
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Fernando Ramasco Rueda | -- | 7286 | 2024-01-30 01:05:12 | | | |
| 2 | Lindsay Dong | Meta information modification | 7286 | 2024-01-30 03:05:19 | | | | |
| 3 | Lindsay Dong | -3 word(s) | 7283 | 2024-02-07 02:25:15 | | |
Video Upload Options
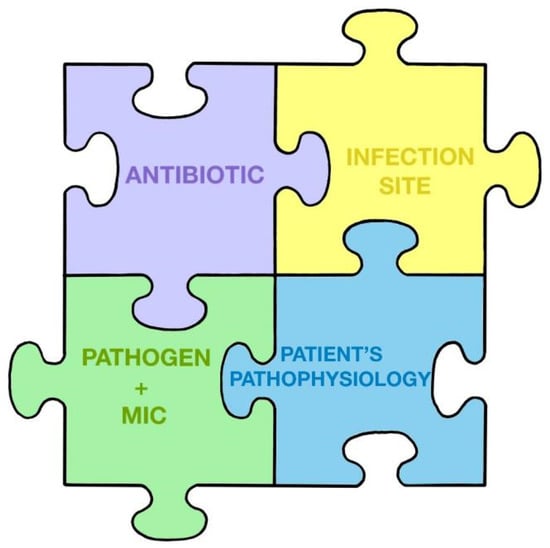
The main recent change observed in the field of critical patient infection has been the universal awareness of the need to make better use of antimicrobials, especially in the most seriously ill patients, beyond the application of simple formulas and rigid protocols. The greatest challenge, therefore, of decision making in this context lies in determining an effective, optimal, and balanced empirical antibiotic treatment. This is sepsis stewardship.
1. Introduction
2. The Current Problem of Antimicrobial Resistance
3. Antimicrobial Stewardship (AMS)
3.1. Start Smart
3.2. Start Smart and then Focus
-
Only start antimicrobial therapy if there is clear suspicion or evidence of infection;
-
Have a complete history of drug allergies and other patient considerations;
-
Initiate early and effective treatment in patients with sepsis and/or life-threatening infections;
-
Avoid the widespread use of broad-spectrum antibiotics, without paying attention to accompanying clinical symptoms, when treating any suspected infection;
-
Be up-to-date and always keep in mind the local microbiology and the patterns of resistance prevalent in the unit, the hospital, and the environment;
-
Obtain cultures before starting therapy when possible, taking into account that treatment should not be too greatly delayed;
-
In critically ill patients with septic shock, use the best antimicrobial alternative available to resolve the infection, in addition to controlling the outbreak whenever feasible, to reduce the bacterial load as soon as possible [12].
3.3. “… And Then Focus”: What Does This Consist of
-
Delay in administration;
-
Inappropriate spectrum of activity;
-
Inadequate blood levels or inadequate penetration into the focus of the infection;
-
Presence of antibiotic neutralizers and/or antagonists;
-
Presence of superbugs;
-
Presence of a superinfection;
-
Non-infectious source of fever;
-
The focus of the infection has not been properly controlled.
4. Microbiology: Key Concepts in Sepsis
4.1. Specimens and Diagnostic Techniques
- -
-
MALDI-TOF (matrix-assisted laser desorption ionization–time of flight): a technique based on mass spectrometry. MALDI-TOF currently allows the identification of microorganisms in less than 30 min (previously, it took up to 18 h) through the analysis of their protein profile. It is perhaps the most widespread rapid technique [16].
- -
-
RT-PCR (real-time polymerase chain reaction): a molecular technique that allows the direct identification of germs from the sample.
4.2. Minimum Inhibitory Concentration (MIC)
4.3. Preventive Concentration of Mutants
4.4. The Importance of Rectal Exudate
5. Pharmacokinetics and Pharmacodynamics of Beta-Lactams
6. Allergy to Beta-Lactams
7. What Should I Know about Old Antibiotics
8. New Antibiotics
8.1. Ceftazidime/Avibactam
8.2. Ceftolozane/Tazobactam
8.3. Cefiderocol
9. Cutting-Edge Approaches to New Antibiotics
9.1. Sparing Carbapenems
9.2. Role of New Antibiotics in the Empirical Treatment of Nosocomial Sepsis and Septic Shock
10. Recommendations for Empiric Antibiotic Treatment of Patients in Septic Shock
10.1. Preliminary Considerations
-
The bacterial load at the focus of infection will usually be high. The higher the bacterial load in the focus of infection, the higher the concentration of antibiotic needed to inhibit the growth of the microorganism and the greater the probability of selecting resistant mutants if the administered dose is not sufficient. The antibiotic exposure required to suppress the emergence of resistance should be maintained above the mutant selection window. Control of the outbreak via surgery or drainage is essential to decrease the bacterial load when possible.
-
As we do not know the microorganisms causing the infection or their patterns of antibiotic susceptibility, we can be guided by the suspected outbreak or guided by surveillance cultures, especially rectal exudate within the previous 48–72 h [52].
-
The local ecology of MDR bacteria influences the decision. A high percentage of resistance to carbapenems makes it necessary to consider the use of new antibiotics [59].
-
Empiric treatment should be active against all potentially involved microorganisms and, whenever possible, should contain a β-lactam antibiotic for its efficacy, spectrum, and bactericidal effect. Among the β-lactam antibiotics currently available, the most recommended for any outbreak, due to their antibacterial spectrum and probability of reaching the optimal target of Pk/Pd against MDR GNB, are ceftazidime/avibactam and meropenem. Depending on the focus of infection and colonization, personalization may be necessary and alternatives may exist.
-
The pharmacokinetics of antibiotic administration in sepsis will be drastically influenced by the inherent characteristics of the critically ill patient [60].
-
A patient in shock is at risk of irreversible damage, so it is urgent to reduce the bacterial load and control the immune response, while offering organ support.
-
Initial empirical therapy for patients in septic shock with pneumonia should be with two antibiotics and be based on risk factors for MDR pathogens discussed above, with an initial approach based on broad-spectrum therapy, followed by a reduction if MDR pathogens are ruled out in cultures [61].
-
Complicated intra-abdominal infection is usually polymicrobial, often with the intervention of GNB, anaerobes, and enterococci. Initial empiric therapy of patients in septic shock in this setting should include beta-lactam with a beta-lactamase inhibitor or carbapenem as well as coverage for anaerobes if beta-lactam does not cover them, coverage for enterococcus if the infection is nosocomial, and, in some patients with risk factors, additional initial coverage should be added for Candida species other than C. albicans. In this situation, it is key to control the outbreak, obtain quality samples, and process them quickly [62].
-
Daptomycin, linezolid, tedizolid, or vancomycin can be used against GPB. The choice depends on the location of the infection, renal function, and the need to use other nephrotoxic drugs simultaneously. It should be recalled that daptomycin does not show activity in the pulmonary focus [63].
-
Fungal infection accounts for 5% of sepsis. It is most commonly due to Candida spp. and can be predicted by specific scores such as the Candida Score as well as by epidemiological data, microbiological data, and biomarkers. Risk factors overlap with those of other causes of sepsis in the ICU. Preventive and empirical therapy is often necessary, and echinocandins are preferred for Candida, but some strains are becoming resistant so, in some scenarios, such as intra-abdominal infection or cases that are difficult to treat, liposomal amphotericin B may be a suitable alternative [64][65].
-
Appropriate cultures should always be obtained, depending on the focus of infection (blood cultures, rectal exudate, or other surveillance cultures, depending on the context), before the start or shortly after the initial empiric antibiotic treatment. The alarm, e.g., the sepsis code, should be triggered to ensure that samples are processed with rapid microbiological identification systems and, if possible, the microbiologist on duty should be alerted and interacted with [66].
-
After the first 24–48 h, the treatment should be re-evaluated in the context of a decrease in bacterial load and clinical improvement. Rapid diagnostic techniques will have allowed us to assess the absence or presence of ESBL-producing enterobacteriaceae or carbapenemases, resistant P. aeruginosa, MRSA, as well as a low value of β-D-glucan or its positivity, which will allow us to narrow the antibiotic spectrum or suggest a need to change treatment [67].
-
Short-term treatments should be attempted. Biomarkers such as procalcitonin (PCT) can help us in the application of short antibiotic treatment regimens [68].
10.2. Individualization of Antibiotic Treatment in Critically Ill Patients
Although the main challenges, in this context of the high prevalence of resistant strains, are to avoid delaying diagnosis through the rapid identification of microorganisms and their sensitivity patterns, adequate treatment is complicated by the peculiarities of the most severely ill patients who present alterations in their extracellular volume, renal function, and immunity, among other symptoms. In this way, the severity of their condition not only produces a higher mortality rate per se, but also affects the clinical response to antimicrobial treatment.
10.3. Early Antibiotic Treatment in Patients in Septic Shock
-
Lack of training;
-
Lack of correct assessment of severity and delay in recognition of sepsis;
-
Increased work;
-
Transfer of the patient (to the operating room, to tests, etc.);
-
Possibility of atypical manifestations, without fever or confusion;
-
Delays due to other diagnostic tests and slow collection of microbiological samples;
-
MDR germ infections and not recognizing MDR risk factors;
-
Waiting to carry out blood cultures before providing the antibiotic;
-
Very importantly, failing to recognize that providing an inappropriate antibiotic is like giving none or even worse. Appropriate antibiotics should not be delayed by inappropriate administration;
-
Not specifying the order in which antibiotics are administered and what the broad-spectrum “key” antibiotic is;
-
Needing to obtain authorization for the prescription, either from another specialist, the head of the infectious diseases department, or the pharmacy, before starting treatment.
-
The presence of hypotension in a patient with suspected infection should be considered septic shock in the absence of an alternative explanation;
-
Failure to transfer or transport the patient before antibiotic treatment has been administered;
-
If an antibiotic is requested in these situations, it must be ensured that it is administered immediately (it has been reported that the delay from the time the treatment is written to the time it is administered can be up to 3 h on average);
-
Combination regimens should be administered with the key antibiotic (the broadest spectrum) provided first;
-
Promote education, training, and teamwork to reduce administration time.
10.4. The Importance of Focus Control in Surgical Units
10.5. Optimization of Antibiotic Treatment According to Kumar’s Hypothesis
10.6. Duration of Antibiotic Treatment within Stewardship Programs
10.7. Tools for Making Sound Decisions
-
Annual update;
-
Provides local epidemiology data;
-
Characteristics of antimicrobials;
-
Dosing of antimicrobials in special situations;
-
Treatment of infections caused by specific microorganisms.
-
It is a guide made in the USA, available in English;
-
Epidemiology contains data from the United States.
11. Executive Summary for the Individualization of Antibiotic Treatment in Critically Ill Patients
References
- Cortegiani, A.; Antonelli, M.; Falcone, M.; Giarratano, A.; Girardis, M.; Leone, M.; Pea, F.; Stefani, S.; Vaggi, B.; Viale, P. Rationale and clinical application of antimicrobial stewardship principles in the intensive care unit: A multidisciplinary statement. J. Anesth. Analg. Crit. Care 2023, 3, 11.
- Liebchen, U.; Briegel, J.; Brinkmann, A.; Frey, O.; Wicha, S.G. Individualised dosing of antibiotics in ICU patients: Timing, target and model selection matter. Intensive Care Med. 2023, 49, 475–476.
- Yoo, J.H. The Infinity War: How to Cope with Carbapenem-resistant Enterobacteriaceae. J. Korean Med. Sci. 2018, 33, e255.
- Tang, K.W.K.; Millar, B.C.; Moore, J.E. Antimicrobial Resistance (AMR). Br. J. Biomed. Sci. 2023, 80, 11387.
- Llor, C.; Bjerrum, L. Antimicrobial resistance: Risk associated with antibiotic overuse and initiatives to reduce the problem. Ther. Adv. Drug Saf. 2014, 5, 229–241.
- Diekema, D.J.; Hsueh, P.R.; Mendes, R.E.; Pfaller, M.A.; Rolston, K.V.; Sader, H.S.; Jones, R.N. The Microbiology of Bloodstream Infection: 20-Year Trends from the SENTRY Antimicrobial Surveillance Program. Antimicrob. Agents Chemother. 2019, 63, e00355-19.
- De Waele, J.J.; Boelens, J.; Leroux-Roels, I. Multidrug-resistant bacteria in ICU: Fact or myth. Curr. Opin. Anaesthesiol. 2020, 33, 156–161.
- Bassetti, M.; Righi, E.; Vena, A.; Graziano, E.; Russo, A.; Peghin, M. Risk stratification and treatment of ICU-acquired pneumonia caused by multidrug- resistant/extensively drug-resistant/pandrug-resistant bacteria. Curr. Opin. Crit. Care 2018, 24, 385–393.
- The Abdominal Sepsis Study (AbSeS) Group on behalf of the Trials Group of the European Society of Intensive Care Medicine; Blot, S.; Antonelli, M.; Arvaniti, K.; Blot, K.; Creagh-Brown, B.; de Lange, D.; De Waele, J.; Deschepper, M.; Dikmen, Y.; et al. Epidemiology of intra-abdominal infection and sepsis in critically ill patients: “AbSeS”, a multinational observational cohort study and ESICM Trials Group Project. Intensive Care Med. 2019, 45, 1703–1717.
- Bassetti, S.; Tschudin-Sutter, S.; Egli, A.; Osthoff, M. Optimizing antibiotic therapies to reduce the risk of bacterial resistance. Eur. J. Intern. Med. 2022, 99, 7–12.
- Wunderink, R.G.; Srinivasan, A.; Barie, P.S.; Chastre, J.; Dela Cruz, C.S.; Douglas, I.S.; Ecklund, M.; Evans, S.E.; Evans, S.R.; Gerlach, A.T.; et al. Antibiotic Stewardship in the Intensive Care Unit. An Official American Thoracic Society Workshop Report in Collaboration with the AACN, CHEST, CDC, and SCCM. Ann. Am. Thorac. Soc. 2020, 17, 531–540.
- Mensa, J.; Barberán, J.; Ferrer, R.; Borges, M.; Rascado, P.; Maseda, E.; Oliver, A.; Marco, F.; Adalia, R.; Aguilar, G.; et al. Recommendations for antibiotic selection for severe nosocomial infections. Rev. Esp. Quimioter. 2021, 34, 511–524.
- Peri, A.M.; Stewart, A.; Hume, A.; Irwin, A.; Harris, P.N.A. New Microbiological Techniques for the Diagnosis of Bacterial Infections and Sepsis in ICU Including Point of Care. Curr. Infect. Dis. Rep. 2021, 23, 12.
- Tamma, P.D.; Miller, M.A.; Cosgrove, S.E. Rethinking How Antibiotics Are Prescribed: Incorporating the 4 Moments of Antibiotic Decision Making Into Clinical Practice. JAMA 2019, 321, 139–140.
- Gupta, E.; Saxena, J.; Kumar, S.; Sharma, U.; Rastogi, S.; Srivastava, V.K.; Kaushik, S.; Jyoti, A. Fast Track Diagnostic Tools for Clinical Management of Sepsis: Paradigm Shift from Conventional to Advanced Methods. Diagnostics 2023, 13, 277.
- Gerace, E.; Mancuso, G.; Midiri, A.; Poidomani, S.; Zummo, S.; Biondo, C. Recent Advances in the Use of Molecular Methods for the Diagnosis of Bacterial Infections. Pathogens 2022, 11, 663.
- Hansen, G.T. Point-of-Care Testing in Microbiology: A Mechanism for Improving Patient Outcomes. Clin. Chem. 2020, 66, 124–137.
- Kowalska-Krochmal, B.; Dudek-Wicher, R. The Minimum Inhibitory Concentration of Antibiotics: Methods, Interpretation, Clinical Relevance. Pathogens 2021, 10, 165.
- Nabal Díaz, S.G.; Algara Robles, O.; García-Lechuz Moya, J.M. New definitions of susceptibility categories EUCAST 2019: Clinic application. Rev. Esp. Quim. 2022, 35 (Suppl. S3), 84–88.
- Drlica, K.; Zhao, X. Mutant Selection Window Hypothesis Updated. Clin. Infect. Dis. 2007, 44, 681–688.
- Schlebusch, S.; Graham, R.M.A.; Jennison, A.V.; Lassig-Smith, M.M.; Harris, P.N.A.; Lipman, J.; Ó Cuív, P.; Paterson, D.L. Standard rectal swabs as a surrogate sample for gut microbiome monitoring in intensive care. BMC Microbiol. 2022, 22, 99.
- Roberts, J.A.; Taccone, F.S.; Lipman, J. Understanding PK/PD. Intensive Care Med. 2016, 42, 1797–1800.
- Roberts, J.A.; Paul, S.K.; Akova, M.; Bassetti, M.; De Waele, J.J.; Dimopoulos, G.; Kaukonen, K.-M.; Koulenti, D.; Martin, C.; Montravers, P.; et al. DALI: Defining antibiotic levels in intensive care unit patients: Are current β-lactam antibiotic doses sufficient for critically ill patients? Clin. Infect. Dis. 2014, 58, 1072–1083.
- Guilhaumou, R.; Benaboud, S.; Bennis, Y.; Dahyot-Fizelier, C.; Dailly, E.; Gandia, P.; Goutelle, S.; Lefeuvre, S.; Mongardon, N.; Roger, C.; et al. Optimization of the treatment with beta-lactam antibiotics in critically ill patients—Guidelines from the French Society of Pharmacology and Therapeutics (Société Française de Pharmacologie et Thérapeutique—SFPT) and the French Society of Anaesthesia and Intensive Care Medicine (Société Française d’Anesthésie et Réanimation—SFAR). Crit. Care 2019, 23, 104.
- Hong, L.T.; Downes, K.J.; FakhriRavari, A.; Abdul-Mutakabbir, J.C.; Kuti, J.L.; Jorgensen, S.; Young, D.C.; Alshaer, M.H.; Bassetti, M.; Bonomo, R.A.; et al. International consensus recommendations for the use of prolonged-infusion beta-lactam antibiotics: Endorsed by the American College of Clinical Pharmacy, British Society for Antimicrobial Chemotherapy, Cystic Fibrosis Foundation, European Society of Clinical Microbiology and Infectious Diseases, Infectious Diseases Society of America, Society of Critical Care Medicine, and Society of Infectious Diseases Pharmacists: An executive summary. Pharmacotherapy 2023, 43, 736–739.
- Tang, R.; Luo, R.; Wu, B.; Wang, F.; Song, H.; Chen, X. Effectiveness and safety of adjunctive inhaled antibiotics for ventilator-associated pneumonia: A systematic review and meta-analysis of randomized controlled trials. J. Crit. Care 2021, 65, 133–139.
- Kalil, A.C.; Metersky, M.L.; Klompas, M.; Muscedere, J.; Sweeney, D.A.; Palmer, L.B.; Napolitano, L.M.; O’Grady, N.P.; Bartlett, J.G.; Carratalà, J.; et al. Management of Adults with Hospital-acquired and Ventilator-associated Pneumonia: 2016 Clinical Practice Guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin. Infect. Dis. 2016, 63, e61–e111.
- Tablan, O.C.; Anderson, L.J.; Besser, R.; Bridges, C.; Hajjeh, R.; CDC; Healthcare Infection Control Practices Advisory Committee. Guidelines for preventing health-care-associated pneumonia, 2003: Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. Morb. Mortal. Wkly. Rep. Recomm. Rep. 2004, 53, 1–179.
- Rello, J.; Solé-Lleonart, C.; Rouby, J.J.; Chastre, J.; Blot, S.; Poulakou, G.; Luyt, C.-E.; Riera, J.; Palmer, L.B.; Pereira, J.M.; et al. Use of nebulized antimicrobials for the treatment of respiratory infections in invasively mechanically ventilated adults: A position paper from the European Society of Clinical Microbiology and Infectious Diseases. Clin. Microbiol. Infect. 2017, 23, 629–639.
- Shenoy, E.S.; Macy, E.; Rowe, T.; Blumenthal, K.G. Evaluation and Management of Penicillin Allergy: A Review. JAMA 2019, 321, 188–199.
- Stone, C.A.; Trubiano, J.; Coleman, D.T.; Rukasin, C.R.F.; Phillips, E.J. The challenge of de-labeling penicillin allergy. Allergy 2020, 75, 273–288.
- Alvarez-Cuesta, E.; Madrigal-Burgaleta, R.; Broyles, A.D.; Cuesta-Herranz, J.; Guzman-Melendez, M.A.; Maciag, M.C.; Phillips, E.J.; Trubiano, J.A.; Wong , J.T.; Ansotegui, I. Standards for practical intravenous rapid drug desensitization & delabeling: A WAO committee statement. World Allergy Organ. J. 2022, 15, 100640.
- Savic, L.; Ardern-Jones, M.; Avery, A.; Cook, T.; Denman, S.; Farooque, S.; Garcez, T.; Gold, R.; Jay, N.; Krishna, M.T.; et al. BSACI guideline for the set-up of penicillin allergy de-labelling services by non-allergists working in a hospital setting. Clin. Exp. Allergy 2022, 52, 1135–1141.
- Trubiano, J.A.; Vogrin, S.; Chua, K.Y.L.; Bourke, J.; Yun, J.; Douglas, A.; Stone, A.C.; Yu, R.; Lauren, G.; Holmes, N.E.; et al. Development and Validation of a Penicillin Allergy Clinical Decision Rule. JAMA Intern. Med. 2020, 180, 745–752.
- Courtemanche, J.; Baril, L.; Clément, A.; Bédard, M.A.; Plourde, M.; Émond, M. Is it possible to identify patients at low risk of having a true penicillin allergy? Can. J. Emerg. Med. 2022, 24, 366–368.
- Trubiano, J.A. A Risk-Based Approach to Penicillin Allergy. Immunol. Allergy Clin. North Am. 2022, 42, 375–389.
- Holmes, M.D.; Vo, N.; Rafeq, R.; Byrne, D.; King, M. Administration of β-lactam antibiotics to patients with reported penicillin allergy in the emergency department. Am. J. Emerg. Med. 2023, 68, 119–123.
- Pulcini, C.; Bush, K.; Craig, W.A.; Frimodt-Møller, N.; Grayson, M.L.; Mouton, J.W.; Turnidge, J.; Harbarth, S.; Gyssens, I.C.; ESCMID Study Group for Antibiotic Policies. Forgotten antibiotics: An inventory in Europe, the United States, Canada, and Australia. Clin. Infect. Dis. 2012, 54, 268–274.
- Brown, G.R. Cotrimoxazole—Optimal dosing in the critically ill. Ann. Intensive Care 2014, 4, 13.
- Yaghoubi, S.; Zekiy, A.O.; Krutova, M.; Gholami, M.; Kouhsari, E.; Sholeh, M.; Ghafouri, Z.; Maleki, F. Tigecycline antibacterial activity, clinical effectiveness, and mechanisms and epidemiology of resistance: Narrative review. Eur. J. Clin. Microbiol. Infect. Dis. 2022, 41, 1003–1022.
- De Pascale, G.; Lisi, L.; Ciotti, G.M.P.; Vallecoccia, M.S.; Cutuli, S.L.; Cascarano, L.; Gelormini, C.; Bello, G.; Montini, L.; Carelli, S.; et al. Pharmacokinetics of high-dose tigecycline in critically ill patients with severe infections. Ann. Intensive Care 2020, 10, 94.
- Brown, N.M.; Goodman, A.L.; Horner, C.; Jenkins, A.; Brown, E.M. Treatment of methicillin-resistant Staphylococcus aureus (MRSA): Updated guidelines from the UK. JAC Antimicrob. Resist. 2021, 3, dlaa114.
- Habib, G.; Lancellotti, P.; Antunes, M.J.; Bongiorni, M.G.; Casalta, J.P.; Del Zotti, F.; Dulgheru, R.; El Khoury, G.; Erba, P.A.; Iung, B.; et al. 2015 ESC Guidelines for the management of infective endocarditis: The Task Force for the Management of Infective Endocarditis of the European Society of Cardiology (ESC). Endorsed by: European Association for Cardio-Thoracic Surgery (EACTS), the European Association of Nuclear Medicine (EANM). Eur. Heart J. 2015, 36, 3075–3128.
- Shirley, M. Ceftazidime-Avibactam: A Review in the Treatment of Serious Gram-Negative Bacterial Infections. Drugs 2018, 78, 675–692.
- Matesanz, M.; Mensa, J. Ceftazidime-Avibactam. Rev. Esp. Quimioter. 2021, 34 (Suppl. S1), 38–40.
- Wang, L.T.; Lin, W.T.; Lai, C.C.; Wang, Y.H.; Chen, C.H.; Chang, Y.T.; Chen, C.-H.; Wang, C.-Y. The safety of ceftolozane-tazobactam for the treatment of acute bacterial infections: A systemic review and meta-analysis. Ther. Adv. Drug Saf. 2021, 12, 20420986211027096.
- Sansone, P.; Giaccari, L.G.; Coppolino, F.; Aurilio, C.; Barbarisi, A.; Passavanti, M.B.; Pota, V.; Pace, M.C. Cefiderocol for Carbapenem-Resistant Bacteria: Handle with Care! A Review of the Real-World Evidence. Antibiotics 2022, 11, 904.
- Maseda, E.; Suárez de la Rica, A. The role of cefiderocol in clinical practice. Rev. Esp. Quimioter. 2022, 35 (Suppl. S2), 39–44.
- Corcione, S.; Lupia, T.; Maraolo, A.E.; Mornese Pinna, S.; Gentile, I.; De Rosa, F.G. Carbapenem-sparing strategy: Carbapenemase, treatment, and stewardship. Curr. Opin. Infect. Dis. 2019, 32, 663–673.
- Jean, S.S.; Harnod, D.; Hsueh, P.R. Global Threat of Carbapenem-Resistant Gram-Negative Bacteria. Front. Cell Infect. Microbiol. 2022, 12, 823684.
- Arulkumaran, N.; Routledge, M.; Schlebusch, S.; Lipman, J.; Conway Morris, A. Antimicrobial-associated harm in critical care: A narrative review. Intensive Care Med. 2020, 46, 225–235.
- Strich, J.R.; Heil, E.L.; Masur, H. Considerations for Empiric Antimicrobial Therapy in Sepsis and Septic Shock in an Era of Antimicrobial Resistance. J. Infect. Dis. 2020, 222 (Suppl. S2), S119–S131.
- Tamma, P.D.; Aitken, S.L.; Bonomo, R.A.; Mathers, A.J.; van Duin, D.; Clancy, C.J. Infectious Diseases Society of America 2023 Guidance on the Treatment of Antimicrobial Resistant Gram-Negative Infections. Clin. Infect. Dis. 2023, ciad428.
- Pintado, V.; Ruiz-Garbajosa, P.; Aguilera-Alonso, D.; Baquero-Artigao, F.; Bou, G.; Cantón, R.; Grau, S.; Gutiérrez-Gutiérrez, B.; Larrosa, N.; Machuca, I.; et al. Executive summary of the consensus document of the Spanish Society of Infectious Diseases and Clinical Microbiology (SEIMC) on the diagnosis and antimicrobial treatment of infections due to carbapenem-resistant Gram-negative bacteria. Enferm. Infecc. Microbiol. Clin. 2023, 41, 360–370.
- Paul, M.; Carrara, E.; Retamar, P.; Tängdén, T.; Bitterman, R.; Bonomo, R.A.; de Waele, J.; Daikos, G.L.; Akova, M.; Harbarth, S.; et al. European Society of Clinical Microbiology and Infectious Diseases (ESCMID) guidelines for the treatment of infections caused by multidrug-resistant Gram-negative bacilli (endorsed by European society of intensive care medicine). Clin. Microbiol. Infect. 2022, 28, 521–547.
- Kumar, A. An alternate pathophysiologic paradigm of sepsis and septic shock: Implications for optimizing antimicrobial therapy. Virulence 2014, 5, 80–97.
- Danjean, M.; Hobson, C.A.; Gits-Muselli, M.; Courroux, C.; Monjault, A.; Bonacorsi, S.; Birgy, A. Evaluation of the inoculum effect of new antibiotics against carbapenem-resistant enterobacterales. Clin. Microbiol. Infect. 2022, 28, 1503.e1–1503.e3.
- Montravers, P.; Bassetti, M. The ideal patient profile for new beta-lactam/beta-lactamase inhibitors. Curr. Opin. Infect. Dis. 2018, 31, 587–593.
- Bassetti, M.; Garau, J. Current and future perspectives in the treatment of multidrug-resistant Gram-negative infections. J. Antimicrob. Chemother. 2021, 76 (Suppl. S4), iv23–iv37.
- Heffernan, A.J.; Mohd Sazlly Lim, S.; Lipman, J.; Roberts, J.A. A personalised approach to antibiotic pharmacokinetics and pharmacodynamics in critically ill patients. Anaesth. Crit. Care Pain. Med. 2021, 40, 100970.
- Zaragoza, R.; Vidal-Cortés, P.; Aguilar, G.; Borges, M.; Diaz, E.; Ferrer, R.; Maseda, E.; Nieto, M.; Nuvials, F.X.; Ramirez, P.; et al. Update of the treatment of nosocomial pneumonia in the ICU. Crit. Care 2020, 24, 383.
- Di Franco, S.; Alfieri, A.; Fiore, M.; Fittipaldi, C.; Pota, V.; Coppolino, F.; Sansone, P.; Pace, M.C.; Passavanti, M.B. A Literature Overview of Secondary Peritonitis Due to Carbapenem-Resistant Enterobacterales (CRE) in Intensive Care Unit (ICU) Patients. Antibiotics 2022, 11, 1347.
- Heidary, M.; Khosravi, A.D.; Khoshnood, S.; Nasiri, M.J.; Soleimani, S.; Goudarzi, M. Daptomycin. J. Antimicrob. Chemother. 2018, 73, 1–11.
- Thomas-Rüddel, D.O.; Schlattmann, P.; Pletz, M.; Kurzai, O.; Bloos, F. Risk Factors for Invasive Candida Infection in Critically Ill Patients: A Systematic Review and Meta-analysis. Chest 2022, 161, 345–355.
- Keane, S.; Geoghegan, P.; Povoa, P.; Nseir, S.; Rodriguez, A.; Martin-Loeches, I. Systematic review on the first line treatment of amphotericin B in critically ill adults with candidemia or invasive candidiasis. Expert Rev. Anti Infect. Ther. 2018, 16, 839–847.
- Princess, I.; Vadala, R. Clinical Microbiology in the Intensive Care Unit: Time for Intensivists to Rejuvenate this Lost Art. Indian J. Crit. Care Med. 2021, 25, 566–574.
- Burillo, A.; Bouza, E. Faster infection diagnostics for intensive care unit (ICU) patients. Expert Rev. Mol. Diagn. 2022, 22, 347–360.
- Méndez Hernández, R.; Ramasco Rueda, F. Biomarkers as Prognostic Predictors and Therapeutic Guide in Critically Ill Patients: Clinical Evidence. J. Pers. Med. 2023, 13, 333.
- Evans, L.; Rhodes, A.; Alhazzani, W.; Antonelli, M.; Coopersmith, C.M.; French, C.; Machado, F.R.; Mcintyre, L.; Ostermann, N.; Prescott, H.C.; et al. Surviving sepsis campaign: International guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021, 47, 1181–1247.
- Kumar, A.; Roberts, D.; Wood, K.E.; Light, B.; Parrillo, J.E.; Sharma, S.; Suppes, R.; Feinstein, D.; Zanotti, S.; Taiberg, L.; et al. Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit. Care Med. 2006, 34, 1589.
- Ferrer, R.; Martin-Loeches, I.; Phillips, G.; Osborn, T.M.; Townsend, S.; Dellinger, R.P.; Artigas, A.; Schorr, C.; Levy, M.M. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: Results from a guideline-based performance improvement program. Crit. Care Med. 2014, 42, 1749–1755.
- Peltan, I.D.; Mitchell, K.H.; Rudd, K.E.; Mann, B.A.; Carlbom, D.J.; Hough, C.L.; Rea, T.D.; Brown, S.M. Physician Variation in Time to Antimicrobial Treatment for Septic Patients Presenting to the Emergency Department. Crit. Care Med. 2017, 45, 1011–1018.
- Roberts, R.J.; Alhammad, A.M.; Crossley, L.; Anketell, E.; Wood, L.; Schumaker, G.; Garpestad, E.; Devlin, J.W. A survey of critical care nurses’ practices and perceptions surrounding early intravenous antibiotic initiation during septic shock. Intensive Crit. Care Nurs. 2017, 41, 90–97.
- Montravers, P.; Blot, S.; Dimopoulos, G.; Eckmann, C.; Eggimann, P.; Guirao, X.; Paiva, J.A.; Sganga, G.; De Waele, J. Therapeutic management of peritonitis: A comprehensive guide for intensivists. Intensive Care Med. 2016, 42, 1234–1247.
- Ordoñez, C.A.; Caicedo, Y.; Parra, M.W.; Rodríguez-Holguín, F.; Serna, J.J.; Salcedo, A.; Franco, M.J.; Toro, L.E.; Pino, L.F.; Guzmán-Rodríguez, M.; et al. Evolution of damage control surgery in non-traumatic abdominal pathology: A light in the darkness. Colomb. Med. 2021, 52, e4194809.
- De Waele, J.J.; Girardis, M.; Martin-Loeches, I. Source control in the management of sepsis and septic shock. Intensive Care Med. 2022, 48, 1799–1802.
- De Pascale, G.; Antonelli, M.; Deschepper, M.; Arvaniti, K.; Blot, K.; Brown, B.C.; de Lange, D.; De Waele, J.; Dikmen, Y.; Dimopoulos, G.; et al. Poor timing and failure of source control are risk factors for mortality in critically ill patients with secondary peritonitis. Intensive Care Med. 2022, 48, 1593–1606.
- Maseda, E.; Suarez-de-la-Rica, A.; Anillo, V.; Tamayo, E.; García-Bernedo, C.A.; Ramasco, F.; Villagran, M.-J.; Maggi, G.; Gimenez, M.-J.; Aguilar, L.; et al. Procalcitonin-guided therapy may reduce length of antibiotic treatment in intensive care unit patients with secondary peritonitis: A multicenter retrospective study. J. Crit. Care 2015, 30, 537–542.
- For the DURAPOP Trial Group; Montravers, P.; Tubach, F.; Lescot, T.; Veber, B.; Esposito-Farèse, M.; Seguin, P.; Paugam, C.; Lepape, A.; Meistelman, C.; et al. Short-course antibiotic therapy for critically ill patients treated for postoperative intra-abdominal infection: The DURAPOP randomised clinical trial. Intensive Care Med. 2018, 44, 300–310.
- Prest, J.; Nguyen, T.; Rajah, T.; Prest, A.B.; Sathananthan, M.; Jeganathan, N. Sepsis-Related Mortality Rates and Trends Based on Site of Infection. Crit. Care Explor. 2022, 4, e0775.
- Cavaillon, J.; Singer, M.; Skirecki, T. Sepsis therapies: Learning from 30 years of failure of translational research to propose new leads. EMBO Mol. Med. 2020, 12, e10128.
- Baggs, J.; Jernigan, J.A.; Halpin, A.L.; Epstein, L.; Hatfield, K.M.; McDonald, L.C. Risk of Subsequent Sepsis within 90 Days after a Hospital Stay by Type of Antibiotic Exposure. Clin. Infect. Dis. 2018, 66, 1004–1012.
- Teshome, B.F.; Vouri, S.M.; Hampton, N.; Kollef, M.H.; Micek, S.T. Duration of Exposure to Antipseudomonal β-Lactam Antibiotics in the Critically Ill and Development of New Resistance. Pharmacotherapy 2019, 39, 261–270.
- Raman, K.; Nailor, M.D.; Nicolau, D.P.; Aslanzadeh, J.; Nadeau, M.; Kuti, J.L. Early Antibiotic Discontinuation in Patients with Clinically Suspected Ventilator-Associated Pneumonia and Negative Quantitative Bronchoscopy Cultures. Crit. Care Med. 2013, 41, 1656–1663.
- Assicot, M.; Bohuon, C.; Gendrel, D.; Raymond, J.; Carsin, H.; Guilbaud, J. High serum procalcitonin concentrations in patients with sepsis and infection. Lancet 1993, 341, 515–518.
- Rau, B.; Krüger, C.M.; Schilling, M.K. Procalcitonin: Improved biochemical severity stratification and postoperative monitoring in severe abdominal inflammation and sepsis. Langenbeck’s Arch. Surg. 2004, 389, 134–144.
- Bouadma, L.; Luyt, C.E.; Tubach, F.; Cracco, C.; Alvarez, A.; Schwebel, C.; Schortgen, F.; Lasocki, S.; Veber, B.; Dehoux, M.; et al. Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): A multicentre randomised controlled trial. Lancet 2010, 375, 463–474.
- Kollef, M.H.; Shorr, A.F.; Bassetti, M.; Timsit, J.F.; Micek, S.T.; Michelson, A.P.; Garnacho-Montero, J. Timing of antibiotic therapy in the ICU. Crit. Care 2021, 25, 360.
- Zilberberg, M.D.; Shorr, A.F.; Micek, S.T.; Vazquez-Guillamet, C.; Kollef, M.H. Multi-drug resistance, inappropriate initial antibiotic therapy and mortality in Gram-negative severe sepsis and septic shock: A retrospective cohort study. Crit. Care 2014, 18, 596.
- Huang, C.T.; Tsai, Y.J.; Tsai, P.R.; Yu, C.J.; Ko, W.J. Severe Sepsis and Septic Shock: Timing of Septic Shock Onset Matters. Shock 2016, 45, 518–524.
- Panidis, D.; Markantonis, S.L.; Boutzouka, E.; Karatzas, S.; Baltopoulos, G. Penetration of gentamicin into the alveolar lining fluid of critically ill patients with ventilator-associated pneumonia. Chest 2005, 128, 545–552.
- Tsuji, B.T.; Pogue, J.M.; Zavascki, A.P.; Paul, M.; Daikos, G.L.; Forrest, A.; Giacobbe, D.R.; Viscoli, C.; Giamarellou, H.; Karaiskos, I.; et al. International Consensus Guidelines for the Optimal Use of the Polymyxins: Endorsed by the American College of Clinical Pharmacy (ACCP), European Society of Clinical Microbiology and Infectious Diseases (ESCMID), Infectious Diseases Society of America (IDSA), International Society for Anti-infective Pharmacology (ISAP), Society of Critical Care Medicine (SCCM), and Society of Infectious Diseases Pharmacists (SIDP). Pharmacotherapy 2019, 39, 10–39.





