
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Sigita Lesinskiene | -- | 1823 | 2023-12-27 21:24:27 | | | |
| 2 | Wendy Huang | Meta information modification | 1823 | 2023-12-28 07:28:24 | | |
Video Upload Options
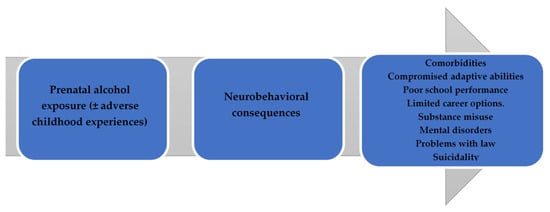
Prenatal alcohol exposure is one of the major avoidable causes of developmental disruption and health abnormalities in children. Fetal alcohol spectrum disorders (FASDs), a significant consequence of prenatal alcohol exposure, have gained more attention. Fetal alcohol spectrum disorders are an umbrella term used to describe a pattern of disabilities and abnormalities that result from fetal exposure to ethanol during pregnancy and are the most common non-heritable causes of intellectual disability. The effects on the fetus may include physical, mental, behavioral, and/or learning disabilities, with possible lifelong implications, and encompass a phenotypic range that can greatly vary between individuals but reliably include one or more of the following: facial dysmorphism, fetal growth deficiency, central nervous system dysfunction, and neurobehavioral impairment.
1. The Concept of FASD
2. Epidemiology
3. Burden of FASDs
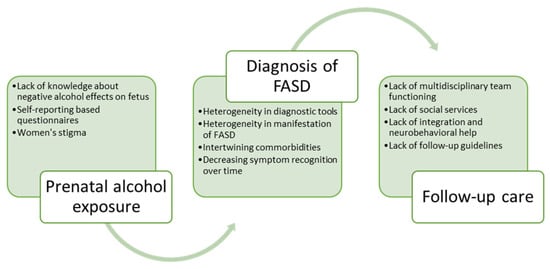
4. Assessing Prenatal Alcohol Exposure
5. Recognition of Signs over Time
6. Challenges in Follow-Up Care
References
- Denny, L.; Coles, S.; Blitz, R. Fetal Alcohol Syndrome and Fetal Alcohol Spectrum Disorders. Am. Fam. Physician 2017, 96, 515–522.
- Children and Young People Exposed Prenatally to Alcohol: A National Clinical Guideline—Digital Collections—National Library of Medicine. Available online: https://digirepo.nlm.nih.gov/catalog/nlm:nlmuid-101772266-pdf (accessed on 7 April 2023).
- Hoyme, H.E.; May, P.A.; Kalberg, W.O.; Kodituwakku, P.; Gossage, J.P.; Trujillo, P.M.; Buckley, D.G.; Miller, J.H.; Aragon, A.S.; Khaole, N.; et al. A practical clinical approach to diagnosis of fetal alcohol spectrum disorders: Clarification of the 1996 institute of medicine criteria. Pediatrics 2005, 115, 39–47.
- Ethen, M.K.; Ramadhani, T.A.; Scheuerle, A.E.; Canfield, M.A.; Wyszynski, D.F.; Druschel, C.M.; Romitti, P.A.; National Birth Defects Prevention Study. Alcohol Consumption by Women Before and During Pregnancy. Matern. Child Health J. 2009, 13, 274–285.
- Lange, S.; Probst, C.; Gmel, G.; Rehm, J.; Burd, L.; Popova, S. Global Prevalence of Fetal Alcohol Spectrum Disorder among Children and Youth: A Systematic Review and Meta-analysis. J. Am. Med. Assoc. Pediatr. 2017, 171, 948–956.
- May, P.A.; Chambers, C.D.; Kalberg, W.O.; Zellner, J.; Feldman, H.; Buckley, D.; Kopald, D.; Hasken, J.M.; Xu, R.; Honerkamp-Smith, G.; et al. Prevalence of Fetal Alcohol Spectrum Disorders in 4 US Communities. J. Am. Med. Assoc. 2018, 319, 474–482.
- Rangmar, J.; Hjern, A.; Vinnerljung, B.; Strömland, K.; Aronson, M.; Fahlke, C. Psychosocial outcomes of fetal alcohol syndrome in adulthood. Pediatrics 2015, 135, e52–e58.
- Wozniak, J.R.; Riley, E.P.; Charness, M.E. Clinical presentation, diagnosis, and management of fetal alcohol spectrum disorder. Lancet Neurol. 2019, 18, 760–770.
- Mattson, S.N.; Bernes, G.A.; Doyle, L.R. Fetal Alcohol Spectrum Disorders: A Review of the Neurobehavioral Deficits Associated with Prenatal Alcohol Exposure. Alcohol Clin. Exp. Res. 2019, 43, 1046–1062.
- Weyrauch, D.; Schwartz, M.; Hart, B.; Klug, M.G.; Burd, L. Comorbid Mental Disorders in Fetal Alcohol Spectrum Disorders: A Systematic Review. J. Dev. Behav. Pediatr. 2017, 38, 283–291.
- Willoughby, K.A.; Sheard, E.D.; Nash, K.; Rovet, J. Effects of prenatal alcohol exposure on hippocampal volume, verbal learning, and verbal and spatial recall in late childhood. J. Int. Neuropsychol. Soc. 2008, 14, 1022–1033.
- Kambeitz, C.; Klug, M.G.; Greenmyer, J.; Popova, S.; Burd, L. Association of adverse childhood experiences and neurodevelopmental disorders in people with fetal alcohol spectrum disorders (FASD) and non-FASD controls. BMC Pediatr. 2019, 19, 498.
- Sessa, F.; Salerno, M.; Esposito, M.; Di Nunno, N.; Rosi, G.L.; Roccuzzo, S.; Pomara, C. Understanding the Relationship between Fetal Alcohol Spectrum Disorder (FASD) and Criminal Justice: A Systematic Review. Healthcare 2022, 10, 84.
- Jones, T.B.; Bailey, B.A.; Sokol, R.J. Alcohol use in pregnancy: Insights in screening and intervention for the clinician. Clin. Obstet. Gynecol. 2013, 56, 114–123.
- Stone, R. Pregnant women and substance use: Fear, stigma, and barriers to care. Health Justice 2015, 3, 2.
- Lange, S.; Shield, K.; Koren, G.; Rehm, J.; Popova, S. A comparison of the prevalence of prenatal alcohol exposure obtained via maternal self-reports versus meconium testing: A systematic literature review and meta-analysis. BMC Pregnancy Childbirth 2014, 14, 127.
- Gupta, K.K.; Gupta, V.K.; Shirasaka, T. An Update on Fetal Alcohol Syndrome-Pathogenesis, Risks, and Treatment. Alcohol Clin. Exp. Res. 2016, 40, 1594–1602.
- Popova, S.; Dozet, D.; Shield, K.; Rehm, J.; Burd, L. Alcohol’s Impact on the Fetus. Nutrients 2021, 13, 3452.
- Kalberg, W.O.; May, P.A.; Buckley, D.; Hasken, J.M.; Marais, A.-S.; De Vries, M.M.; Bezuidenhout, H.; Manning, M.A.; Robinson, L.K.; Adam, M.P.; et al. Early-Life Predictors of Fetal Alcohol Spectrum Disorders. Pediatrics 2019, 14, e20182141.
- Jacobson, S.W.; Hoyme, H.E.; Carter, R.C.; Dodge, N.C.; Molteno, C.D.; Meintjes, E.M.; Jacobson, J.L. Evolution of the Physical Phenotype of Fetal Alcohol Spectrum Disorders from Childhood through Adolescence. Alcohol Clin. Exp. Res. 2021, 45, 395–408.
- Clarren, S.K.; Randels, S.P.; Sanderson, M.; Fineman, R.M. Screening for fetal alcohol syndrome in primary schools: A feasibility study. Teratology 2001, 63, 3–10.
- Wells, A.M.; Chasnoff, I.J.; Schmidt, C.A.; Telford, E.; Schwartz, L.D. Neurocognitive Habilitation Therapy for Children with Fetal Alcohol Spectrum Disorders: An Adaptation of the Alert Program®. Am. J. Occup. Ther. 2012, 66, 24–34.
- Reid, N.; Dawe, S.; Shelton, D.; Harnett, P.; Warner, J.; Armstrong, E.; LeGros, K.; O’Callaghan, F. Systematic Review of Fetal Alcohol Spectrum Disorder Interventions across the Life Span. Alcohol Clin. Exp. Res. 2015, 39, 2283–2295.
- Pruett, D.; Waterman, E.H.; Caughey, A.B. Fetal alcohol exposure: Consequences, diagnosis, and treatment. Obstet. Gynecol. Surv. 2013, 68, 62–69.




