Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Anubha Kalra | -- | 1235 | 2024-02-27 08:12:06 | | | |
| 2 | Catherine Yang | Meta information modification | 1235 | 2024-02-27 08:37:24 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Dahiya, E.S.; Kalra, A.M.; Lowe, A.; Anand, G. Wearable Technology for Monitoring Electrocardiograms in Adults. Encyclopedia. Available online: https://encyclopedia.pub/entry/55502 (accessed on 08 February 2026).
Dahiya ES, Kalra AM, Lowe A, Anand G. Wearable Technology for Monitoring Electrocardiograms in Adults. Encyclopedia. Available at: https://encyclopedia.pub/entry/55502. Accessed February 08, 2026.
Dahiya, Ekta Singh, Anubha Manju Kalra, Andrew Lowe, Gautam Anand. "Wearable Technology for Monitoring Electrocardiograms in Adults" Encyclopedia, https://encyclopedia.pub/entry/55502 (accessed February 08, 2026).
Dahiya, E.S., Kalra, A.M., Lowe, A., & Anand, G. (2024, February 27). Wearable Technology for Monitoring Electrocardiograms in Adults. In Encyclopedia. https://encyclopedia.pub/entry/55502
Dahiya, Ekta Singh, et al. "Wearable Technology for Monitoring Electrocardiograms in Adults." Encyclopedia. Web. 27 February, 2024.
Copy Citation
In the rapidly evolving landscape of continuous electrocardiogram (ECG) monitoring systems, there is a heightened demand for non-invasive sensors capable of measuring ECGs and detecting heart rate variability (HRV) in diverse populations, ranging from cardiovascular patients to sports enthusiasts. Challenges like device accuracy, patient privacy, signal noise, and long-term safety impede the use of wearable devices in clinical practice.
electrocardiography
wearables
electronic devices
1. Introduction
Cardiovascular diseases (CVDs) cross geographic, socioeconomic, or gender boundaries [1]. Developed and lower-/middle-income countries have a higher prevalence of cardiovascular risk factors, incidences of CVD and stroke, and all-cause mortality [1][2]. Additionally, the 2015 Update on Heart Disease and Stroke Statistics by the American Heart Association (AHA) highlighted that both CVD and stroke are the leading causes of health and economic burden in the US and worldwide. According to the World Health Organization (WHO), CVDs are the primary cause of global mortality, with 17.9 million deaths per year. The reported number of CVD deaths is expected to reach >23.6 million by 2030, up from 17.3 million in 2015 [3].
Electrocardiograms (ECGs) have become a routine part of any complete medical evaluation and have been used as a diagnostic test since their discovery over 70 years ago. As an ECG provides a waveform showing the electrical activity through the cardiac muscles, many but not all types of damage to the heart tissue can be detected by the ECG [4]. The gold standard 12-lead ECG configuration with its three bipolar limb leads (I, II, and III), three unipolar augmented leads (aVL, aVR, and aVF), six unipolar chest leads (V1–V6), and a reference electrode, as shown in Figure 1, gives spatial information about the cardiac electrical activity [5]. A vital clinical utility of ECG measurement is in detecting acute and chronic myocardial infarction, helping to differentiate coronary artery chest pain from non-cardiac chest pain. Another common diagnostic role is in the identification and management of arrhythmias localizing supraventricular and ventricular arrhythmias [6]. Other cardiovascular diseases, such as myocarditis, pericarditis, and structural deformities, and non-cardiovascular diseases, including hyperthyroidism and hypothyroidism, electrolyte imbalance, and pulmonary embolisms, can manifest as alterations of the ECG curve [7].
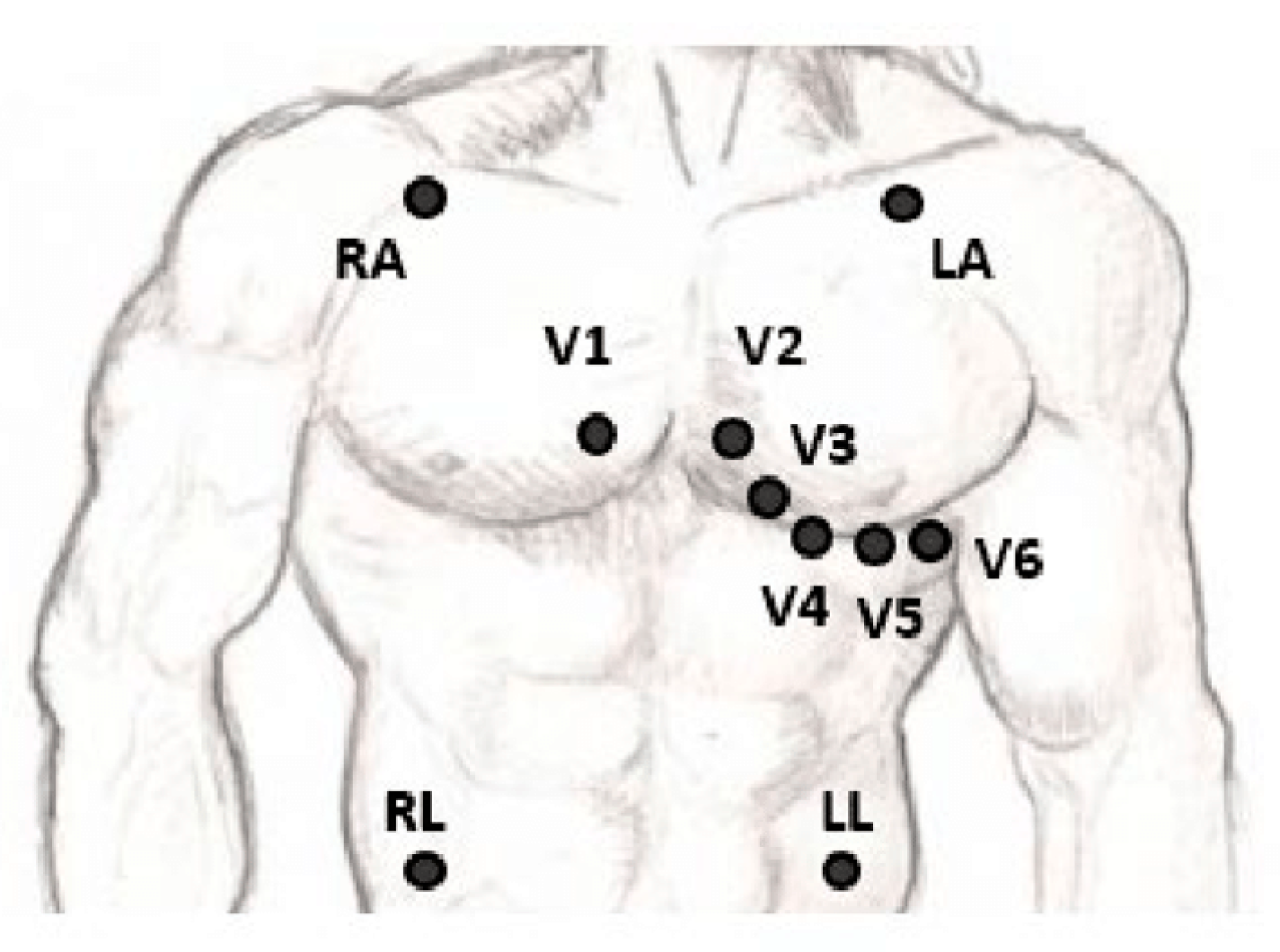
Figure 1. The placement of the leads in a standard 12-lead ECG [5].
2. Wearable Technology for Monitoring Electrocardiograms in Adults
Currently, ECG monitoring is being used in hospitals (e.g., ICUs, wards, and clinics), homes (telemonitoring, outpatient ambulatory monitoring, and elderly people continuous monitoring at home), and remotely (real-time monitoring, self-diagnosis, and activity monitoring [8]. Some clinical indications for which short intermittent or continuous ECG monitoring has been used are medical drug monitoring, cardiac stress testing, sports performance, fetal ECG, pre-operative assessment, and in operative patients under general anesthesia [9][10][11]. ECG monitoring has been used as a tool for proactive health monitoring by tracking the physiological changes in non-clinical high-stress environments such as deep-sea explorations, wearables in construction, high-altitude environments, and long-duration space exploration missions, with the goal of leveraging ECGs for the early detection of cardiovascular issues and timely intervention [12][13].
In the past few decades, ECG monitoring systems have been developed, evolved, and are widely used in the healthcare system. ECG monitoring systems are medical devices designed to record and display the electrical activity of the heart over a period of time. There is worldwide demand for a continuous health monitoring system that can detect heart rate variability through which cardiovascular diseases (accounting for 48% of non-communicable disease deaths, as per 2012 WHO Statistics) can be diagnosed and cured at an early stage [14]. Serhani et al. (2020) defined a taxonomy of ‘clusters’ for ECG monitoring systems (EMSs) as Context-aware EMS, Technology-aware EMS, EMS based on Schemes and Frequency, EMS Targets and Purposes, and Futuristic EMS, as shown in Figure 2. The second cluster of technology-aware individuals emphasized wearable devices integrated within an ambulatory, home, or patient/user setup, providing the means for the wireless monitoring of cardiovascular health [8].
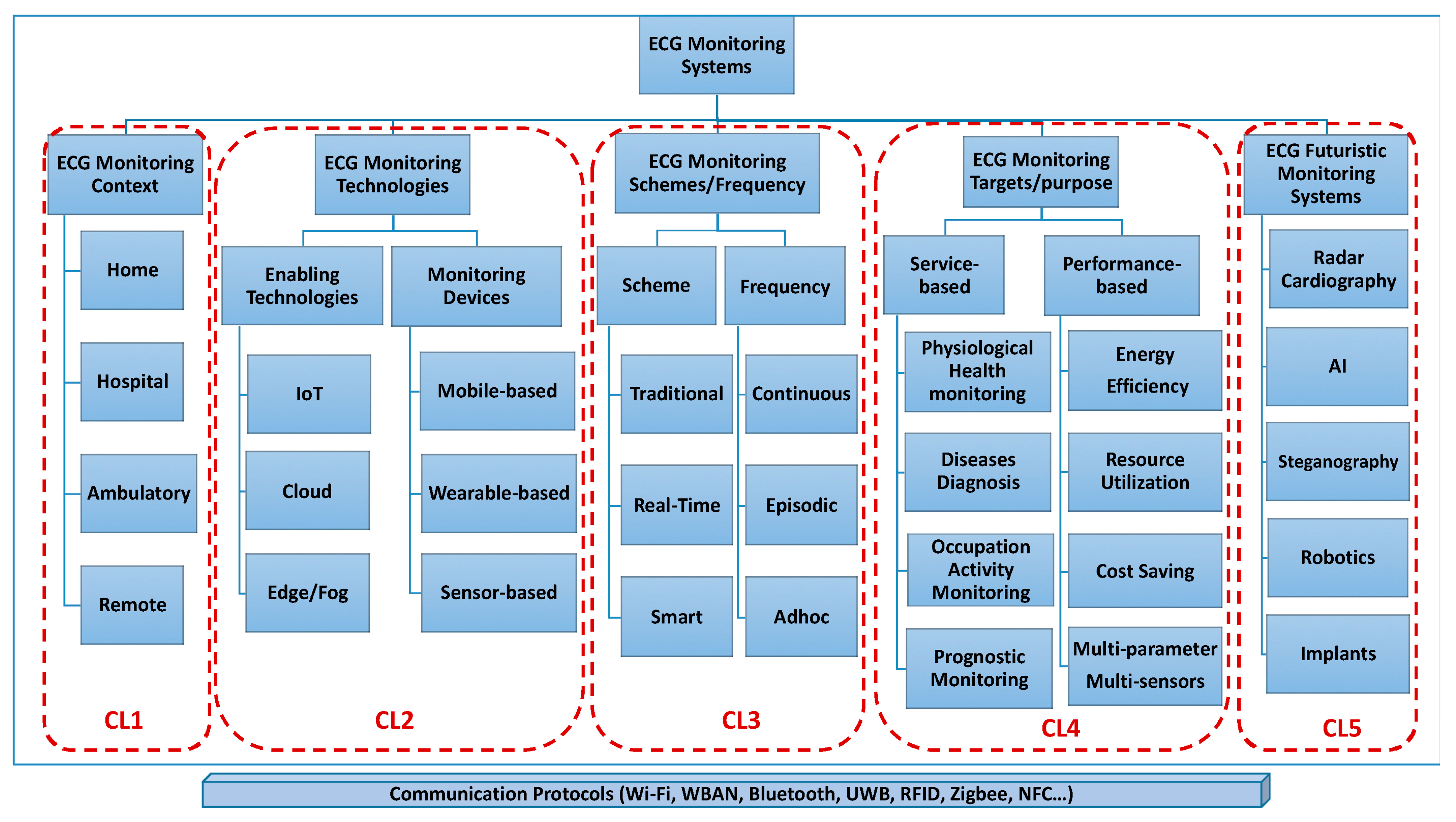
Figure 2. ECG monitoring system clustering (used with permission) [8].
Wearable ECG devices could be in the form of an ‘on-body patch’ or a contact-less sensor as a smart watch, ‘textile-base’ vest, or capacitive sensors integrated within patients’ stretchers, beds, and wheelchairs [8]. Regardless of the type of sensor, these EMSs integrate with the device to record and retrieve the ECG signals and conduct processing to present a trackable outcome. Prieto-Avalos et al. (2022) reviewed the commercial and non-commercial wearable devices for the physical monitoring of the heart, and they concluded that the majority of such devices have ECG monitoring capacity along with other data; however, improvement in the user’s health is limited without healthy personal habits [15]. Table 1 categorizes these wearable devices with ECG monitoring capacity using either single-lead or multi-lead continuous or real-time ECG. Heart rate during rest and activity can be calculated through the ECG or photoplethysmography (PPG) sensors by calculating beat-to-beat time intervals.
| Company/Brand | Product | FDA Status |
|---|---|---|
| Watches | ||
| Adidas | miCoach Fit Smart | NA |
| Apple | Apple Watch series | A |
| Biobeat | BB-613WP | A |
| Fitbit | Flex, One, Charge, Sense, Versa, Luxe, Inspire | A |
| Garmin | Epix Pro, Fenix 7 pro, Venu, Tactix 7 | A |
| Pixle Watch | NA | |
| Huawei | Huawei Watch GT, Ultimate, Huawei Band | NA |
| Karacus | DIONE, TRITON | NA |
| Omron | HeartGuide | A |
| Samsung | Galaxy Watch 3, 4, 5, 6 | A |
| SmartCardia | INYU | NA |
| Tom Tom | TomTom Spark | NA |
| Withings | Steel HR, Move, ScanWatch Horizon | A |
| Bands/bracelets | ||
| AliveCor | Kardiaband | A |
| BIOSTRAP | Armband HRM | NA |
| Fitbit | Charge 4 | A |
| HEALBE | GoBe3 | U |
| Microsoft | Microsoft Band | NA |
| MOCACARE | MOC cuff | A |
| Under Armour | UA Band | NA |
| Visi Mobile | The Visi Mobile System | A |
| Xiaomi | Mi Smart Band 5 | U |
| Patches | ||
| BardyDx | Zio Patch | A |
| BioTelemetry | Bio Tel Heart | A |
| Corventis Inc | Nuvant MCT | A |
| Huinno | MEMO Patch | NA |
| iRhythm | Zio Patch | A |
| MediBioSense | MediBio Sense MBS HealthStream | A |
| Preventice Solutions | BodyGuardian | A |
| Samsung | S-Patch Ex | A |
| Clothes | ||
| HealthWatch Technologies (smart garments) | Master Caution | A |
| Hexoskin (smart shirt) | Astroskin | NA |
| Medtronic (chest strap) | Zephyr | A |
| Polar (chest strap) | Polar H7 Strap | |
| Sleeplay (smart sock) | Owlet Smart Sock 3 | NA |
| Spire Health Tag | Spire | NA |
| Vivometrics (smart shirt) | The LifeShirt System | A |
| Zoll (vest) | LifeVest | A |
| Miscellaneous | ||
| AliveCor (phone attachment) | KardiaMobile | A |
| Personal Activity Intelligence (phone attachment) | PAI Health | U |
| Motiv (ring) | Motiv Ring | NA |
| Oura (finger ring) | Oura Ring | NA |
| FreeWavz (smart earphones) | FreeWavz-Blue | U |
| BioSensive Technologies (earrings) | Joule Earrings | NA |
| SonoHealth | EK Graph | NA |
| Jabra (headphones) | Sports Pulse Wireless Headphone | NA |
The FDA status is current as of January 2024. A: approved; NA: not Approved; and U: unknown.
The wearable wireless ECG devices are designed as a system of electrodes, an analog front-end (AFE), a data acquisition (DAQ) system, a digital signal processing (DSP) unit, wireless communication technology such as Bluetooth, IR, WiFi, and power consumption [8][17][18]. Although many ambulatory ECG monitoring systems have been commercialized to date, a major problem is still faced due to patients/athletes performing motion-related activities that introduce unwanted signal noise that makes monitoring less effective [19]. The frequency spectrum of the motion artifact overlaps the ECG; therefore, it is the most difficult form of noise to be removed [20]. A recent systematic review discussed the challenges of the present monitoring systems, which are rich in diversity and variability. The key challenges identified were manual static screening, the need to learn device operations at the user’s end, the effect on signal quality during real-time long-term monitoring, data processing, analysis and interpretation for the amount of data generated, sensor type and size and designs to keep it user-friendly, and being biocompatible for long-term monitoring [8][17]. Moreover, advances in mobile operating systems and the emergence of artificial intelligence bring their own benefits and challenges [15].
References
- Deaton, C.; Froelicher, E.S.; Wu, L.H.; Ho, C.; Shishani, K.; Jaarsma, T. The global burden of cardiovascular disease. Eur. J. Cardiovasc. Nurs. 2011, 10 (Suppl. S2), S5–S13.
- Feigin, V.L.; Krishnamurthi, R.V.; Barker-Collo, S.; McPherson, K.M.; Barber, P.A.; Parag, V.; Arroll, B.; Bennett, D.A.; Tobias, M.; Jones, A. 30-year trends in stroke rates and outcome in Auckland, New Zealand (1981–2012): A multi-ethnic population-based series of studies. PLoS ONE 2015, 10, e0134609.
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; De Ferranti, S.; Després, J.-P.; Fullerton, H.J.; Howard, V.J. Heart disease and stroke statistics—2015 update: A report from the American Heart Association. Circulation 2015, 131, e29–e322.
- Delano, M.K. A Long Term Wearable Electrocardiogram (ECG) Measurement System. Ph.D. Thesis, Massachusetts Institute of Technology, Cambridge, MA, USA, 2012.
- Kalra, A.; Lowe, A.; Al-Jumaily, A. Critical review of electrocardiography measurement systems and technology. Meas. Sci. Technol. 2018, 30, 012001.
- Rafie, N.; Kashou, A.H.; Noseworthy, P.A. ECG interpretation: Clinical relevance, challenges, and advances. Hearts 2021, 2, 505–513.
- Stracina, T.; Ronzhina, M.; Redina, R.; Novakova, M. Golden standard or obsolete method? Review of ECG applications in clinical and experimental context. Front. Physiol. 2022, 13, 867033.
- Serhani, M.A.; El Kassabi, H.T.; Ismail, H.; Nujum Navaz, A. ECG Monitoring Systems: Review, Architecture, Processes, and Key Challenges. Sensors 2020, 20, 1796.
- Drew, B.J.; Califf, R.M.; Funk, M.; Kaufman, E.S.; Krucoff, M.W.; Laks, M.M.; Macfarlane, P.W.; Sommargren, C.; Swiryn, S.; Van Hare, G.F. Practice standards for electrocardiographic monitoring in hospital settings: An American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young: Endorsed by the International Society of Computerized Electrocardiology and the American Association of Critical-Care Nurses. Circulation 2004, 110, 2721–2746.
- Khunti, K. Accurate interpretation of the 12-lead ECG electrode placement: A systematic review. Health Educ. J. 2014, 73, 610–623.
- Lilly, L.S. Pathophysiology of Heart Disease: A Collaborative Project of Medical Students and Faculty; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2012.
- Abuwarda, Z.; Mostafa, K.; Oetomo, A.; Hegazy, T.; Morita, P. Wearable devices: Cross benefits from healthcare to construction. Autom. Constr. 2022, 142, 104501.
- Vinetti, G.; Lopomo, N.F.; Taboni, A.; Fagoni, N.; Ferretti, G. The current use of wearable sensors to enhance safety and performance in breath-hold diving: A systematic review. Diving Hyperb. Med. 2020, 50, 54.
- Hayward, J.; Chansin, G. Wearable Sensors 2015–2025: Market Forecasts, Technologies, Players; IDTechEx: Cambridge, UK, 2015.
- Prieto-Avalos, G.; Cruz-Ramos, N.A.; Alor-Hernández, G.; Sánchez-Cervantes, J.L.; Rodríguez-Mazahua, L.; Guarneros-Nolasco, L.R. Wearable devices for physical monitoring of heart: A review. Biosensors 2022, 12, 292.
- Bayoumy, K.; Gaber, M.; Elshafeey, A.; Mhaimeed, O.; Dineen, E.H.; Marvel, F.A.; Martin, S.S.; Muse, E.D.; Turakhia, M.P.; Tarakji, K.G. Smart wearable devices in cardiovascular care: Where we are and how to move forward. Nat. Rev. Cardiol. 2021, 18, 581–599.
- Cosoli, G.; Spinsante, S.; Scardulla, F.; D’Acquisto, L.; Scalise, L. Wireless ECG and cardiac monitoring systems: State of the art, available commercial devices and useful electronic components. Measurement 2021, 177, 109243.
- Sequeira, L.; Perrotta, S.; LaGrassa, J.; Merikangas, K.; Kreindler, D.; Kundur, D.; Courtney, D.; Szatmari, P.; Battaglia, M.; Strauss, J. Mobile and wearable technology for monitoring depressive symptoms in children and adolescents: A scoping review. J. Affect. Disord. 2020, 265, 314–324.
- Yan, L.; Yoo, J.; Kim, B.; Yoo, H.-J. A 0.5-μ Vrms 12-μ W Wirelessly Powered Patch-Type Healthcare Sensor for Wearable Body Sensor Network. IEEE J. Solid-State Circuits 2010, 45, 2356–2365.
- Kim, D.-H.; Lu, N.; Ma, R.; Kim, Y.-S.; Kim, R.-H.; Wang, S.; Wu, J.; Won, S.M.; Tao, H.; Islam, A. Epidermal electronics. Science 2011, 333, 838–843.
More
Information
Subjects:
Engineering, Biomedical
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.4K
Entry Collection:
Hypertension and Cardiovascular Diseases
Revisions:
2 times
(View History)
Update Date:
27 Feb 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




