
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Marcin Piechocki | -- | 5401 | 2024-03-16 11:41:35 | | | |
| 2 | Mona Zou | Meta information modification | 5401 | 2024-03-18 10:18:07 | | |
Video Upload Options
Atherosclerosis is a generalized and progressive disease. Ageing is a key risk factor for atherosclerosis progression that is associated with the increased incidence of ischemic events in supplied organs, including stroke, coronary events, limb ischemia, or renal failure. Cardiovascular disease is the leading cause of death and major disability in adults ≥ 75 years of age. Atherosclerotic occlusive disease affects everyday activity and quality of life, and it is associated with reduced life expectancy. Although there is evidence on coronary artery disease management in the elderly, there is insufficient data on the management in older patients presented with atherosclerotic lesions outside the coronary territory. Despite this, trials and observational studies systematically exclude older patients, particularly those with severe comorbidities, physical or cognitive dysfunctions, frailty, or residence in a nursing home. This results in serious critical gaps in knowledge and a lack of guidance on the appropriate medical treatment and referral for endovascular or surgical interventions.
1. Epidemiology, Risk Factors, and Clinical Course of Atherosclerosis in Arterial Territories outside Coronary Arteries, with a Particular Emphasis in Elderly Patients
2. Familial Hypercholesterolemia and the Extent of Atherosclerotic Lesions
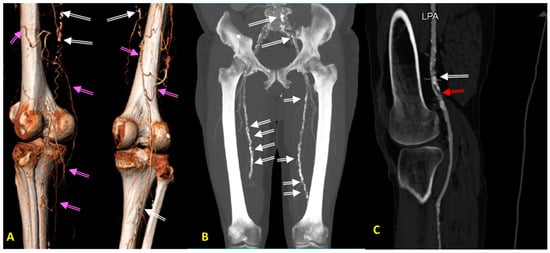
3. Lower Extremity Peripheral Arterial Disease
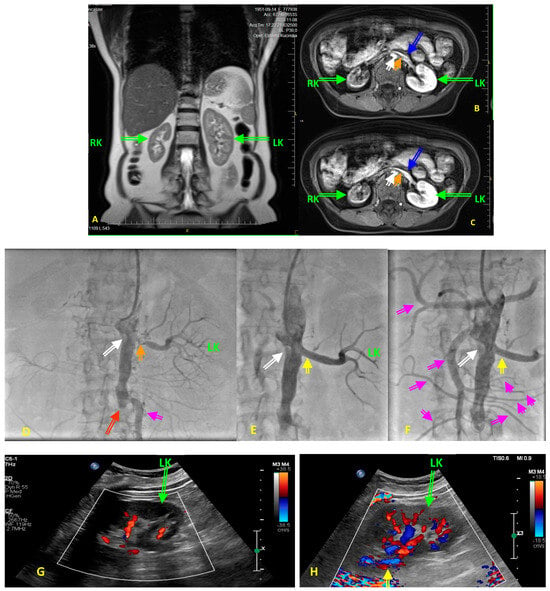
4. Renal Artery Atherosclerosis
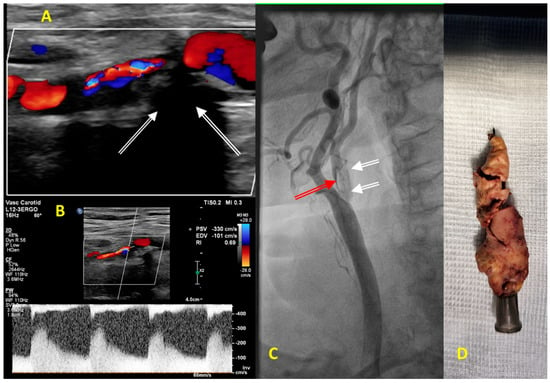
5. Carotid Artery Atherosclerosis
References
- Przewłocki, T.; Kabłak-Ziembicka, A.; Kozanecki, A.; Rzeźnik, D.; Pieniazek, P.; Musiałek, P.; Piskorz, A.; Sokołowski, A.; Rosławiecka, A.; Tracz, W. Polyvascular Extracoronary Atherosclerotic Disease in Patients with Coronary Artery Disease. Kardiol. Pol. 2009, 67, 978–984.
- Ness, J.; Aronow, W.S. Prevalence of Coexistence of Coronary Artery Disease, Ischemic Stroke, and Peripheral Arterial Disease in Older Persons, Mean Age 80 Years, in an Academic Hospital-Based Geriatrics Practice. J. Am. Geriatr. Soc. 1999, 47, 1255–1256.
- Márquez, A.B.; van der Vorst, E.P.C.; Maas, S.L. Key Chemokine Pathways in Atherosclerosis and Their Therapeutic Potential. J. Clin. Med. 2021, 10, 3825.
- Adams, H.P. Secondary Prevention of Atherothrombotic Events after Ischemic Stroke. Mayo Clin. Proc. 2009, 84, 43–51.
- Fleg, J.L.; Forman, D.E.; Berra, K.; Bittner, V.; Blumenthal, J.A.; Chen, M.A.; Cheng, S.; Kitzman, D.W.; Maurer, M.S.; Rich, M.W.; et al. Secondary Prevention of Atherosclerotic Cardiovascular Disease in Older Adults: A Scientific Statement from the American Heart Association. Circulation 2013, 128, 2422–2446.
- Samsky, M.D.; Mentz, R.J.; Stebbins, A.; Lokhnygina, Y.; Aday, A.W.; Pagidipati, N.J.; Jones, W.S.; Katona, B.G.; Patel, M.R.; Holman, R.R.; et al. Polyvascular disease and increased risk of cardiovascular events in patients with type 2 diabetes: Insights from the EXSCEL trial. Atherosclerosis 2021, 338, 1–6.
- Eagle, K.A.; Hirsch, A.T.; Califf, R.M.; Alberts, M.J.; Steg, P.G.; Cannon, C.P.; Brennan, D.M.; Bhatt, D.L.; REACH Registry Investigators. Cardiovascular ischemic event rates in outpatients with symptomatic atherothrombosis or risk factors in the united states: Insights from the REACH Registry. Crit. Pathw. Cardiol. 2009, 8, 91–97.
- Yakubov, S. Polyvascular atherosclerotic disease: Recognizing the risks and managing the syndrome. Curr. Med. Res. Opin. 2009, 25, 2631–2641.
- Badacz, R.; Przewłocki, T.; Pieniażek, P.; Rosławiecka, A.; Kleczyński, P.; Legutko, J.; Żmudka, K.; Kabłak-Ziembicka, A. MicroRNA-134-5p and the Extent of Arterial Occlusive Disease Are Associated with Risk of Future Adverse Cardiac and Cerebral Events in Diabetic Patients Undergoing Carotid Artery Stenting for Symptomatic Carotid Artery Disease. Molecules 2022, 27, 2472.
- Matsushita, K.; Sang, Y.; Ning, H.; Ballew, S.H.; Chow, E.K.; Grams, M.E.; Selvin, E.; Allison, M.; Criqui, M.; Coresh, J.; et al. Lifetime Risk of Lower-Extremity Peripheral Artery Disease Defined by Ankle-Brachial Index in the United States. J. Am. Heart Assoc. 2019, 8, 012177.
- Saleh, M.; Ali, H.; Atalla, K.; Shahat, M.; Cieri, E. Predictors of Carotid Artery Stenting-Induced Hemodynamic Instability. Vasc. Endovasc. Surg. 2021, 55, 475–481.
- Wilson, P.W.F.; Hoeg, J.M.; D’Agostino, R.B.; Silbershatz, H.; Belanger, A.M.; Poehlmann, H.; O’Leary, D.; Wolf, P.A. Cumulative Effects of High Cholesterol Levels, High Blood Pressure, and Cigarette Smoking on Carotid Stenosis. N. Engl. J. Med. 1997, 337, 516–522.
- Meijer, W.T.; Grobbee, D.E.; Hunink, M.G.M.; Hofman, A.; Hoes, A.W. Determinants of Peripheral Arterial Disease in the Elderly. Arch. Intern. Med. 2000, 160, 2934.
- Triana-Ricci, R.; Martinez-de-Jesús, F.; Aragón-Carreño, M.P.; Saurral, R.; Tamayo-Acosta, C.A.; García-Puerta, M.; Bernal, P.V.; Silva-Quiñonez, K.; Feijo, D.F.; Reyes, C.; et al. Management Recommendations for Diabetic Foot Patients. Instructional Course. Rev. Colomb. Ortop. Traumatol. 2021, 35, 330–357.
- Li, Y.; Liu, Y.; Liu, S.; Gao, M.; Wang, W.; Chen, K.; Huang, L.; Liu, Y. Diabetic vascular diseases: Molecular mechanisms and therapeutic strategies. Signal Transduct. Target. Ther. 2023, 8, 152.
- Zhou, X.; Yu, L.; Zhao, Y.; Ge, J. Panvascular medicine: An emerging discipline focusing on atherosclerotic diseases. Eur. Heart. J. 2022, 43, 4528–4531.
- Sniderman, A.D.; Glavinovic, T.; Thanassoulis, G. Key questions about familial hypercholesterolemia: JACC review topic of the week. J. Am. Coll. Cardiol. 2022, 79, 1023–1031.
- Jóźwiak, J.J.; Kasperczyk, S.; Tomasik, T.; Osadnik, T.; Windak, A.; Studziński, K.; Mastej, M.; Catapano, A.; Ray, K.K.; Mikhailidis, D.P.; et al. Design and rationale of a nationwide screening analysis from the LIPIDOGRAM2015 and LIPIDOGEN2015 studies. Arch. Med. Sci. 2020, 18, 604–616.
- Shah, N.P.; Ahmed, H.M.; Wilson Tang, W.H. Familial hypercholesterolemia: Detect, treat, and ask about family. Cleve. Clin. J. Med. 2020, 87, 109–120.
- Aparicio, A.; Villazón, F.; Suárez-Gutiérrez, L.; Gómez, J.; Martínez-Faedo, C.; Méndez-Torre, E.; Avanzas, P.; Álvarez-Velasco, R.; Cuesta-Llavona, E.; García-Lago, C.; et al. Clinical Evaluation of Patients with Genetically Confirmed Familial Hypercholesterolemia. J. Clin. Med. 2023, 12, 1030.
- Timoshchenko, O.; Ivanoshchuk, D.; Semaev, S.; Orlov, P.; Zorina, V.; Shakhtshneider, E. Diagnosis of Familial Hypercholesterolemia in Children and Young Adults. Int. J. Mol. Sci. 2024, 25, 314.
- Dobrowolski, P.; Kabat, M.; Kepka, C.; Januszewicz, A.; Prejbisz, A. Atherosclerotic cardiovascular disease burden in patients with familial hypercholesterolemia: Interpretation of data on involvement of different vascular beds. Pol. Arch. Intern. Med. 2022, 132, 16248.
- Pajak, A.; Szafraniec, K.; Polak, M.; Drygas, W.; Piotrowski, W.; Zdrojewski, T.; Jankowski, P. Prevalence of familial hypercholesterolemia: A meta-analysis of six large, observational, population-based studies in Poland. Arch. Med. Sci. 2016, 4, 687–696.
- Araki, M.; Yonetsu, T.; Kurihara, O.; Nakajima, A.; Lee, H.; Soeda, T.; Minami, Y.; McNulty, I.; Uemura, S.; Kakuta, T.; et al. Predictors of Rapid Plaque Progression: An Optical Coherence Tomography Study. JACC Cardiovasc. Imaging 2021, 14, 1628–1638.
- Anagnostis, P.; Vaitsi, K.; Mintziori, G.; Goulis, D.G.; Mikhailidis, D.P. Non-coronary atherosclerotic cardiovascular disease in patients with familial hypercholesterolaemia. Curr. Med. Res. Opin. 2020, 36, 731–740.
- Gałąska, R.; Kulawiak-Gałąska, D.; Dorniak, K.; Stróżyk, A.; Sabisz, A.; Chmara, M.; Wasąg, B.; Mickiewicz, A.; Rynkiewicz, A.; Fijałkowski, M.; et al. Aortic Wall Thickness as a Surrogate for Subclinical Atherosclerosis in Familial and Nonfamilial Hypercholesterolemia: Quantitative 3D Magnetic Resonance Imaging Study and Interrelations with Computed Tomography Calcium Scores, and Carotid Ultrasonography. J. Clin. Med. 2023, 12, 5589.
- Anagnostis, P.; Antza, C.; Florentin, M.; Kotsis, V. Familial hypercholesterolemia and its manifestations: Practical considerations for general practitioners. Kardiol. Pol. 2023, 81, 1081–1088.
- Simon Broome Register Group. Risk of fatal coronary heart disease in familial hypercholesterolaemia. Scientific Steering Committee on behalf of the Simon Broome Register Group. BMJ 1991, 303, 893–896.
- Marco-Benedí, V.; Bea, A.M.; Cenarro, A.; Jarauta, E.; Laclaustra, M.; Civeira, F. Current causes of death in familial hypercholesterolemia. Lipids Health Dis. 2022, 21, 64.
- Criqui, M.H.; Matsushita, K.; Aboyans, V.; Hess, C.N.; Hicks, C.W.; Kwan, T.W.; McDermott, M.M.; Misra, S.; Ujueta, F.; American Heart Association Council on Epidemiology and Prevention; et al. Lower Extremity Peripheral Artery Disease: Contemporary Epidemiology, Management Gaps, and Future Directions: A Scientific Statement From the American Heart Association. Circulation 2021, 144, e171–e191.
- Ziegler-Graham, K.; MacKenzie, E.J.; Ephraim, P.L.; Travison, T.G.; Brookmeyer, R. Estimating the Prevalence of Limb Loss in the United States: 2005 to 2050. Arch. Phys. Med. Rehabil. 2008, 89, 422–429.
- Krasinski, Z.; Gaciong, Z.; Szymański, F.; Kowalewski, R.; Urbanek, T. The Position of Polish Experts on Conservative Management in Patients with Artery Diseases of Lower Limbs. Acta Angiol. 2019, 25, 41–76.
- Lin, J.; Chen, Y.; Jiang, N.; Li, Z.; Xu, S. Burden of Peripheral Artery Disease and Its Attributable Risk Factors in 204 Countries and Territories From 1990 to 2019. Front. Cardiovasc. Med. 2022, 9, 868370.
- De Matteis, G.; Biscetti, F.; Della Polla, D.A.; Serra, A.; Burzo, M.L.; Fuorlo, M.; Nicolazzi, M.A.; Novelli, A.; Santoliquido, A.; Gambassi, G.; et al. Sex-Based Differences in Clinical Characteristics and Outcomes among Patients with Peripheral Artery Disease: A Retrospective Analysis. J. Clin. Med. 2023, 12, 5094.
- Meijer, W.T.; Hoes, A.W.; Rutgers, D.; Bots, M.L.; Hofman, A.; Grobbee, D.E. Peripheral Arterial Disease in the Elderly: The Rotterdam Study. Arterioscler. Thromb. Vasc. Biol. 1998, 18, 645–654.
- Park, Y.S.; Ryu, G.W.; Choi, M. Multiple Metabolic Comorbidities and Their Consequences among Patients with Peripheral Arterial Disease. PLoS ONE 2022, 17, e0268201.
- Bevan, G.H.; White Solaru, K.T. Evidence-Based Medical Management of Peripheral Artery Disease. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 541–553.
- Sykora, D.; Firth, C.; Girardo, M.; Bhatt, S.; Matti, L.; Tseng, A.; Shipman, J.; Liedl, D.; Wennberg, P.; Shamoun, F.E. Patient Age at Diagnosis of Peripheral Artery Disease and Its Impact on Cardiovascular and Limb Outcomes. Am. J. Cardiol. 2022, 177, 144–150.
- Rammos, C.; Kontogiannis, A.; Mahabadi, A.A.; Steinmetz, M.; Messiha, D.; Lortz, J.; Rassaf, T. Risk Stratification and Mortality Prediction in Octo- and Nonagenarians with Peripheral Artery Disease: A Retrospective Analysis. BMC Cardiovasc. Disord. 2021, 21, 370.
- Aboyans, V.; Ho, E.; Denenberg, J.O.; Ho, L.A.; Natarajan, L.; Criqui, M.H. The Association between Elevated Ankle Systolic Pressures and Peripheral Occlusive Arterial Disease in Diabetic and Nondiabetic Subjects. J. Vasc. Surg. 2008, 48, 1197–1203.
- Zhang, P.; Ma, X.; Guo, R.; Ye, Z.; Fu, H.; Fu, N.; Guo, Z.; Zhang, J.; Zhang, J. Organic Nanoplatforms for Iodinated Contrast Media in CT Imaging. Molecules 2021, 26, 7063.
- Acar, R.D.; Sahin, M.; Kirma, C. One of the Most Urgent Vascular Circumstances: Acute Limb Ischemia. SAGE Open Med. 2013, 1, 205031211351611.
- Baumgartner, I.; Lerman, L.O. Renovascular Hypertension: Screening and Modern Management. Eur. Heart J. 2011, 32, 1590–1598.
- Harding, M.B.; Smith, L.R.; Himmelstein, S.I.; Harrison, K.; Phillips, H.R.; Schwab, S.J.; Hermiller, J.B.; Davidson, C.J.; Bashore, T.M. Renal Artery Stenosis: Prevalence and Associated Risk Factors in Patients Undergoing Routine Cardiac Catheterization. J. Am. Soc. Nephrol. 1992, 2, 609–611.
- Olin, J.W.; Melia, M.; Young, J.R.; Graor, R.A.; Risius, B. Prevalence of Atherosclerotic Renal Artery Stenosis in Patients with Atherosclerosis Elsewhere. Am. J. Med. 1990, 88, 46N–51N.
- de Leeuw, P.W.; Postma, C.T.; Spiering, W.; Kroon, A.A. Atherosclerotic Renal Artery Stenosis: Should We Intervene Earlier? Curr. Hypertens. Rep. 2018, 20, 35.
- Shekhar, S.; Varghese, K.; Li, M.; Fan, L.; Booz, G.W.; Roman, R.J.; Fan, F. Conflicting Roles of 20-HETE in Hypertension and Stroke. Int. J. Mol. Sci. 2019, 20, 4500.
- Conlon, P.J.; Little, M.A.; Pieper, K.; Mark, D.B. Severity of Renal Vascular Disease Predicts Mortality in Patients Undergoing Coronary Angiography. Kidney Int. 2001, 60, 1490–1497.
- Kalra, P.A.; Guo, H.; Kausz, A.T.; Gilbertson, D.T.; Liu, J.; Chen, S.C.; Ishani, A.; Collins, A.J.; Foley, R.N. Atherosclerotic Renovascular Disease in United States Patients Aged 67 Years or Older: Risk Factors, Revascularization, and Prognosis. Kidney Int. 2005, 68, 293–301.
- Przewłocki, T.; Kabłak-Ziembicka, A.; Tracz, W.; Kozanecki, A.; Kopeć, G.; Rubiś, P.; Kostkiewicz, M.; Rosławiecka, A.; Rzeźnik, D.; Stompór, T. Renal Artery Stenosis in Patients with Coronary Artery Disease. Kardiol. Pol. 2008, 66, 856–862.
- Hansen, K.J.; Edwards, M.S.; Craven, T.E.; Cherr, G.S.; Jackson, S.A.; Appel, R.G.; Burke, G.L.; Dean, R.H. Prevalence of Renovascular Disease in the Elderly: A Population-Based Study. J. Vasc. Surg. 2002, 36, 443–451.
- Buller, C.E.; Nogareda, J.G.; Ramanathan, K.; Ricci, D.R.; Djurdjev, O.; Tinckam, K.J.; Penn, I.M.; Fox, R.S.; Stevens, L.A.; Duncan, J.A.; et al. The Profile of Cardiac Patients with Renal Artery Stenosis. J. Am. Coll. Cardiol. 2004, 43, 1606–1613.
- De Mast, Q.; Beutler, J.J. The Prevalence of Atherosclerotic Renal Artery Stenosis in Risk Groups: A Systematic Literature Review. J. Hypertens. 2009, 27, 1333–1340.
- Gunawardena, T. Atherosclerotic Renal Artery Stenosis: A Review. AORTA 2021, 9, 95–99.
- Przewlocki, T.; Kablak-Ziembicka, A.; Tracz, W.; Kopec, G.; Rubis, P.; Pasowicz, M.; Musialek, P.; Kostkiewicz, M.; Kozanecki, A.; Stompór, T.; et al. Prevalence and Prediction of Renal Artery Stenosis in Patients with Coronary and Supraaortic Artery Atherosclerotic Disease. Nephrol. Dial. Transplant. 2008, 23, 580–585.
- van Jaarsveld, B.C.; Krijnen, P.; Pieterman, H.; Derkx, F.H.M.; Deinum, J.; Postma, C.T.; Dees, A.; Woittiez, A.J.J.; Bartelink, A.K.M.; Man in `t Veld, A.J.; et al. The Effect of Balloon Angioplasty on Hypertension in Atherosclerotic Renal-Artery Stenosis. Dutch Renal Artery Stenosis Intervention Cooperative Study Group. N. Engl. J. Med. 2000, 342, 1007–1014.
- Olin, J.W.; Piedmonte, M.R.; Young, J.R.; DeAnna, S.; Grubb, M.; Childs, M.B. The Utility of Duplex Ultrasound Scanning of the Renal Arteries for Diagnosing Significant Renal Artery Stenosis. Ann. Intern. Med. 1995, 122, 833–838.
- Wang, X.; Cai, S.; Wang, H.; Li, J.; Yang, Y. Deep-learning-based renal artery stenosis diagnosis via multimodal fusion. J. Appl. Clin. Med. Phys. 2024, e14298, Epub ahead of print.
- Orman, G.; Masand, P.M.; Kukreja, K.U.; Acosta, A.A.; Guillerman, R.P.; Jadhav, S.P. Diagnostic sensitivity and specificity of CT angiography for renal artery stenosis in children. Pediatr. Radiol. 2021, 51, 419–426.
- Flors, L.; Leiva-Salinas, C.; Ahmad, E.A.; Norton, P.T.; Turba, U.C.; Bozlar, U.; Hagspiel, K.D. MD CT angiography and MR angiography of nonatherosclerotic renal artery disease. Cardiovasc. Interv. Radiol. 2011, 34, 1151–1164.
- Guo, X.; Gong, Y.; Wu, Z.; Yan, F.; Ding, X.; Xu, X. Renal artery assessment with non-enhanced MR angiography versus digital subtraction angiography: Comparison between 1.5 and 3.0 T. Eur. Radiol. 2020, 30, 1747–1754.
- Hirsch, A.T.; Haskal, Z.J.; Hertzer, N.R.; Bakal, C.W.; Creager, M.A.; Halperin, J.L.; Hiratzka, L.F.; Murphy, W.R.C.; Olin, J.W.; Puschett, J.B.; et al. ACC/AHA 2005 Practice Guidelines for the Management of Patients With Peripheral Arterial Disease (Lower Extremity, Renal, Mesenteric, and Abdominal Aortic). Circulation 2006, 113, e463–e654.
- Chrysochou, C.; Foley, R.N.; Young, J.F.; Khavandi, K.; Cheung, C.M.; Kalra, P.A. Dispelling the Myth: The Use of Renin-Angiotensin Blockade in Atheromatous Renovascular Disease. Nephrol. Dial. Transplant. 2012, 27, 1403–1409.
- Losito, A.; Errico, R.; Santirosi, P.; Lupattelli, T.; Scalera, G.B.; Lupattelli, L. Long-Term Follow-up of Atherosclerotic Renovascular Disease. Beneficial Effect of ACE Inhibition. Nephrol. Dial. Transplant. 2005, 20, 1604–1609.
- Cheung, C.M.; Patel, A.; Shaheen, N.; Cain, S.; Eddington, H.; Hegarty, J.; Middleton, R.J.; Cowie, A.; Mamtora, H.; Kalra, P.A. The Effects of Statins on the Progression of Atherosclerotic Renovascular Disease. Nephron Clin. Pract. 2007, 107, c35–c42.
- De Silva, R.; Nikitin, N.P.; Bhandari, S.; Nicholson, A.; Clark, A.L.; Cleland, J.G.F. Atherosclerotic Renovascular Disease in Chronic Heart Failure: Should We Intervene? Eur. Heart J. 2005, 26, 1596–1605.
- Bates, M.C.; Campbell, J.E.; Stone, P.A.; Jaff, M.R.; Broce, M.; Lavigne, P.S. Factors affecting long-term survival following renal artery stenting. Catheter Cardiovasc. Interv. 2007, 69, 1037–1043.
- Hackam, D.G.; Wu, F.; Li, P.; Austin, P.C.; Tobe, S.W.; Mamdani, M.M.; Garg, A.X. Statins and Renovascular Disease in the Elderly: A Population-Based Cohort Study. Eur. Heart J. 2011, 32, 598–610.
- Hackam, D.G.; Duong-Hua, M.L.; Mamdani, M.; Li, P.; Tobe, S.W.; Spence, J.D.; Garg, A.X. Angiotensin Inhibition in Renovascular Disease: A Population-Based Cohort Study. Am. Heart J. 2008, 156, 549–555.
- Deshmukh, H.; Barker, E.; Anbarasan, T.; Levin, D.; Bell, S.; Witham, M.D.; George, J. Calcium Channel Blockers Are Associated with Improved Survival and Lower Cardiovascular Mortality in Patients with Renovascular Disease. Cardiovasc. Ther. 2018, 36, e12474.
- Ritchie, J.; Green, D.; Alderson, H.V.; Chrysochou, C.; Vassallo, D.; Sinha, S.; Kalra, P.A. Associations of Antiplatelet Therapy and Beta Blockade with Patient Outcomes in Atherosclerotic Renovascular Disease. J. Am. Soc. Hypertens. 2016, 10, 149–158.e3.
- Badacz, R.; Kabłak-Ziembicka, A.; Rosławiecka, A.; Rzeźnik, D.; Baran, J.; Trystuła, M.; Legutko, J.; Przewłocki, T. The Maintained Glycemic Target Goal and Renal Function Are Associated with Cardiovascular and Renal Outcomes in Diabetic Patients Following Stent-Supported Angioplasty for Renovascular Atherosclerotic Disease. J. Pers. Med. 2022, 12, 537.
- Moura, F.A.; Berg, D.D.; Bellavia, A.; Dwyer, J.P.; Mosenzon, O.; Scirica, B.M.; Wiviott, S.D.; Bhatt, D.L.; Raz, I.; Feinberg, M.W.; et al. Risk Assessment of Kidney Disease Progression and Efficacy of SGLT2 Inhibition in Patients With Type 2 Diabetes. Diabetes Care 2023, 46, 1807–1815.
- Leertouwer, T.C.; Gussenhoven, E.J.; Bosch, J.L.; Van Jaarsveld, B.C.; Van Dijk, L.C.; Deinum, J.; Manin’t Veld, A.J. Stent Placement for Renal Arterial Stenosis: Where Do We Stand? A Meta-Analysis. Radiology 2000, 216, 78–85.
- Bhalla, V.; Textor, S.C.; Beckman, J.A.; Casanegra, A.I.; Cooper, C.J.; Kim, E.S.H.; Luther, J.M.; Misra, S.; Oderich, G.S. Revascularization for Renovascular Disease: A Scientific Statement From the American Heart Association. Hypertension 2022, 79, E128–E143.
- Caielli, P.; Frigo, A.C.; Pengo, M.F.; Rossitto, G.; Maiolino, G.; Seccia, T.M.; Calò, L.A.; Miotto, D.; Rossi, G.P. Treatment of Atherosclerotic Renovascular Hypertension: Review of Observational Studies and a Meta-Analysis of Randomized Clinical Trials. Nephrol. Dial. Transplant. 2015, 30, 541–553.
- Kane, G.C.; Xu, N.; Mistrik, E.; Roubicek, T.; Stanson, A.W.; Garovic, V.D. Renal Artery Revascularization Improves Heart Failure Control in Patients with Atherosclerotic Renal Artery Stenosis. Nephrol. Dial. Transplant. 2010, 25, 813–820.
- Ritchie, J.; Green, D.; Chrysochou, C.; Chalmers, N.; Foley, R.N.; Kalra, P.A. High-Risk Clinical Presentations in Atherosclerotic Renovascular Disease: Prognosis and Response to Renal Artery Revascularization. Am. J. Kidney Dis. 2014, 63, 186–197.
- De Weerd, M.; Greving, J.P.; De Jong, A.W.F.; Buskens, E.; Bots, M.L. Prevalence of Asymptomatic Carotid Artery Stenosis According to Age and Sex: Systematic Review and Metaregression Analysis. Stroke 2009, 40, 1105–1113.
- Van Oostrom, O.; Velema, E.; Schoneveld, A.H.; De Vries, J.P.P.M.; De Bruin, P.; Seldenrijk, C.A.; De Kleijn, D.P.V.; Busser, E.; Moll, F.L.; Verheijen, J.H.; et al. Age-Related Changes in Plaque Composition: A Study in Patients Suffering from Carotid Artery Stenosis. Cardiovasc. Pathol. 2005, 14, 126–134.
- Heo, S.H.; Bushnell, C.D. Factors Influencing Decision Making for Carotid Endarterectomy versus Stenting in the Very Elderly. Front. Neurol. 2017, 8, 220.
- Underhill, H.R.; Yuan, C.; Zhao, X.Q.; Kraiss, L.W.; Parker, D.L.; Saam, T.; Chu, B.; Takaya, N.; Liu, F.; Polissar, N.L.; et al. Effect of Rosuvastatin Therapy on Carotid Plaque Morphology and Composition in Moderately Hypercholesterolemic Patients: A High-Resolution Magnetic Resonance Imaging Trial. Am. Heart J. 2008, 155, 584.e1–584.e8.
- Stoll, F.; Eidam, A.; Michael, L.; Bauer, J.M.; Haefeli, W.E. Drug Treatment of Hypercholesterolemia in Older Adults: Focus on Newer Agents. Drugs Aging 2022, 39, 251–256.
- Faggiano, P.; Scodro, M.; Sbolli, M.; Branca, L.; Cani, D.; Valentini, F.; Perego, C.; Provini, M. Blood Pressure Control in Older Patients with Carotid Artery Stenosis. Monaldi Arch. Chest Dis. 2018, 88, 41–43.
- Klimontov, V.V.; Koroleva, E.A.; Khapaev, R.S.; Korbut, A.I.; Lykov, A.P. Carotid Artery Disease in Subjects with Type 2 Diabetes: Risk Factors and Biomarkers. J. Clin. Med. 2021, 11, 72.
- Marquardt, L.; Geraghty, O.C.; Mehta, Z.; Rothwell, P.M. Low risk of ipsilateral stroke in patients with asymptomatic carotid stenosis on best medical treatment: A prospective, population-based study. Stroke 2010, 41, e11–e17.
- Abbott, A.L. Medical (nonsurgical) intervention alone is now best for prevention of stroke associated with asymptomatic severe carotid stenosis: Results of a systematic review and analysis. Stroke 2009, 40, e573–e583.
- Narins, C.R.; Illig, K.A. Patient Selection for Carotid Stenting versus Endarterectomy: A Systematic Review. J. Vasc. Surg. 2006, 44, 661–672.
- Roffi, M.; Mukherjee, D.; Clair, D.G. Carotid artery stenting vs. endarterectomy. Eur. Heart J. 2009, 30, 2693–2704.
- Bonati, L.H.; Dobson, J.; Featherstone, R.L.; Ederle, J.; Van Der Worp, H.B.; De Borst, G.J.; Mali, W.P.T.M.; Beard, J.D.; Cleveland, T.; Engelter, S.T.; et al. Long-Term Outcomes after Stenting versus Endarterectomy for Treatment of Symptomatic Carotid Stenosis: The International Carotid Stenting Study (ICSS) Randomised Trial. Lancet 2015, 385, 529–538.
- Kernan, W.N.; Ovbiagele, B.; Black, H.R.; Bravata, D.M.; Chimowitz, M.I.; Ezekowitz, M.D.; Fang, M.C.; Fisher, M.; Furie, K.L.; Heck, D.V.; et al. Guidelines for the Prevention of Stroke in Patients with Stroke and Transient Ischemic Attack: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2014, 45, 2160–2236.
- Pandit, V.; Lee, A.; Zeeshan, M.; Goshima, K.; Tan, T.-W.; Jhajj, S.; Trinidad, B.; Weinkauf, C.; Zhou, W. Effect of Frailty Syndrome on the Outcomes of Patients with Carotid Stenosis. J. Vasc. Surg. 2020, 71, 1595–1600.
- Ballotta, E.; Toniato, A.; Da Roit, A.; Lorenzetti, R.; Piatto, G.; Baracchini, C. Carotid Endarterectomy for Asymptomatic Carotid Stenosis in the Very Elderly. J. Vasc. Surg. 2015, 61, 382–388.
- Chiam, P.T.L.; Roubin, G.S.; Panagopoulos, G.; Iyer, S.S.; Green, R.M.; Brennan, C.; Vitek, J.J. One-Year Clinical Outcomes, Midterm Survival, and Predictors of Mortality after Carotid Stenting in Elderly Patients. Circulation 2009, 119, 2343–2348.
- Grant, A.; White, C.; Ansel, G.; Bacharach, M.; Metzger, C.; Velez, C. Safety and Efficacy of Carotid Stenting in the Very Elderly. Catheter. Cardiovasc. Interv. 2010, 75, 651–655.
- Dzierwa, K.; Pieniazek, P.; Tekieli, L.; Musialek, P.; Przewlocki, T.; Kablak-Ziembicka, A.; Kosobucka-Peszat, R.; Machnik, R.; Trystula, M.; Podolec, P. Carotid Artery Stenting According to the “Tailored CAS” Algorithm Performed in the Very Elderly Patients: The Thirty Day Outcome. Catheter. Cardiovasc. Interv. 2013, 82, 681–688.
- Thinggaard, M.; McGue, M.; Jeune, B.; Osler, M.; Vaupel, J.W.; Christensen, K. Survival Prognosis in Very Old Adults. J. Am. Geriatr. Soc. 2016, 64, 81–88.





