
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Hideaki Kanemura | -- | 2632 | 2024-01-15 09:14:01 | | | |
| 2 | Catherine Yang | Meta information modification | 2632 | 2024-01-15 09:52:31 | | |
Video Upload Options
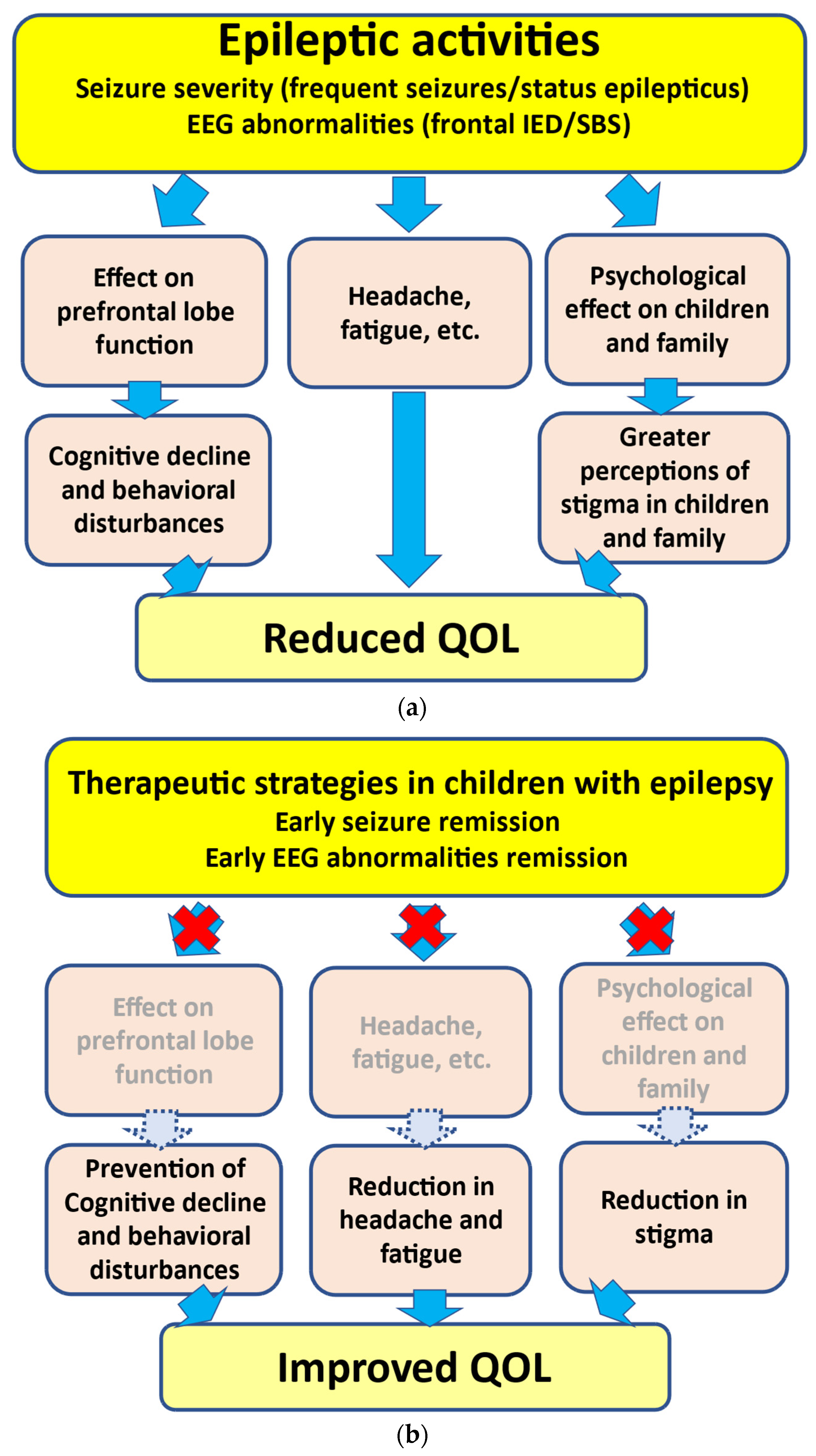
Children with epilepsy are affected by several factors, including clinical and social variables. Among these variables, cognitive decline and behavioral disturbances, perceptions of stigma, and fatigue can lead to reductions in quality of life (QOL). Epileptic activities, including seizure severity, frequent seizures, and status epilepticus (SE), have been identified as important predictors of QOL. In addition, the frequency of interictal epileptiform discharges (IEDs) on electroencephalogram (EEG) may also be an important predictor of QOL, because IEDs can lead to cognitive decline and behavioral disturbances. Moreover, frequent seizures and/or IEDs may play a role in emotional mediators, such as stigma and fatigue, in childhood epilepsy. Seizure severity and/or IEDs are, therefore, important QOL-related factors in childhood epilepsy.
1. Introduction
2. Seizure Severity in Childhood Epilepsy
2.1. Seizure Severity and Cognitive/Behavioral Disturbances
2.1.1. Prefrontal Lobe Growth in Frontal Lobe Epilepsy
| Epileptic Syndrome | Findings |
|---|---|
| Frontal lobe epilepsy (FLE) | # Frontal/prefrontal lobe volumes and the prefrontal-to-frontal lobe volume ratio increased serially in the drug-responsive FLE patients without cognitive decline/behavioral disturbances and non-epilepsy children. # Frontal and prefrontal lobe growth disturbances were present during the active seizure period in the refractory FLE patients with cognitive decline and behavioral disturbances. # Active seizure period was short in children with prompt growth recovery. # The growth disturbance was more severe, and the growth recovery was required a long time in children with a longer active seizure period. |
| Self-limited epilepsy with centrotemporal spikes (SeLECTS) | # Frontal and prefrontal lobe growth disturbances were present during the active seizure period in patients presenting atypical evolution. # The growth disturbance was more severe, and the growth recovery was required a long time in a patient with a longer active seizure period. |
| Self-limited epilepsy with autonomic seizures (SeLEAS) | # Frontal and prefrontal lobe growth disturbances were present after episodes of SE in SeLEAS patients presenting with behavioral disturbances. # In a patient with only one episode of SE, growth disturbance soon recovered. # Conversely, recovery of growth ratios was delayed in patients with several episodes of SE. |
2.1.2. Prefrontal Lobe Growth in SeLECTS
2.1.3. Prefrontal Lobe Growth in Self-Limited Epilepsy with Autonomic Seizures
2.2. QOL-Related Factors: Headache
| QOL-Related Factors | Findings |
|---|---|
| Headache | # The frequency of seizures was 4.1 times per year in children with seizure-associated headache. # The frequency of seizures was 1.3 times per year in those with non-seizure-associated headache. # Frequent seizures may be in association with seizure-associated headache. |
| Fatigue | # The mean Fatigue Severity Scale scores of the children with epilepsy were significantly higher than those of the non-epilepsy children. # Frequency of seizures was sole significant clinical manifestation in association with fatigue. # A higher frequency of seizures was associated with more severe fatigue. |
| Stigma in children | # Children with frequent seizures presented psychosocial impairments in comparison with seizure-remission children. # Greater perceptions of stigma were in association with greater frequency of seizures. |
| Stigma in parents | # Parents of children with epilepsy showed significantly higher scores on the questionnaire than those of non-epilepsy children. # Greater perceptions of stigma were in association with frequency of seizures. |
2.3. QOL-Related Factors: Fatigue
2.4. QOL-Related Factors: Perception of Stigma among Children
2.5. QOL-Related Factors: Perception of Stigma among Parents
3. The Treatment of Epilepsy in Children
3.1. Is the Urgent Suppression of Clinical Seizures Needed?
3.2. Is the Urgent Suppression of IEDs on EEG Needed?
3.3. Therapeutic Strategies in Children with Epilepsy
References
- Terra, V.C.; Furlanetti, L.L.; Nunes, A.A.; Thome, U.; Nishiyama, M.A.; Sakamoto, A.C.; Machado, H.R. Vagus nerve stimulation in pediatric patients: Is it really worthwhile? Epilepsy Behav. 2014, 31, 329–333.
- Chung, S.; Szaflarski, J.P.; Choi, E.J.; Wilson, J.C.; Kharawara, S.; Kauer, G.; Hirsch, L.J. A systematic review of seizure clusters: Prevalence, risk factors, burden of disease and treatment patterns. Epilepsy Res. 2021, 177, 106748.
- Kanemura, H.; Sano, F.; Tando, T.; Sugita, K.; Aihara, M. Repeated seizures induce prefrontal growth disturbance in frontal lobe epilepsy. Brain Dev. 2012, 34, 175–180.
- Kanemura, H.; Sano, F.; Ohyama, T.; Aoyagi, K.; Sugita, K.; Aihara, M. Sequential prefrontal lobe volume changes and cognitive dysfunctions in children with Panayiotopoulos syndrome presenting with status epilepticus. Epilepsy Res. 2015, 112, 122–129.
- Binnie, C.D. Cognitive impairment during epileptiform discharges: Is it ever justifiable to treat the EEG? Lancet Neurol. 2003, 2, 725–730.
- Aydemir, N.; Ozkara, C.; Unsal, P.; Canbeyli, R. A comparative study of health related quality of life, psychological well-being, impact of illness and stigma in epilepsy and migraine. Seizure 2011, 20, 679–685.
- Espinola-Nadurille, M.; Crail-Melendez, D.; Sanchez-Guzman, M.A. Stigma experience of people with epilepsy in Mexico and views of health care providers. Epilepsy Behav. 2014, 32, 162–169.
- Hamelin, S.; Kahane, P.; Vercueil, L. Fatigue in epilepsy: A prospective inter-ictal and post-ictal survey. Epilepsy Res. 2010, 91, 153–160.
- Hernandez-Ronquillo, L.; Moien-Afshari, F.; Knox, K.; Britz, J.; TellezZenteno, J.F. How to measure fatigue in epilepsy? The validation of three scales for clinical use. Epilepsy Res. 2011, 95, 119–129.
- Weglage, J.; Demsky, A.; Pietsch, M.; Kurlemann, G. Neuropsychological, intellectual, and behavioral findings in patients with centrotemporal spikes with and without seizures. Dev. Med. Child Neurol. 1997, 39, 646–651.
- Hoare, P. The development of psychiatric disorder among school children with epilepsy. Dev. Med. Child Neurol. 1984, 26, 3–13.
- Austin, J.K.; Risinger, M.W.; Beckett, L.A. Correlates of behavior problems in children with epilepsy. Epilepsia 1992, 33, 1115–1122.
- Holmes, G.L.; Ben-Ari, Y. The neurobiology and consequences of epilepsy in the developing brain. Pediatr. Res. 2001, 49, 320–325.
- Kanemura, H.; Hata, S.; Aoyagi, K.; Sugita, K.; Aihara, M. Serial changes of prefrontal lobe growth in the patients with benign childhood epilepsy with centrotemporal spikes presenting with cognitive impairments/behavioral problems. Brain Dev. 2011, 33, 106–113.
- Sinclair, D.B.; Wheatley, M.; Snyder, T. Frontal lobe epilepsy in childhood. Pediatr. Neurol. 2004, 30, 169–176.
- Williamson, P.D.; Spencer, D.D.; Spencer, S.S.; Novelly, R.A.; Mattson, R.H. Complex partial seizures of frontal lobe origin. Ann. Neurol. 1985, 18, 497–504.
- Engel, J., Jr.; Williamson, P.D.; Wieser, H.G. Mesial temporal lobe epilepsy with hippocampal sclerosis. In Epilepsy. A Comprehensive Textbook, 2nd ed.; Engel, J., Pedley, T., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2008; pp. 2479–2486.
- Fejerman, N.; Caraballo, R.H. Early-onset benign childhood occipital epilepsy (Panayiotopoulos type). In Benign Focal Epilepsies in Infancy, Childhood and Adolescence; Fejerman, N., Caraballo, R.H., Eds.; John Libbey Eurotext: Montrouge, France, 2007; pp. 115–144.
- Andermann, F. Clinical features of migraine–epilepsy syndrome. In Migraine and Epilepsy; Andermann, F., Lugaresi, E., Eds.; Butterworths: Boston, MA, USA, 1987; pp. 3–30.
- Kanemura, H.; Sano, F.; Ishii, S.; Ohyama, T.; Sugita, K.; Aihara, M. Characteristics of headache in children with epilepsy. Seizure 2013, 22, 647–650.
- Vercoulen, J.H.; Hommes, O.R.; Swanink, C.M.; Jongen, P.J.; Fennis, J.F.; Galama, J.M.; van der Meer, J.W.M.; Bleijenberg, G. The measurement of fatigue in patients with multiple sclerosis. A multidimensional comparison with chronic fatigue syndrome and healthy subjects. Arch. Neurol. 1996, 53, 642–649.
- Dittner, A.J.; Wessely, S.C.; Brown, R.G. The assessment of fatigue: A practical guide for clinicians and researchers. J. Psychosom. Res. 2004, 56, 157–170.
- Christensen, D.; Johnsen, S.P.; Watt, T.; Harder, I.; Kirkevold, M.; Andersen, G. Dimensions of post-stroke fatigue: A two-year follow-up study. Cerebrovasc. Dis. 2008, 26, 134–141.
- Kanemura, H.; Sano, F.; Ohyama, T.; Sugita, K.; Aihara, M. Association between seizure frequency and fatigue levels in children with epilepsy. J. Paediatr. Child Health 2018, 54, 1336–1340.
- Jacoby, A.; Baker, G.; Smith, D.; Dewey, M.; Chadwick, D. Measuring the impact of epilepsy: The development of a novel scale. Epilepsy Res. 1993, 16, 83–88.
- Rodenburg, R.; Meijer, A.M.; Dekovic, M.; Aldenkamp, A.P. Parents of children with enduring epilepsy: Predictions of parenting stress and parenting. Epilepsy Behav. 2007, 11, 197–207.
- Modi, A.C. The impact of a new pediatric epilepsy diagnosis on parents: Parenting stress and activity patterns. Epilepsy Behav. 2008, 13, 169–173.
- Chiou, H.H.; Hsieh, L.P. Parenting stress in patients of children with epilepsy and asthma. J. Child Neurol. 2008, 23, 301–306.
- Cushner-Weinstein, S.; Dassoulas, K.; Salpekar, J.A.; Henderson, S.E.; Pearl, P.L.; Gaillard, W.D.; Weinstein, S.L. Parenting stress and childhood epilepsy: The impact of depression, learning, and seizure-related factors. Epilepsy Behav. 2008, 13, 109–114.
- Kerne, V.; Chapieski, L. Adaptive functioning in pediatric epilepsy: Contributions of seizure-related variables and parental anxiety. Epilepsy Behav. 2015, 43, 48–52.
- Braams, O.; Meekes, J.; Braun, K.; Schappin, R.; van Rijen, P.C.; Hendriks, M.P.H.; Jennekens-Schinkel, A.; van Nieuwenhuizen, O. Parenting stress does not normalize after child’s epilepsy surgery. Epilepsy Behav. 2015, 42, 147–152.
- Kanemura, H.; Sano, F.; Ohyama, T.; Sugita, K.; Aihara, M. Seizure severity in children with epilepsy is associated with their parents’ perception of stigma. Epilepsy Behav. 2016, 63, 42–45.
- Austin, J.K.; Dunn, D.W.; Caffrey, H.M.; Perkins, S.M.; Harezlak, J.; Rose, D.F. Recurrent seizures and behavior problems in children with first recognized seizures: A prospective study. Epilepsia 2002, 43, 1564–1573.
- Aihara, M.; Aoyagi, K.; Goldberg, E.; Nakazawa, S. Age shifts frontal cortical control in a cognitive bias task from right to left: Part I. Neuropsychological study. Brain Dev. 2003, 25, 555–559.
- Kanemura, H.; Sano, F.; Aoyagi, K.; Sugita, K.; Aihara, M. Do sequential EEG changes predict atypical clinical features in rolandic epilepsy? Dev. Med. Child Neurol. 2012, 54, 912–917.
- Kanemura, H.; Sano, F.; Tando, T.; Hosaka, H.; Sugita, K.; Aihara, M. EEG improvements with antiepileptic drug treatment can show a high correlation with behavior recovery in children with ADHD. Epilepsy Behav. 2013, 27, 443–448.
- Kanemura, H.; Sano, F.; Hoshino, H.; Aihara, M. Efficacy of perampanel in epilepsy patients with autism spectrum disorder. Epilepsy Res. 2021, 170, 106550.
- Kanemura, H.; Sano, F.; Ohyama, T.; Sugita, K.; Aihara, M. Effect of levetiracetam on behavioral problems in pervasive developmental disorder children with epilepsy. Eur. J. Paediatr. Neurol. 2014, 18, 482–488.
- De Negri, M.; Baglietto, M.G.; Battaglia, F.M.; Gaggero, R.; Pessagno, A.; Recanati, L. Treatment of electrical status epilepticus by short diazepam (DZP) cycles after DZP rectal bolus test. Brain Dev. 1995, 17, 330–333.
- Morikawa, T.; Seino, M.; Yagi, K. Long-term outcome of four children with continuous spike-waves during sleep. In Epileptic Syndromes in Infancy, Childhood and Adolescence, 2nd ed.; Roger, J., Bureau, M., Dravet, C.H., Dreifuss, F.E., Perret, A., Wolf, P., Eds.; John Libbey: London, UK, 1992; pp. 257–266.
- Kanemura, H.; Sano, F.; Hoshino, H.; Takayama, K.; Aihara, M. Effects of perampanel on secondary bilateral synchrony and behavioral problems in adolescents with epilepsy showing insufficient response with levetiracetam. Seizure 2020, 80, 131–137.
- Kanemura, H.; Aihara, M. Neurobiological effects of CSWS on brain growth: A magnetic resonance imaging volumetric study. J. Pediatr. Epilepsy 2012, 1, 187–193.
- Stodieck, S.; Steinhoff, B.J.; Kolmsee, S.; Van Rijckevorsel, K. Effect of levetiracetam in patients with epilepsy and interictal epileptiform discharges. Seizure 2001, 10, 583–587.
- Kanemura, H.; Sano, F.; Ohyama, T.; Aihara, M. Efficacy of levetiracetam for reducing rolandic discharges in comparison with carbamazepine and valproate sodium in rolandic epilepsy. Seizure 2018, 62, 79–83.
- Wu, T.; Ido, K.; Ohgoh, M.; Hanada, T. Mode of seizure inhibition by sodium channel blockers, an SV2A ligand, and an AMPA receptor antagonist in a rat amygdala kindling model. Epilepsy Res. 2019, 154, 42–49.




