Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Reema Tayyem | -- | 2763 | 2024-03-04 08:49:56 | | | |
| 2 | Lindsay Dong | + 3 word(s) | 2766 | 2024-03-04 09:57:41 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Zamzam, S.; Said, S.; Yaghi, J.; Faisal, F.S.; Hassan, D.; Abdul Majeed, S.; Al Rajabi, A.; Tayyem, R. Dietary Patterns of Breast Cancer in Middle East. Encyclopedia. Available online: https://encyclopedia.pub/entry/55801 (accessed on 13 March 2026).
Zamzam S, Said S, Yaghi J, Faisal FS, Hassan D, Abdul Majeed S, et al. Dietary Patterns of Breast Cancer in Middle East. Encyclopedia. Available at: https://encyclopedia.pub/entry/55801. Accessed March 13, 2026.
Zamzam, Syed, Suad Said, Juman Yaghi, Fathima Sahar Faisal, Dana Hassan, Safa Abdul Majeed, Ala Al Rajabi, Reema Tayyem. "Dietary Patterns of Breast Cancer in Middle East" Encyclopedia, https://encyclopedia.pub/entry/55801 (accessed March 13, 2026).
Zamzam, S., Said, S., Yaghi, J., Faisal, F.S., Hassan, D., Abdul Majeed, S., Al Rajabi, A., & Tayyem, R. (2024, March 04). Dietary Patterns of Breast Cancer in Middle East. In Encyclopedia. https://encyclopedia.pub/entry/55801
Zamzam, Syed, et al. "Dietary Patterns of Breast Cancer in Middle East." Encyclopedia. Web. 04 March, 2024.
Copy Citation
Breast cancer (BC) is the most predominant malignancy in Arab women in the Middle East. Most dietary patterns (DPs) such as the Dietary Approaches to Stop Hypertension, Mediterranean, Plant-based and Paleolithic diets are identified to decrease the probability of BC by being rich sources of fiber, healthy fats, and vitamins and minerals. However, there are few DPs that increase the risk of BC, because of the existence of foods such as unhealthy fats, low fiber, sugars, and fried foods in those patterns which contribute to increasing the risk factors associated with BC.
breast cancer
dietary pattern
middle east
1. Introduction
Breast Cancer (BC) is diagnosed in 2.3 million women, ranking 1st in terms of new cases, and 4th in terms of associated mortality, accounting for 685,000 deaths as reported by World Health Organization’s GLOBOCAN, thereby emerging as a predominant cancer globally as of 2020 [1][2]. Additionally, it is also reported in GLOBOCAN, as of 2020, even in the Middle East Region, BC is the leading type of cancer in women [3][4][5][6][7][8][9][10][11][12][13][14][15][16][17]. The reason for such increase in cases is attributed partly to the advancement in medical care resulting in better diagnosis and to the shift in women’s lifestyle to more westernized, characterized by dietary habits, late marriages and pregnancy, lower rate of reproduction, smoking, and the use of contraceptives and hormone replacement therapies [18].
BC is described as a disease with an unusual growth of breast cells. When these cells grow out of control, they form tumors which can be benign and are often not life-threatening. Once these cells become malignant, the cells spread to nearby breast tissues, lymph nodes, and other organs through metastasis, resulting in an increased risk of fatality [2].
The likelihood of BC occurrence is predisposed by a variety of modifiable and non-modifiable risk factors. Non-modifiable risk factors include gender (females face a heightened risk of BC development, with men accounting for only 0.5–1% of cases), age (with a higher incidence in those over 40 years), family history of BC, and genetic mutations in the BRCA1, BRCA2, and PALB-2 genes. On the other hand, the modifiable risk factors may include alcohol consumption, tobacco use, exposure to radiation, body mass index (BMI), physical inactivity, unhealthy diet, oral contraceptives, and high stress [2][19][20]. Dietary factors alone account for 35% of the risk factors that can promote BC [19].
Dietary pattern (DP) is defined as the composition of the diet, the foods, food groups, and nutrients it contains, as well as how frequently and how much of each is regularly consumed [21]. DP grouping and classification are determined by the degree of similarity between the stressed or limited/restricted food groups, macronutrient profiles, or both. The most common DP include DASH (Dietary Approaches to Stop Hypertension)-style, Mediterranean-style, pescetarian, ovo/lacto-vegetarian, vegan, low-fat, very low-fat, low-carbohydrate, Paleolithic (Paleo) and very low-carbohydrate/ketogenic patterns [22].
2. Dietary Patterns of Breast Cancer in the Middle East
2.1. Mediterranean Dietary Pattern
The Mediterranean diet (MD) advocates plant-centric foods, such as whole grains, fruits, legumes, vegetables, and healthful fats which are obtained from sources like fatty fish, nuts, and olive oil. It limits the intake of saturated fats, vegetable oils, red meat, and processed foods [23].
A case-control study by Sadeghi et al. revealed a noteworthy inverse correlation relating to MD and BC. Notably, a 57% reduction in the likelihood of developing BC was observed following MD (95%CI 0.28–0.67) [24]. Similarly, 55% BC risk reduction was observed in another Iranian study (95%CI 0.21–0.94) [25]. Postmenopausal women who followed MD displayed a 63–76% reduction in BC odds risk with no statistical significance among premenopausal women [24][25]. The results from these Middle Eastern countries are similar to other countries where the risk was decreased by 8–18% when adhering to MD [26][27][28]
The Mediterranean DP is a rich source of many nutrients that have been showed to decrease the risk of BC. Vitamin C helps strengthen immunity, Vitamin E, and Carotenoids exert chemo-preventive effects and omega 3 fatty acids reduce BC cell production by restraining the epidermal growth factor receptor [29]. Vitamin D, B Vitamins, phytochemicals, and essential minerals like calcium, magnesium and zinc also help to decrease the risk of BC. All of these nutrients help to mitigate inflammation, oxidative damage, and angiogenesis, all implicated in disease pathogenesis as demonstrated by scientific evidence [23][29].
In conclusion, a growing body of evidence from multiple Middle Eastern countries supports that following Mediterranean DP is correlated to a lower likelihood of developing BC. The MD’s diverse dietary components, rich in antioxidants and anti-inflammatory properties, exhibit pleiotropic, multi-target effects, positioning them as potential agents for BC prevention.
2.2. Plant-Based Dietary Pattern
A case-control study done in Iran established the association between adhering to indices of plant-based diet and reducing the odds of BC [30]. Subjects with the highest plant dietary indices (PDI) score had 67% lower odds of BC compared to those in the lowest quartile (95%CI 0.22 to 0.5). Furthermore, women with the utmost devotion to the healthy PDI were 36% less likely to develop BC compared to women with unhealthy PDI that had 2.23 times increased odds of BC (95%CI 1.48–3.36) [30]. This is similar to another study done by Sasanfar et al., that reported BC risk reduced by 37% (95%CI 0.43–0.93) in people who followed healthy PDI compared to unhealthy PDI who reported no significant association [31]. Even in studies from other than Middle East countries, participants with better devotion to plant dietary indices, and healthy plant dietary indices had a lesser risk of developing BC, through a powerful reverse association between healthy PDI and BC detected with Estrogen receptor (ER)-negative tumours [32][33][34].
However, a study in Iran failed to capture any association and is attributed to a lower average fruit and vegetable intake in the region compared to other regions and the suggestions of the Food and Agriculture Organization (FAO) and WHO [35]. The adequate intake of dietary fiber can cut the danger of BC by 12% [36]. In the Middle East, whole grains, the primary source of dietary fiber are consumed less than the recommended daily intake of 50 g [37].
In conclusion, studies in the Middle East outlined the reverse correlation between plant-based DPs and BC risk [30][31]. In particular, the healthy plant dietary indices showed the strongest association, and this is relevant to the elevated ingestion of healthy vegetables, grains, and fruits with the lower ingestion of meats, meat products, refined sugars, juices, and sweets. However, the number of studies done in the Middle East was limited. Advanced studies are needed across other countries in the Middle East.
2.3. Prudent Dietary Pattern
Within the Middle East, one study done in Iran, measured for the correlation between prudent diet and gene expression causing metastasis in BC. According to Foroutan-Ghaznai et al., a prudent diet is recognized by spices, plant-based oils, low-fat dairy, and seafood. Additionally, it is high in fruits, vegetables, legumes, poultry, and whole grains [38].
In an Iranian study, the relationship linking the prudent DP and the expression of genes RhoA (Ras homolog family member-A) and ROCK (Rho-associated kinase) which are pro-metastatic in BC was examined. Expressions of genes RhoA and ROCK were reduced extensively by 74% (95%CI: 0.09–0.95) and 71% (95%CI: 0.08–0.84), respectively, by strictly following Prudent Diet [39]. This significant reduction is observed even in global studies, including several meta-analyses which also show that prudent diet lowers BC risk by 11% [40][41][42].
It is found that the intake of spices such as turmeric and saffron, which contain curcumin and crocetin respectively, have inhibitory effects on the RhoA and ROCK gene expression. Additionally, a prudent DP, which is rich in seafood, is high in omega 3 polyunsaturated fatty acids. These PUFA’s are known to transport the RhoA back into the cytoplasm from the cell membrane surface, thereby downregulating the activity of RhoA and ROCK [39]. Fiber and antioxidants such as polyphenols glycosylate, and indoles found in fruits, vegetables, and whole grains can lessen BC risk by inhibiting inflammation and reducing oxidative through the inducing of detoxifying enzymes, and fiber binding with estrogens, leading to improved elimination thereby reducing the concentration of estrogen in the plasma [43][44][45].
2.4. Western Dietary Pattern
Western DP is illustrated by elevated intake of soft drinks, hydrogenated fat, animal fat, sugar, fast food, refined cereals, sweets, meat, and processed meat as reported in two Iranian studies [39][46]. Foroutan-Ghaznavi et al. found that the overexpression of the gene RhoA in patients who followed a western DP was significant (OR: 3.15) and this may increase cell proliferation (Figure 1) [39]. Another study assessed the correlation linking Western DP and two subtypes of BC, namely ILC (invasive lobular carcinoma and IDC (invasive ductal carcinoma).
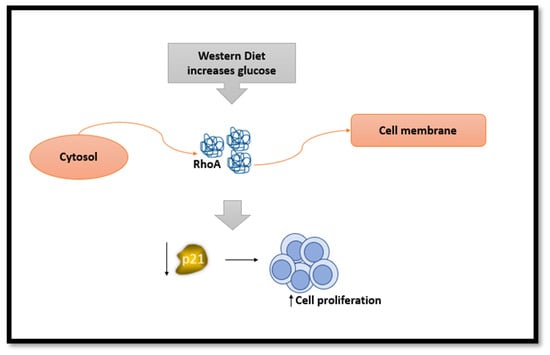
Figure 1. The effect of Western diet on RhoA gene and its consequences.
Increased devotion to the western diet was substantially and positively associated with a heightened risk of IDC by 63 percent. However, no substantial association was reflected between ILC risk and western diet (OR: 1.63; 95%CI: 0.63–3.25). Similar outcomes were observed when the results were classified based on menopausal status [46]. Furthermore, global studies have found similar conclusions to western diet with 14% increased BC risk [41][47] could be due to consumption of high amounts of red and processed meat daily (Figure 2) [42].
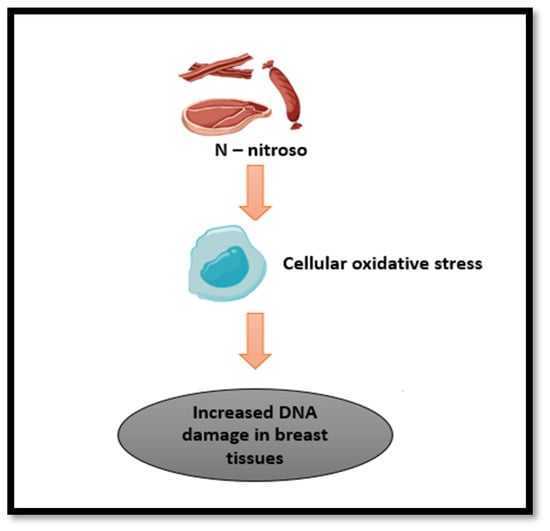
Figure 2. The effect of carcinogens found in processed/cured meat.
One of the possible mechanisms mentioned by Foroozani et al., is that N-nitroso components found in the western diet upsurge cancer progression through an increase in cellular oxidative stress leading to increased damage to DNA, affecting breast tissues (Figure 2). Another possibility is that western diet can alter gut microbiota, driving to decrease in the beneficial short chain fatty acids formation [38][46]. Another mechanism related to elevated glucose levels in a laboratory setting found RhoA moved from the cytosol to the cell membrane, indicating a decrease in the levels of p21. p21 reduction promotes the cells to grow and multiply more rapidly (Figure 1).
Also, the body’s growth factor, IGF-1, might activate a specific pathway (RhoA/ROCK) through a series of signals (PI3K/Akt/mTOR). This activation could aid in the increased growth of breast tumors [39].
2.5. Unhealthy Dietary Pattern
An unhealthy DP is high in sugars, processed juices, soft drinks, French fries, potato chips, boiled potato, sweets, desserts, nuts, saturated and hydrogenated fats, solid oils, red and processed meat, mayonnaise, and salt intake as reported by two Iranian case-control studies [48][49]. These dietary choices align with a pattern that is commonly associated with poor nutritional quality, excess calorie intake, and an imbalance of essential nutrients.
Two case-control studies done in hospitals found a significant correlation between unhealthy DP and an increased risk of BC among Iranian women (OR:7.78; 95%CI: 2.31–26.22; OR: 2.21; 95%CI: 1.04, 4.690; p-trend = 0.5) [48][49]. Furthermore, only among post-menopausal women, unhealthy DP had a significant association with the risk of BC (OR: 3.56; 95%CI: 1.16–10.95; p-trend = 0.008) [48].
The possible mechanism for the increased BC risk because of following the unhealthy DP could be attributed to the presence of oncogenic compounds. Carcinogens such as heterocyclic amines, polycyclic aromatic and N-nitroso are found in processed/cured meat and unprocessed meat cooked at high temperatures (Figure 2). They have been confirmed to raise the risk of breast tumors in animal models [48][49]. Foods high in sugar and fat increase blood glucose and insulin. Insulin is known to induce cell division and, hence, can cause cell proliferation and growth of tumors. It also inhibits the production of a protein that binds to sex hormones, known as sex hormone binding globulin, thereby increasing free estrogen levels [48].
2.6. Healthy Dietary Pattern
A healthy DP is portrayed by the utilization of foods that are nutrient-dense and provide essential vitamins, minerals, and other beneficial compounds. According to two studies done in Iran, a healthy DP is considered to be high in fruits, vegetables, legumes, seeds and nuts, fish and seafood, whole grains, soya, olives, olive oils, vegetable oils, low fat dairy products, condiments, pickles, poultry, and organ meat along with low intake of salt [48][49].
In a 2014 case-control study done by Karimi et al., it was found that BC risk decreased by 75% in the highest tertile compared to lowest tertile when following a healthy DP after adjusting for all confounders [49]. Unfortunately, Heidari et al., found no correlation (95%CI: 0.36–1.89) between healthy DP and the risk of BC after adjusting for confounders [48].
It is suggested that the cancer-protective effect of a healthy DP is correlated with the high intake of fiber and the diet being high in foods containing vitamins and antioxidants [49]. Fibers bind to estrogen, reducing its absorption and preventing its binding to the nuclear receptor ERα. This, in turn, inhibits cell multiplication. Furthermore, it also binds with bile acids which are responsible for promoting cell proliferation and reducing the risk of mutations and cancers [38].
2.7. Ketogenic Dietary Pattern
A well-known high-fat, low-carb diet first utilized as a treatment for diseases, including obesity and epilepsy, is the ketogenic diet (KD). KD affects the energy metabolism of cancer cells, as shown in multiple studies done in Middle East which revealed that a ketogenic diet might decrease the progression of tumors in people with BC [50][51][52][53]. Studies support the effectiveness of the ketogenic diet and metabolically supported chemotherapy in treating aggressive cancer types like triple-negative breast cancer. Triple-negative breast cancer is characterized by the lack of receptors for progesterone, estrogen and human epidermal growth factor receptor 2 (HER2), contributing to 20% of breast cancers [53].
The metabolism of fatty acids and the production of ketone bodies are suggested to prevent the development and survival of cancer cells [53]. KD may help prevent BC by reducing appetite, calories, and glycolytic activity. Additionally, KD has anti-inflammatory effects. This may inhibit the growth of tumors and control apoptosis via insulin- or IGF-I-dependent cell signaling pathways [50][51]. KD being low in carbohydrates, lowers the glycolytic activity leading to decreased availability of lactate, thereby decreasing acidity of the tumor microenvironment, hence decreasing its biosynthesis. ALP, which is a negative marker in BC, is reduced in KD, suggesting potential benefit in impeding metastatic progression [50].
In conclusion, KD may improve the quality of life of BC, but making conclusive results on the correlation between ketogenic diets and the occurrence of BC in the Middle East is difficult owing to the limited availability of studies in the Middle Eastern Region.
2.8. Pro-Inflammatory Dietary Pattern
Pro-inflammatory DP is categorized by the ingestion of processed/cured meat, red meats, butter, eggs, fries, dairy, refined grains, tubers, pizza, mayonnaise, snack, confections, desserts, trans fats and oils, and soft drinks as reported by Ghanbari et al. [54]. Six studies have been done in the Middle East to assess the association between BC risk with pro-inflammatory DP using dietary inflammatory index scores for participants. The Iranian case-control study reported that a higher food-based empirical dietary inflammatory index score (FDII score) was significantly associated with increased BC risk (OR: 2.38; 95%CI: 1.23–4.59) where participants in the fourth quartile of FDII score had 2.8 times higher risk of breast cancer compared to the first quartile [54]. Similar results were observed in three other Iranian case-control studies done by Vahid et al., Jalali et al., and Gholamalizadeh et al. who found that dietary inflammatory index (DII) was significantly high, and the risk of BC increased significantly when subjects followed a proinflammatory diet with odds ratio ranging from 2.64 to 7.24 with a positive trend [55][56][57].
2.9. Paleolithic Dietary Pattern
The Paleolithic diet (PD) is a dietary approach that assumes our bodies are better adapted to the types of foods consumed during that Paleolithic period. Foods categorized under this DP are vegetables, fruits, lean meats, fish, nuts, and seeds, while eliminating or limiting dairy products, grains, legumes, refined sugar, and processed/cured foods with an emphasis on whole, unprocessed foods similar to a pre-agriculture period [58][59].
A study done in Iran by Sohouli et al. found there was a 76% decreased risk of BC when the highest quartile was compared to the lowest quartile for PD score in all women (95%CI 0.13–0.53). Furthermore, a noteworthy reduction in the risk of this cancer was viewed in premenopausal by 71% and post-menopausal by 83% [58]. Although a single study was done in the Middle East, studies done in other global countries had similar reductions in BC risk [60][61].
2.10. Dietary Approaches to Stop Hypertension (DASH) Dietary Pattern
The DASH diet, short for Dietary Approaches to Stop Hypertension, a powerful tool to manage and prevent high blood pressure is now being found to be effective in preventing cancer [62]. This balanced eating plan emphasizes on fruits, vegetables, low-fat dairy, legumes, nuts, wholegrain and foods low in saturated fat, sodium, red and processed/cured meat, and sweetened drinks [62][63].
A case-control study conducted by Heidari et al. assessed the relationship between four DASH diet indices and the risk of BC in Iranian women. Dixon’s Index scored eight food groups and a nutrient whereas Mellen’s Index evaluated 9 nutrient intakes. Fung’s Index scored eight food groups and sodium and lastly Günther’s Index assessed ten food components. Gunther’s DASH index lowered the odds of BC by 52% in the highest quintile, compared to lowest quintile and Mellen’s lowered it by 50% indicating significant association (95%CI 0.25–0.93 and 0.62–0.97) of both these indices in lowering the risk of BC.
References
- Global Cancer Observatory: Breast Cancer Fact Sheet; World Health Organization, International Agency for Research on Cancer: Lyon, France, 2020.
- Breast Cancer. Available online: https://www.who.int/news-room/fact-sheets/detail/breast-cancer (accessed on 18 November 2023).
- Global Cancer Observatory—Syrian Arab Republic Fact Sheet; World Health Organization, International Agency for Research on Cancer: Lyon, France, 2020.
- Global Cancer Observatory: Bahrain Fact Sheet; World Health Organization, International Agency for Research on Cancer: Lyon, France, 2020.
- Global Cancer Observatory: Egypt Fact Sheet; World Health Organization, International Agency for Research on Cancer: Lyon, France, 2020.
- Global Cancer Observatory: Gaza Strip and West Bank Fact Sheet; World Health Organization, International Agency for Research on Cancer: Lyon, France, 2020.
- Global Cancer Observatory: Iraq Fact Sheet; World Health Organization, International Agency for Research on Cancer: Lyon, France, 2020.
- Global Cancer Observatory: Islamic Republic of Iran Fact Sheet; World Health Organization, International Agency for Research on Cancer: Lyon, France, 2020.
- Global Cancer Observatory: Jordan Fact Sheet; World Health Organization, International Agency for Research on Cancer: Lyon, France, 2020.
- Global Cancer Observatory: Kuwait Fact Sheet; World Health Organization, International Agency for Research on Cancer: Lyon, France, 2020.
- Global Cancer Observatory: Lebanon Fact Sheet; World Health Organization, International Agency for Research on Cancer: Lyon, France, 2020.
- Global Cancer Observatory: Oman Fact Sheet; World Health Organization, International Agency for Research on Cancer: Lyon, France, 2020.
- Global Cancer Observatory: Qatar Fact Sheet; World Health Organization, International Agency for Research on Cancer: Lyon, France, 2020.
- Global Cancer Observatory: Saudi Arabia Fact Sheet; World Health Organization, International Agency for Research on Cancer: Lyon, France, 2020.
- Global Cancer Observatory: Turkey Fact Sheet; World Health Organisation, International Agency for Research on Cancer: Lyon, France, 2020.
- Global Cancer Observatory: United Arab Emirates Fact Sheet; World Health Organization, International Agency for Research on Cancer: Lyon, France, 2020.
- Global Cancer Observatory: Yemen Fact Sheet; World Health Organization, International Agency for Research on Cancer: Lyon, France, 2020.
- Saadeh, S.; Abdel-Razeq, H. Breast Cancer in the Arab World. In Cancer in the Arab World; Al-Shamsi, H.O., Abu-Gheida, I.H., Iqbal, F., Al-Awadhi, A., Eds.; Springer: Singapore, 2022; pp. 353–362.
- Shin, S.; Fu, J.; Shin, W.K.; Huang, D.; Min, S.; Kang, D. Association of food groups and dietary pattern with breast cancer risk: A systematic review and meta-analysis. Clin. Nutr. 2023, 42, 282–297.
- De Cicco, P.; Catani, M.V.; Gasperi, V.; Sibilano, M.; Quaglietta, M.; Savini, I. Nutrition and Breast Cancer: A Literature Review on Prevention, Treatment and Recurrence. Nutrients 2019, 11, 1514.
- Cespedes, E.M.; Hu, F.B. Dietary patterns: From nutritional epidemiologic analysis to national guidelines. Am. J. Clin. Nutr. 2015, 101, 899–900.
- Gardner, C.D.; Vadiveloo, M.K.; Petersen, K.S.; Anderson, C.A.M.; Springfield, S.; Horn, L.V.; Khera, A.; Lamendola, C.; Mayo, S.M.; Joseph, J.J. Popular Dietary Patterns: Alignment with American Heart Association 2021 Dietary Guidance: A Scientific Statement from the American Heart Association. Circulation 2023, 147, 1715–1730.
- Sikalidis, A.K.; Kelleher, A.H.; Kristo, A.S. Mediterranean Diet. Encyclopedia 2021, 1, 371–387.
- Sadeghi, O.; Eshaghian, N.; Benisi-Kohansal, S.; Azadbakht, L.; Esmaillzadeh, A. A case-control study on the association between adherence to a Mediterranean-style diet and breast cancer. Front. Nutr. 2023, 10, 1140014.
- Djafari, F.; Ghorbaninejad, P.; Firouzabadi, F.D.; Sheikhhossein, F.; Shahinfar, H.; Safabakhsh, M.; Imani, H.; Shab-Bidar, S. Adherence to Mediterranean dietary quality index and risk of breast cancer in adult women: A case-control study. BMC Women’s Health 2023, 23, 107.
- Castro-Espin, C.; Bonet, C.; Crous-Bou, M.; Nadal-Zaragoza, N.; Tjønneland, A.; Mellemkjær, L.; Hajji-Louati, M.; Truong, T.; Katzke, V.; Le Cornet, C.; et al. Association of Mediterranean diet with survival after breast cancer diagnosis in women from nine European countries: Results from the EPIC cohort study. BMC Med. 2023, 21, 225.
- Li, Y.; Hu, B.-Q.; Wu, X.-J.; Qi, X.-W.; Jiang, J.; Cui, X.; Zhang, F.; Yang, X.-H. Adherence to Mediterranean diet and the risk of breast cancer: A meta-analysis. Transl. Cancer Res. 2018, 7, 1290–1297.
- Turati, F.; Carioli, G.; Bravi, F.; Ferraroni, M.; Serraino, D.; Montella, M.; Giacosa, A.; Toffolutti, F.; Negri, E.; Levi, F.; et al. Mediterranean Diet and Breast Cancer Risk. Nutrients 2018, 10, 326.
- Azzeh, F.S.; Hasanain, D.M.; Qadhi, A.H.; Ghafouri, K.J.; Azhar, W.F.; Ghaith, M.M.; Aldairi, A.F.; Almasmoum, H.A.; Assaggaf, H.M.; Alhussain, M.H.; et al. Consumption of Food Components of the Mediterranean Diet Decreases the Risk of Breast Cancer in the Makkah Region, Saudi Arabia: A Case-Control Study. Front. Nutr. 2022, 9, 863029.
- Rigi, S.; Mousavi, S.M.; Benisi-Kohansal, S.; Azadbakht, L.; Esmaillzadeh, A. The association between plant-based dietary patterns and risk of breast cancer: A case-control study. Sci. Rep. 2021, 11, 3391.
- Sasanfar, B.; Toorang, F.; Booyani, Z.; Vassalami, F.; Mohebbi, E.; Azadbakht, L.; Zendehdel, K. Adherence to plant-based dietary pattern and risk of breast cancer among Iranian women. Eur. J. Clin. Nutr. 2021, 75, 1578–1587.
- Romanos-Nanclares, A.; Willett, W.C.; Rosner, B.A.; Collins, L.C.; Hu, F.B.; Toledo, E.; Eliassen, A.H. Healthful and Unhealthful Plant-Based Diets and Risk of Breast Cancer in U.S. Women: Results from the Nurses’ Health Studies. Cancer Epidemiol. Biomark. Prev. 2021, 30, 1921–1931.
- Shah, S.; Mahamat-Saleh, Y.; Ait-Hadad, W.; Koemel, N.A.; Varraso, R.; Boutron-Ruault, M.C.; Laouali, N. Long-term adherence to healthful and unhealthful plant-based diets and breast cancer risk overall and by hormone receptor and histologic subtypes among postmenopausal females. Am. J. Clin. Nutr. 2023, 117, 467–476.
- DeClercq, V.; Nearing, J.T.; Sweeney, E. Plant-Based Diets and Cancer Risk: What is the Evidence? Curr. Nutr. Rep. 2022, 11, 354–369.
- Payandeh, N.; Shahinfar, H.; Amini, M.R.; Jafari, A.; Safabakhsh, M.; Imani, H.; Shab-Bidar, S. The Lack of Association between Plant-Based Dietary Pattern and Breast Cancer: A Hospital-Based Case-Control Study. Clin. Nutr. Res. 2021, 10, 115.
- Abbas, M.O.; Baig, M. Knowledge and Practice Concerning Breast Cancer Risk Factors and Screening among Females in UAE. Asian Pac. J. Cancer Prev. 2023, 24, 479–487.
- Alfawaz, H.; Khan, N.; Alhuthayli, H.; Wani, K.; Aljumah, M.A.; Khattak, M.N.K.; Alghanim, S.A.; Al-Daghri, N.M. Awareness and Knowledge Regarding the Consumption of Dietary Fiber and Its Relation to Self-Reported Health Status in an Adult Arab Population: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2020, 17, 4226.
- Naja, F.; Nasreddine, L.; Awada, S.; El Sayed Ahmad, R.; Hwalla, N. Nutrition in the Prevention of Breast Cancer: A Middle Eastern Perspective. Front. Public Health 2019, 7, 316.
- Foroutan-Ghaznavi, M.; Mazloomi, S.M.; Montazeri, V.; Pirouzpanah, S. Dietary patterns in association with the expression of pro-metastatic genes in primary breast cancer. Eur. J. Nutr. 2022, 61, 3267–3284.
- Brennan, S.F.; Cantwell, M.M.; Cardwell, C.R.; Velentzis, L.S.; Woodside, J.V. Dietary patterns and breast cancer risk: A systematic review and meta-analysis. Am. J. Clin. Nutr. 2010, 91, 1294–1302.
- Xiao, Y.; Xia, J.; Li, L.; Ke, Y.; Cheng, J.; Xie, Y.; Chu, W.; Cheung, P.; Kim, J.H.; Colditz, G.A.; et al. Associations between dietary patterns and the risk of breast cancer: A systematic review and meta-analysis of observational studies. Breast Cancer Res. 2019, 21, 16.
- Flores-García, M.K.; Mérida-Ortega, Á.; Denova-Gutiérrez, E.; Rothenberg, S.J.; López-Carrillo, L. “Western” and “prudent” dietary patterns are associated with breast cancer among Mexican pre- and postmenopausal women. Nutr. Res. 2022, 105, 138–146.
- Fu, L.; Xu, B.T.; Xu, X.R.; Gan, R.Y.; Zhang, Y.; Xia, E.Q.; Li, H.B. Antioxidant capacities and total phenolic contents of 62 fruits. Food Chem. 2011, 129, 345–350.
- Andersen, J.L.M.; Hansen, L.; Thomsen, B.L.R.; Christiansen, L.R.; Dragsted, L.O.; Olsen, A. Pre- and post-diagnostic intake of whole grain and dairy products and breast cancer prognosis: The Danish Diet, Cancer and Health cohort. Breast Cancer Res. Treat. 2020, 179, 743–753.
- Roswall, N.; Weiderpass, E. Alcohol as a risk factor for cancer: Existing evidence in a global perspective. J. Prev. Med. Public Health 2015, 48, 1–9.
- Foroozani, E.; Akbari, A.; Amanat, S.; Rashidi, N.; Bastam, D.; Ataee, S.; Sharifnia, G.; Faraouei, M.; Dianatinasab, M.; Safdari, H. Adherence to a western dietary pattern and risk of invasive ductal and lobular breast carcinomas: A case-control study. Sci. Rep. 2022, 12, 5859.
- Tsai, H.H.; Yu, J.C.; Hsu, H.M.; Chu, C.H.; Chang, T.M.; Hong, Z.J.; Feng, A.C.; Fu, C.Y.; Hsu, K.F.; Dai, M.S.; et al. The Risk of Breast Cancer between Western and Mediterranean Dietary Patterns. Nutrients 2023, 15, 2057.
- Heidari, Z.; Jalali, S.; Sedaghat, F.; Ehteshami, M.; Rashidkhani, B. Dietary patterns and breast cancer risk among Iranian women: A case-control study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018, 230, 73–78.
- Karimi, Z.; Jessri, M.; Houshiar-Rad, A.; Mirzaei, H.R.; Rashidkhani, B. Dietary patterns and breast cancer risk among women. Public Health Nutr. 2014, 17, 1098–1106.
- Khodabakhshi, A.; Seyfried, T.N.; Kalamian, M.; Beheshti, M.; Davoodi, S.H. Does a ketogenic diet have beneficial effects on quality of life, physical activity or biomarkers in patients with breast cancer: A randomized controlled clinical trial. Nutr. J. 2020, 19, 87.
- Sasanfar, B.; Toorang, F.; Esmaillzadeh, A.; Zendehdel, K. Adherence to the low carbohydrate diet and the risk of breast Cancer in Iran. Nutr. J. 2019, 18, 86.
- Khodabakhshi, A.; Akbari, M.E.; Mirzaei, H.R.; Mehrad-Majd, H.; Kalamian, M.; Davoodi, S.H. Feasibility, Safety, and Beneficial Effects of MCT-Based Ketogenic Diet for Breast Cancer Treatment: A Randomized Controlled Trial Study. Nutr. Cancer 2020, 72, 627–634.
- İyikesici, M.S.; Slocum, A.K.; Slocum, A.; Berkarda, F.B.; Kalamian, M.; Seyfried, T.N. Efficacy of Metabolically Supported Chemotherapy Combined with Ketogenic Diet, Hyperthermia, and Hyperbaric Oxygen Therapy for Stage IV Triple-Negative Breast Cancer. Cureus 2017, 9, e1445.
- Ghanbari, M.; Shahinfar, H.; Imani, H.; Safabakhsh, M.; Shab-Bidar, S. Association of Empirically Derived Food-Based Inflammatory Potential of the Diet and Breast Cancer: A Hospital-Based Case-Control Study. Clin. Breast Cancer 2022, 22, e567–e575.
- Gholamalizadeh, M.; Afsharfar, M.; Fathi, S.; Tajadod, S.; Mohseni, G.K.; Shekari, S.; Vahid, F.; Doaei, S.; Shafaei Kachaei, H.; Majidi, N.; et al. Relationship between breast cancer and dietary inflammatory index; a case-control study. Clin. Nutr. ESPEN 2022, 51, 353–358.
- Vahid, F.; Shivappa, N.; Hatami, M.; Sadeghi, M.; Ameri, F.; Jamshidi Naeini, Y.; Hebert, J.R.; Davoodi, S.H. Association between Dietary Inflammatory Index (DII) and Risk of Breast Cancer: A Case-Control Study. Asian Pac. J. Cancer Prev. 2018, 19, 1215–1221.
- Jalali, S.; Shivappa, N.; Hébert, J.R.; Heidari, Z.; Hekmatdoost, A.; Rashidkhani, B. Dietary Inflammatory Index and Odds of Breast Cancer in a Case-Control Study from Iran. Nutr. Cancer 2018, 70, 1034–1042.
- Sohouli, M.H.; Baniasadi, M.; Hernández-Ruiz, Á.; Magalhães, E.; Santos, H.O.; Akbari, A.; Zarrati, M. Associations of the Paleolithic Diet Pattern Scores and the Risk of Breast Cancer among Adults: A Case-Control Study. Nutr. Cancer 2023, 75, 256–264.
- Dixon, K.A.; Michelsen, M.K.; Carpenter, C.L. Modern Diets and the Health of Our Planet: An Investigation into the Environmental Impacts of Food Choices. Nutrients 2023, 15, 692.
- Xiao, Y.; Wang, Y.; Gu, H.; Xu, Z.; Tang, Y.; He, H.; Peng, L.; Xiang, L. Adherence to the Paleolithic diet and Paleolithic-like lifestyle reduce the risk of colorectal cancer in the United States: A prospective cohort study. J. Transl. Med. 2023, 21, 482.
- Shah, S.; Mahamat-Saleh, Y.; Hajji-Louati, M.; Correia, E.; Oulhote, Y.; Boutron-Ruault, M.-C.; Laouali, N. Palaeolithic diet score and risk of breast cancer among postmenopausal women overall and by hormone receptor and histologic subtypes. Eur. J. Clin. Nutr. 2023, 77, 596–602.
- Heidari, Z.; Mohammadi, E.; Aghamohammadi, V.; Jalali, S.; Rezazadeh, A.; Sedaghat, F.; Assadi, M.; Rashidkhani, B. Dietary Approaches to Stop Hypertension (DASH) diets and breast cancer among women: A case control study. BMC Cancer 2020, 20, 708.
- Toorang, F.; Sasanfar, B.; Esmaillzadeh, A.; Zendehdel, K. Adherence to the DASH Diet and Risk of Breast Cancer. Clin. Breast Cancer 2022, 22, 244–251.
More
Information
Subjects:
Nutrition & Dietetics
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
470
Revisions:
2 times
(View History)
Update Date:
04 Mar 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





