Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Gabriele Savioli | -- | 2859 | 2024-01-19 04:41:33 |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Savioli, G.; Ceresa, I.F.; Bavestrello Piccini, G.; Gri, N.; Nardone, A.; La Russa, R.; Saviano, A.; Piccioni, A.; Ricevuti, G.; Esposito, C. Hypothermia. Encyclopedia. Available online: https://encyclopedia.pub/entry/54076 (accessed on 06 March 2026).
Savioli G, Ceresa IF, Bavestrello Piccini G, Gri N, Nardone A, La Russa R, et al. Hypothermia. Encyclopedia. Available at: https://encyclopedia.pub/entry/54076. Accessed March 06, 2026.
Savioli, Gabriele, Iride Francesca Ceresa, Gaia Bavestrello Piccini, Nicole Gri, Alba Nardone, Raffaele La Russa, Angela Saviano, Andrea Piccioni, Giovanni Ricevuti, Ciro Esposito. "Hypothermia" Encyclopedia, https://encyclopedia.pub/entry/54076 (accessed March 06, 2026).
Savioli, G., Ceresa, I.F., Bavestrello Piccini, G., Gri, N., Nardone, A., La Russa, R., Saviano, A., Piccioni, A., Ricevuti, G., & Esposito, C. (2024, January 19). Hypothermia. In Encyclopedia. https://encyclopedia.pub/entry/54076
Savioli, Gabriele, et al. "Hypothermia." Encyclopedia. Web. 19 January, 2024.
Copy Citation
Hypothermia is a widespread condition all over the world, with a high risk of mortality in pre-hospital and in-hospital settings when it is not promptly and adequately treated. Hypothermia can occur due to unfavorable environmental conditions as well as internal causes, such as pathological states that result in reduced heat production, increased heat loss or ineffectiveness of the thermal regulation system. The consequences of hypothermia affect several systems in the body—the cardiovascular system, the central and peripheral nervous systems, the respiratory system, the endocrine system and the gastrointestinal system—but also kidney function, electrolyte balance and coagulation.
hypothermia
emergency department
homeostasis
1. Introduction
Hypothermia is a widespread condition observed all over the world, with a high risk of mortality in pre-hospital and in-hospital settings when its treatment is not implemented quickly and adequately [1]. It has been estimated that the incidence of mortality in hypothermic patients fluctuates between 13.3% and 43% in various prehospital settings around the world [2][3][4][5]. In a prehospital setting, the risk for hypothermia increases exponentially in the case of disease as well as of trauma, especially major trauma [6][7][8].
Hypothermia is defined as a reduction in core body temperature to less than 35.0 °C [9][10][11][12][13][14][15].
- -
-
Mild hypothermia: 32 °C < core body temperature < 35 °C.
- -
-
Moderate hypothermia: 28 °C < core body temperature < 32 °C.
- -
-
Severe hypothermia: core body temperature < 28 °C.
When taking into consideration the etiopathology of hypothermia, it is important to differentiate between spontaneous and induced hypothermia.
Spontaneous hypothermia can, in turn, be divided into the following:
- -
-
Primary hypothermia is due to environmental exposure, with no underlying medical condition causing the disruption of temperature regulation [17]. It therefore occurs when a person is exposed to the cold without adequate protection.
- -
-
Secondary hypothermia is a complication of pathological and paraphysiological conditions that determine the hypothermia itself or cause either an alteration of the thermoregulation mechanisms, reduced heat production or increased heat dispersion.
Induced hypothermia can, in turn, be divided into:
- -
-
Therapeutic hypothermia;
- -
-
Trauma-induced hypothermia [18].
Hypothermia is caused by a disturbance in an individual’s thermal homeostasis which causes physiological dysfunctions in several vital organs (Table 1).
Table 1. Classification of hypothermia from etiopathology.
| Classification from Etiopathology | ||
|---|---|---|
| Spontaneous hypothermia | Primary hypothermia | Secondary hypothermia |
| Induced hypothermia | Therapeutic hypothermia | Trauma-induced hypothermia |
2. Physiopathology
Thermal homeostasis is the maintenance of a stable temperature between 34 °C and 37.5 °C due to automatic regulation mechanisms that allow the body to be a system open to the external environment in continuous thermal equilibrium. These mechanisms are regulated by a thermoregulation system that balances the production of heat and its dispersion (Figure 1) [19][20].
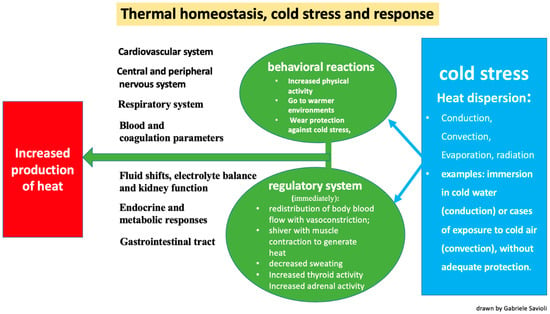
Figure 1. Thermal homeostasis and physiological response to cold stress.
The process of thermoregulation takes place at the level of the preoptic nucleus of the hypothalamus, which acts by activating subsequent effectors. In turn, this center continuously receives information on the state of temperature from thermal receptors located in the skin, aorta, arteries, and brain. The organs mainly involved in the production of heat in basal conditions are the liver and heart, followed in dynamic conditions by the musculoskeletal system. On the other hand, the organs most involved in the dispersion of heat are the skin, which undertakes an estimated 90% of the dispersion, and the respiratory system, which is responsible for the remaining 10% [21][22][23].
The mechanisms (Figure 1) by which the skin and lungs can dissipate heat are [24]:
-
Conduction: the transfer of heat to a cooler object through direct contact (for example, when immersed in cold water).
-
Convection: the transfer of heat at the body surface via air circulation (for example, when exposed to cold air or wind).
-
Evaporation: cooling of the skin surfaces when sweat changes from a liquid to a vapor form.
-
Radiation: occurs through the transmission of electromagnetic waves.
Of these mechanisms, the ones most frequently responsible for accidental or spontaneous hypothermia are conduction and convection.
The automatic thermo-regulatory response to maintain hemostasis occurs through several mechanisms (Figure 1):
- -
-
The redistribution of blood flow via vasoconstriction and a subsequent reduction in blood volume directed towards the skin and subcutis to reduce heat loss;
- -
-
Shivering, which generates heat via muscle contraction;
- -
-
Decreased sweating;
- -
-
Increased thyroid activity due to hypothalamic stimulus;
- -
-
Increased adrenal activity due to hypothalamic stimulus.
The stimulus of cold also determines, in a conscious subject who is able to perform them, some behavioral reactions (Figure 1):
- -
-
Increased physical activity;
- -
-
A shift to warmer environments;
- -
-
Wearing protection against the cold;
- -
-
Taking off wet clothes and replacing them with dry clothes.
Hypothermia therefore develops when there is a malfunction in one of the stages of thermal regulation or when there is either increased heat loss or reduced heat production that exceeds the compensation capacity of the regulatory centers.
3. Etiology and Risk Factors
Spontaneous hypothermia (primary) can occur due to unfavorable environmental conditions that exceed the body’s ability to defend itself from the cold.
Environmental causes related to hypothermia are, for example, exposure to the cold with wet clothes or without adequate protection or simply exposure to excessively cold temperatures.
Spontaneous hypothermia (secondary) can also occur due to internal causes, such as pathological states, which result in reduced heat production or increased heat loss or ineffectiveness of the thermal regulation system.
Internal causes that can lead to hypothermia are:
- -
-
Impaired thermoregulation (Figure 2): This may be paraphysiological in the extreme ages of life (geriatric people or infants). Impaired thermoregulation may also occur following pathological conditions such as mental illnesses, or pathologies of the nervous system (such as Parkinson’s disease, stroke, multiple sclerosis, hypothalamic dysfunction, brain trauma or subarachnoid hemorrhage) or pathologies affecting the peripheral nervous system (neuropathies, diabetes mellitus, trauma to a section of the spinal cord). Impaired thermoregulation may also be due to an iatrogenic effect of drugs such as anxiolytics, antidepressants, phenothiazines, barbiturates, opioids, antipsychotics, oral antihyperglycemics, β-blockers and α-blockers [25][26].
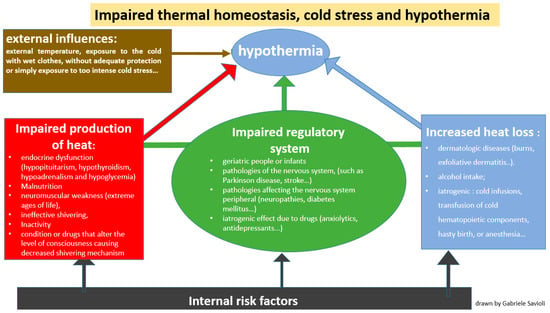 Figure 2. Mechanisms by which hypothermia develops: disruption of thermal homeostasis and dysregulated response to cold stress.
Figure 2. Mechanisms by which hypothermia develops: disruption of thermal homeostasis and dysregulated response to cold stress. - -
-
Increased heat loss (Figure 2): This can be caused by dermatologic diseases such as burns, exfoliative dermatitis or psoriasis [27][28][29]. Heat loss can also be increased in the case of indulgent habits such as alcohol intake [30][31] but it can also have an iatrogenic origin, as in the case of cold infusions, the transfusion of cold hematopoietic components, hasty birth or anesthesia.
- -
-
Decreased heat production (Figure 2): This is secondary to endocrine dysfunction (hypopituitarism, hypothyroidism, hypoadrenalism and hypoglycemia), malnutrition or either conditions or drugs that alter the level of consciousness, causing an impaired shivering mechanism.
Hypothermia can also be induced intentionally in medical settings for its neuroprotective effect following cardiac arrest, stroke or traumatic brain or spinal cord injury.
Risk factors that can predispose a patient to spontaneous hypothermia include external environmental factors not related to the individual, such as winter sports activities, immersion in cold water, wearing wet or insufficiently warm clothing or a lack of areas in which to shelter from cold [12][13].
There are also risk factors determined by physiological or paraphysiological conditions, such as the extreme ages of life. Infants and the elderly are fragile populations at high risk for developing hypothermia as they have less effective regulatory mechanisms; they are less able to generate heat through the shivering mechanism, both due to reduced muscle mass and, in the elderly, reduced function of their reflexes, and peripheral vasoconstriction is usually less effective for the retention of heat. In addition, it should be remembered that children are more susceptible to hypothermia than adults since they have a higher body surface index, causing a greater loss of heat via convection [32]. While it is true that children generate more metabolic heat than adults, enough to maintain body heat during exercise, this is not true during prolonged rest, during which they are more at risk of developing hypothermia [33]. In the elderly, the ability to self-regulate their internal temperature is also impaired due to possible pathologies affecting the cardiovascular, endocrinological and musculoskeletal systems. It should be remembered that this fragile category of patients are often polymedicated or have numerous comorbidities that can further compromise their ability to respond to cold stress.
The risk of hypothermia is also greater in malnourished patients or in those who abuse alcoholic drinks [30][31].
In addition to the aforementioned pathologies that can compromise thermogenic homeostasis, it is also important to remember patients affected by psychiatric disorders, septic/shocked patients or those whose mobility is limited by recent disabilities or injuries, who are therefore unable to implement normal behavioral mechanisms in response to the cold or who have an acutely impaired autonomic response capacity to reactions such as heat generation with muscle contraction [13][14][32][34][35].
The most common sources of temperature loss in trauma patients include exposure (environmental, as well as cavitary), the administration of i.v. fluids, anesthesia/loss of shivering mechanisms, and blood loss per se [13][18][36], but also possible brain injuries and burns. Hypothermia is one of the detrimental physiological effects that come with severe injury and hemorrhage (and thus, acidosis and coagulopathy). Awareness and the diligent screening of current body temperature in injured patients is necessary to detect, prevent and treat further temperature loss [37].
4. From Pathophysiology to Clinical Manifestations
Any situation that results in significant sudden heat loss can result in hypothermia because the mechanisms that cause heat build-up are slower [7] than the ones responsible for heat dispersion (60% of heat is lost through radiation, 10–15% through conduction and convection and 25–30% through evaporation and respiratory expiration [14]).
As already mentioned above, thermal homeostasis is performed by the regulatory center in the preoptic area of the hypothalamus and integrated by effectors of autonomous mechanisms and by behavioral attitudes. Resistance to hypothermia therefore improves both the correctness of the behavioral adaptation and the integrity of the complex regulatory center.
The main physiological responses to cold stress occur at the level of several systems and are hereby described in detail.
4.1. Cardiovascular System
In cases of mild hyperthermia, the thermoregulatory center can determine increased secretion of catecholamines following the activation of the sympathetic nervous system. The result is an increase in mean arterial pressure and cardiac output by means of tachycardia and increased peripheral resistance [38]. On the other hand, when moderate hypothermia occurs, cardiovascular function gradually deteriorates [39][40].
Cardiac conduction is also affected by hypothermia through decreased pacemaker cell activity, resulting in bradycardia [41]. This bradycardia is typically refractory to atropine, because it is not vaguely mediated [42][43]. If cold stress causes severe hypothermia, there is a risk of developing atrial and ventricular arrhythmias due to a reduction in transmembrane resting potentials [43][44][45].
4.2. Central and Peripheral Nervous Systems
Hypothermia causes a linear decrease in central nervous system metabolism as the internal body temperature decreases; more specifically, there is a decrease in oxygen consumption of about 6% for each reduction of 1 °C after the first loss [46][47][48][49]. This is reflected in a brain syndrome characterized by behavioral changes, amnesia, disorientation, dysarthria and ataxia [38]. Consciousness is progressively impaired with the progression of hypothermia.
4.3. Respiratory System
Hypothermia can affect pulmonary functions via different mechanisms: pulmonary vascular resistance is increased with increased cutaneous vasoconstriction [50][51][52].
As the exposure to cold progresses and hypothermia becomes more severe, there is a progressive decrease in tidal volume and respiratory rate, a decrease in thoracic compliance and an increase in dead space.
In the case of severe hypothermia, the control of respiration is depressed until a picture of respiratory acidosis is formed, due to tissue accumulation of CO2 [15][32][38].
4.4. Fluid Shifts, Electrolyte Balance and Kidney Function
Cold stress causes peripheral vasoconstriction with sequestration of the plasma volume and an increase in hematocrit [53]. This phenomenon, in conjunction with the loss of distal tubular water and the reabsorption of electrolytes, would determine the suppression of the release of the antidiuretic hormone, causing so-called “cold diuresis” [54].
Cold stress is also responsible for a reduction in renal oxygen consumption, compromising tubular function. In cases of severe hypoxia, the kidney is no longer able to guarantee serum levels of electrolytes, and a reduction in the tubular secretion of hydrogen ions is observed [55]. In these cases of impaired renal function, intense muscle contraction following shivering can lead to rhabdomyolysis.
4.5. Blood and Coagulation Parameters
Hypothermia can be responsible for an increased risk of thrombosis through several mechanisms [56][57][58][59]. Blood viscosity increases due to the previously discussed hematological concentration and increase in hematocrit [38][60]. Hypothermia also causes an alteration in the homeostatic enzymatic activity of coagulation factors, leading to coagulation disorders [57][61][62][63]. An increase in spontaneous platelet activation is observed at temperatures below 37 degrees Celsius, and hypothermia also causes bleeding due to thrombocytopenia following hepatic sequestration [59].
With moderate hypothermia, a reduction in fibrinogen synthesis is also observed, with a consequent increased risk of bleeding [62][64].
4.6. Endocrine and Metabolic Responses
The release of catecholamines stimulates thermogenesis when the core temperature is greater than 32 °C [65]. Catecholamine-induced glycogenolysis also induces hyperglycemia, with a decrease in insulin release, the inhibition of insulin transport (that becomes inactive at core temperatures < 31 °C), a decrease in liver enzyme function, and a decrease in the renal clearance of glucose that promotes hyperglycemia. However, glycemic levels during hypothermia have been reported to be both high and low [66], thus indicating that glycemic control is primarily dependent on the metabolic state of the patient [49][50]. Interestingly, pancreatitis is a common finding in autopsies of hypothermic patients [67].
4.7. Gastrointestinal Tract
Intestinal motility decreases below about 34.8 °C, resulting in an ileus when the temperature falls below 28.8 °C; therefore, a nasogastric tube should be placed to reduce the chance of aspiration in hypothermic patients.
The absorption of medication given orally or via a nasogastric tube will also be impaired in this situation, and this administration route should therefore be avoided. Punctate hemorrhages may occur throughout the gastrointestinal tract. Hepatic impairment can develop, probably as a consequence of reduced cardiac output, and the decreased metabolic clearance of lactic acid contributes to acidosis. Pancreatitis frequently occurs as a consequence of hypothermia, being found at autopsy in 20–30% of cases, and mildly elevated serum amylase without clinical evidence of pancreatitis is even more common, being present in 50% of patients in one series [68].
5. Clinical Diagnosis
The diagnosis of accidental hypothermia includes (i) a history or evidence of exposure to cold stress and (ii) an internal temperature < 35 °C.
For a correct diagnosis, it is necessary to use the correct instrument (thermometer). A low-reading thermometer (capable of measuring temperatures up to 25 °C) is preferred, and it should be used via the rectal, esophageal (more suitable) or bladder route. Bladder and rectal temperatures should not be used in critically ill patients during rewarming [69][70].
Tympanic temperature measurement may also represent a practical, non-invasive approach to core temperature monitoring in an emergency setting [71]. It has indeed been demonstrated that tympanic temperature is a good index of core temperature and it accurately reflects both esophageal and bladder temperatures with a very small discrepancy [72][73].
The signs and symptoms that can guide us to a diagnosis depend on the severity of hypothermia. The various physiological alterations that occur in hypothermia can be grouped summarily according to the degree of severity of the hypothermia itself [74].
In mild hypothermia, the patient is conscious and presents vigorous shivering, increased cardiac output due to increased peripheral resistance, and tachycardia; they also present tachypnoea, and in cases of the persistence of the cold stress, neurological signs such as dysarthria, ataxia and motor impediment are observed. Cold diuresis occurs secondary to peripheral vasoconstriction, which is also responsible for cold extremities and pallor. At the gastrointestinal level, cold stress can lead to the formation of gastric ulcers and pancreatitis. For what concerns the blood system, the risk of thrombosis due to hemoconcentration and the risk of bleeding due to the inactivation of coagulation factors are already seen in the early stages of hypothermia.
Moderate hypothermia is characterized by decreased cardiac output and blood pressure, hypoventilation and hyporeflexia. The loss of the shivering mechanism is also observed. The resulting picture ranges from an impairment of mental function up to a loss of consciousness. The gross impairment of motor control, cessation of shivering, cyanosis, muscle rigidity, mydriasis, atrial or ventricular cardiac dysrhythmias and bradycardia also occur. In this phase, the behavioral defenses are compromised in some subjects, who paradoxically undress.
If the cold stress perdures, or if the regulatory mechanisms are so compromised as to progress to a state of severe hypothermia, the patient may present in a state of shock or pre-shock with hypotension, pulmonary congestion, edema, muscle rigidity, areflexia, oliguria and coma.
Tissues have decreased oxygen consumption at lower temperatures; at 28 °C, oxygen consumption is reduced by about 50%, and at 22 °C by about 75%.
More severe pictures include spontaneous ventricular fibrillation and cardiac arrest. [75] Severe cases can mimic death. At 18 °C, the brain can tolerate ten times longer periods of cardiac arrest than at 37 °C. When faced with a patient in cardiac arrest who is hypothermic, it is important to remember that they should not be declared dead until they have been rewarmed [10][11][12][32][34].
When the core temperature cannot readily be measured, the Swiss staging system, which distinguishes among five levels of hypothermia based on clinical appearance, can be a useful tool to determine the severity of hypothermia:
References
- Hypothermia: Background, Pathophysiology, Etiology. Available online: https://emedicine.medscape.com/article/770542-overview (accessed on 15 August 2023).
- Petrone, P.; Asensio, J.A.; Marini, C.P. In brief: Hypothermia. Curr. Probl. Surg. 2014, 51, 414–415.
- Epstein, E.; Anna, K. Accidental shypothermia. BMJ 2006, 332, 706–709.
- Spencer, M.R.; Hedegaard, H.B. QuickStats: Death Rates* Attributed to Excessive Cold or Hypothermia† Among Persons Aged ≥15 Years, by Urban-Rural Status§ and Age Group—National Vital Statistics System, United States, 2019. MMWR Morb. Mortal. Wkly. Rep. 2021, 70, 258.
- van Veelen, M.J.; Brodmann Maeder, M. Hypothermia in Trauma. Int. J. Environ. Res. Public Health 2021, 18, 8719.
- Luna, G.K.; Maier, R.V.; Pavlin, E.G.; Anardi, D.; Copass, M.K.; Oreskovich, M.R. Incidence and effect of hypothermia in seriously injured patients. J. Trauma 1987, 27, 1014–1018.
- Forristal, C.; Van Aarsen, K.; Columbus, M.; Wei, J.; Vogt, K.; Mal, S. Predictors of Hypothermia upon Trauma Center Arrival in Severe Trauma Patients Transported to Hospital via EMS. Prehosp. Emerg. Care 2020, 24, 15–22.
- Meiman, J.; Anderson, H.; Tomasallo, C.; Centers for Disease Control and Prevention (CDC). Hypothermia-related deaths—Wisconsin, 2014, and United States, 2003–2013. MMWR Morb. Mortal. Wkly. Rep. 2015, 64, 141–143.
- Cheshire, W.P., Jr. Thermoregulatory disorders and illness related to heat and cold stress. Auton. Neurosci. 2016, 196, 91–104.
- Polderman, K.H. Mechanisms of action, physiological effects, and complications of hypothermia. Crit. Care Med. 2009, 37 (Suppl. 7), S186–S202.
- Cappaert, T.A.; Stone, J.A.; Castellani, J.W.; Krause, B.A.; Smith, D.; Stephens, B.A. National Athletic Trainers’ Association Position Statement: Environmental Cold Injuries. J. Athl. Train. 2008, 43, 640–658.
- Jurkovich, G.J. Environmental Cold-Induced Injury. Surg. Clin. N. Am. 2007, 87, 247–267.
- Ulrich, A.S.; Rathlev, N.K. Hypothermia and localized cold injuries. Emerg. Med. Clin. N. Am. 2004, 22, 281–298.
- Giesbrecht, G.G. Cold stress, near drowning and accidental hypothermia: A review. Aviat. Space Environ. Med. 2000, 71, 733–752.
- Durrer, B.; Brugger, H.; Syme, D.; Elsensohn, F.; Deslarzes, T.; Yersin, B.; Paal, P.; Gordon, L.; Strapazzon, G.; Maeder, M.B.; et al. The Medical On-site Treatment of Hypothermia: ICAR-MEDCOM Recommendation. High Alt. Med. Biol. 2003, 4, 99–103.
- Long, W.B.; Edlich, R.F.; Winters, K.L.; Britt, L.D. Cold injuries. J. Long Term Eff. Med. Implant. 2005, 15, 67–78.
- Søreide, K. Clinical and translational aspects of hypothermia in major trauma patients: From pathophysiology to prevention, prognosis and potential preservation. Injury 2014, 45, 647–654.
- Schumacker, P.T.; Rowland, J.; Saltz, S.; Nelson, D.P.; Wood, L.D. Effects of hyperthermia and hypothermia on oxygen extraction by tissues during hypovolemia. J. Appl. Physiol. 1987, 63, 1246–1252.
- D’Angelo, J. Treating heat-related illness in the elderly. Emerg. Med. Serv. 2004, 33, 111–113.
- Morrison, S.F.; Nakamura, K. Central Mechanisms for Thermoregulation. Annu. Rev. Physiol. 2019, 81, 285–308.
- Romanovsky, A.A. The thermoregulation system and how it works. Handb. Clin. Neurol. 2018, 156, 3–43.
- Osilla, E.V.; Marsidi, J.L.; Sharma, S. Physiology, Temperature Regulation; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: http://www.ncbi.nlm.nih.gov/books/NBK507838/ (accessed on 15 August 2023).
- Atha, W.F. Heat-related illness. Emerg. Med. Clin. N. Am. 2013, 31, 1097–1108.
- Severe Recurrent Hypothermia in an Elderly Patient with Refractory Mania Associated with Atypical Antipsychotic, Valproic Acid and Oxcarbazepine Therapy|BMJ Case Reports. Available online: https://casereports.bmj.com/content/2017/bcr-2017-222462 (accessed on 17 August 2023).
- Rumbus, Z.; Garami, A. Fever, hypothermia, and mortality in sepsis. Temperature 2018, 6, 101–103.
- Fox, R.H.; Shuster, S.; Williams, R.; Marks, J.; Goldsmith, R.; Condon, R.E. Cardiovascular, Metabolic, and Ther Moregulatory Disturbances in Patients with Erythrodermic Skin Diseases. Br. Med. J. 1965, 1, 619–622.
- Cucinell, S.A. Hypothermia and Generalized Skin Disease. Arch. Dermatol. 1978, 114, 1244–1245.
- Krook, G. Hypothermia in patients with exfoliative dermatitis. Acta Derm. Venereol. 1960, 40, 142–160.
- Kalant, H.; Lê, A. Effects of ethanol on thermoregulation. Pharmacol. Ther. 1983, 23, 313–364.
- Ristuccia, R.C.; Hernandez, M.; Wilmouth, C.E.; Spear, L.P. Differential Expression of Ethanol-Induced Hypothermia in Adolescent and Adult Rats Induced by Pretest Familiarization to the Handling/Injection Procedure. Alcohol. Clin. Exp. Res. 2007, 31, 575–581.
- Brown, D.J.A.; Brugger, H.; Boyd, J.; Paal, P. Accidental hypothermia. N. Engl. J. Med. 2012, 367, 1930–1938.
- Périard, J.D.; Eijsvogels, T.M.H.; Daanen, H.A.M. Exercise under heat stress: Thermoregulation, hydration, performance implications, and mitigation strategies. Physiol. Rev. 2021, 101, 1873–1979.
- Biem, J.; Koehncke, N.; Classen, D.; Dosman, J. Out of the cold: Management of hypothermia and frostbite. CMAJ 2003, 168, 305–311.
- Hislop, L.J.; Wyatt, J.P.; McNaughton, G.W.; Ireland, A.J.; Rainer, T.H.; Olverman, G.; Laughton, L.M. Urban hypothermia in the west of Scotland. West of Scotland Accident and Emergency Trainees Research Group. BMJ 1995, 311, 725.
- Tsuei, B.J.; Kearney, P.A. Hypothermia in the trauma patient. Injury 2004, 35, 7–15.
- Ireland, S.; Endacott, R.; Cameron, P.; Fitzgerald, M.; Paul, E. The incidence and significance of accidental hypothermia in major trauma—A prospective observational study. Resuscitation 2011, 82, 300–306.
- Danzl, D.F.; Pozos, R.S. Accidental hypothermia. N. Engl. J. Med. 1994, 331, 1756–1760.
- Deussen, A. Hyperthermia and hypothermia. Effects on the cardiovascular system. Anaesthesist 2007, 56, 907–911.
- Brooks, D.P.; Chapman, B.J.; Munday, K.A. The Effect of Hypothermia on the Cardiovascular System and the Pressor Actions of Angiotensin II. J. Therm. Biol. 1984, 9, 243–246.
- Dietrichs, E.S.; McGlynn, K.; Allan, A.; Connolly, A.; Bishop, M.; Burton, F.; Kettlewell, S.; Myles, R.; Tveita, T.; Smith, G.L. Moderate but not severe hypothermia causes pro-arrhythmic changes in cardiac electrophysiology. Cardiovasc. Res. 2020, 116, 2081–2090.
- Prec, O.; Rosenman, R.; Braun, K.; Rodbard, S.; Katz, L.N. The cardiovascular effects of acutely induced hypothermia. J. Clin. Investig. 1949, 28, 293–300.
- Covino, B.G.; D’Amato, H.E. Mechanism of Ventricular Fibrillation in Hypothermia. Circ. Res. 1962, 10, 148–155.
- Bjørnstad, H.; Tande, P.M.; Refsum, H. Cardiac electrophysiology during hypothermia. Implications for medical treatment. Arctic Med. Res. 1991, 50 (Suppl. 6), 71–75.
- Roscher, R.; Arlock, P.; Sjöberg, T.; Steen, S. Effects of dopamine on porcine myocardial action potentials and contractions at 37 degrees C and 32 degrees C. Acta Anaesthesiol. Scand. 2001, 45, 421–426.
- Ehrlich, M.P.; McCullough, J.N.; Zhang, N.; Weisz, D.J.; Juvonen, T.; Bodian, C.A.; Griepp, R.B. Effect of hypothermia on cerebral blood flow and metabolism in the pig. Ann. Thorac. Surg. 2002, 73, 191–197.
- McCullough, J.N.; Zhang, N.; Reich, D.L.; Juvonen, T.S.; Klein, J.J.; Spielvogel, D.; Ergin, M.; Griepp, R.B. Cerebral metabolic suppression during hypothermic circulatory arrest in humans. Ann. Thorac. Surg. 1999, 67, 1895–1899.
- Yager, J.Y.; Asselin, J. Effect of Mild Hypothermia on Cerebral Energy Metabolism During the Evolution of Hypoxic-Ischemic Brain Damage in the Immature Rat. Stroke 1996, 27, 919–926.
- Erecinska, M.; Thoresen, M.; Silver, I.A. Effects of Hypothermia on Energy Metabolism in Mammalian Central Nervous System. J. Cereb. Blood Flow Metab. 2003, 23, 513–530.
- Frappell, P. Experimental Biology 1997 Symposium on Neurobiology of Thermoregulation: Role of Stress: Hypothermia and physiological control: The respiratory system. Clin. Exp. Pharmacol. Physiol. 1998, 25, 159–164.
- Dill, D.B.; Forbes, W.H. Respiratory and metabolic effects of hypothermia. Am. J. Physiol. Leg. Content 1941, 132, 685–697.
- Taiji, S.; Nishino, T.; Jin, H.; Shinozuka, N.; Isono, S.; Nozaki-Taguchi, N. Changes in breathing pattern during severe hypothermia and autoresuscitation from hypothermic respiratory arrest in anesthetized mice. Physiol. Rep. 2021, 9, e15139.
- D’Amato, H.E.; Hegnauer, A.H. Blood Volume in the Hypothermic Dog. Am. J. Physiol. Content 1953, 173, 100–102.
- Moyer, J.H. The effect of hypothermia on renal function and renal damage from ischemia. Ann. N. Y. Acad. Sci. 1959, 80, 424–434.
- Rosenfeld, J.B. Acid-base and electrolyte disturbances in hypothermia. Am. J. Cardiol. 1963, 12, 678–682.
- Sharma, T.; Kunkes, J.; O’Sullivan, D.; Fernandez, A.B. Elevated risk of venous thromboembolism in patients undergoing therapeutic hypothermia after cardiac arrest. Resuscitation 2021, 162, 251–256.
- Polderman, K.H. Hypothermia and coagulation. Crit. Care 2012, 16 (Suppl. 2), A20.
- Li, L.; Chen, X.; Ma, W.; Li, Y. The effects of hypothermia in thrombosis: A systematic review and meta-analysis. Ann. Palliat. Med. 2021, 10, 9564–9571.
- Van Poucke, S.; Stevens, K.; Marcus, A.E.; Lancé, M. Hypothermia: Effects on platelet function and hemostasis. Thromb. J. 2014, 12, 31.
- Paal, P.; Brugger, H.; Boyd, J. Accidental hypothermia. N. Engl. J. Med. 2013, 368, 682.
- Rohrer, M.J.; Natale, A.M. Effect of hypothermia on the coagulation cascade. Crit. Care Med. 1992, 20, 1402–1405.
- Watts, D.D. Hypothermic Coagulopathy in Trauma: Effect of Varying Levels of Hypothermia on Enzyme Speed, Platelet Function and Fibrinolytic Activity. 1997. Available online: https://archive.hshsl.umaryland.edu/handle/10713/1405 (accessed on 15 August 2023).
- Martini, W.Z. Coagulopathy by Hypothermia and Acidosis: Mechanisms of Thrombin Generation and Fibrinogen Availability. J. Trauma Inj. Infect. Crit. Care 2009, 67, 202–209.
- Watts, D.D.; Trask, A.; Soeken, K.; Perdue, P.; Dols, S.; Kaufmann, C. Hypothermic Coagulopathy in Trauma: Effect of Varying Levels of Hypothermia on Enzyme Speed, Platelet Function, and Fibrinolytic Activity. J. Trauma Acute Care Surg. 1998, 44, 846.
- Gale, E.A.M.; Bennett, T.; Green, J.H.; MacDonald, I.A. Hypoglycaemia, Hypothermia and Shivering in Man. Clin. Sci. 1981, 61, 463–469.
- Strapazzon, G.; Nardin, M.; Zanon, P.; Kaufmann, M.; Kritzinger, M.; Brugger, H. Respiratory Failure and Spontaneous Hypoglycemia During Noninvasive Rewarming From 24.7 °C (76.5 °F) Core Body Temperature After Prolonged Avalanche Burial. Ann. Emerg. Med. 2012, 60, 193–196.
- Savides, E.P.; Hoffbrand, B.I. Hypothermia, thrombosis, and acute pancreatitis. Br. Med. J. 1974, 1, 614.
- Castellani, J.W.; Young, A.J.; Ducharme, M.B.; Giesbrecht, G.G.; Glickman, E.; Sallis, R.E.; American College of Sports Medicine. American College of Sports Medicine position stand: Prevention of cold injuries during exercise. Med. Sci. Sports Exerc. 2006, 38, 2012–2029.
- Buchanan, J.T.; Thurman, J. EMS Management of Traumatic and Medical Disorders in a Wilderness Environment; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: http://www.ncbi.nlm.nih.gov/books/NBK553188/ (accessed on 15 August 2023).
- Dow, J.; Giesbrecht, G.G.; Danzl, D.F.; Brugger, H.; Sagalyn, E.B.; Walpoth, B.; Auerbach, P.S.; McIntosh, S.E.; Némethy, M.; McDevitt, M.; et al. Wilderness Medical Society Clinical Practice Guidelines for the Out-of-Hospital Evaluation and Treatment of Accidental Hypothermia: 2019 Update. Wilderness Environ. Med. 2019, 30, S47–S69.
- Masè, M.; Micarelli, A.; Falla, M.; Regli, I.B.; Strapazzon, G. Insight into the use of tympanic temperature during target temperature management in emergency and critical care: A scoping review. J. Intensiv. Care 2021, 9, 43.
- Hasper, D.; Nee, J.; Schefold, J.C.; Krueger, A.; Storm, C. Tympanic temperature during therapeutic hypothermia. Emerg. Med. J. 2010, 28, 483–485.
- Childs, C.; Harrison, R.; Hodkinson, C. Tympanic membrane temperature as a measure of core temperature. Arch. Dis. Child. 1999, 80, 262–266.
- Duong, H.; Patel, G. Hypothermia; StatPearls Publishing: Treasure Island, FL, USA, 2023. Available online: http://www.ncbi.nlm.nih.gov/books/NBK545239/ (accessed on 17 August 2023).
- Reed, R.L.; Johnston, T.D.; Hudson, J.D.; Fischer, R.P. The disparity between hypothermic coagulopathy and clotting studies. J. Trauma Inj. Infect. Crit. Care 1992, 33, 465–470.
- Brändström, H.; Johansson, G.; Giesbrecht, G.G.; Ängquist, K.-A.; Haney, M.F. Accidental Cold-Related Injury Leading to Hospitalization in Northern Sweden: An Eight-Year Retrospective Analysis. Scand. J. Trauma Resusc. Emerg. Med. 2014, 22, 6.
More
Information
Subjects:
Emergency Medicine
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
1.3K
Revision:
1 time
(View History)
Update Date:
19 Jan 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





