
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Jia Xian Law | -- | 3628 | 2024-03-14 08:48:57 | | | |
| 2 | Dean Liu | Meta information modification | 3628 | 2024-04-15 07:16:01 | | |
Video Upload Options
Antibiotic resistance (ABR) in aquatic environments can cause detrimental effects on ecosystems and public health.
1. Importance and Multifaceted Nature of the Aquatic Environment
2. Antibiotic Resistance (ABR) in Aquatic Environments
3. Potential Negative Effects of ABR in Aquatic Environments on Human and Animal Health
4. Summary
The aquatic environment is a vital ecosystem encompassing oceans, seas, lakes, and rivers, crucial for sustaining diverse species and providing essential ecosystem services. However, the rampant use of antibiotics in aquaculture and widespread human activities have led to the emergence of ABR within various antibiotic classes. Better understanding of ABR and its impacts on aquatic environments is crucial to deciphering microbial interactions, comprehending antibiotic resistance dissemination, and managing the ecological impact of microbial communities. A future-oriented perspective on addressing ABR in aquatic environments involves advancing scientific knowledge, fostering collaboration among stakeholders, implementing stringent regulations, and raising public awareness. By embracing these approaches, we can work toward effectively mitigating the spread of ABR and safeguarding the health of aquatic ecosystems and public well-being.
References
- Bashir, I.; Lone, F.A.; Bhat, R.A.; Mir, S.A.; Dar, Z.A.; Dar, S.A. Concerns and threats of contamination on aquatic ecosystems. Bioremediat. Biotechnol. 2020, 1–26.
- Visbeck, M. Ocean science research is key for a sustainable future. Nat. Commun. 2018, 9, 690.
- Nava, V.; Leoni, B. A critical review of interactions between microplastics, microalgae and aquatic ecosystem function. Water Res. 2021, 188, 116476.
- Shivanna, K.R. Climate change and its impact on biodiversity and human welfare. Proc. Indian Natl. Sci. Acad. 2022, 88, 160–171.
- Tang, X.; Xie, G.; Shao, K.; Tian, W.; Gao, G.; Qin, B. Aquatic bacterial diversity, community composition and assembly in the semi-arid inner Mongolia plateau: Combined effects of salinity and nutrient levels. Microorganisms 2021, 9, 208.
- Schar, D.; Klein, E.Y.; Laxminarayan, R.; Gilbert, M.; Van Boeckel, T.P. Global trends in antimicrobial use in aquaculture. Sci. Rep. 2020, 10, 21878.
- Boyd, C.E.; McNevin, A.A.; Davis, R.P. The contribution of fisheries and aquaculture to the global protein supply. Food Secur. 2022, 14, 805–827.
- Manyi-Loh, C.; Mamphweli, S.; Meyer, E.; Okoh, A. Antibiotic use in agriculture and its consequential resistance in environmental sources: Potential public health implications. Molecules 2018, 23, 795.
- Chowdhury, S.; Rheman, S.; Debnath, N.; Delamare-Deboutteville, J.; Akhtar, Z.; Ghosh, S.; Parveen, S.; Islam, K.; Islam, M.A.; Rashid, M.M.; et al. Antibiotics usage practices in aquaculture in Bangladesh and their associated factors. One Health 2022, 15, 100445.
- Tangcharoensathien, V.; Sommanustweechai, A.; Chanthong, B.; Sumpradit, N.; Sakulbumrungsil, R.; Jaroenpoj, S.; Sermsinsiri, V.; Thai SAC Working Group. Surveillance of antimicrobial consumption: Methodological review for systems development in Thailand. J. Glob. Health 2017, 7, 010307.
- Lenz, K.D.; Klosterman, K.E.; Mukundan, H.; Kubicek-Sutherland, J.Z. Macrolides: From toxins to therapeutics. Toxins 2021, 13, 347.
- Bush, K.; Bradford, P.A. β-Lactams and β-Lactamase inhibitors: An overview. Cold Spring Harb. Perspect. Med. 2016, 6, a025247.
- Granados-Chinchilla, F.; Rodríguez, C. Tetracyclines in food and feedingstuffs: From regulation to analytical methods, bacterial resistance, and environmental and health implications. J. Anal. Methods Chem. 2017, 2017, 1315497.
- Chang, D.; Mao, Y.; Qiu, W.; Wu, Y.; Cai, B. The source and distribution of tetracycline antibiotics in China: A review. Toxics 2023, 11, 214.
- Ben, Y.; Fu, C.; Hu, M.; Liu, L.; Wong, M.H.; Zheng, C. Human health risk assessment of antibiotic resistance associated with antibiotic residues in the environment: A review. Environ. Res. 2019, 169, 483–493.
- Liang, X.; Chen, B.; Nie, X.; Shi, Z.; Huang, X.; Li, X. The distribution and partitioning of common antibiotics in water and sediment of the Pearl River Estuary, South China. Chemosphere 2013, 92, 1410–1416.
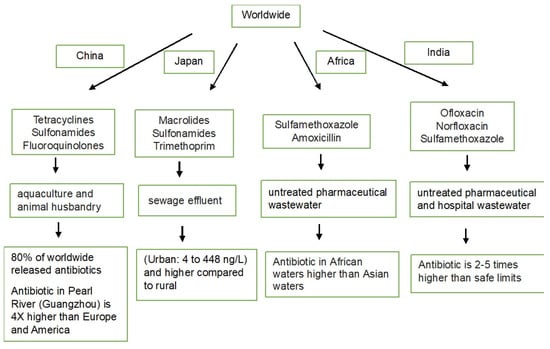
- Polianciuc, S.I.; Gurzău, A.E.; Kiss, B.; Ştefan, M.G.; Loghin, F. Antibiotics in the environment: Causes and consequences. Med. Pharm. Rep. 2020, 93, 231–240.
- Murata, A.; Takada, H.; Mutoh, K.; Hosoda, H.; Harada, A.; Nakada, N. Nationwide monitoring of selected antibiotics: Distribution and sources of sulfonamides, trimethoprim, and macrolides in Japanese rivers. Sci. Total Environ. 2011, 409, 5305–5312.
- Baba, H.; Nishiyama, M.; Watanabe, T.; Kanamori, H. Review of antimicrobial resistance in wastewater in Japan: Current challenges and future perspectives. Antibiotics 2022, 11, 849.
- Medina-Pizzali, M.L.; Hartinger, S.M.; Salmon-Mulanovich, G.; Larson, A.; Riveros, M.; Mäusezahl, D. Antimicrobial resistance in rural settings in Latin America: A scoping review with a one health lens. Int. J. Environ. Res. Public Health 2021, 18, 9837.
- Taneja, N.; Sharma, M. Antimicrobial resistance in the environment: The Indian scenario. Indian J. Med. Res. 2019, 149, 119–128.
- Hanna, N.; Tamhankar, A.J.; Stålsby Lundborg, C. Antibiotic concentrations and antibiotic resistance in aquatic environments of the WHO Western Pacific and South-East Asia regions: A systematic review and probabilistic environmental hazard assessment. Lancet Planet. Health 2023, 7, e45–e54.
- Waleng, N.J.; Nomngongo, P.N. Occurrence of pharmaceuticals in the environmental waters: African and Asian perspectives. Environ. Chem. Ecotoxicol. 2022, 4, 50–66.
- Okeke, E.S.; Chukwudozie, K.I.; Nyaruaba, R.; Ita, R.E.; Oladipo, A.; Ejeromedoghene, O.; Atakpa, E.O.; Agu, C.V.; Okoye, C.O. Antibiotic resistance in aquaculture and aquatic organisms: A review of current nanotechnology applications for sustainable management. Environ. Sci. Pollut. Res. Int. 2022, 29, 69241–69274.
- Watts, J.E.M.; Schreier, H.J.; Lanska, L.; Hale, M.S. The rising tide of antimicrobial resistance in aquaculture: Sources, sinks and solutions. Mar. Drugs 2017, 15, 158.
- Maghsodian, Z.; Sanati, A.M.; Mashifana, T.; Sillanpää, M.; Feng, S.; Nhat, T.; Ramavandi, B. Occurrence and distribution of antibiotics in the water, sediment, and biota of freshwater and marine environments: A review. Antibiotics 2022, 11, 1461.
- Yang, Q.; Gao, Y.; Ke, J.; Show, P.L.; Ge, Y.; Liu, Y.; Guo, R.; Chen, J. Antibiotics: An overview on the environmental occurrence, toxicity, degradation, and removal methods. Bioengineered 2021, 12, 7376–7416.
- Ezzariai, A.; Hafidi, M.; Khadra, A.; Aemig, Q.; El Fels, L.; Barret, M.; Merlina, G.; Patureau, D.; Pinelli, E. Human and veterinary antibiotics during composting of sludge or manure: Global perspectives on persistence, degradation, and resistance genes. J. Hazard. Mater. 2018, 359, 465–481.
- Daeseleire, E.; De Graef, E.; Rasschaert, G.; De Mulder, T.; Van den Meersche, T.; Van Coillie, E.; Dewulf, J.; Heyndrickx, M. Antibiotic use and resistance in animals: Belgian initiatives. Drug Test. Anal. 2016, 8, 549–555.
- Santos, L.; Ramos, F. Antimicrobial resistance in aquaculture: Current knowledge and alternatives to tackle the problem. Int. J. Antimicrob. Agents 2018, 52, 135–143.
- Kariuki, S.; Kering, K.; Wairimu, C.; Onsare, R.; Mbae, C. Antimicrobial resistance rates and surveillance in Sub-Saharan Africa: Where are we now? Infect. Drug Resist. 2022, 15, 3589–3609.
- Zhou, N.; Cheng, Z.; Zhang, X.; Lv, C.; Guo, C.; Liu, H.; Dong, K.; Zhang, Y.; Liu, C.; Chang, Y.F.; et al. Correction: Global antimicrobial resistance: A system-wide comprehensive investigation using the Global One Health Index. Infect. Dis. Poverty 2022, 11, 100.
- Fumagalli, D. Antibiotic resistance, meat consumption and the harm principle. Ethics Policy Environ. 2023, 26, 53–68.
- Suyamud, B.; Chen, Y.; Quyen, D.T.T.; Dong, Z.; Zhao, C.; Hu, J. Antimicrobial resistance in aquaculture: Occurrence and strategies in Southeast Asia. Sci. Total Environ. 2024, 907, 167942.
- Nappier, S.P.; Liguori, K.; Ichida, A.M.; Stewart, J.R.; Jones, K.R. Antibiotic resistance in recreational waters: State of the science. Int. J. Environ. Res. Public Health. 2020, 17, 8034.
- Duarte, A.C.; Rodrigues, S.; Afonso, A.; Nogueira, A.; Coutinho, P. Antibiotic resistance in the drinking water: Old and new strategies to remove antibiotics, resistant bacteria, and resistance genes. Pharmaceuticals 2022, 15, 393.
- Zhang, K.; Li, K.; Xin, R.; Han, Y.; Guo, Z.; Zou, W.; Wei, W.; Cui, X.; Zhang, Z.; Zhang, Y. Antibiotic resistomes in water supply reservoirs sediments of central China: Main biotic drivers and distribution pattern. Environ. Sci. Pollut. Res. Int. 2022, 29, 37712–37721.
- Ahmed, H.; Zolfo, M.; Williams, A.; Ashubwe-Jalemba, J.; Tweya, H.; Adeapena, W.; Labi, A.K.; Adomako, L.A.B.; Addico, G.N.D.; Banu, R.A.; et al. Antibiotic-resistant bacteria in drinking water from the greater Accra region, Ghana: A cross-sectional study, December 2021–March 2022. Int. J. Environ. Res. Public Health 2022, 19, 12300.
- Zhang, K.; Fan, Y.; Chang, S.; Fu, Q.; Zhang, Q.; Yang, G.; Sun, X. Characterization of antibiotic resistance genes in drinking water sources of the Douhe Reservoir, Tangshan, northern China: The correlation with bacterial communities and environmental factors. Environ. Sci. Eur. 2022, 34, 56.
- Landrigan, P.J.; Stegeman, J.J.; Fleming, L.E.; Allemand, D.; Anderson, D.M.; Backer, L.C.; Brucker-Davis, F.; Chevalier, N.; Corra, L.; Czerucka, D.; et al. Human health and ocean pollution. Ann. Glob. Health 2020, 86, 151.
- Fleming, L.E.; McDonough, N.; Austen, M.; Mee, L.; Moore, M.; Hess, P.; Depledge, M.H.; White, M.; Philippart, K.; Bradbrook, P.; et al. Oceans and human health: A rising tide of challenges and opportunities for Europe. Mar. Environ. Res. 2014, 99, 16–19.
- Tchounwou, P.B.; Yedjou, C.G.; Patlolla, A.K.; Sutton, D.J. Heavy metal toxicity and the environment. Exp. Suppl. 2012, 101, 133–164.
- Kraemer, S.A.; Ramachandran, A.; Perron, G.G. Antibiotic pollution in the environment: From microbial ecology to public policy. Microorganisms 2019, 7, 180.
- Gupta, S.; Sreekrishnan, T.R.; Ahammad, S.Z. Effects of heavy metals on the development and proliferation of antibiotic resistance in urban sewage treatment plants. Environ. Pollut. 2022, 308, 119649.
- Tuvo, B.; Scarpaci, M.; Bracaloni, S.; Esposito, E.; Costa, A.L.; Ioppolo, M.; Casini, B. Microplastics and antibiotic resistance: The magnitude of the problem and the emerging role of hospital wastewater. Int. J. Environ. Res. Public Health 2023, 20, 5868.
- Bong, C.W.; Low, K.Y.; Chai, L.C.; Lee, C.W. Prevalence and diversity of antibiotic resistant Escherichia coli from anthropogenic-impacted Larut river. Front. Public Health 2022, 10, 794513.
- Salam, M.A.; Al-Amin, M.Y.; Salam, M.T.; Pawar, J.S.; Akhter, N.; Rabaan, A.A.; Alqumber, M.A.A. Antimicrobial resistance: A growing serious threat for global public health. Healthcare 2023, 11, 1946.
- Michaelis, C.; Grohmann, E. Horizontal gene transfer of antibiotic resistance genes in biofilms. Antibiotics 2023, 12, 328.
- Aslam, B.; Khurshid, M.; Arshad, M.I.; Muzammil, S.; Rasool, M.; Yasmeen, N.; Shah, T.; Chaudhry, T.H.; Rasool, M.H.; Shahid, A.; et al. Antibiotic resistance: One health one world outlook. Front. Cell. Infect. Microbiol. 2021, 11, 771510.
- Monahan, C.; Nag, R.; Morris, D.; Cummins, E. Antibiotic residues in the aquatic environment—Current perspective and risk considerations. J. Environ. Sci. Health A Tox. Hazard. Subst. Environ. Eng. 2021, 56, 733–751.
- Iwu, C.D.; Korsten, L.; Okoh, A.I. The incidence of antibiotic resistance within and beyond the agricultural ecosystem: A concern for public health. Microbiologyopen 2020, 9, e1035.
- Pepi, M.; Focardi, S. Antibiotic-resistant bacteria in aquaculture and climate change: A challenge for health in the Mediterranean area. Int. J. Environ. Res. Public Health 2021, 18, 5723.
- Velazquez-Meza, M.E.; Galarde-López, M.; Carrillo-Quiróz, B.; Alpuche-Aranda, C.M. Antimicrobial resistance: One health approach. Vet. World 2022, 15, 743–749.
- Cella, E.; Giovanetti, M.; Benedetti, F.; Scarpa, F.; Johnston, C.; Borsetti, A.; Ceccarelli, G.; Azarian, T.; Zella, D.; Ciccozzi, M. Joining forces against antibiotic resistance: The one health solution. Pathogens 2023, 12, 1074.
- Philippot, L.; Griffiths, B.S.; Langenheder, S. Microbial community resilience across ecosystems and multiple disturbances. Microbiol. Mol. Biol. Rev. 2021, 85, e00026-20.
- Singer, A.C.; Shaw, H.; Rhodes, V.; Hart, A. Review of antimicrobial resistance in the environment and its relevance to environmental regulators. Front. Microbiol. 2016, 7, 1728.
- Founou, L.L.; Founou, R.C.; Essack, S.Y. Antibiotic resistance in the food chain: A developing country-perspective. Front. Microbiol. 2016, 7, 1881.
- Caneschi, A.; Bardhi, A.; Barbarossa, A.; Zaghini, A. The use of antibiotics and antimicrobial resistance in veterinary medicine, a complex phenomenon: A narrative review. Antibiotics 2023, 12, 487.
- Heuer, O.E.; Kruse, H.; Grave, K.; Collignon, P.; Karunasagar, I.; Angulo, F.J. Human health consequences of use of antimicrobial agents in aquaculture. Clin. Infect. Dis. 2009, 49, 1248–1253.
- Olmo, R.; Wetzels, S.U.; Armanhi, J.S.L.; Arruda, P.; Berg, G.; Cernava, T.; Cotter, P.D.; Araujo, S.C.; de Souza, R.S.C.; Ferrocino, I.; et al. Microbiome research as an effective driver of success stories in agrifood systems—A selection of Ccse studies. Front. Microbiol. 2022, 13, 834622.
- Dadgostar, P. Antimicrobial resistance: Implications and costs. Infect. Drug Resist. 2019, 12, 3903–3910.
- Aminov, R.I. The role of antibiotics and antibiotic resistance in nature. Environ. Microbiol. 2009, 11, 2970–2988.
- Samrot, A.V.; Wilson, S.; Preeth, R.S.S.; Prakash, P.; Sathiyasree, M.; Saigeetha, S.; Shobana, N.; Pachiyappan, S.; Rajesh, V.V. Sources of antibiotic contamination in wastewater and approaches to their removal—An overview. Sustainability 2023, 15, 12639.




