
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Errico Zupi | -- | 2775 | 2024-01-22 12:37:22 | | | |
| 2 | Lindsay Dong | Meta information modification | 2775 | 2024-01-23 02:06:16 | | | | |
| 3 | Lindsay Dong | Meta information modification | 2775 | 2024-01-31 06:20:02 | | |
Video Upload Options
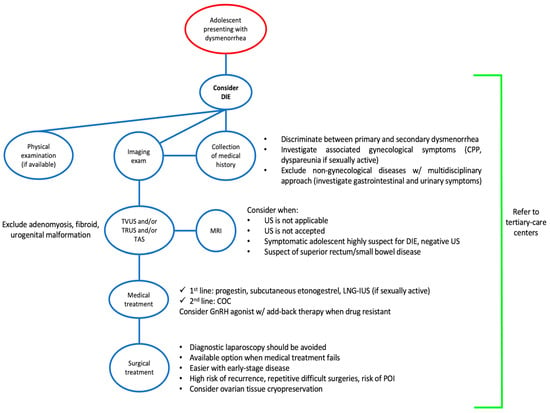
Endometriosis has a prevalence of 10% worldwide in premenopausal women. Probably, endometriosis begins early in the life of young girls, and it is commonly diagnosed later in life. The prevalence of deep infiltrating endometriosis (DIE) in adolescence is currently unknown due to diagnostic limits and underestimation of clinical symptoms. Dysmenorrhea is a common symptom in adolescents affected by DIE, often accompanied by dyspareunia and chronic acyclic pelvic pain. Ultrasonography—either performed transabdominal, transvaginal or transrectal—should be considered the first-line imaging technique despite the potential for missed diagnosis due to early-stage disease. Magnetic resonance imaging should be preferred in the case of virgo patients or when ultrasonographic exam is not accepted. Diagnostic laparoscopy is deemed acceptable in the case of suspected DIE not responding to conventional hormonal therapy. An early medical and/or surgical treatment may reduce disease progression with an immediate improvement in quality of life and fertility, but at the same time, painful symptoms may persist or even recur due to the surgery itself.
1. Introduction
2. Pathogenesis of DIE in Adolescents
3. Prevalence of DIE in Adolescents
4. DIE Symptoms
5. The Role of Imaging in Adolescence DIE Diagnosis
6. Adenomyosis and DIE in Adolescence
7. Management
8. Conclusions
References
- Zondervan, K.T.; Becker, C.M.; Missmer, S.A. Endometriosis. N. Engl. J. Med. 2020, 382, 1244–1256.
- D’alterio, M.N.; D’ancona, G.; Raslan, M.; Tinelli, R.; Daniilidis, A.; Angioni, S. Management Challenges of Deep Infiltrating Endometriosis. Int. J. Fertil. Steril. 2021, 15, 88.
- Treloar, S.A.; Bell, T.A.; Nagle, C.M.; Purdie, D.M.; Green, A.C. Early menstrual characteristics associated with subsequent diagnosis of endometriosis. Am. J. Obstet. Gynecol. 2010, 202, 534.e1–534.e6.
- Banikarim, C.; Chacko, M.R.; Kelder, S.H. Prevalence and impact of dysmenorrhea on Hispanic female adolescents. Arch. Pediatr. Adolesc. Med. 2000, 154, 1226–1229.
- Becker, C.M.; Bokor, A.; Heikinheimo, O.; Horne, A.; Jansen, F.; Kiesel, L.; King, K.; Kvaskoff, M.; Nap, A.; Petersen, K.; et al. ESHRE guideline: Endometriosis. Hum. Reprod. Open 2022, 2022, hoac009.
- Chapron, C.; Lafay-Pillet, M.C.; Monceau, E.; Borghese, B.; Ngô, C.; Souza, C.; de Ziegler, D. Questioning patients about their adolescent history can identify markers associated with deep infiltrating endometriosis. Fertil. Steril. 2011, 95, 877–881.
- Laufer, M.R. Helping “adult gynecologists” diagnose and treat adolescent endometriosis: Reflections on my 20 years of personal experience. J. Pediatr. Adolesc. Gynecol. 2011, 24 (Suppl. S5), S13–S17.
- Geysenbergh, B.; Dancet, E.A.F.; D’hooghe, T. Detecting Endometriosis in Adolescents: Why Not Start from Self-Report Screening Questionnaires for Adult Women? Gynecol. Obstet. Investig. 2017, 82, 322–328.
- Koninckx, P.R.; Fernandes, R.; Ussia, A.; Schindler, L.; Wattiez, A.; Al-Suwaidi, S.; Amro, B.; Al-Maamari, B.; Hakim, Z.; Tahlak, M. Pathogenesis Based Diagnosis and Treatment of Endometriosis. Front. Endocrinol. 2021, 12, 745548.
- Brosens, I.A.; Brosens, J.J. Redefining endometriosis: Is deep endometriosis a progressive disease? Hum. Reprod. 2000, 15, 1–3.
- Gargett, C.E.; Schwab, K.E.; Brosens, J.J.; Puttemans, P.; Benagiano, G.; Brosens, I. Potential role of endometrial stem/progenitor cells in the pathogenesis of early-onset endometriosis. Mol. Hum. Reprod. 2014, 20, 591–598.
- Brosens, I.; Gargett, C.E.; Guo, S.W.; Puttemans, P.; Gordts, S.; Brosens, J.J.; Benagiano, G. Origins and Progression of Adolescent Endometriosis. Reprod. Sci. 2016, 23, 1282–1288.
- Benagiano, G.; Guo, S.W.; Puttemans, P.; Gordts, S.; Brosens, I. Progress in the diagnosis and management of adolescent endometriosis: An opinion. Reprod. Biomed. Online 2018, 36, 102–114.
- Kondo, W.; Bourdel, N.; Tamburro, S.; Cavoli, D.; Jardon, K.; Rabischong, B.; Botchorishvili, R.; Pouly, J.; Mage, G.; Canis, M. Complications after surgery for deeply infiltrating pelvic endometriosis. BJOG 2011, 118, 292–298.
- Martire, F.G.; Zupi, E.; Lazzeri, L.; Morosetti, G.; Conway, F.; Centini, G.; Solima, E.; Pietropolli, A.; Piccione, E.; Exacoustos, C. Transvaginal Ultrasound Findings After Laparoscopic Rectosigmoid Segmental Resection for Deep Infiltrating Endometriosis. J. Ultrasound Med. 2021, 40, 1219–1228.
- Martire, F.G.; Russo, C.; Selntigia, A.; Siciliano, T.; Lazzeri, L.; Piccione, E.; Zupi, E.; Exacoustos, C. Transvaginal ultrasound evaluation of the pelvis and symptoms after laparoscopic partial cystectomy for bladder endometriosis. J. Turk. Ger. Gynecol. Assoc. 2022, 23, 145–153.
- Gordts, S.; Koninckx, P.; Brosens, I. Pathogenesis of deep endometriosis. Fertil. Steril. 2017, 108, 872–885.e1.
- Balun, J.; Dominick, K.; Cabral, M.D.; Taubel, D. Endometriosis in adolescents: A narrative review. Pediatr. Med. 2019, 2, 33.
- Brosens, I.; Benagiano, G. Is neonatal uterine bleeding involved in the pathogenesis of endometriosis as a source of stem cells? Fertil. Steril. 2013, 100, 622–623.
- Brosens, I.; Benagiano, G. Clinical significance of neonatal menstruation. Eur. J. Obstet. Gynecol. Reprod. Biol. 2016, 196, 57–59.
- Liakopoulou, M.K.; Tsarna, E.; Eleftheriades, A.; Arapaki, A.; Toutoudaki, K.; Christopoulos, P. Medical and Behavioral Aspects of Adolescent Endometriosis: A Review of the Literature. Children 2022, 9, 384.
- Mendiola, J.; Sánchez-Ferrer, M.L.; Jiménez-Velázquez, R.; Cánovas-López, L.; Hernández-Peñalver, A.I.; Corbalán-Biyang, S.; Carmona-Barnosi, A.; Prieto-Sánchez, M.T.; Nieto, A.; Torres-Cantero, A.M. Endometriomas and deep infiltrating endometriosis in adulthood are strongly associated with anogenital distance, a biomarker for prenatal hormonal environment. Hum. Reprod. 2016, 31, 2377–2383.
- Donnez, J. Introduction: From pathogenesis to therapy, deep endometriosis remains a source of controversy. Fertil. Steril. 2017, 108, 869–871.
- Sampson, J.A. Peritoneal endometriosis due to the menstrual dissemination of endometrial tissue into the peritoneal cavity. Am. J. Obstet. Gynecol. 1927, 14, 422–469.
- Nisolle, M.; Donnez, J. Peritoneal endometriosis, ovarian endometriosis, and adenomyotic nodules of the rectovaginal septum are three different entities. Fertil. Steril. 1997, 68, 585–596.
- Amro, B.; Aristondo, M.E.R.; Alsuwaidi, S.; Almaamari, B.; Hakim, Z.; Tahlak, M.; Wattiez, A.; Koninckx, P.R. New Understanding of Diagnosis, Treatment and Prevention of Endometriosis. Int. J. Environ. Res. Public. Health 2022, 19, 6725.
- Sinaii, N.; Cleary, S.D.; Ballweg, M.L.; Nieman, L.K.; Stratton, P. High rates of autoimmune and endocrine disorders, fibromyalgia, chronic fatigue syndrome and atopic diseases among women with endometriosis: A survey analysis. Hum. Reprod. 2002, 17, 2715–2724.
- Solnik, M.J. Chronic pelvic pain and endometriosis in adolescents. Curr. Opin. Obstet. Gynecol. 2006, 18, 511–518.
- Sasamoto, N.; Ngo, L.; Vitonis, A.F.; Dillon, S.T.; Sieberg, C.B.; A Missmer, S.; A Libermann, T.; Terry, K.L. Plasma proteomic profiles of pain subtypes in adolescents and young adults with endometriosis. Hum. Reprod. 2023, 38, 1509–1519.
- Han, S.J.; O’Malley, B.W. The dynamics of nuclear receptors and nuclear receptor coregulators in the pathogenesis of endometriosis. Hum. Reprod. Update 2014, 20, 467.
- Knox, B.; Ong, Y.C.; Bakar, M.A.; Grover, S.R. A longitudinal study of adolescent dysmenorrhoea into adulthood. Eur. J. Pediatr. 2019, 178, 1325–1332.
- Gubbels, A.; Spivack, L.; Lindheim, S.R.; Bhagavath, B. Adolescent Endometriosis. Obstet. Gynecol. Surv. 2020, 75, 483–496.
- Hirsch, M.; Dhillon-Smith, R.; Cutner, A.S.; Yap, M.; Creighton, S.M. The Prevalence of Endometriosis in Adolescents with Pelvic Pain: A Systematic Review. J. Pediatr. Adolesc. Gynecol. 2020, 33, 623–630.
- Koninckx, P.R.; Ussia, A.; Adamyan, L.; Wattiez, A.; Donnez, J. Deep endometriosis: Definition, diagnosis, and treatment. Fertil. Steril. 2012, 98, 564–571.
- DiVasta, A.D.; Vitonis, A.F.; Laufer, M.R.; Missmer, S.A. Spectrum of symptoms in women diagnosed with endometriosis during adolescence vs. adulthood. Am. J. Obstet. Gynecol. 2018, 218, 324.e1–324.e11.
- Suvitie, P.A.; Hallamaa, M.K.; Matomäki, J.M.; Mäkinen, J.I.; Perheentupa, A.H. Prevalence of Pain Symptoms Suggestive of Endometriosis Among Finnish Adolescent Girls (TEENMAPS Study). J. Pediatr. Adolesc. Gynecol. 2016, 29, 97–103.
- Sasamoto, N.; Shafrir, A.L.; Wallace, B.M.; Vitonis, A.F.; Fraer, C.J.; Gallagher, J.S.; DePari, M.; Ghiasi, M.; Laufer, M.R.; Sieberg, C.B.; et al. Trends in pelvic pain symptoms over 2 years of follow-up among adolescents and young adults with and without endometriosis. Pain 2023, 164, 613–624.
- Bush, D.; Brick, E.; East, M.C.; Johnson, N. Endometriosis education in schools: A New Zealand model examining the impact of an education program in schools on early recognition of symptoms suggesting endometriosis. Aust. N. Z. J. Obstet. Gynaecol. 2017, 57, 452–457.
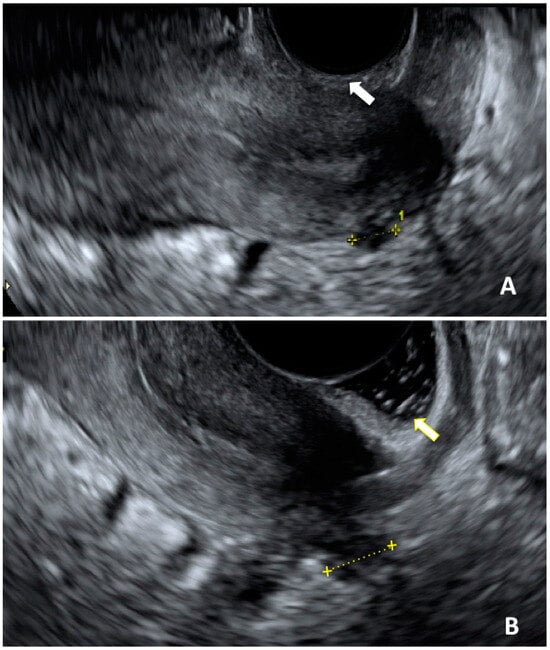
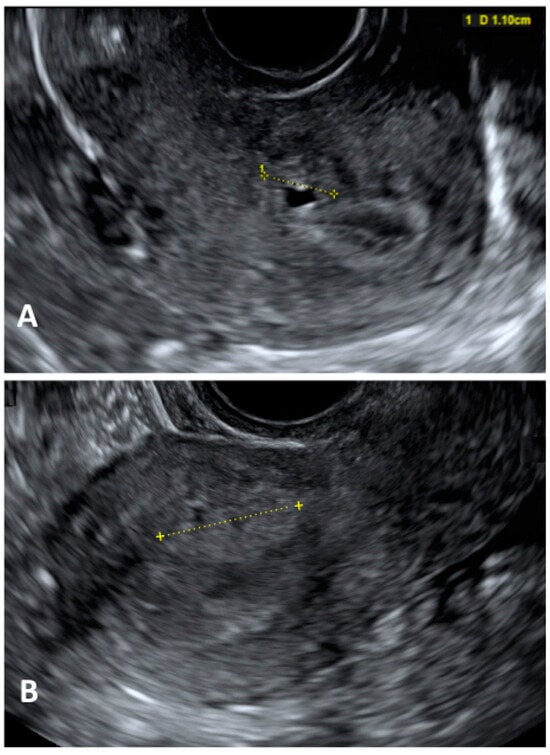
- Martire, F.G.; Russo, C.; Selntigia, A.; Nocita, E.; Soreca, G.; Lazzeri, L.; Zupi, E.; Exacoustos, C. Early noninvasive diagnosis of endometriosis: Dysmenorrhea and specific ultrasound findings are important indicators in young women. Fertil. Steril. 2023, 119, 455–464.
- Millischer, A.E.; Santulli, P.; Da Costa, S.; Bordonne, C.; Cazaubon, E.; Marcellin, L.; Chapron, C. Adolescent endometriosis: Prevalence increases with age on magnetic resonance imaging scan. Fertil. Steril. 2023, 119, 626–633.
- Martire, F.G.; Lazzeri, L.; Conway, F.; Siciliano, T.; Pietropolli, A.; Piccione, E.; Solima, E.; Centini, G.; Zupi, E.; Exacoustos, C. Adolescence and endometriosis: Symptoms, ultrasound signs and early diagnosis. Fertil. Steril. 2020, 114, 1049–1057.
- Lazzeri, L.; Andersson, K.L.; Angioni, S.; Arena, A.; Arena, S.; Bartiromo, L.; Berlanda, N.; Bonin, C.; Candiani, M.; Centini, G.; et al. How to Manage Endometriosis in Adolescence: The Endometriosis Treatment Italian Club Approach. J. Minim. Invasive Gynecol. 2023, 30, 616–626.
- Greene, R.; Stratton, P.; Cleary, S.D.; Ballweg, M.L.; Sinaii, N. Diagnostic experience among 4,334 women reporting surgically diagnosed endometriosis. Fertil. Steril. 2009, 91, 32–39.
- Martire, F.G.; Piccione, E.; Exacoustos, C.; Zupi, E. Endometriosis and Adolescence: The Impact of Dysmenorrhea. J. Clin. Med. 2023, 12, 5624.
- Centini, G.; Lazzeri, L.; Dores, D.; Pianigiani, L.; Iannone, P.; Luisi, S.; Petraglia, F.; Zupi, E. Chronic Pelvic Pain and Quality of Life in Women with and without Endometriosis. J. Endometr. Pelvic Pain Disord. 2013, 5, 27–33.
- Hailemeskel, S.; Demissie, A.; Assefa, N. Primary dysmenorrhea magnitude, associated risk factors, and its effect on academic performance: Evidence from female university students in Ethiopia. Int. J. Women’s Health 2016, 8, 489.
- Moumane, K.; Idri, A. Mobile applications for endometriosis management functionalities: Analysis and potential. Sci. Afr. 2023, 21, e01833.
- Chapron, C.; Santulli, P.; De Ziegler, D.; Noel, J.-C.; Anaf, V.; Streuli, I.; Foulot, H.; Souza, C.; Borghese, B. Ovarian endometrioma: Severe pelvic pain is associated with deeply infiltrating endometriosis. Hum. Reprod. 2012, 27, 702–711.
- Pino, I.; Belloni, G.M.; Barbera, V.; Solima, E.; Radice, D.; Angioni, S.; Arena, S.; Bergamini, V.; Candiani, M.; Maiorana, A.; et al. Better late than never but never late is better”, especially in young women. A multicenter Italian study on diagnostic delay for symptomatic endometriosis. Eur. J. Contracept. Reprod. Health Care 2023, 28, 10–16.
- Tsonis, O.; Barmpalia, Z.; Gkrozou, F.; Chandraharan, E.; Pandey, S.; Siafaka, V.; Paschopoulos, M. Endometriosis in adolescence: Early manifestation of the traditional disease or a unique variant? Eur. J. Obstet. Gynecol. Reprod. Biol. 2020, 247, 238–243.
- Shim, J.Y.; Laufer, M.R. Adolescent Endometriosis: An Update. J. Pediatr. Adolesc. Gynecol. 2020, 33, 112–119.
- Laufer, M.R.; Goitein, L.; Bush, M.; Cramer, D.W.; Emans, S.J. Prevalence of endometriosis in adolescent girls with chronic pelvic pain not responding to conventional therapy. J. Pediatr. Adolesc. Gynecol. 1997, 10, 199–202.
- Marcellin, L.; Santulli, P.; Pinzauti, S.; Bourdon, M.; Lamau, M.C.; Borghese, B.; Petraglia, F.; Chapron, C. Age at menarche does not correlate with the endometriosis phenotype. PLoS ONE 2019, 14, e0219497.
- Janssen, E.B.; Rijkers, A.C.M.; Hoppenbrouwers, K.; Meuleman, C.; D’Hooghe, T.M. Prevalence of endometriosis diagnosed by laparoscopy in adolescents with dysmenorrhea or chronic pelvic pain: A systematic review. Hum. Reprod. Update 2013, 19, 570–582.
- Raimondo, D.; Raffone, A.; Renzulli, F.; Sanna, G.; Raspollini, A.; Bertoldo, L.; Maletta, M.; Lenzi, J.; Rovero, G.; Travaglino, A.; et al. Prevalence and Risk Factors of Central Sensitization in Women with Endometriosis. J. Minim. Invasive Gynecol. 2023, 30, 73–80.e1.
- Miller, J.A.; Missmer, S.A.; Vitonis, A.F.; Sarda, V.; Laufer, M.R.; DiVasta, A.D. Prevalence of migraines in adolescents with endometriosis. Fertil. Steril. 2018, 109, 685–690.
- Schneider, M.P.; Vitonis, A.F.; Fadayomi, A.B.; Charlton, B.M.; Missmer, S.A.; DiVasta, A.D. Quality of Life in Adolescent and Young Adult Women With Dyspareunia and Endometriosis. J. Adolesc. Health 2020, 67, 557–561.
- Schomacker, M.L.; Hansen, K.E.; Ramlau-Hansen, C.H.; Forman, A. Is endometriosis associated with irritable bowel syndrome? A cross-sectional study. Eur. J. Obstet. Gynecol. Reprod. Biol. 2018, 231, 65–69.
- El-Matary, W.; Deora, V.; Grover, K. Barriers to clinical research in children with inflammatory bowel disease: The patients’ perspective. PLoS ONE 2018, 13, e0206965.
- Sharma, M.; Singh, P.; Agnihotri, A.; Das, P.; Mishra, A.; Verma, A.K.; Ahuja, A.; Sreenivas, V.; Khadgawat, R.; Gupta, S.D.; et al. Celiac disease: A disease with varied manifestations in adults and adolescents. J. Dig. Dis. 2013, 14, 518–525.
- Hansen, C.C.; Søreide, K. Systematic review of epidemiology, presentation, and management of Meckel’s diverticulum in the 21st century. Medicine 2018, 97, e12154.
- Dun, E.C.; Kho, K.A.; Morozov, V.V.; Kearney, S.; Zurawin, J.L.; Nezhat, C.H. Endometriosis in adolescents. JSLS 2015, 19, e2015.00019.
- Wright, K.N.; Laufer, M.R. Endometriomas in adolescents. Fertil. Steril. 2010, 94, 1529.e7–1529.e9.
- Hudelist, G.; Ballard, K.; English, J.; Wright, J.; Banerjee, S.; Mastoroudes, H.; Thomas, A.; Singer, C.F.; Keckstein, J. Transvaginal sonography vs. clinical examination in the preoperative diagnosis of deep infiltrating endometriosis. Ultrasound Obstet. Gynecol. 2011, 37, 480–487.
- Hudelist, G.; Fritzer, N.; Staettner, S.; Tammaa, A.; Tinelli, A.; Sparic, R.; Keckstein, J. Uterine sliding sign: A simple sonographic predictor for presence of deep infiltrating endometriosis of the rectum. Ultrasound Obstet. Gynecol. 2013, 41, 692–695.
- Nisenblat, V.; Bossuyt, P.M.M.; Farquhar, C.; Johnson, N.; Hull, M.L. Imaging modalities for the non-invasive diagnosis of endometriosis. Cochrane Database Syst. Rev. 2016, 2, CD009591.
- Margueritte, F.; Fauconnier, A. Adolescent endometriosis: Should we really use magnetic resonance imaging scans in this population? Fertil. Steril. 2023, 120 Pt 2, 706.
- Güdücü, N.; Sidar, G.; Işçi, H.; Yiǧiter, A.B.; Dünder, I. The Utility of Transrectal Ultrasound in Adolescents When Transabdominal or Transvaginal Ultrasound Is Not Feasible. J. Pediatr. Adolesc. Gynecol. 2013, 26, 265–268.
- Ohba, T.; Mizutani, H.; Maeda, T.; Matsuura, K.; Okamura, H. Evaluation of endometriosis in uterosacral ligaments by transrectal ultrasonography. Hum. Reprod. 1996, 11, 2014–2017.
- Koga, K.; Osuga, Y.; Yano, T.; Momoeda, M.; Yoshino, O.; Hirota, Y.; Kugu, K.; Nishii, O.; Tsutsumi, O.; Taketani, Y. Characteristic images of deeply infiltrating rectosigmoid endometriosis on transvaginal and transrectal ultrasonography. Hum. Reprod. 2003, 18, 1328–1333.
- Stochino-Loi, E.; Millochau, J.C.; Angioni, S.; Touleimat, S.; Abo, C.; Chanavaz-Lacheray, I.; Hennetier, C.; Roman, H. Relationship between Patient Age and Disease Features in a Prospective Cohort of 1560 Women Affected by Endometriosis. J. Minim. Invasive Gynecol. 2020, 27, 1158–1166.
- Zannoni, L.; Del Forno, S.; Paradisi, R.; Seracchioli, R. Endometriosis in Adolescence: Practical Rules for an Earlier Diagnosis. Pediatr. Ann. 2016, 45, e332–e335.
- Alborzi, S.; Rasekhi, A.; Shomali, Z.; Madadi, G.; Alborzi, M.; Kazemi, M.; Nohandani, A.H. Diagnostic accuracy of magnetic resonance imaging, transvaginal, and transrectal ultrasonography in deep infiltrating endometriosis. Medicine 2018, 97, e9536.
- Bazot, M.; Bharwani, N.; Huchon, C.; Kinkel, K.; Cunha, T.M.; Guerra, A.; Manganaro, L.; Buñesch, L.; Kido, A.; Togashi, K.; et al. European society of urogenital radiology (ESUR) guidelines: MR imaging of pelvic endometriosis. Eur. Radiol. 2017, 27, 2765–2775.
- Kinkel, K.; Frei, K.A.; Balleyguier, C.; Chapron, C. Diagnosis of endometriosis with imaging: A review. Eur. Radiol. 2006, 16, 285–298.
- Vercellini, P.; Viganò, P.; Somigliana, E.; Daguati, R.; Abbiati, A.; Fedele, L. Adenomyosis: Epidemiological factors. Best. Pract. Res. Clin. Obstet. Gynaecol. 2006, 20, 465–477.
- Viganò, P.; Parazzini, F.; Somigliana, E.; Vercellini, P. Endometriosis: Epidemiology and aetiological factors. Best. Pract. Res. Clin. Obstet. Gynaecol. 2004, 18, 177–200.
- Kunz, G.; Herbertz, M.; Beil, D.; Huppert, G.; Leyendecker, G. Adenomyosis as a disorder of the early and late human reproductive period. Reprod. Biomed. Online 2007, 15, 681–685.
- Exacoustos, C.; Lazzeri, L.; Martire, F.G.; Russo, C.; Martone, S.; Centini, G.; Piccione, E.; Zupi, E. Ultrasound Findings of Adenomyosis in Adolescents: Type and Grade of the Disease. J. Minim. Invasive Gynecol. 2022, 29, 291–299.e1.
- Dietrich, J.E. An update on adenomyosis in the adolescent. Curr. Opin. Obstet. Gynecol. 2010, 22, 388–392.
- Exacoustos, C.; Morosetti, G.; Conway, F.; Camilli, S.; Martire, F.G.; Lazzeri, L.; Piccione, E.; Zupi, E. New Sonographic Classification of Adenomyosis: Do Type and Degree of Adenomyosis Correlate to Severity of Symptoms? J. Minim. Invasive Gynecol. 2020, 27, 1308–1315.
- Conway, F.; Morosetti, G.; Camilli, S.; Martire, F.G.; Sorrenti, G.; Piccione, E.; Zupi, E.; Exacoustos, C. Ulipristal acetate therapy increases ultrasound features of adenomyosis: A good treatment given in an erroneous diagnosis of uterine fibroids. Gynecol. Endocrinol. 2019, 35, 207–210.
- Hewitt, G.D.; Gerancher, K.R. ACOG Committee Opinion No. 760: Dysmenorrhea and Endometriosis in the Adolescent. Obstet. Gynecol. 2018, 132, E249–E258.




