1000/1000
Hot
Most Recent

Chronic neuropathic pain (NP) is an increasingly prevalent disease and leading cause of disability which is challenging to treat. Several distinct classes of drugs are currently used for the treatment of chronic NP, but each drug targets only narrow components of the underlying pathophysiological mechanisms, bears limited efficacy, and comes with dose-limiting side effects. Multimodal therapies have been increasingly proposed as potential therapeutic approaches to target the multiple mechanisms underlying nociceptive transmission and modulation. However, while preclinical studies with combination therapies showed promise to improve efficacy over monotherapy, clinical trial data on their efficacy in specific populations are lacking and increased risk for adverse effects should be carefully considered. Drug-drug co-crystallization has emerged as an innovative pharmacological approach which can combine two or more different active pharmaceutical ingredients in a single crystal, optimizing pharmacokinetic and physicochemical characteristics of the native molecules, thus potentially capitalizing on the synergistic efficacy between classes of drugs while simplifying adherence and minimizing the risk of side effects by reducing the doses.
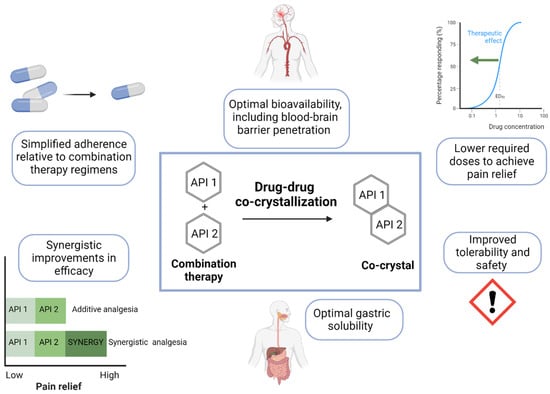
The heterogenous and multimodal nature of chronic NP makes it a very challenging condition to treat. The underlying etiology of a given peripheral or central NP condition is important to consider in selecting optimal treatment regimens or assessing new data regarding novel therapeutic approaches like those described here. Currently available analgesics are associated with significant safety concerns, including renal toxicity, gastrointestinal toxicity, cardiotoxicity, nephrotoxicity, and abuse liability, underscoring the need to fine-tune the balance of the risk/benefit ratio and closely monitor the tolerability of doses and durations of current treatment prescribed. Multimodal therapeutic approaches represent an important step forward in improving patient outcomes. Drug-drug co-crystallization has the potential to offer several key advantages over combination therapy regimens in this context, improving physicochemical and pharmacokinetic properties of the existing molecules and conveying consequent higher efficacy and/or reduced dose requirements superior to those achieved with combination therapy of the single agents. Critically, the selection of APIs with pharmacodynamic profiles suitable for synergistic efficacy and physicochemical properties which align with stoichiometric constraints is challenging [128]. There are limited examples of drug-drug co-crystals in the pain area that have been published thus far [118].