Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Stoyan Kostov | -- | 1692 | 2024-01-13 10:44:15 | | | |
| 2 | Catherine Yang | Meta information modification | 1692 | 2024-01-15 01:56:35 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Kostov, S.; Sorokin, P.; Rezende, B.; Yalçın, H.; Selçuk, I. Ontogenetic Anatomy. Encyclopedia. Available online: https://encyclopedia.pub/entry/53797 (accessed on 08 February 2026).
Kostov S, Sorokin P, Rezende B, Yalçın H, Selçuk I. Ontogenetic Anatomy. Encyclopedia. Available at: https://encyclopedia.pub/entry/53797. Accessed February 08, 2026.
Kostov, Stoyan, Pavel Sorokin, Bruno Rezende, Hakan Yalçın, Ilker Selçuk. "Ontogenetic Anatomy" Encyclopedia, https://encyclopedia.pub/entry/53797 (accessed February 08, 2026).
Kostov, S., Sorokin, P., Rezende, B., Yalçın, H., & Selçuk, I. (2024, January 13). Ontogenetic Anatomy. In Encyclopedia. https://encyclopedia.pub/entry/53797
Kostov, Stoyan, et al. "Ontogenetic Anatomy." Encyclopedia. Web. 13 January, 2024.
Copy Citation
Ontogenetic anatomy is a relatively novel concept based on embryologic development. During early embryologic development, the proliferating groups of cells do not mix with each other. They form units—ontogenetic compartments—which can be identified and mapped in mature organisms. The ontogenetic cancer field model was developed by Höckel and considered malignant tumor growth as an anisotropic process. According to the theory, tumor growth is confined by a permissive compartment during the long time of its natural history, and the compartment’s borders are tumor suppressive. It is also a predictive model, which contributes to selecting the proper surgical procedure for every single patient according to the probability of the compartment’s involvement. The term “meso” is widely used in ontogenetic surgery. It is an abbreviation of “mesentery”, which differs from the classical anatomical definition. In general, the term “mesentery” means the structure attaches the organ to the posterior abdominal wall and is covered by the peritoneum on both sides. In ontogenetic anatomy, the prefix “meso-” defines a compartment derived from distinct primordial tissue. Mesotissues abut the corresponding organ, although their origin differs from the organ. It contains fibro-fatty tissue, blood vessels, lymphatics, and nerves. Sometimes, meso-structures are enveloped by an easily dissectible fascia (e.g., mesorectum and mesorectal fascia); in other cases, it could not be dissected in an avascular plane and the related veins may communicate between different compartments (e.g., the Mullerian compartment and mesobladder).
ontogenic anatomy
parametrium
inferior hypogastric plexus
mesometrium
1. Ontogenetic Anatomy and Total Mesometrial Resection
Any tissue in a mature organism can be identified according to its developmental mapping. In the female pelvis, the embryological margins and tissue planes of these compartments are more or less apparent [1][2][3]. One of the most obvious borders is the mesorectal fascia. The mesorectal fascia envelopes the mesorectum circumferentially and can be sharply dissected. The mesorectal ontogenetic compartment is formed from the hindgut—the posterior part of the alimentary canal (Figure 1) [4]. The clinical translation of this knowledge is the total mesorectal excision (TME)—the current standard of rectal carcinoma treatment [5].
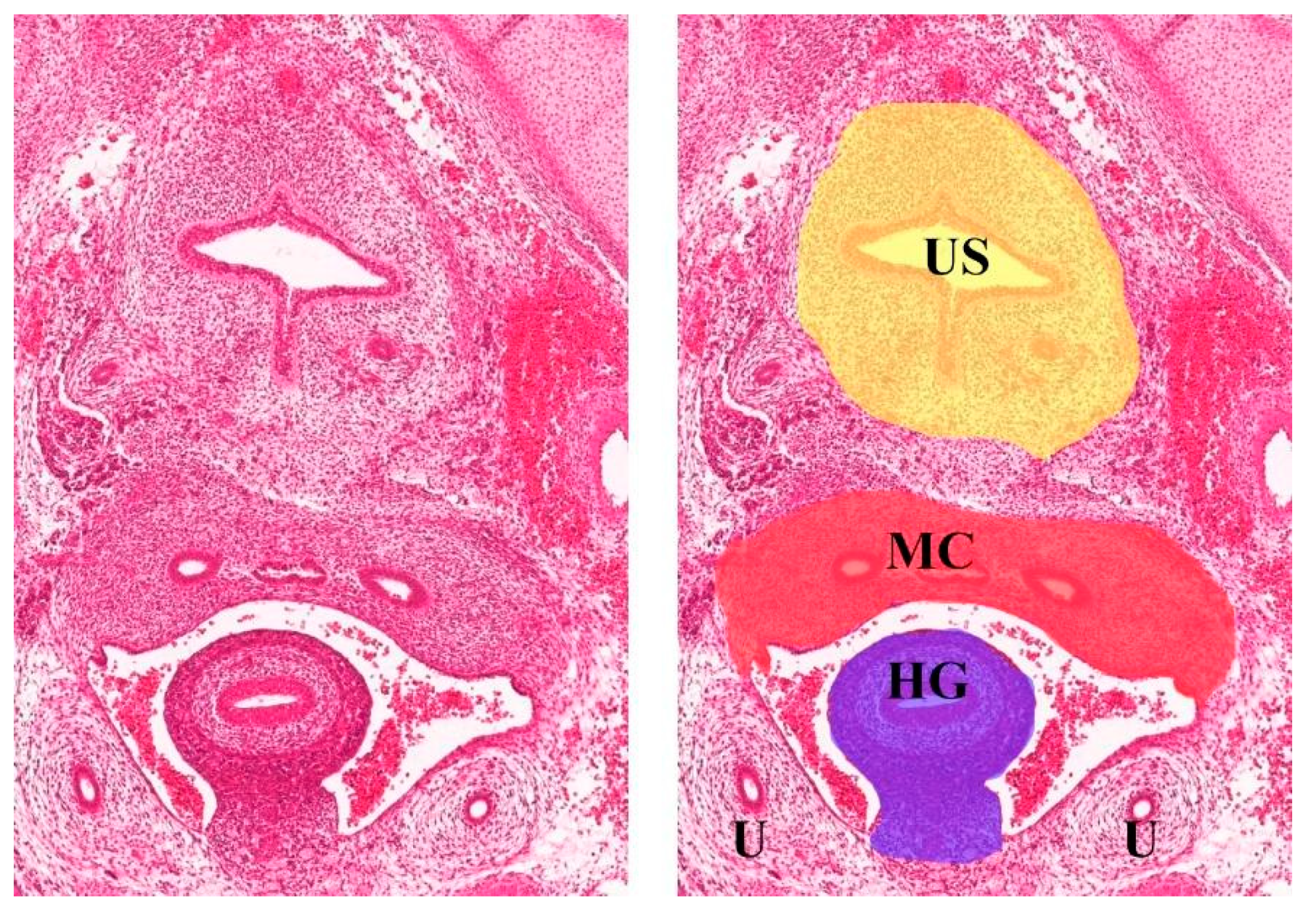
Figure 1. Transverse section of Carnegie stage 23 female embryo (the human histology images were provided by the Joint MRC/Wellcome Trust (MR/R006237/1) Human Developmental Biology Resource (www.hdbr.org, accessed on 8 June 2023; Gerrelli et al. (2015)) reference [4]. HG—hindgut, MC—Mullerian compartment, US—urogenital sinus, U—ureter.
Some discrepancies exist between conventional and ontogenetic anatomy concerning TME. The lateral rectal ligament and middle rectal artery have been accepted by some surgeons as a part of the rectal anatomy with no doubt [6][7]. However, when TME becomes the main procedure in rectal cancer surgery, these structures are no longer mentioned during mesorectal dissection. According to development, the hindgut is located intraperitoneally, and there is no middle rectal artery as a branch of the internal iliac artery, and there is no lateral ligament of the rectum [7][8].
The urogenital sinus (part of the ventral cloaca) gives rise to the urinary bladder, urethra, and distal 1/3 vagina. The intrapelvic part of this compartment has a well-demarcated border. Paramesonephric (Mullerian) ducts are differentiated into the fallopian tubes, uterus, cervix, and proximal 2/3 of the vagina. The most complex part of the Mullerian compartment is located subperitoneally. Some parts of the subperitoneal compartment are covered by an enveloped fascia, which is well demarcated, but some other parts are dissected from other compartments by their proper fascia [2][3][9] (Figure 2).

Figure 2. Total mesometrial resection specimen (author’s own material). VM—vascular mesometrium, LM—ligamentous mesometrium, C—cervix, V—vagina. Right picture (black box on left figure) shows fascia that partially covers vascular mesometria.
Two pairs of wings—vascular and ligamentous mesometria—are noticed. These mesotissues (especially vascular mesometria) contain intercalated lymph nodes and should be removed during a TMMR. Despite the proximity to the Mullerian compartment, mesometria originate from other compartments: vascular mesometria from anterior cloacal mesenchyme and ligamentous mesometria from distal splanchnic coelom. In the context of TMMR, a few parts of the urogenital sinus derivatives should be sharply dissected from the Mullerian and mesotissues compartments: the dorsal bladder adventitia from the cervix and the bladder mesentery from the vascular mesometrium. The vascular mesometrium contains the uterine artery and fibro-fatty and lymphatic tissues. This structure is similar to the LP during a type C RH. Ligamentous mesometrium is comparable with dorsal parametrium, which includes the most dorsal part close to the sacrum and also the deep or caudal part, called the rectovaginal ligament. The ligamentous mesometrium can be easily dissected from the edge of the mesorectal fascia [2][3][9].
The next part of the subperitoneal Mullerian compartment is the proximal 2/3 of the vagina and mesocolpium. The distal part of the vagina is formed from the urogenital sinus and is no longer a part of the TMMR procedure [10]. However, if a clear vaginal margin can be achieved without extirpation of the whole Mullerian vagina, an intracompartmental transection is appropriate to preserve the vaginal function [2][3].
The ureter is located below (caudal to) the vascular mesometrium and laterally to the ligamentous mesometrium. It develops as an outgrowth from the mesonephric duct and opens into the bladder (part of the urogenital sinus). According to developmental anatomy, the ureter and its mesentery—the mesoureter—can be sharply dissected from parts of the Mullerian compartment [11].
The HN is located between the mesoureter and the ligamentous mesometria proximally [2][3][9]. This concept differs from the Japanese one, where the mesoureter contains the HN [12][13][14]. Distally, the hypogastric nerve fuses with the PSNs and they together form the IHP. The IHP is located between the mesoureter and mesocolpium. For distal mesoureter mobilization, vaginal branches of the IHP should be transected and the bladder branches are preserved [2][3][9]. Conventional anatomy describes mesoureter as a lamina close to the rectum and without a clear ventral border at the ureterovesical junction [15][16]. In ontogenetic anatomy, the mesoureter can be dissected at the ventral side of the vascular mesometrium and up to the bladder. Höckel preserves the hypogastric nerve plane during total mesometrial resection [2][3][9].
The onion model was suggested by Höckel to explain ontogenetic anatomy (Figure 3). In contrast to conventional anatomy, this model is devoid of dissection artifacts—spaces and ligaments. According to the ontogenetic anatomy, the only ligaments that exist are derived from the gubernaculum—round ligaments and utero-ovarian ligaments [2][3][9].
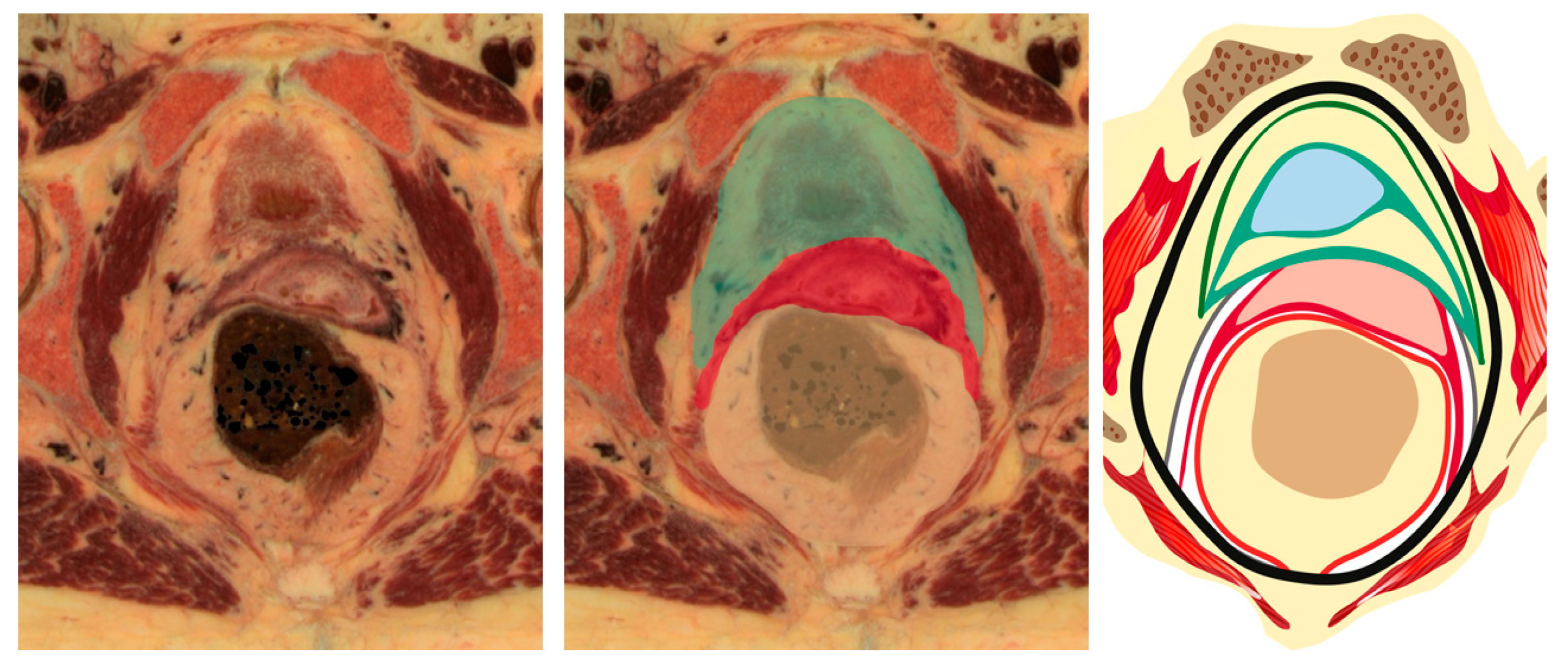
Figure 3. Onion model of female pelvis (author’s own material). Green—urogenital sinus derivate, red—mullerian compartment, yellow—hindgut derivate, gray—ureter and mesoureter.
2. Differences between the Ontogenetic Anatomy and Traditional Anatomy for Radical Hysterectomy
The ontogenetic anatomy has some discrepancies when compared to the traditional anatomy. Surgical anatomy for RH is based on the principle of uterocentricity. Any tissues located close to the cervix are called the parametrium or paracervix. Some independent data suggest the absence of the infraureteral parametrium (paracervix), which is part of a type C RH [17]. According to the ontogenetic approach, the LP consists of three different parts: the vascular mesometrium, bladder mesentery, and mesoureter (Figure 4). The dorsal parametrium can focus on ontogenetically different tissues—the mesoureter, hypogastric nerve, partial mesorectum, and ligamentous mesometrium. The VP, except its most proximal part, does not exist according to ontogenetic anatomy. It is a part of the bladder adventitia, and it belongs to the urogenital sinus compartment and does not contain intercalated lymph nodes related to the uterine cervix [2][3][9]. Data from the conventional RH anatomy are also contradictive, and some of these do not confirm lymphatic flow through the VP [18][19]. As a result, in the ontogenetic anatomy and TMMR, the surgical experience shows that the dissection of the VUL should be performed at the 11 o’clock position anterior to the ureter on the right side and at the 1 o’clock position anterior to the ureter on the left side to get a safe margin of a mesoureter dissection from the anterolateral vaginal wall. By the way, during a TMMR, the distal portion of the VUL is not excised, and the VVL with the paracolpium located posterior (caudal) to the distal ureter at the paravaginal zone are also not excised [2][3][9]. An intraoperative view during a TMMR is shown in Figure 5.

Figure 4. Ontogenetic anatomy for TMMR. Three-dimensional pelvic anatomy model (author’s own material). Lateral parametrium (left side—author’s own material) is split into 3 parts: vascular mesometrium (red), mesoureter (yellow), and bladder mesentery (green). Ventral parametrium is not shown as it is dissection artefact according to ontogenetic onion model.
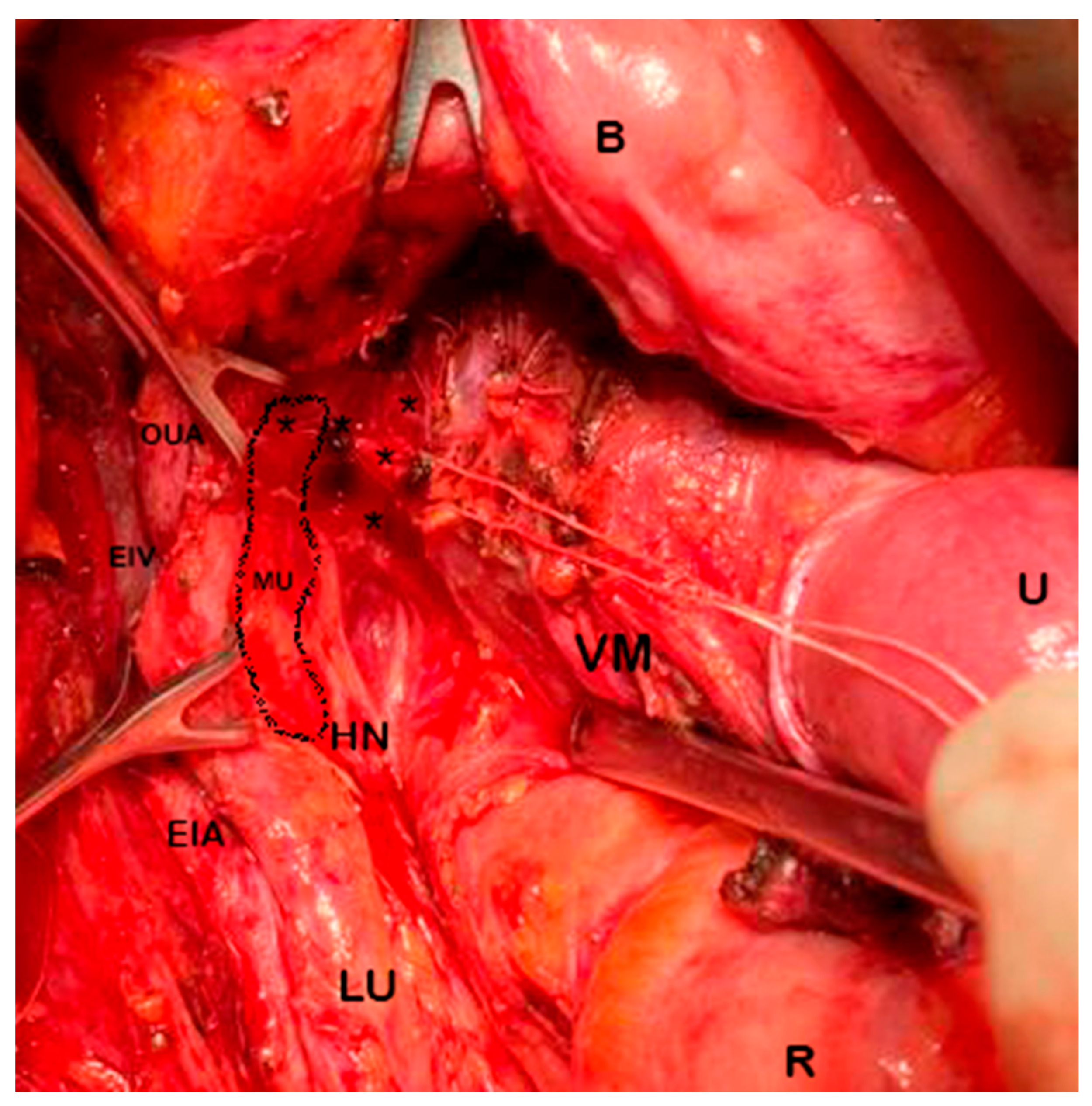
Figure 5. Total mesometrial resection—intraoperative view (left pelvic sidewall—author’s own material). U: uterus; B: bladder; R: rectum; LU: left ureter; EIA: external iliac artery; EIV: external iliac vein; HN: hypogastric nerve; VM: vascular mesometrium; OUA: obliterated umbilical artery; MU: mesoureter demarcated; (*): uterine branches from inferior hypogastric plexus repaired with cotton. Vascular mesometrium is grasped by forceps and guided dorsally. Vaginal veins are ligated and transected medial to mesoureter. Distal mesoureter, hypogastric nerves, and inferior hypogastric plexus are preserved.
Some surgical landmarks and steps during a TMMR are shown in Figure 6.

Figure 6. Dissection for ureter and pelvic nerve plane/plexus during total mesometrial resection (TMMR) (cadaveric dissection by Michael Höckel and author IS) (SHP: superior hypogastric plexus, HN: hypogastric nerve, IHP: inferior hypogastric plexus, IHPvf: inferior hypogastric plexus vesical fibers, IIA: internal iliac artery, OUA: obliterated umbilical artery, a: vascular mesometrium, b: ligamentous mesometrium, c: medial paracervix).
The differences regarding the terminology between RH and TMMR are shown in Table 1.
Table 1. Differences regarding terminology and conception of anatomy between RH and TMMR.
| Differences in Terminology and Conception of Anatomy | Radical Hysterectomy (C1/C2) | Total Mesometrial Resection |
|---|---|---|
| Avascular pelvic spaces | Exist | The concept of avascular spaces is not applicable for TMMR, despite some of the spaces developed during procedure (Latzko, Okabayashi, presacral) |
| Uterus ligaments | Exist | Only round and ovarian ligaments |
| Lateral parametrium | ||
| Cranial part | Parauterine tissue | Vascular mesometrium Distal mesoureter Mesobladder |
| Caudal part | Paracervix | Mesobladder IHP Mesocolpos |
| Ventral parametrium | ||
| Cranial part | Vesicouterine ligament | Mesobladder Vesicovaginal venous plexus |
| Caudal part | Vesicovaginal ligament | Mesobladder |
| Dorsal parametrium | ||
| Cranial part | Sacrouterine ligament | Ligamentous mesometrium—upper part |
| Caudal part | Rectovaginal ligament | Ligamentous mesometrium—lower part |
| Lateral ligament of the rectum | Exist | Does not exist |
| Middle rectal artery | Exist | Does not exist |
| Mesoureter | In the same axis and part of the hypogastric nerve | Not part of the hypogastric nerve. The nerve is located between the mesoureter and ligamentous mesometria |
References
- Sinnatamby, C.S. Last’s Anatomy, International Edition: Regional and Applied; Elsevier Health Sciences: Amsterdam, The Netherlands, 2011.
- Höckel, M. Cancer field surgery for locoregional tumor control of cervical carcinoma. J. Cancer Metastasis Treat. 2021, 7, 64.
- Höckel, M.; Horn, L.-C.; Manthey, N.; Braumann, U.-D.; Wolf, U.; Teichmann, G.; Frauenschläger, K.; Dornhöfer, N.; Einenkel, J. Resection of the embryologically defined uterovaginal (Müllerian) compartment and pelvic control in patients with cervical cancer: A prospective analysis. Lancet Oncol. 2009, 10, 683–692.
- Gerrelli, D.; Lisgo, S.; Copp, A.J.; Lindsay, S. Enabling research with human embryonic and fetal tissue resources. Development 2015, 142, 3073–3076.
- Heald, R.J. The ‘Holy Plane’ of rectal surgery. J. R. Soc. Med. 1988, 81, 503–508.
- Wang, J.; Sun, L.; Ni, T.; Huang, Y.; Wang, L.; Yuan, J.; Fan, Q.; Li, Y.; Wang, Y. A practical method of using the anatomical space of the vesicouterine ligament for laparoscopic radical hysterectomy: A retrospective cohort study. J. Int. Med. Res. 2020, 48, 300060520926857.
- Wang, G.J.; Gao, C.F.; Wei, D.; Wang, C.; Meng, W.J. Anatomy of the lateral ligaments of the rectum: A controversial point of view. World J. Gastroenterol. 2010, 16, 5411–5415.
- Zarzecki, M.P.; Ostrowski, P.; Wałęga, P.; Iwanaga, J.; Walocha, J.A. The middle anorectal artery: A systematic review and meta-analysis of 880 patients/1905 pelvic sides. Clin. Anat. 2022, 35, 934–945.
- Höckel, M. Principles and practice of surgical treatment for cervical cancer: It’s time for a change. Women’s Health 2009, 5, 459–462.
- Santiago, I.A.; Gomes, A.P.; Heald, R.J. An ontogenetic approach to gynecologic malignancies. Insights Imaging 2016, 7, 329–339.
- Rehman, S.; Ahmed, D. Embryology, Kidney, Bladder, and Ureter. In StatPearls ; StatPearls Publishing: Treasure Island, FL, USA, 2023.
- Yabuki, Y. Twenty-first century radical hysterectomy—Journey from descriptive to practical anatomy. Gynecol. Oncol. Rep. 2020, 34, 100623.
- Fujii, S.; Takakura, K.; Matsumura, N.; Higuchi, T.; Yura, S.; Mandai, M.; Baba, T.; Yoshioka, S. Anatomic identification and functional outcomes of the nerve sparing Okabayashi radical hysterectomy. Gynecol. Oncol. 2007, 107, 4–13.
- Sekiyama, K.; Fujii, S.; Mandai, M. Anatomical location of the surgically identifiable bladder branch of the inferior hypogastric plexus for nerve-sparing radical hysterectomy. Gynecol. Oncol. Rep. 2023, 46, 101152.
- Cibula, D.; Abu-Rustum, N.R.; Benedetti-Panici, P.; Köhler, C.; Raspagliesi, F.; Querleu, D.; Morrow, C.P. New classification system of radical hysterectomy: Emphasis on a three-dimensional anatomic template for parametrial resection. Gynecol. Oncol. 2011, 122, 264–268.
- Yabuki, Y. Two lateral parametria in radical hysterectomy: History and outcome. J. Obstet. Gynaecol. Res. 2023, 49, 1069–1078.
- Touboul, C.; Fauconnier, A.; Zareski, E.; Bouhanna, P.; Daraï, E. The lateral infraureteral parametrium: Myth or reality? Am. J. Obstet. Gynecol. 2008, 199, 242.e1–242.e6.
- Ercoli, A.; Delmas, V.; Iannone, V.; Fagotti, A.; Fanfani, F.; Corrado, G.; Ferrandina, G.; Scambia, G. The lymphatic drainage of the uterine cervix in adult fresh cadavers: Anatomy and surgical implications. Eur. J. Surg. Oncol. 2010, 36, 298–303.
- Kraima, A.C.; Derks, M.; Smit, N.N.; Van Munsteren, J.C.; Van der Velden, J.; Kenter, G.G.; DeRuiter, M.C. Lymphatic drainage pathways from the cervix uteri: Implications for radical hysterectomy? Gynecol. Oncol. 2014, 132, 107–113.
More
Information
Subjects:
Obstetrics & Gynaecology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
688
Revisions:
2 times
(View History)
Update Date:
15 Jan 2024
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




