
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | tiantian niu | -- | 5090 | 2024-02-21 06:20:02 | | | |
| 2 | Lindsay Dong | + 299 word(s) | 5389 | 2024-02-23 01:52:06 | | |
Video Upload Options
In the face of an increasingly high-demand environment for outpatients, achieving a balance between allocation of limited medical resources and patient satisfaction has considerable social and economic benefits. Therefore, appointment scheduling (AS) system operation is used in clinics and hospitals, and its operation optimization research is of great significance.
1. Introduction
2. System Structure of AS
2.1. AS Characteristics
- 2.
-
ASs can be extended to represent other industries.
2.2. System Structure of AS
2.2.1. Appointment Rules
- 2.
-
Variable-interval rules.
-
The “offset” rule.
-
The “dome” appointment rule.
- The “plateau-dome” appointment rule.
2.2.2. Patient Classification
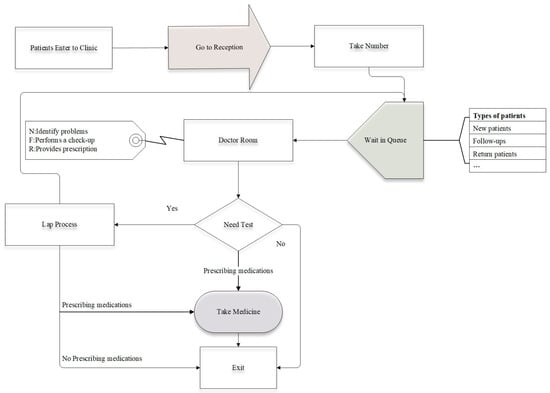
Several investigations have explored the implementation of patient classification (PC) based on the assumption that populations can be categorized into distinct groups. For example, in practice, a prevalent method of classifying patients is according to whether they are new or old who have been examined for a different length of time. This allows patients to be sorted at the time of the appointment, and diversity in consultation duration is combined by patient categorization to adjust the length of the appointment interval according to the characteristics of each group. Most studies are only concerned with the scheduling of patients attending elective appointments [49]. Meersman et al. proposed the scheduling horizon involves the time slots for elective and urgent patient categories [50], considering the slot allocation of non-elective patients.
2.3. AS System Decision Framework
2.3.1. Strategic Decisions
2.3.2. Tactical Decisions
2.3.3. Operational Decisions
3. Optimization Framework
3.1. Optimization Objective
3.1.1. Societal Benefit
3.1.2. Economic Performance
3.1.3. Resource Utilization
3.1.4. Other Objectives
3.2. Decision Variable
3.3. Constraints
4. Optimization Algorithms
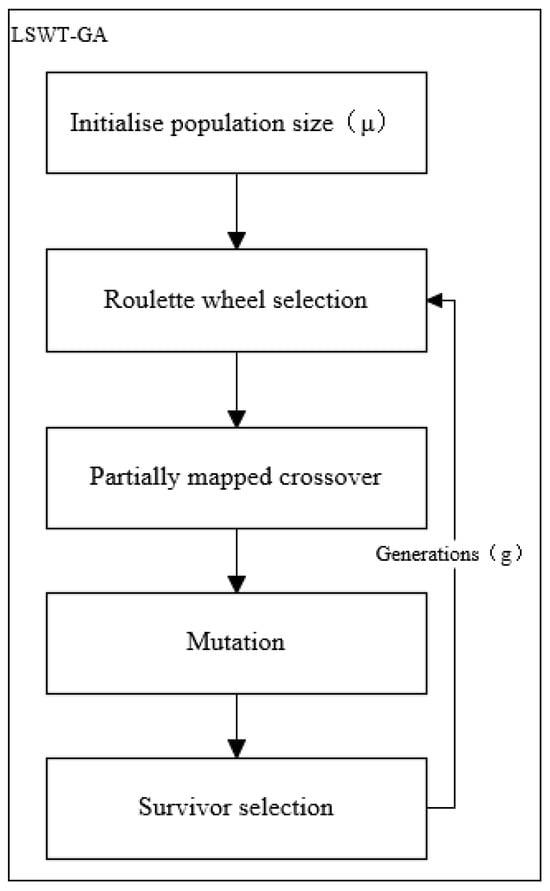
4.1. Genetic Algorithm
4.1.1. Objective Function and Constraint
4.1.2. Optimization Process
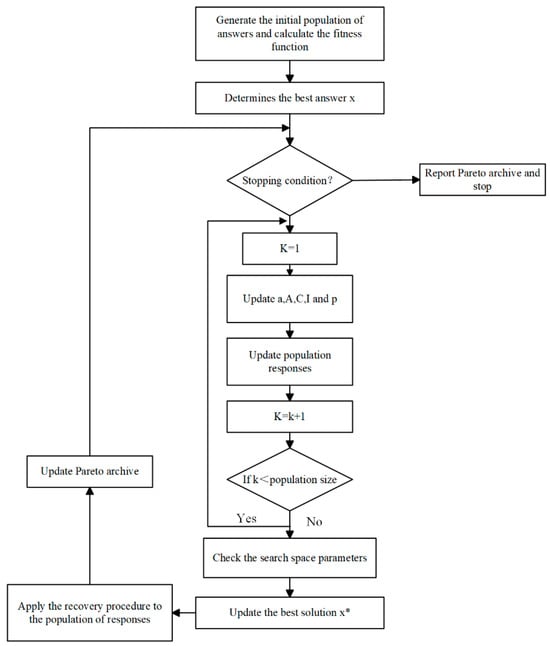
4.2. Whale Optimization Algorithm
4.2.1. Optimization Model
4.2.2. Objective Function
4.2.3. Constraint
4.2.4. Model Solving
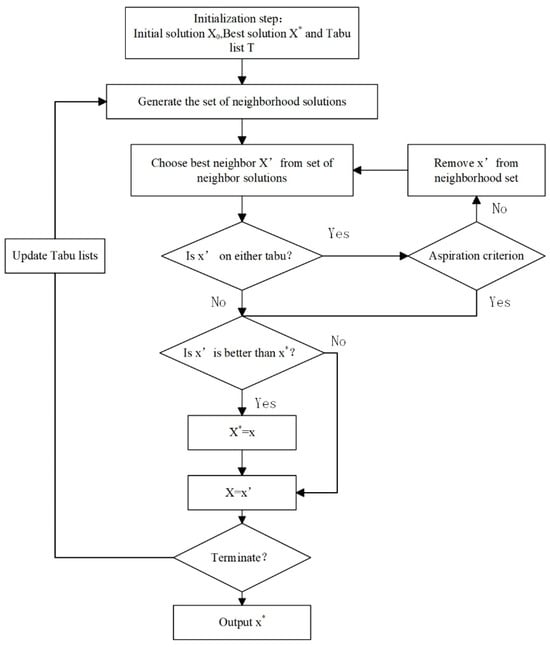
4.3. Tabu Search Algorithm
4.3.1. The Integer Programming Model in a Definitive Model
4.3.2. Algorithm Optimal Progress
4.4. Other Heuristic Algorithm
4.4.1. Problem Description
4.4.2. Constraint
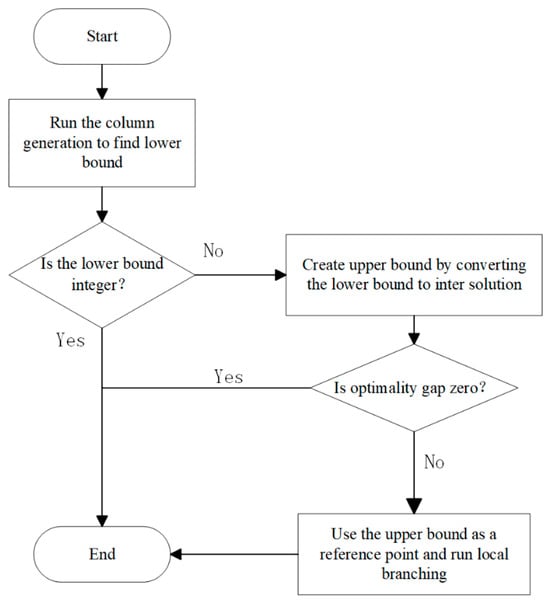
4.4.3. Solution Methodology
References
- Li, L. Development of China’s Health Care System in the Time of COVID-19: Challenges, Opportunities, and Call for Actions. Health Care Sci. 2022, 1, 33–40.
- Batko, K.; Ślęzak, A. The Use of Big Data Analytics in Healthcare. J. Big Data 2022, 9, 3.
- Gupta, D.; Denton, B. Appointment Scheduling in Health Care: Challenges and Opportunities. IIE Trans. 2008, 40, 800–819.
- Gao, K.; Shi, X.; Wang, W. The Life-Course Impact of Smoking on Hypertension, Myocardial Infarction and Respiratory Diseases. Sci. Rep. 2017, 7, 4330.
- Qu, L.; Gao, K.; Chen, X.; He, Q.; Ma, Y.; Peng, R. Optimal Quarantine Duration for Preventing Epidemic with Window Period. J. Infect. Non Infect. Dis. 2020, 5, 28.
- Alrefaei, M.H.; Diabat, A. Modelling and Optimization of Outpatient Appointment Scheduling. RAIRO-Oper. Res. 2015, 49, 435–450.
- Hulshof, P.J.H.; Vanberkel, P.T.; Boucherie, R.J.; Hans, E.W.; Van Houdenhoven, M.; Van Ommeren, J.-K.C.W. Analytical Models to Determine Room Requirements in Outpatient Clinics. OR Spectr. 2012, 34, 391–405.
- Huang, Y.-L.; Marcak, J. Grid Patient Appointment Template Design to Improve Scheduling Effectiveness. J. Healthc. Eng. 2015, 6, 239–258.
- Liu, N.; Finkelstein, S.R.; Kruk, M.E.; Rosenthal, D. When Waiting to See a Doctor Is Less Irritating: Understanding Patient Preferences and Choice Behavior in Appointment Scheduling. Manag. Sci. 2018, 64, 1975–1996.
- Wright, P.D.; Bretthauer, K.M.; Cote, M.J. Reexamining the Nurse Scheduling Problem: Staffing Ratios and Nursing Shortages. Decis. Sci. 2006, 37, 39–70.
- Talluri, K.; Van Ryzin, G. Revenue Management Under a General Discrete Choice Model of Consumer Behavior. Manag. Sci. 2004, 50, 15–33.
- Gao, K.; Wang, T.; Peng, K.; Wang, Z.; He, Q.; Peng, R. A Recursive Model of Residual Life Prediction for Human Beings with Health Information from Activities of Daily Living and Memory. Syst. Sci. Control Eng. 2021, 9, 529–541.
- Gao, K.; Peng, R.; Qu, L.; Xing, L.; Wang, S.; Wu, D. Linear System Design with Application in Wireless Sensor Networks. J. Ind. Inf. Integr. 2022, 27, 100279.
- Feldman, J.; Liu, N.; Topaloglu, H.; Ziya, S. Appointment Scheduling Under Patient Preference and No-Show Behavior. Oper. Res. 2014, 62, 794–811.
- Gupta, D.; Wang, W.-Y. Patient appointments in ambulatory care. In Handbook of Healthcare System Scheduling; Hall, R., Ed.; International Series in Operations Research & Management Science; Springer US: Boston, MA, USA, 2012; Volume 168, pp. 65–104. ISBN 978-1-4614-1733-0.
- Vieira, B.; Hans, E.W.; Van Vliet-Vroegindeweij, C.; Van De Kamer, J.; Van Harten, W. Operations Research for Resource Planning and -Use in Radiotherapy: A Literature Review. BMC Med. Inf. Decis. Mak. 2016, 16, 149.
- Leeftink, A.G.; Vliegen, I.M.H.; Hans, E.W. Stochastic Integer Programming for Multi-Disciplinary Outpatient Clinic Planning. Health Care Manag. Sci. 2019, 22, 53–67.
- Green, L.V.; Savin, S. Reducing Delays for Medical Appointments: A Queueing Approach. Oper. Res. 2008, 56, 1526–1538.
- Bobbie, A.; Karwowski, W. Simulation-Based Evaluation of Patient Appointment Policies for a Primary Care Clinic with Unscheduled Visits: A Case Study. Int. J. Hum. Factors Model. Simul. 2019, 7, 152.
- Lin, C.K.Y.; Ling, T.W.C.; Yeung, W.K. Resource Allocation and Outpatient Appointment Scheduling Using Simulation Optimization. J. Healthc. Eng. 2017, 2017, 9034737.
- Robinson, L.W.; Chen, R.R. Scheduling Doctors’ Appointments: Optimal and Empirically-Based Heuristic Policies. IIE Trans. 2003, 35, 295–307.
- Shonick, W. An Approach to Reducing the Adverse Effects of Broken Appointments in Primary Care Systems. Med. Care 1977, 15, 419–429.
- Chen, P.-S.; Hong, I.-H.; Hou, Y.; Shao, Y.-C. Healthcare Scheduling Policies in a Sequence-Number Based Appointment System for Outpatients’ Arrivals: Early, on Time, or Late? Comput. Ind. Eng. 2019, 130, 298–308.
- Tomkins, A.; Naylor, S.; Morgan, E. Short Message Service Cancellation Intervention to Reduce Integrated Sexual Health and HIV ‘Did Not Attend’ Appointment Rates. Int. J. STD AIDS 2019, 30, 201–203.
- Williamson, A.E.; Ellis, D.A.; Wilson, P.; McQueenie, R.; McConnachie, A. Understanding Repeated Non-Attendance in Health Services: A Pilot Analysis of Administrative Data and Full Study Protocol for a National Retrospective Cohort. BMJ Open 2017, 7, e014120.
- Dickey, W.; Morrow, J.I. Can Outpatient Non-Attendance Be Predicted from the Referral Letter? An Audit of Default at Neurology Clinics. J. R. Soc. Med. 1991, 84, 662–663.
- Barz, C.; Rajaram, K. Elective Patient Admission and Scheduling under Multiple Resource Constraints. Prod. Oper. Manag. 2015, 24, 1907–1930.
- Burke, E.K.; De Causmaecker, P.; Berghe, G.V.; Van Landeghem, H. The State of the Art of Nurse Rostering. J. Sched. 2004, 7, 441–499.
- Jansson, B. Choosing a Good Appointment System—A Study of Queues of the Type (D, M, 1). Oper. Res. 1966, 14, 292–312.
- Chiu, C.-K. Understanding Relationship Quality and Online Purchase Intention in E-Tourism: A Qualitative Application. Qual. Quant. 2009, 43, 669–675.
- Mak, H.-Y.; Rong, Y.; Zhang, J. Sequencing Appointments for Service Systems Using Inventory Approximations. Manuf. Serv. Oper. Manag. 2014, 16, 251–262.
- Denton, B.; Gupta, D. A Sequential Bounding Approach for Optimal Appointment Scheduling. IIE Trans. 2003, 35, 1003–1016.
- Klassen, K.J.; Rohleder, T.R. Outpatient Appointment Scheduling with Urgent Clients in a Dynamic, Multi-period Environment. Int. J. Serv. Ind. Manag. 2004, 15, 167–186.
- Cayirli, T.; Veral, E. Outpatient Scheduling in Health Care: A Review of Literature. Prod. Oper. Manag. 2009, 12, 519–549.
- Cayirli, T.; Veral, E.; Rosen, H. Designing Appointment Scheduling Systems for Ambulatory Care Services. Health Care Manag. Sci. 2006, 9, 47–58.
- Patrick, J.; Puterman, M.L.; Queyranne, M. Dynamic Multipriority Patient Scheduling for a Diagnostic Resource. Oper. Res. 2008, 56, 1507–1525.
- Solmaz, H. Comparison of Patients’ Admissions to the Cardiology Outpatient Clinics Between the Appointment System and the Queue System. Arch. Turk. Soc. Cardiol. 2023, 51, 188–195.
- Afrane, S.; Appah, A. Queuing Theory and the Management of Waiting-Time in Hospitals: The Case of Anglo Gold Ashanti Hospital in Ghana. Int. J. Acad. Res. Bus. Soc. Sci. 2014, 4, 34–44.
- Soriano, A.; Cayirli, T.; Yang, K.K.; Kong, Q.; Lee, C.-Y.; Teo, C.-P.; Zheng, Z.; Robinson, L.W.; Chen, R.R.; Denton, B.T.; et al. Comparison of Two Scheduling Systems. Oper. Res. 1966, 14, 388–397.
- LaGanga, L.R.; Lawrence, S.R. Appointment Overbooking in Health Care Clinics to Improve Patient Service and Clinic Performance. Prod. Oper. Manag. 2012, 21, 874–888.
- Shnits, B.; Bendavid, I.; Marmor, Y.N. An Appointment Scheduling Policy for Healthcare Systems with Parallel Servers and Pre-Determined Quality of Service. Omega 2020, 97, 102095.
- Cayirli, T.; Yang, K.K. Altering the Environment to Improve Appointment System Performance. Serv. Sci. 2019, 11, 138–154.
- Rohleder, T.; Klassen, K.J. Using Client-Variance Information to Improve Dynamic Appointment Scheduling Performance. Omega 2000, 28, 293–302.
- Creemers, S.; Lambrecht, M.R.; Beliën, J.; Van Den Broeke, M. Evaluation of Appointment Scheduling Rules: A Multi-Performance Measurement Approach. Omega 2021, 100, 102231.
- Bosch, P.M.V.; Dietz, D.C. Minimizing Expected Waiting in a Medical Appointment System. IIE Trans. 2000, 32, 841–848.
- Cayirli, T.; Yang, K.K.; Quek, S.A. A Universal Appointment Rule in the Presence of No-Shows and Walk-Ins. Prod. Oper. Manag. 2012, 21, 682–697.
- Klassen, K.J.; Yoogalingam, R. An Assessment of the Interruption Level of Doctors in Outpatient Appointment Scheduling. Oper. Manag. Res. 2008, 1, 95–102.
- Klassen, K.J.; Yoogalingam, R. Improving Performance in Outpatient Appointment Services with a Simulation Optimization Approach. Prod. Oper. Manag. 2009, 18, 447–458.
- Peng, Y.; Qu, X.; Shi, J. A Hybrid Simulation and Genetic Algorithm Approach to Determine the Optimal Scheduling Templates for Open Access Clinics Admitting Walk-in Patients. Comput. Ind. Eng. 2014, 72, 282–296.
- Meersman, T.; Maenhout, B. Multi-Objective Optimisation for Constructing Cyclic Appointment Schedules for Elective and Urgent Patients. Ann. Oper. Res. 2022, 312, 909–948.
- Ahmadi-Javid, A.; Jalali, Z.; Klassen, K.J. Outpatient Appointment Systems in Healthcare: A Review of Optimization Studies. Eur. J. Oper. Res. 2017, 258, 3–34.
- Robinson, L.W.; Chen, R.R. A Comparison of Traditional and Open-Access Policies for Appointment Scheduling. Manuf. Serv. Oper. Manag. 2010, 12, 330–346.
- Saghafian, S.; Austin, G.; Traub, S.J. Operations Research/Management Contributions to Emergency Department Patient Flow Optimization: Review and Research Prospects. IIE Trans. Healthc. Syst. Eng. 2015, 5, 101–123.
- Sauré, A.; Puterman, M.L. The Appointment Scheduling Game. INFORMS Trans. Educ. 2014, 14, 73–85.
- Wang, W.-Y.; Gupta, D. Adaptive Appointment Systems with Patient Preferences. Manuf. Serv. Oper. Manag. 2011, 13, 373–389.
- Kong, Q.; Lee, C.-Y.; Teo, C.-P.; Zheng, Z. Scheduling Arrivals to a Stochastic Service Delivery System Using Copositive Cones. Oper. Res. 2013, 61, 711–726.
- Erdogan, S.A.; Denton, B. Dynamic Appointment Scheduling of a Stochastic Server with Uncertain Demand. INFORMS J. Comput. 2013, 25, 116–132.
- Turkcan, A.; Zeng, B.; Muthuraman, K.; Lawley, M. Sequential Clinical Scheduling with Service Criteria. Eur. J. Oper. Res. 2011, 214, 780–795.
- Ozen, A.; Balasubramanian, H. The Impact of Case Mix on Timely Access to Appointments in a Primary Care Group Practice. Health Care Manag. Sci. 2013, 16, 101–118.
- Balasubramanian, H.; Biehl, S.; Dai, L.; Muriel, A. Dynamic Allocation of Same-Day Requests in Multi-Physician Primary Care Practices in the Presence of Prescheduled Appointments. Health Care Manag. Sci. 2014, 17, 31–48.
- Dharmadhikari, N.; Zhang, D.J. Simulation Optimization of Blocking Appointment Scheduling Policies for Multi-Clinic Appointments in Centralized Scheduling Systems. Ph.D. Thesis, North Dakota State University, Fargo, ND, USA, 2013. Volume 2.
- Cordier, J.-P.; Riane, F. Towards a Centralised Appointments System to Optimise the Length of Patient Stay. Decis. Support. Syst. 2013, 55, 629–639.
- Aslani, N.; Zhang, J. Integration of Simulation and DEA to Determine the Most Efficient Patient Appointment Scheduling Model for a Specific Healthcare Setting. J. Ind. Eng. Manag. 2014, 7, 785–815.
- Gao, K.; Peng, R.; Qu, L.; Wu, S. Jointly Optimizing Lot Sizing and Maintenance Policy for a Production System with Two Failure Modes. Reliab. Eng. Syst. Saf. 2020, 202, 106996.
- Bai, G.; Chi, Y.; Gao, K.; Peng, R. Reliability Evaluation of Multi-State Systems with Common Bus Performance Sharing Considering Performance Excess. IEEE Access 2022, 10, 19174–19185.
- Lei, B.; Ren, Y.; Luan, H.; Dong, R.; Wang, X.; Liao, J.; Fang, S.; Gao, K. A Review of Optimization for System Reliability of Microgrid. Mathematics 2023, 11, 822.
- Gao, K.; Wang, T.; Han, C.; Xie, J.; Ma, Y.; Peng, R. A Review of Optimization of Microgrid Operation. Energies 2021, 14, 2842.
- El-Sharo, M.; Zheng, B.; Yoon, S.W.; Khasawneh, M.T. An Overbooking Scheduling Model for Outpatient Appointments in a Multi-Provider Clinic. Oper. Res. Health Care 2015, 6, 1–10.
- Nguyen, T.B.T.; Sivakumar, A.I.; Graves, S.C. A Network Flow Approach for Tactical Resource Planning in Outpatient Clinics. Health Care Manag. Sci. 2015, 18, 124–136.
- Zeng, B.; Turkcan, A.; Lin, J.; Lawley, M. Clinic Scheduling Models with Overbooking for Patients with Heterogeneous No-Show Probabilities. Ann. Oper. Res. 2010, 178, 121–144.
- Savelsbergh, M.; Smilowitz, K. Stratified Patient Appointment Scheduling for Mobile Community-Based Chronic Disease Management Programs. IIE Trans. Healthc. Syst. Eng. 2016, 6, 65–78.
- Ren, Y.; Jin, C.; Fang, S.; Yang, L.; Wu, Z.; Wang, Z.; Peng, R.; Gao, K. A Comprehensive Review of Key Technologies for Enhancing the Reliability of Lithium-Ion Power Batteries. Energies 2023, 16, 6144.
- Homem-de-Mello, T.; Kong, Q.; Godoy-Barba, R. A Simulation Optimization Approach for the Appointment Scheduling Problem with Decision-Dependent Uncertainties. INFORMS J. Comput. 2022, 34, 2845–2865.
- Gao, K.; Yan, X.; Peng, R.; Xing, L. Economic Design of a Linear Consecutively Connected System Considering Cost and Signal Loss. IEEE Trans. Syst. Man. Cybern. Syst. 2021, 51, 5116–5128.
- Braune, R.; Gutjahr, W.J.; Vogl, P. Stochastic Radiotherapy Appointment Scheduling. Cent. Eur. J. Oper. Res. 2022, 30, 1239–1277.
- Fan, X.; Tang, J.; Yan, C.; Guo, H.; Cao, Z. Outpatient Appointment Scheduling Problem Considering Patient Selection Behavior: Data Modeling and Simulation Optimization. J. Comb. Optim. 2021, 42, 677–699.
- Dehghanimohammadabadi, M.; Rezaeiahari, M.; Seif, J. Multi-Objective Patient Appointment Scheduling Framework (MO-PASS): A Data-Table Input Simulation–Optimization Approach. Simulation 2023, 99, 363–383.
- Ala, A.; Alsaadi, F.E.; Ahmadi, M.; Mirjalili, S. Optimization of an Appointment Scheduling Problem for Healthcare Systems Based on the Quality of Fairness Service Using Whale Optimization Algorithm and NSGA-II. Sci. Rep. 2021, 11, 19816.
- Garaix, T.; Rostami, S.; Xie, X. Daily Outpatient Chemotherapy Appointment Scheduling with Random Deferrals. Flex. Serv. Manuf. J. 2020, 32, 129–153.
- Akbarzadeh, B.; Moslehi, G.; Reisi-Nafchi, M.; Maenhout, B. The Re-Planning and Scheduling of Surgical Cases in the Operating Room Department after Block Release Time with Resource Rescheduling. Eur. J. Oper. Res. 2019, 278, 596–614.





