2. Sarcopenic Obesity
Physical changes associated with aging include reduced bone mass, increased hypervolemic retention of extracellular fluids, and sarcopenia, a condition of reduced skeletal muscle mass due to muscle atrophy, reduced muscle strength, and low quality of muscle (e.g., changes in muscle architecture and composition from fat infiltration), all of which increase the burden of health care costs [
5]. These physical changes are associated with lower nutritional status and physical disability which accelerate “molecular and cellular damage overtime”, according to the WHO definition of biological aging [
1]. Furthermore, changes associated with lower nutritional status and physical disability, including unintended weight loss, low energy, exhaustion, slow walking gait, and weak grip strength, contribute to a state of
frailty with increased risk of all-cause and cause-specific mortality [
6]. Decreased quality of life and increased comorbid conditions occur most often in older adults who have both sarcopenia and excessive body fat—known as sarcopenic obesity [
7]. Accurate measurements of body fat and fat-free mass in sarcopenic obesity can be obtained with dual-energy X-ray absorptiometry.
Excess body weight in older adults is associated with a higher prevalence of cardiovascular disease, several cancers, metabolic disease, and many other medical conditions [
8]. A study published in 2000 analyzed obesity, sarcopenia, and sarcopenic obesity by age in the New Mexico Elder Health Survey and New Mexico Aging Process Study [
7]. Sarcopenia prevalence, independent of body fat levels, increased from about 15% in adults aged 60 to 69 years to about 40% in adults older than 80 years. Sarcopenic obesity increased from about 2% in adults aged 60 to 69 years to about 10% in adults over 80 years. The study also found that the prevalence of people having obesity without sarcopenia decreased with aging within an approximate range of 55% to 30%. However, the researchers suggested that rather than losing body fat with age, obese people are more likely to lose muscle mass as they age, which causes sarcopenic obesity.
3. The Obesity Paradox and Body Composition
In 1999, Fleischmann et al. observed protective health benefits in overweight people, including higher survival rates among patients in hemodialysis who weighed more than patients classified as normal weight or lower according to the Body Mass Index (BMI) which is based on height and body weight [
9]. Similarly, researchers studying myocardial infarction in patients with coronary artery disease also found that patients who were classified as obese or overweight by BMI standards had lower mortality rates at one year and fewer in-hospital complications compared to patients classified as normal weight, which the researchers described with the coined term
obesity paradox [
10].
Based on published findings on the obesity paradox, recent research continues to search for answers explaining how excessive body weight in aging protects health [
11]. Nevertheless, the obesity paradox in older adults is most likely an artifact of information bias due to overestimating adiposity based on body weight and height, as measured by the BMI, instead of measuring specific body fat and fat-free mass levels. Consequently, the BMI may miscategorize healthy people as overweight for their height because they carry more protective fat-free mass such as skeletal muscle, bone, and other healthy organ and cellular tissue.
Body fat tends to infiltrate internal organs in aging adults as increasing levels of body fat are redistributed into the trunk, especially the abdomen, while subcutaneous fat in the appendages decreases [
14]. A recent study in Taiwan investigating associations of body composition, age, and gender with all-cause mortality measured participants’ fat mass index (FMI), fat-free mass index (FFMI), skeletal muscle mass index (SMMI), and visceral-fat-area index (VFAI) [
15]. In adults aged 65 years, the FFMI and SMMI were found to have a negative association with all-cause mortality in the total group, in both males and females, while the FMI and VFAI were only positively associated with mortality in females.
Another lesser-known paradox related to the obesity paradox, coined here as the
gender body fat paradox, implies that healthy females normally carry a higher amount of body fat than healthy males, which is implied from higher body fat percentages in women compared to men [
16]. Once again, this is likely an artifact of information bias when calculating body fat percentages while failing to account for differences in fat-free mass between average females and males [
17]. Proportions of fat-free mass from skeletal muscle in overall body weight are higher in average males than females, thereby mathematically lowering the calculation of body fat percentages in males. In other words, even allowing for additional fat in reproductive tissue, women generally have higher body fat percentages compared to men mostly because women have lower muscle mass levels in proportion to their body weight.
Interestingly, healthy females who compete in physique events attain low body fat levels and use resistance exercise training to increase skeletal muscle levels, displaying muscle and body fat proportions for their body weight approaching the proportions of male athletes [
18]. This is not surprising when considering that higher levels of protein synthesis in skeletal muscle were found in women compared to men at young and older ages [
19], and young and older women have the same muscle volume response from strength training as young and older men [
20].
Figure 1 shows Charmion, a strongwoman from the late 19th century, before modern performance-enhancing drugs became popular.
Unfortunately, cultural stereotypes continue to associate muscle mass in females with masculinity [
18], which may discourage females, especially younger females, from achieving levels of skeletal muscle mass that could protect their health as they advance in age. Additionally, cultural stereotypes that associate higher body fat levels with females may also support yet another paradox, the
fat but fit paradox which states that “high cardiorespiratory fitness (CRF) might mitigate the detrimental effects of excess body weight on cardiometabolic health” [
23]. Based on the association of the higher BMI levels observed in healthy people, the evidence is insufficient to suggest that one can be fat and still be fit, mainly because, due to the lack of body composition assessments as previously described, BMI levels are biased and overestimate a healthy individual’s level of body fat.
At the other extreme, collateral harm to heavier people from society’s stigmatization of excessive body weight and body fat [
24] has spawned movements such as Healthy At Every Size (HAES) and the fat acceptance movement [
25]. All people at every physical size have a right to be treated with fairness and respect without prejudgment by others, which is among the aims of HAES. Fat acceptance social movements emphasize the need to establish a healthy balance in how society views and handles the epidemic of overweight and obesity, which is as much a societal problem as a medical one, as it has many determinants beyond the control of individuals [
26]. By contrast, the biomedical and health science model of the cause of obesity blames an individual’s “excess caloric consumption and lack of physical activity” as the principal causes of the pathophysiological mechanisms and adverse health outcomes associated with obesity [
27]. Furthermore, controversy arises if the public views fat acceptance as a movement that denies or disparages credible evidence-based health risks associated with obesity and overweight [
28].
4. Obesity Determinants
According to adult obesity facts published by the U.S. Centers for Disease Control and Prevention (CDC) [
29], U.S. obesity prevalence in 2017 was 41.9%, which increased from 30.5% in 1999–2000. During the same time period, severe obesity prevalence also increased from 4.7% to 9.2%. Obesity-related conditions “are among the leading causes of preventable, premature death”, and include heart disease, stroke, type 2 diabetes, and certain cancers. Estimated in 2019 dollars, the annual medical cost of obesity in the United States in 2017 was approximately $173 billion.
The two social determinants most consistently associated with obesity are socio-economic status (SES) and inequality [
30]. Higher obesity rates are found in adults with lower SES in high-income countries and in countries with more social inequality in general. In addition to social determinants, individual and environmental determinants also play a role in the development of obesity [
26]. Specific to the aging population, a qualitative study investigating determinants of health that affect obesity in older people found three main themes within a community context [
31]:
-
Influences of the neighborhood food environment, with easy access to unhealthy food, and no choices to select nutritious food.
-
Social network influence on obesity, including family preferences for food choices, low priority for exercise, and beliefs and perceptions of body image socially imposed on the aged that contribute to obesity.
-
Individual knowledge, attitudes, and beliefs behind lifestyle choices that cause obesity in older adults, including lack of awareness, personal attitudes, and job and familial duties as barriers to engaging in physical activities, as well as over-consumption behaviors leading to obesity in older people.
5. Weight Management Knowledge and Skills
The accuracy of an individual’s body image perceptions can determine an individual’s control of body weight. “Overweight people misperceiving their weight were observed to be less likely to desire or pursuit weight control than accurate weight perceivers” [
2]. Because weight gain with increasing age is associated with increased risk of disease and comorbid conditions, strengthening accuracy of body image and perception of overweight in older people “may contribute to more effective health practices and higher quality of life”. Of some concern, a systematic review of studies in aging adults suggests that “aging is associated with a decrease in weight concerns and lower overweight perception” [
2]. Interestingly, the systematic review also found that women over 55 years of age had less concern for losing weight than similarly aged men, which is reversed in younger men who have less concern for losing weight than younger women.
6. Healthy Dietary Patterns
Even if one calculates the exact quantity of calories required for weight management, other factors that influence food intake must be considered. One such factor is the influence of the quality of food consumed. Dietary patterns can range from providing predominantly whole unprocessed natural foods with a high nutritional value, which contribute to health, to providing highly refined ultra-processed foods with a lower nutritional value, which increase illness and disease risks. The following research shows that consuming highly processed food is also associated with weight gain and biological aging.
The popularity of ultra-processed foods that are high in fat, sugar, and salt coincides with the worldwide rise in obesity [
49], and ultra-processed foods currently provide the majority of energy from calories, 57.9%, in the U.S. diet [
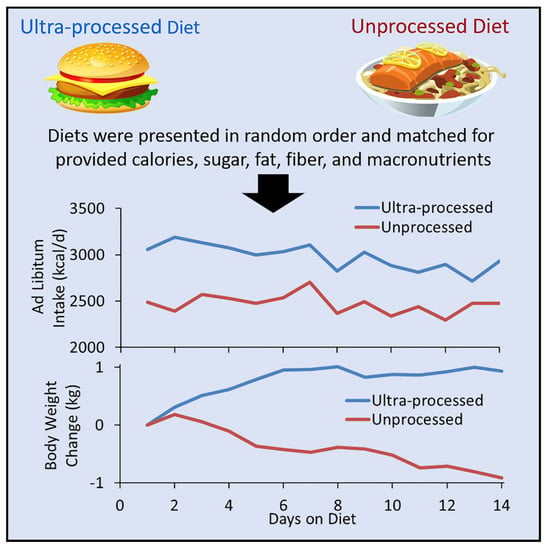
50]. A 2019 randomized controlled trial sponsored by the U.S. National Institutes of Health provided twenty adults with three meals a day and snacks on a diet consisting entirely of either ultra-processed foods or unprocessed foods [
51]. After two weeks, the participants switched diets for an additional two weeks. Each diet contained similar amounts of calories, macronutrients, fiber, sodium, and sugar, and participants were allowed to eat any amount of food they desired. Results showed that participants eating the ultra-processed diet consumed approximately 500 additional daily calories compared to those consuming the unprocessed diet, and participants on the ultra-processed diet gained an average of two pounds of body weight over two weeks. Weight gain was reversed when participants consumed the unprocessed diet, with losses of approximately two pounds of body weight over two weeks.
Figure 2 shows body weight changes in participants when following ultra-processed and unprocessed diets during the trial. Importantly, participants reported favorable taste and satiety on both diets. The implications of the results of this controlled experiment are that ultra-processed food is flavorful and satisfying but stimulates people to overeat and gain excessive body weight, while unprocessed food provides flavor and satisfaction with smaller amounts of food without inducing people to overeat. Although both diets were matched for energy density; fiber; and macronutrients, i.e., calories, protein, fat, and carbohydrates, the diets were not matched for overall nutrient density, including vitamins, minerals, enzymes, phytochemicals, etc. as they naturally occur in whole foods The study’s results may be causatively linked to greater overall nutrient density in unprocessed food compared to ultra-processed food, implying that consumption of lower amounts of natural, whole, unprocessed food is sufficient for adequate nourishment, but further investigations are warranted.
Figure 2. Body weight change with ultra–processed and unprocessed diets [
51].