 | 2024-03-18 07:45:06 | | |
Video Upload Options
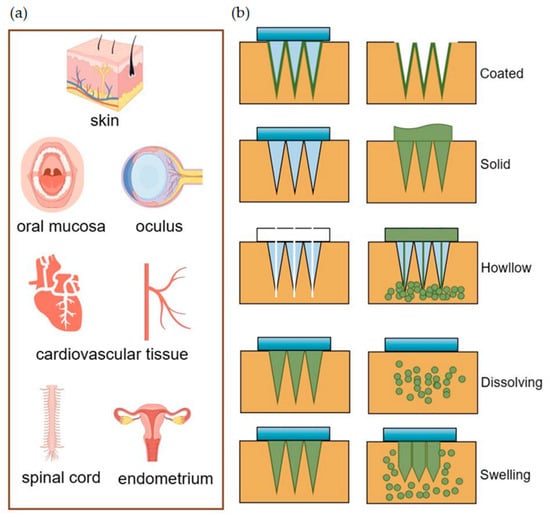
Microneedles (MNs), renowned for their painless and minimally invasive qualities, exhibit significant potential for facilitating effective drug delivery, vaccination, and targeted sample extraction. Extracellular vesicles (EVs), serving as cargo for MNs, are naturally occurring nanovesicles secreted by cells and characterized by novel biomarkers, low immunogenicity, and cell-source-specific traits. MNs prove instrumental in extracting EVs from the sample fluid, thereby facilitating a promising diagnostic and prognostic tool. To harness the therapeutic potential of EVs in tissue repair, MNs with sustained delivery of EVs leverage micron-sized channels to enhance targeted site concentration, demonstrating efficacy in treating various diseases, such as Achillea tendinopathy, hair loss, spinal cord injury, and diabetic ulcers. EV-loaded MNs emerge as a promising platform for repair applications of skin, cardiac, tendon, hair, and spinal cord tissues.
1. Introduction
2. Types and Materials of Microneedles
3. Loaded Cargos of Microneedles
References
- Akhtar, N. Microneedles: An Innovative Approach to Transdermal Delivery—A Review. Int. J. Pharm. Pharm. Sci. 2014, 6, 18–25.
- Larrañeta, E.; Lutton, R.E.M.; Woolfson, A.D.; Donnelly, R.F. Microneedle Arrays as Transdermal and Intradermal Drug Delivery Systems: Materials Science, Manufacture and Commercial Development. Mater. Sci. Eng. R Rep. 2016, 104, 1–32.
- Waghule, T.; Singhvi, G.; Dubey, S.K.; Pandey, M.M.; Gupta, G.; Singh, M.; Dua, K. Microneedles: A Smart Approach and Increasing Potential for Transdermal Drug Delivery System. Biomed. Pharmacother. 2019, 109, 1249–1258.
- Abdullah, H.; Phairatana, T.; Jeerapan, I. Tackling the Challenges of Developing Microneedle-Based Electrochemical Sensors. Mikrochim. Acta 2022, 189, 440.
- Nguyen, T.T.; Nguyen, T.T.D.; Tran, N.-M.-A.; Vo, G.V. Advances of Microneedles in Hormone Delivery. Biomed. Pharmacother. 2022, 145, 112393.
- Donnelly, R.F.; Singh, T.R.R.; Woolfson, A.D. Microneedle-Based Drug Delivery Systems: Microfabrication, Drug Delivery, and Safety. Drug Deliv. 2010, 17, 187–207.
- Creighton, R.L.; Woodrow, K.A. Microneedle-Mediated Vaccine Delivery to the Oral Mucosa. Adv. Healthc. Mater. 2019, 8, 1801180.
- Than, A.; Liu, C.; Chang, H.; Duong, P.K.; Cheung, C.M.G.; Xu, C.; Wang, X.; Chen, P. Self-Implantable Double-Layered Micro-Drug-Reservoirs for Efficient and Controlled Ocular Drug Delivery. Nat. Commun. 2018, 9, 4433.
- Shi, H.; Zhou, J.; Wang, Y.; Zhu, Y.; Lin, D.; Lei, L.; Vakal, S.; Wang, J.; Li, X. A Rapid Corneal Healing Microneedle for Efficient Ocular Drug Delivery. Small 2022, 18, 2104657.
- Huang, L.; Fang, H.; Zhang, T.; Hu, B.; Liu, S.; Lv, F.; Zeng, Z.; Liu, H.; Zhou, W.; Wang, X. Drug-Loaded Balloon with Built-in NIR Controlled Tip-Separable Microneedles for Long-Effective Arteriosclerosis Treatment. Bioact. Mater. 2023, 23, 526–538.
- Chen, H.; Fan, L.; Peng, N.; Yin, Y.; Mu, D.; Wang, J.; Meng, R.; Xie, J. Galunisertib-Loaded Gelatin Methacryloyl Hydrogel Microneedle Patch for Cardiac Repair after Myocardial Infarction. ACS Appl. Mater. Interfaces 2022, 14, 40491.
- Lyu, S.; Dong, Z.; Xu, X.; Bei, H.-P.; Yuen, H.-Y.; James Cheung, C.-W.; Wong, M.-S.; He, Y.; Zhao, X. Going below and beyond the Surface: Microneedle Structure, Materials, Drugs, Fabrication, and Applications for Wound Healing and Tissue Regeneration. Bioact. Mater. 2023, 27, 303–326.
- Han, M.; Yang, H.; Lu, X.; Li, Y.; Liu, Z.; Li, F.; Shang, Z.; Wang, X.; Li, X.; Li, J.; et al. Three-Dimensional-Cultured MSC-Derived Exosome-Hydrogel Hybrid Microneedle Array Patch for Spinal Cord Repair. Nano Lett. 2022, 22, 6391–6401.
- Shi, Y.; Zhao, J.; Li, H.; Yu, M.; Zhang, W.; Qin, D.; Qiu, K.; Chen, X.; Kong, M. A Drug-Free, Hair Follicle Cycling Regulatable, Separable, Antibacterial Microneedle Patch for Hair Regeneration Therapy. Adv. Healthc. Mater. 2022, 11, e2200908.
- Zhu, Y.; Li, S.; Li, Y.; Tan, H.; Zhao, Y.; Sun, L. Antioxidant Nanozyme Microneedles with Stem Cell Loading for in Situ Endometrial Repair. Chem. Eng. J. 2022, 449, 137786.
- Donnelly, R.F.; Mooney, K.; Caffarel-Salvador, E.; Torrisi, B.M.; Eltayib, E.; McElnay, J.C. Microneedle-mediated minimally invasive patient monitoring. Ther. Drug Monit. 2014, 36, 10–17.
- Huang, X.; Zheng, S.; Liang, B.; He, M.; Wu, F.; Yang, J.; Chen, H.-J.; Xie, X. 3D-Assembled Microneedle Ion Sensor-Based Wearable System for the Transdermal Monitoring of Physiological Ion Fluctuations. Microsyst. Nanoeng. 2023, 9, 25.
- Keyvani, F.; Zheng, H.; Kaysir, M.R.; Mantaila, D.F.; Ghavami Nejad, P.; Rahman, F.A.; Quadrilatero, J.; Ban, D.; Poudineh, M. A Hydrogel Microneedle Assay Combined with Nucleic Acid Probes for On-Site Detection of Small Molecules and Proteins. Angew. Chem. Int. Ed. Engl. 2023, 62, e202301624.
- Khalid, R.; Mahmood, S.; Mohamed Sofian, Z.; Hilles, A.R.; Hashim, N.M.; Ge, Y. Microneedles and Their Application in Transdermal Delivery of Antihypertensive Drugs—A Review. Pharmaceutics 2023, 15, 2029.
- Wang, Y.; Lu, H.; Guo, M.; Chu, J.; Gao, B.; He, B. Personalized and Programmable Microneedle Dressing for Promoting Wound Healing. Adv. Healthc. Mater. 2022, 11, 2101659.
- Zhang, Y.; Wang, S.; Yang, Y.; Zhao, S.; You, J.; Wang, J.; Cai, J.; Wang, H.; Wang, J.; Zhang, W.; et al. Scarless Wound Healing Programmed by Core-Shell Microneedles. Nat. Commun. 2023, 14, 3431.
- Whitford, W.; Guterstam, P. Exosome Manufacturing Status. Future Med. Chem. 2019, 11, 1225–1236.
- Rilla, K.; Mustonen, A.-M.; Arasu, U.T.; Härkönen, K.; Matilainen, J.; Nieminen, P. Extracellular Vesicles Are Integral and Functional Components of the Extracellular Matrix. Matrix Biol. 2019, 75–76, 201–219.
- Su, G.; Zhang, D.; Li, T.; Pei, T.; Yang, J.; Tu, S.; Liu, S.; Ren, J.; Zhang, Y.; Duan, M.; et al. Annexin A5 Derived from Matrix Vesicles Protects against Osteoporotic Bone Loss via Mineralization. Bone Res. 2023, 11, 60.
- Colombo, M.; Raposo, G.; Théry, C. Biogenesis, Secretion, and Intercellular Interactions of Exosomes and Other Extracellular Vesicles. Annu. Rev. Cell Dev. Biol. 2014, 30, 255–289.
- Driedonks, T.; Jiang, L.; Carlson, B.; Han, Z.; Liu, G.; Queen, S.E.; Shirk, E.N.; Gololobova, O.; Liao, Z.; Nyberg, L.H.; et al. Pharmacokinetics and Biodistribution of Extracellular Vesicles Administered Intravenously and Intranasally to Macaca Nemestrina. J. Extracell. Biol. 2022, 1, e59.
- Lim, D.-J.; Kim, H.-J. Microneedles in Action: Microneedling and Microneedles-Assisted Transdermal Delivery. Polymers 2022, 14, 1608.
- Subra, C.; Grand, D.; Laulagnier, K.; Stella, A.; Lambeau, G.; Paillasse, M.; De Medina, P.; Monsarrat, B.; Perret, B.; Silvente-Poirot, S.; et al. Exosomes Account for Vesicle-Mediated Transcellular Transport of Activatable Phospholipases and Prostaglandins. J. Lipid Res. 2010, 51, 2105–2120.
- Zhang, F.; Guo, J.; Zhang, Z.; Duan, M.; Wang, G.; Qian, Y.; Zhao, H.; Yang, Z.; Jiang, X. Application of engineered extracellular vesicles for targeted tumor therapy. J. Biomed. Sci. 2022, 29, 14.
- Yang, C.; Xue, Y.; Duan, Y.; Mao, C.; Wan, M. Extracellular Vesicles and Their Engineering Strategies, Delivery Systems, and Biomedical Applications. J. Control. Release Off. J. Control. Release Soc. 2024, 365, 1089–1112.
- Fathi-Karkan, S.; Heidarzadeh, M.; Narmi, M.T.; Mardi, N.; Amini, H.; Saghati, S.; Abrbekoh, F.N.; Saghebasl, S.; Rahbarghazi, R.; Khoshfetrat, A.B. Exosome-Loaded Microneedle Patches: Promising Factor Delivery Route. Int. J. Biol. Macromol. 2023, 243, 125232.
- Cao, Z.; Jin, S.; Wang, P.; He, Q.; Yang, Y.; Gao, Z.; Wang, X. Microneedle Based Adipose Derived Stem Cells-derived Extracellular Vesicles Therapy Ameliorates UV-induced Photoaging in SKH-1 Mice. J. Biomed. Mater. Res. 2021, 109, 1849–1857.
- Yuan, M.; Liu, K.; Jiang, T.; Li, S.; Chen, J.; Wu, Z.; Li, W.; Tan, R.; Wei, W.; Yang, X.; et al. GelMA/PEGDA microneedles patch loaded with HUVECs-derived exosomes and Tazarotene promote diabetic wound healing. J. Nanobiotechnology 2022, 20, 147.
- You, Y.; Tian, Y.; Yang, Z.; Shi, J.; Kwak, K.J.; Tong, Y.; Estania, A.P.; Cao, J.; Hsu, W.-H.; Liu, Y.; et al. Intradermally Delivered mRNA-Encapsulating Extracellular Vesicles for Collagen-Replacement Therapy. Nat. Biomed. Eng. 2023, 7, 887–900.
- Park, W.; Maeng, S.-W.; Mok, J.W.; Choi, M.; Cha, H.J.; Joo, C.-K.; Hahn, S.K. Hydrogel Microneedles Extracting Exosomes for Early Detection of Colorectal Cancer. Biomacromolecules 2023, 24, 1445–1452.
- Cao, Y.; Xu, Y.; Chen, C.; Xie, H.; Lu, H.; Hu, J. Local Delivery of USC-Derived Exosomes Harboring ANGPTL3 Enhances Spinal Cord Functional Recovery after Injury by Promoting Angiogenesis. Stem Cell Res. Ther. 2021, 12, 20.
- Taylor, R.M.; Miller, P.R.; Ebrahimi, P.; Polsky, R.; Baca, J.T. Minimally-Invasive, Microneedle-Array Extraction of Interstitial Fluid for Comprehensive Biomedical Applications: Transcriptomics, Proteomics, Metabolomics, Exosome Research, and Biomarker Identification. Lab. Anim. 2018, 52, 526–530.
- Esposito, S.; Ascione, T.; Pagliano, P. Management of Bacterial Skin and Skin Structure Infections with Polymicrobial Etiology. Expert Rev. Anti-Infect. Ther. 2019, 17, 17–25.
- Savin, J.A.; Noble, W.C. Immunosuppression and Skin Infection. Br. J. Dermatol. 1975, 93, 115–120.
- Russell, L.M.; Wiedersberg, S.; Delgado-Charro, M.B. The Determination of Stratum Corneum Thickness: An Alternative Approach. Eur. J. Pharm. Biopharm. 2008, 69, 861–870.
- Jiang, X.; Zhao, H.; Li, W. Microneedle-Mediated Transdermal Delivery of Drug-Carrying Nanoparticles. Front. Bioeng. Biotechnol. 2022, 10, 840395.
- Gill, H.S.; Denson, D.D.; Burris, B.A.; Prausnitz, M.R. Effect of Microneedle Design on Pain in Human Volunteers. Clin. J. Pain 2008, 24, 585.
- Miller, P.R.; Taylor, R.M.; Tran, B.Q.; Boyd, G.; Glaros, T.; Chavez, V.H.; Krishnakumar, R.; Sinha, A.; Poorey, K.; Williams, K.P.; et al. Extraction and Biomolecular Analysis of Dermal Interstitial Fluid Collected with Hollow Microneedles. Commun. Biol. 2018, 1, 173.
- Narayan, R.J. Transdermal delivery of insulin via microneedles. J. Biomed. Nanotechnol. 2014, 10, 2244–2260.
- Bariya, S.H.; Gohel, M.C.; Mehta, T.A.; Sharma, O.P. Microneedles: An Emerging Transdermal Drug Delivery System. J. Pharm. Pharmacol. 2012, 64, 11–29.
- Jeong, H.R.; Lee, H.S.; Choi, I.J.; Park, J.H. Considerations in the Use of Microneedles: Pain, Convenience, Anxiety and Safety. J. Drug Target. 2017, 25, 29–40.
- Ni, M.; Li, W.; Yuan, B.; Zou, S.; Cheng, W.; Yang, K.; Su, J.; Sun, B.; Su, X. Micro-Structured P-N Junction Surfaces: Large-Scale Preparation, Antifouling Properties, and a Synergistic Antibacterial Mechanism. J. Mater. Chem. B 2023, 11, 1312–1319.
- Mohandas, A.; Deepthi, S.; Biswas, R.; Jayakumar, R. Chitosan Based Metallic Nanocomposite Scaffolds as Antimicrobial Wound Dressings. Bioact. Mater. 2018, 3, 267–277.
- Ni, M.; Jiang, C.; Cheng, W.; Yang, K.; Dai, L.; Zeng, Y.; Su, J.; Lu, Z.; Zou, S.; Su, X. A Solid Strategy to Realize Efficient Antibacterial Activity on the Shade Surface of Bulk Silicon under Natural or Indoor Lighting. Chem. Eng. J. 2024, 479, 147734.
- Erdem, Ö.; Eş, I.; Akceoglu, G.A.; Saylan, Y.; Inci, F. Recent Advances in Microneedle-Based Sensors for Sampling, Diagnosis and Monitoring of Chronic Diseases. Biosensors 2021, 11, 296.
- Zhang, B.L.; Yang, Y.; Zhao, Z.Q.; Guo, X.D. A gold nanoparticles deposited polymer microneedle enzymatic biosensor for glucose sensing. Electrochim. Acta 2020, 358, 136917.
- Molinero-Fernández, Á.; Casanova, A.; Wang, Q.; Cuartero, M.; Crespo, G.A. In Vivo Transdermal Multi-Ion Monitoring with a Potentiometric Microneedle-Based Sensor Patch. ACS Sens. 2023, 8, 158–166.
- Dervisevic, M.; Dervisevic, E.; Esser, L.; Easton, C.D.; Cadarso, V.J.; Voelcker, N.H. Wearable Microneedle Array-Based Sensor for Transdermal Monitoring of pH Levels in Interstitial Fluid. Biosens. Bioelectron. 2023, 222, 114955.
- Dervisevic, M.; Alba, M.; Adams, T.E.; Prieto-Simon, B.; Voelcker, N.H. Electrochemical Immunosensor for Breast Cancer Biomarker Detection Using High-Density Silicon Microneedle Array. Biosens. Bioelectron. 2021, 192, 113496.
- Chen, L.; Zhang, C.; Xiao, J.; You, J.; Zhang, W.; Liu, Y.; Xu, L.; Liu, A.; Xin, H.; Wang, X. Local Extraction and Detection of Early Stage Breast Cancers through a Microneedle and Nano-Ag/MBL Film Based Painless and Blood-Free Strategy. Mater. Sci. Eng. C 2020, 109, 110402.
- Tran, B.Q.; Miller, P.R.; Taylor, R.M.; Boyd, G.; Mach, P.M.; Rosenzweig, C.N.; Baca, J.T.; Polsky, R.; Glaros, T. Proteomic Characterization of Dermal Interstitial Fluid Extracted Using a Novel Microneedle-Assisted Technique. J. Proteome Res. 2018, 17, 479–485.
- Ita, K. Transdermal Delivery of Drugs with Microneedles: Strategies and Outcomes. J. Drug Deliv. Sci. Technol. 2015, 29, 16–23.
- Gupta, J.; Gill, H.S.; Andrews, S.N.; Prausnitz, M.R. Kinetics of Skin Resealing after Insertion of Microneedles in Human Subjects. J. Control Release 2011, 154, 148–155.
- Yang, J.; Liu, X.; Fu, Y.; Song, Y. Recent Advances of Microneedles for Biomedical Applications: Drug Delivery and Beyond. Acta Pharm. Sin. B 2019, 9, 469–483.
- Gill, H.S.; Prausnitz, M.R. Coating Formulations for Microneedles. Pharm. Res. 2007, 24, 1369–1380.
- Gidlöf, Z. Coating of Bioceramic Microneedles. 2017. Available online: https://www.diva-portal.org/smash/get/diva2:1091657/FULLTEXT01.pdf (accessed on 15 February 2024).
- Camović, M.; Biščević, A.; Brčić, I.; Borčak, K.; Bušatlić, S.; Ćenanović, N.; Dedović, A.; Mulalić, A.; Osmanlić, M.; Sirbubalo, M.; et al. Coated 3D Printed PLA Microneedles as Transdermal Drug Delivery Systems. In Proceedings of the CMBEBIH 2019, Banja Luka, Bosnia and Herzegovina, 16–18 May 2019; Springer International Publishing: Cham, Switzerland, 2020; Volume 73, pp. 735–742.
- Tarbox, T.N.; Watts, A.B.; Cui, Z.; Williams, R.O., III. An update on coating/manufacturing techniques of microneedles. Drug Deliv. Transl. Res. 2018, 8, 1828–1843.
- Khare, N.; Shende, P. Microneedle System: A Modulated Approach for Penetration Enhancement. Drug Dev. Ind. Pharm. 2021, 47, 1183–1192.
- Van Der Maaden, K.; Jiskoot, W.; Bouwstra, J. Microneedle Technologies for (Trans)Dermal Drug and Vaccine Delivery. J. Control. Release 2012, 161, 645–655.
- Wang, T.; Gao, H.; Wang, D.; Zhang, C.; Hu, K.; Zhang, H.; Lin, J.; Chen, X. Stem cell-derived exosomes in the treatment of melasma and its percutaneous penetration. Lasers Surg. Med. 2023, 55, 178–189.
- Badnikar, K.; Jayadevi, S.N.; Pahal, S.; Vemula, P.K.; Nayak, M.M.; Subramanyam, D.N. Microscale Engineering of Hollow Microneedle Tips: Design, Manufacturing, Optimization and Validation. Drug Deliv. Transl. Res. 2022, 12, 350–367.
- Wang, P.M.; Cornwell, M.; Hill, J.; Prausnitz, M.R. Precise Microinjection into Skin Using Hollow Microneedles. J. Investig. Dermatol. 2006, 126, 1080–1087.
- Aghabegi Moghanjoughi, A.; Khoshnevis, D.; Zarrabi, A. A Concise Review on Smart Polymers for Controlled Drug Release. Drug Deliv. Transl. Res. 2016, 6, 333–340.
- Han, D.; Morde, R.S.; Mariani, S.; La Mattina, A.A.; Vignali, E.; Yang, C.; Barillaro, G.; Lee, H. 4D Printing of a Bioinspired Microneedle Array with Backward-Facing Barbs for Enhanced Tissue Adhesion. Adv. Funct. Mater. 2020, 30, 1909197.
- El-Husseiny, H.M.; Mady, E.A.; Hamabe, L.; Abugomaa, A.; Shimada, K.; Yoshida, T.; Tanaka, T.; Yokoi, A.; Elbadawy, M.; Tanaka, R. Smart/Stimuli-Responsive Hydrogels: Cutting-Edge Platforms for Tissue Engineering and Other Biomedical Applications. Mater. Today Bio 2022, 13, 100186.
- Chai, Q.; Jiao, Y.; Yu, X. Hydrogels for Biomedical Applications: Their Characteristics and the Mechanisms behind Them. Gels 2017, 3, 6.
- Cheng, W.; Wang, X.; Zou, S.; Ni, M.; Lu, Z.; Dai, L.; Su, J.; Yang, K.; Su, X. Fabrication of Black Silicon Microneedle Arrays for High Drug Loading. JFB 2023, 14, 245.
- Hartmann, X.H.M.; van der Linde, P.; Homburg, E.F.G.A.; van Breemen, L.C.A.; de Jong, A.M.; Luttge, R. Insertion Process of Ceramic Nanoporous Microneedles by Means of a Novel Mechanical Applicator Design. Pharmaceutics 2015, 7, 503–522.
- Lin, Z.; Li, Y.; Meng, G.; Hu, X.; Zeng, Z.; Zhao, B.; Lin, N.; Liu, X.Y. Reinforcement of Silk Microneedle Patches for Accurate Transdermal Delivery. Biomacromolecules 2021, 22, 5319–5326.
- Shriky, B.; Babenko, M.; Whiteside, B.R. Dissolving and Swelling Hydrogel-Based Microneedles: An Overview of Their Materials, Fabrication, Characterization Methods, and Challenges. Gels 2023, 9, 806.
- Aldawood, F.K.; Andar, A.; Desai, S. A Comprehensive Review of Microneedles: Types, Materials, Processes, Characterizations and Applications. Polymers 2021, 13, 2815.
- Ahmed Saeed AL-Japairai, K.; Mahmood, S.; Hamed Almurisi, S.; Reddy Venugopal, J.; Rebhi Hilles, A.; Azmana, M.; Raman, S. Current Trends in Polymer Microneedle for Transdermal Drug Delivery. Int. J. Pharm. 2020, 587, 119673.
- Luo, Z.; Sun, W.; Fang, J.; Lee, K.; Li, S.; Gu, Z.; Dokmeci, M.R.; Khademhosseini, A. Biodegradable Gelatin Methacryloyl Microneedles for Transdermal Drug Delivery. Adv. Healthc. Mater. 2019, 8, 1801054.
- Rouphael, N.G.; Paine, M.; Mosley, R.; Henry, S.; McAllister, D.V.; Kalluri, H.; Pewin, W.; Frew, P.M.; Yu, T.; Thornburg, N.J.; et al. The Safety, Immunogenicity, and Acceptability of Inactivated Influenza Vaccine Delivered by Microneedle Patch (TIV-MNP 2015): A Randomised, Partly Blinded, Placebo-Controlled, Phase 1 Trial. Lancet 2017, 390, 649–658.
- Ito, Y.; Hagiwara, E.; Saeki, A.; Sugioka, N.; Takada, K. Feasibility of Microneedles for Percutaneous Absorption of Insulin. Eur. J. Pharm. Sci. 2006, 29, 82–88.
- Hong, X.; Wei, L.; Wu, F.; Wu, Z.; Chen, L.; Liu, Z.; Yuan, W. Dissolving and Biodegradable Microneedle Technologies for Transdermal Sustained Delivery of Drug and Vaccine. Drug Des. Dev. Ther. 2013, 945, 945–952.
- Ono, A.; Azukizawa, H.; Ito, S.; Nakamura, Y.; Asada, H.; Quan, Y.-S.; Kamiyama, F.; Katayama, I.; Hirobe, S.; Okada, N. Development of Novel Double-Decker Microneedle Patches for Transcutaneous Vaccine Delivery. Int. J. Pharm. 2017, 532, 374–383.
- Younas, A.; Dong, Z.; Hou, Z.; Asad, M.; Li, M.; Zhang, N. A Chitosan/Fucoidan Nanoparticle-Loaded Pullulan Microneedle Patch for Differential Drug Release to Promote Wound Healing. Carbohydr. Polym. 2023, 306, 120593.
- Chen, M.-C.; Lai, K.-Y.; Ling, M.-H.; Lin, C.-W. Enhancing Immunogenicity of Antigens through Sustained Intradermal Delivery Using Chitosan Microneedles with a Patch-Dissolvable Design. Acta Biomater. 2018, 65, 66–75.
- González-Vázquez, P.; Larrañeta, E.; McCrudden, M.T.C.; Jarrahian, C.; Rein-Weston, A.; Quintanar-Solares, M.; Zehrung, D.; McCarthy, H.; Courtenay, A.J.; Donnelly, R.F. Transdermal Delivery of Gentamicin Using Dissolving Microneedle Arrays for Potential Treatment of Neonatal Sepsis. J. Control Release 2017, 265, 30–40.
- Zhang, X.; Hasani-Sadrabadi, M.M.; Zarubova, J.; Dashtimighadam, E.; Haghniaz, R.; Khademhosseini, A.; Butte, M.J.; Moshaverinia, A.; Aghaloo, T.; Li, S. Immunomodulatory Microneedle Patch for Periodontal Tissue Regeneration. Matter 2022, 5, 666–682.
- Bui, V.D.; Son, S.; Xavier, W.; Jung, J.M.; Lee, J.; Shin, S.; Um, W.; An, J.Y.; Kim, C.H.; Song, Y.; et al. Dissolving Microneedles for Long-Term Storage and Transdermal Delivery of Extracellular Vesicles. Biomaterials 2022, 287, 121644.
- Sartawi, Z.; Blackshields, C.; Faisal, W. Dissolving Microneedles: Applications and Growing Therapeutic Potential. J. Control. Release 2022, 348, 186–205.
- Liu, Y.; Zhang, H.; Zhang, J.; Zheng, Y. Transient Swelling of Polymeric Hydrogels: A New Finite Element Solution Framework. Int. J. Solids Struct. 2016, 80, 246–260.
- Mozhdehi, D.; Ayala, S.; Cromwell, O.R.; Guan, Z. Self-healing multiphase polymers via dynamic metal-ligand interactions. J. Am. Chem. Soc. 2014, 136, 16128–16131.
- Liao, H.; Guo, X.; Wan, P.; Yu, G. Conductive MXene Nanocomposite Organohydrogel for Flexible, Healable, Low-Temperature Tolerant Strain Sensors. Adv. Funct. Mater. 2019, 29, 1904507.
- Liu, X.; Liu, J.; Lin, S.; Zhao, X. Hydrogel Machines. Mater. Today 2020, 36, 102–124.
- Sun, W.; Duan, T.; Cao, Y.; Li, H. An Injectable Self-Healing Protein Hydrogel with Multiple Dissipation Modes and Tunable Dynamic Response. Biomacromolecules 2019, 20, 4199–4207.
- Shen, H.; Lin, Q.; Tang, H.; Tian, Y.; Zhang, X. Fabrication of Temperature- and Alcohol-Responsive Photonic Crystal Hydrogel and Its Application for Sustained Drug Release. Langmuir 2022, 38, 3785–3794.
- Su, X.; Feng, Y.; Shi, H.; Wang, F.; Wang, Z.; Hou, S.; Song, X.; Yang, J.; Liu, L. A Hydrogel Dressing with Tunable Critical Temperature and Photothermal Modulating Melittin Release for Multiply Antibacterial Treatment. Int. J. Biol. Macromol. 2023, 239, 124272.
- Chen, G.; Zhou, Y.; Dai, J.; Yan, S.; Miao, W.; Ren, L. Calcium Alginate/PNIPAAm Hydrogel with Body Temperature Response and Great Biocompatibility: Application as Burn Wound Dressing. Int. J. Biol. Macromol. 2022, 216, 686–697.
- Jiang, B.; Liu, X.; Yang, C.; Yang, Z.; Luo, J.; Kou, S.; Liu, K.; Sun, F. Injectable, Photoresponsive Hydrogels for Delivering Neuroprotective Proteins Enabled by Metal-Directed Protein Assembly. Sci. Adv. 2020, 6, eabc4824.
- Odinotski, S.; Dhingra, K.; GhavamiNejad, A.; Zheng, H.; GhavamiNejad, P.; Gaouda, H.; Mohammadrezaei, D.; Poudineh, M. A Conductive Hydrogel-Based Microneedle Platform for Real-Time pH Measurement in Live Animals. Small 2022, 18, e2200201.
- Edirisinghe, D.I.U.; D’Souza, A.; Ramezani, M.; Carroll, R.J.; Chicón, Q.; Muenzel, C.L.; Soule, J.; Monroe, M.B.B.; Patteson, A.E.; Makhlynets, O.V. Antibacterial and Cytocompatible pH-Responsive Peptide Hydrogel. Molecules 2023, 28, 4390.
- Xu, Z.; Liu, G.; Liu, P.; Hu, Y.; Chen, Y.; Fang, Y.; Sun, G.; Huang, H.; Wu, J. Hyaluronic Acid-Based Glucose-Responsive Antioxidant Hydrogel Platform for Enhanced Diabetic Wound Repair. Acta Biomater. 2022, 147, 147–157.
- Yu, H.; Huang, C.; Kong, X.; Ma, J.; Ren, P.; Chen, J.; Zhang, X.; Luo, H.; Chen, G. Nanoarchitectonics of Cartilage-Targeting Hydrogel Microspheres with Reactive Oxygen Species Responsiveness for the Repair of Osteoarthritis. ACS Appl. Mater. Interfaces 2022, 14, 40711–40723.
- Su, M.; Ruan, L.; Dong, X.; Tian, S.; Lang, W.; Wu, M.; Chen, Y.; Lv, Q.; Lei, L. Current State of Knowledge on Intelligent-Response Biological and Other Macromolecular Hydrogels in Biomedical Engineering: A Review. Int. J. Biol. Macromol. 2023, 227, 472–492.
- Liang, Y.; He, J.; Guo, B. Functional Hydrogels as Wound Dressing to Enhance Wound Healing. ACS Nano 2021, 15, 12687–12722.
- Guo, Z.; Liu, H.; Shi, Z.; Lin, L.; Li, Y.; Wang, M.; Pan, G.; Lei, Y.; Xue, L. Responsive Hydrogel-Based Microneedle Dressing for Diabetic Wound Healing. J. Mater. Chem. B 2022, 10, 3501–3511.
- Razzaghi, M.; Seyfoori, A.; Pagan, E.; Askari, E.; Hassani Najafabadi, A.; Akbari, M. 3D Printed Hydrogel Microneedle Arrays for Interstitial Fluid Biomarker Extraction and Colorimetric Detection. Polymers 2023, 15, 1389.
- Ma, W.; Zhang, X.; Liu, Y.; Fan, L.; Gan, J.; Liu, W.; Zhao, Y.; Sun, L. Polydopamine Decorated Microneedles with Fe-MSC-Derived Nanovesicles Encapsulation for Wound Healing. Adv. Sci. 2022, 9, 2103317.
- Chi, J.; Zhang, X.; Chen, C.; Shao, C.; Zhao, Y.; Wang, Y. Antibacterial and Angiogenic Chitosan Microneedle Array Patch for Promoting Wound Healing. Bioact. Mater. 2020, 5, 253–259.
- Li, B.; Lu, G.; Liu, W.; Liao, L.; Ban, J.; Lu, Z. Formulation and Evaluation of PLGA Nanoparticulate-Based Microneedle System for Potential Treatment of Neurological Diseases. Int. J. Nanomed. 2023, 18, 3745–3760.
- Yin, M.; Wu, J.; Deng, M.; Wang, P.; Ji, G.; Wang, M.; Zhou, C.; Blum, N.T.; Zhang, W.; Shi, H.; et al. Multifunctional Magnesium Organic Framework-Based Microneedle Patch for Accelerating Diabetic Wound Healing. ACS Nano 2021, 15, 17842–17853.
- Wu, T.; Hou, X.; Li, J.; Ruan, H.; Pei, L.; Guo, T.; Wang, Z.; Ci, T.; Ruan, S.; He, Y.; et al. Microneedle-Mediated Biomimetic Cyclodextrin Metal Organic Frameworks for Active Targeting and Treatment of Hypertrophic Scars. ACS Nano 2021, 15, 20087–20104.
- Choi, S.Y.; Kwon, H.J.; Ahn, G.R.; Ko, E.J.; Yoo, K.H.; Kim, B.J.; Lee, C.; Kim, D. Hyaluronic Acid Microneedle Patch for the Improvement of Crow’s Feet Wrinkles. Dermatol. Ther. 2017, 30, e12546.
- Xing, M.; Liu, H.; Meng, F.; Ma, Y.; Zhang, S.; Gao, Y. Design and Evaluation of Complex Polypeptide-Loaded Dissolving Microneedles for Improving Facial Wrinkles in Different Areas. Polymers 2022, 14, 4475.
- He, M.; Yang, G.; Zhao, X.; Zhang, S.; Gao, Y. Intradermal Implantable PLGA Microneedles for Etonogestrel Sustained Release. J. Pharm. Sci. 2020, 109, 1958–1966.
- Jin, X.; Zhu, D.D.; Chen, B.Z.; Ashfaq, M.; Guo, X.D. Insulin Delivery Systems Combined with Microneedle Technology. Adv. Drug Deliv. Rev. 2018, 127, 119–137.
- Jamaledin, R.; Yiu, C.K.Y.; Zare, E.N.; Niu, L.-N.; Vecchione, R.; Chen, G.; Gu, Z.; Tay, F.R.; Makvandi, P. Advances in Antimicrobial Microneedle Patches for Combating Infections. Adv. Mater. 2020, 32, 2002129.
- Wolf, P. The Nature and Significance of Platelet Products in Human Plasma. Br. J. Haematol. 1967, 13, 269–288.
- Schrier, S.L.; Godin, D.; Gould, R.G.; Swyryd, B.; Junga, I.; Seeger, M. Characterization of Microvesicles Produced by Shearing of Human Erythrocyte Membranes. Biochim. Biophys. Acta 1971, 233, 26–36.
- Anderson, H.C. Electron Microscopic Studies of Induced Cartilage Development and Calcification. J. Cell Biol. 1967, 35, 81–101.
- Azoidis, I.; Cox, S.C.; Davies, O.G. The Role of Extracellular Vesicles in Biomineralisation: Current Perspective and Application in Regenerative Medicine. J. Tissue Eng. 2018, 9, 2041731418810130.
- Tan, T.T.; Toh, W.S.; Lai, R.C.; Lim, S.K. Practical Considerations in Transforming MSC Therapy for Neurological Diseases from Cell to EV. Exp. Neurol. 2022, 349, 113953.
- Gill, S.; Catchpole, R.; Forterre, P. Extracellular Membrane Vesicles in the Three Domains of Life and Beyond. FEMS Microbiol. Rev. 2019, 43, 273–303.
- Ratajczak, M.Z.; Ratajczak, J. Extracellular Microvesicles/Exosomes: Discovery, Disbelief, Acceptance, and the Future? Leukemia 2020, 34, 3126–3135.
- Fyfe, J.; Casari, I.; Manfredi, M.; Falasca, M. Role of Lipid Signalling in Extracellular Vesicles-Mediated Cell-to-Cell Communication. Cytokine Growth Factor. Rev. 2023, 73, 20–26.
- Jadli, A.S.; Ballasy, N.; Edalat, P.; Patel, V.B. Inside(Sight) of Tiny Communicator: Exosome Biogenesis, Secretion, and Uptake. Mol. Cell Biochem. 2020, 467, 77–94.
- Sheta, M.; Taha, E.A.; Lu, Y.; Eguchi, T. Extracellular Vesicles: New Classification and Tumor Immunosuppression. Biology 2023, 12, 110.
- Gomez, I.; Ward, B.; Souilhol, C.; Recarti, C.; Ariaans, M.; Johnston, J.; Burnett, A.; Mahmoud, M.; Luong, L.A.; West, L.; et al. Neutrophil Microvesicles Drive Atherosclerosis by Delivering miR-155 to Atheroprone Endothelium. Nat. Commun. 2020, 11, 214.
- Thakur, A.; Ke, X.; Chen, Y.-W.; Motallebnejad, P.; Zhang, K.; Lian, Q.; Chen, H.J. The Mini Player with Diverse Functions: Extracellular Vesicles in Cell Biology, Disease, and Therapeutics. Protein Cell 2022, 13, 631–654.
- Janouskova, O.; Herma, R.; Semeradtova, A.; Poustka, D.; Liegertova, M.; Malinska, H.A.; Maly, J. Conventional and Nonconventional Sources of Exosomes–Isolation Methods and Influence on Their Downstream Biomedical Application. Front. Mol. Biosci. 2022, 9, 846650.




