
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Ronald B. Brown | -- | 2278 | 2024-03-13 14:07:11 | | | |
| 2 | Peter Tang | Meta information modification | 2278 | 2024-03-14 03:51:00 | | |
Video Upload Options
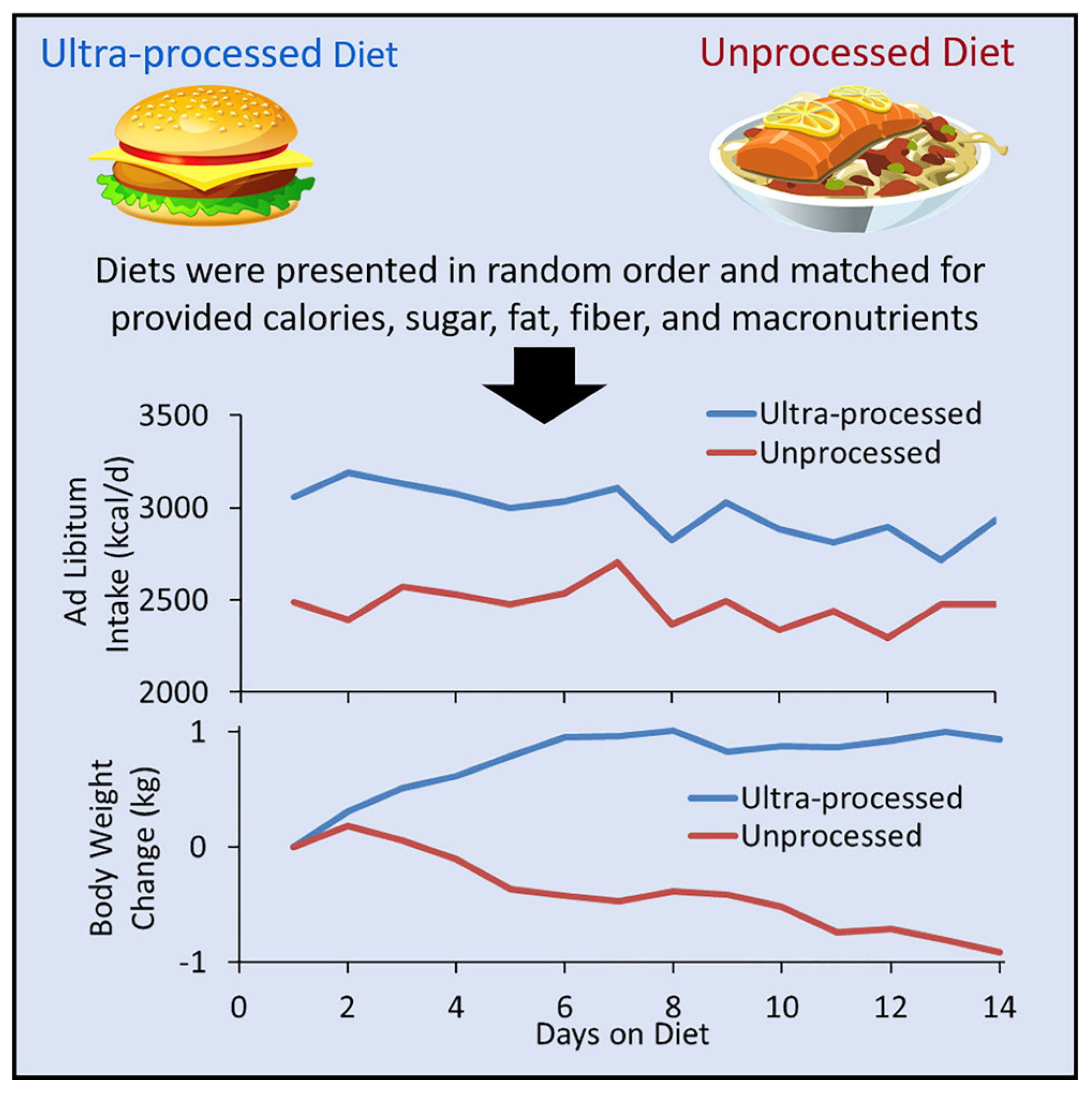
Sarcopenia, a condition of low muscle mass, is associated with aging, and sarcopenia in combination with excessive body fat causes sarcopenic obesity. Findings of improved health in people with a higher body mass index, known as the obesity paradox, are due to misclassifying healthy people as overweight according to height and body weight instead of according to fat mass and fat-free mass. Body fat infiltrates internal organs in aging adults as increasing levels of body fat are redistributed into the trunk, especially in the abdomen, while subcutaneous fat in the appendages decreases. Accuracy of body image perceptions can determine an individual’s control of body weight. Aging women can protect against sarcopenic obesity by increasing fat-free mass with resistance training and by lowering body fat levels with weight management knowledge and skills. Healthy dietary patterns are low in ultra-processed foods that stimulate excessive consumption of calories and increase body fat levels.
1. Introduction
2. Sarcopenic Obesity
3. The Obesity Paradox and Body Composition
4. Obesity Determinants
-
Influences of the neighborhood food environment, with easy access to unhealthy food, and no choices to select nutritious food.
-
Social network influence on obesity, including family preferences for food choices, low priority for exercise, and beliefs and perceptions of body image socially imposed on the aged that contribute to obesity.
-
Individual knowledge, attitudes, and beliefs behind lifestyle choices that cause obesity in older adults, including lack of awareness, personal attitudes, and job and familial duties as barriers to engaging in physical activities, as well as over-consumption behaviors leading to obesity in older people.
5. Weight Management Knowledge and Skills
6. Healthy Dietary Patterns
References
- WHO.Int. Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 23 February 2023).
- Cruz-Jentoft, A.J.; Bahat, G.; Bauer, J.; Boirie, Y.; Bruyère, O.; Cederholm, T.; Cooper, C.; Landi, F.; Rolland, Y.; Sayer, A.A.; et al. Sarcopenia: Revised European consensus on definition and diagnosis. Age Ageing 2018, 48, 16–31.
- Peng, Y.; Zhong, G.-C.; Zhou, X.; Guan, L.; Zhou, L. Frailty and risks of all-cause and cause-specific death in community-dwelling adults: A systematic review and meta-analysis. BMC Geriatr. 2022, 22, 725.
- Baumgartner, R.N. Body composition in healthy aging. Ann. N. Y. Acad. Sci. 2000, 904, 437–448.
- Samper-Ternent, R.; Al Snih, S. Obesity in Older Adults: Epidemiology and Implications for Disability and Disease. Rev. Clin. Gerontol. 2012, 22, 10–34.
- Fleischmann, E.; Teal, N.; Dudley, J.; May, W.; Bower, J.D.; Salahudeen, A.K. Influence of excess weight on mortality and hospital stay in 1346 hemodialysis patients. Kidney Int. 1999, 55, 1560–1567.
- Gruberg, L.; Weissman, N.J.; Waksman, R.; Fuchs, S.; Deible, R.; Pinnow, E.E.; Ahmed, L.M.; Kent, K.M.; Pichard, A.D.; Suddath, W.O.; et al. The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: The obesity paradox? J. Am. Coll. Cardiol. 2002, 39, 578–584.
- Bosello, O.; Vanzo, A. Obesity paradox and aging. Eat. Weight Disord. 2021, 26, 27–35.
- Ponti, F.; Santoro, A.; Mercatelli, D.; Gasperini, C.; Conte, M.; Martucci, M.; Sangiorgi, L.; Franceschi, C.; Bazzocchi, A. Aging and Imaging Assessment of Body Composition: From Fat to Facts. Front. Endocrinol. 2019, 10, 861.
- Chang, C.-S.; Liu, I.T.; Liang, F.-W.; Li, C.-C.; Sun, Z.-J.; Chang, Y.-F.; Chao, T.-H.; Wu, C.-H. Effects of age and gender on body composition indices as predictors of mortality in middle-aged and old people. Sci. Rep. 2022, 12, 7912.
- Karastergiou, K.; Smith, S.R.; Greenberg, A.S.; Fried, S.K. Sex differences in human adipose tissues—The biology of pear shape. Biol. Sex Differ. 2012, 3, 13.
- Janssen, I.; Heymsfield, S.B.; Wang, Z.; Ross, R. Skeletal muscle mass and distribution in 468 men and women aged 18–88 yr. J. Appl. Physiol. 2000, 89, 81–88.
- Musolino, E.A.; O’Connor, B.P.; Cioe, J.D. Bigger isn’t always better: An exploration of social perception bias against high levels of muscularity in women. J. Soc. Psychol. 2022, 162, 523–539.
- Henderson, G.C.; Dhatariya, K.; Ford, G.C.; Klaus, K.A.; Basu, R.; Rizza, R.A.; Jensen, M.D.; Khosla, S.; O’Brien, P.; Nair, K.S. Higher muscle protein synthesis in women than men across the lifespan, and failure of androgen administration to amend age-related decrements. FASEB J. 2009, 23, 631–641.
- Roth, S.M.; Ivey, F.M.; Martel, G.F.; Lemmer, J.T.; Hurlbut, D.E.; Siegel, E.L.; Metter, E.J.; Fleg, J.L.; Fozard, J.L.; Kostek, M.C.; et al. Muscle size responses to strength training in young and older men and women. J. Am. Geriatr. Soc. 2001, 49, 1428–1433.
- Valenzuela, P.L.; Santos-Lozano, A.; Barrán, A.T.; Fernández-Navarro, P.; Castillo-García, A.; Ruilope, L.M.; Ríos Insua, D.; Ordovas, J.M.; Ley, V.; Lucia, A. Joint association of physical activity and body mass index with cardiovascular risk: A nationwide population-based cross-sectional study. Eur. J. Prev. Cardiol. 2021, 29, e50–e52.
- Tomiyama, A.J.; Carr, D.; Granberg, E.M.; Major, B.; Robinson, E.; Sutin, A.R.; Brewis, A. How and why weight stigma drives the obesity ‘epidemic’ and harms health. BMC Med. 2018, 16, 123.
- Penney, T.L.; Kirk, S.F. The Health at Every Size paradigm and obesity: Missing empirical evidence may help push the reframing obesity debate forward. Am. J. Public Health 2015, 105, e38–e42.
- Lee, A.; Cardel, M.; Donahoo, W.T. Social and Environmental Factors Influencing Obesity. In Endotext; Feingold, K.R., Anawalt, B., Blackman, M.R., Boyce, A., Chrousos, G., Corpas, E., de Herder, W.W., Dhatariya, K., Dungan, K., Hofland, J., et al., Eds.; MDText.com, Inc.: South Dartmouth, MA, USA, 2000.
- Medvedyuk, S.; Ali, A.; Raphael, D. Ideology, obesity and the social determinants of health: A critical analysis of the obesity and health relationship. Crit. Public Health 2018, 28, 573–585.
- Sainsbury, A.; Hay, P. Call for an urgent rethink of the ‘health at every size’ concept. J. Eat. Disord. 2014, 2, 8.
- CDC. Adult Obesity Facts. Available online: https://www.cdc.gov/obesity/data/adult.html (accessed on 27 February 2023).
- Lakerveld, J.; Mackenbach, J. The Upstream Determinants of Adult Obesity. Obes. Facts 2017, 10, 216–222.
- Chumpunuch, P.; Jaraeprapal, U. The social determinants of health influencing obesity for the aged in the Pakpoon community context: A qualitative study. Int. J. Nurs. Sci. 2022, 9, 211–221.
- Bouzas, C.; Bibiloni, M.D.M.; Tur, J.A. Relationship between Body Image and Body Weight Control in Overweight ≥55-Year-Old Adults: A Systematic Review. Int. J. Environ. Res. Public Health 2019, 16, 1622.
- Stuckler, D.; McKee, M.; Ebrahim, S.; Basu, S. Manufacturing epidemics: The role of global producers in increased consumption of unhealthy commodities including processed foods, alcohol, and tobacco. PLoS Med. 2012, 9, e1001235.
- Martínez Steele, E.; Baraldi, L.G.; Louzada, M.L.; Moubarac, J.C.; Mozaffarian, D.; Monteiro, C.A. Ultra-processed foods and added sugars in the US diet: Evidence from a nationally representative cross-sectional study. BMJ Open. 2016, 6, e009892.
- Hall, K.D.; Ayuketah, A.; Brychta, R.; Cai, H.; Cassimatis, T.; Chen, K.Y.; Chung, S.T.; Costa, E.; Courville, A.; Darcey, V.; et al. Ultra-Processed Diets Cause Excess Calorie Intake and Weight Gain: An Inpatient Randomized Controlled Trial of Ad Libitum Food Intake. Cell. Metab. 2019, 30, 67–77.




