Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Payal Ganguly | -- | 2047 | 2023-11-21 11:13:58 | | | |
| 2 | Jason Zhu | -2 word(s) | 2045 | 2023-11-22 02:25:23 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Iqbal, N.; Pant, T.; Rohra, N.; Goyal, A.; Lawrence, M.; Dey, A.; Ganguly, P. Nanoscale Materials for Scaffold Structure and Function. Encyclopedia. Available online: https://encyclopedia.pub/entry/51842 (accessed on 05 March 2026).
Iqbal N, Pant T, Rohra N, Goyal A, Lawrence M, Dey A, et al. Nanoscale Materials for Scaffold Structure and Function. Encyclopedia. Available at: https://encyclopedia.pub/entry/51842. Accessed March 05, 2026.
Iqbal, Neelam, Tejal Pant, Nanda Rohra, Abhishek Goyal, Merin Lawrence, Anomitra Dey, Payal Ganguly. "Nanoscale Materials for Scaffold Structure and Function" Encyclopedia, https://encyclopedia.pub/entry/51842 (accessed March 05, 2026).
Iqbal, N., Pant, T., Rohra, N., Goyal, A., Lawrence, M., Dey, A., & Ganguly, P. (2023, November 21). Nanoscale Materials for Scaffold Structure and Function. In Encyclopedia. https://encyclopedia.pub/entry/51842
Iqbal, Neelam, et al. "Nanoscale Materials for Scaffold Structure and Function." Encyclopedia. Web. 21 November, 2023.
Copy Citation
Bone regeneration and repair are complex processes with the potential of added complications, like delayed repair, fracture non-union, and post-surgical infections. These conditions remain a challenge globally, pressurizing the economy and patients suffering from these conditions. Applications of nanotechnology (NBT) in the field of medicine have provided a medium for several approaches to support these global challenges. Tissue engineering is one such field that has been on the rise in the past through the utilization of NBT for addressing the challenges related to bone regeneration.
bone repair
tissue engineering
bone regeneration
nanomedicine
nanobiotechnology (NBT)
nanoparticle (NP)
regenerative medicine
bone tissue engineering (BTE)
1. Introduction
Nanoscale materials have emerged as pivotal players in BTE due to their inherent advantages, including biocompatibility, biodegradability, mechanical tunability, and their capacity to mimic the natural bone ECM [1][2][3][4][5]. Several types of materials are being used either individually or more commonly in combination with materials providing complementary benefits towards the final scaffold. For example, several polymers, including natural polymers such as chitosan, gelatin, and collagen, are used in hydrogel preparation for BTE due to their biochemical and biophysical properties [6]. Other polymers, discussed below, were also found to be beneficial at nanoscale for applications in drug delivery and tissue engineering [7]. They may also be used in combination with harder materials, like bioactive glass, or metals, like titanium, zinc, strontium, and others in their nanoscale forms, offering biocompatibility, enhanced mechanical strength, and biodegradability towards scaffold formulation [8][9]. The various materials used for BTE, as shown in Figure 1, broadly explores polymeric and non-polymeric materials that have been used in BTE applications, specifically for scaffold formation.
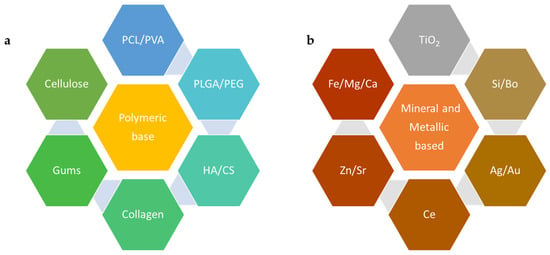
Figure 1. Example of materials used in nanoscale forms for BTE: (a)—polymeric materials and (b)—metallic elements, PCL—poly(ε-caprolactone), PVA—poly(vinyl alcohol), PLGA—poly(lactic-co-glycolic acid), PEG—polyethylene glycol, HA—hyaluronic acid, CS—chitosan, TiO2—titanium dioxide, Si—silicon, Bo—boron, Ag—argentum (silver), Au—aurum (gold), Ce—cerium, Zn—zinc, Sr—strontium, Fe—ferrous/ferric (Iron), Mg—magnesium, Ca—calcium.
2. Polymeric Materials Used at the Nanoscale for BTE
2.1. Synthetic Polymers
Polycaprolactone (ε-PCL) is a biodegradable, biocompatible polyester that has attracted substantial attention in BTE due to its adaptable biodegradation and ease of manipulation into NFs, NPs, and scaffolds [10]. A PCL fiber mesh fabricated via electrospinning demonstrated enhanced osteoblast cell proliferation and differentiation, whereby the structure mimicked the natural ECM, facilitating cell adhesion and growth essential for successful BTE [11]. Poly(lactic-co-glycolic acid) (PLGA), a copolymer of lactic and glycolic acids, is another example of a biodegradable and biocompatible polymer commonly used in BTE. Nanostructured PLGAs can be formed into NPs for drug delivery, NFs, or scaffolds for cell growth and have each contributed unique benefits to BTE [12][13].
PLGA NFs combined with nano hydroxyapatite (HA), a major inorganic component of bone, exhibited improved cell attachment, proliferation, and differentiation [14]. Polyethylene glycol (PEG) is another polymer that is often utilized in nanoscale form due to its excellent biocompatibility and resistance to protein adsorption. PEGylated gelatin nanospheres have been used to deliver BMP-2, which enhances bone regeneration in vivo, signifying the importance of PEG in nanoscale drug delivery systems for BTE [15]. Other nanoscale polymers, such as poly(lactic acid) (PLA), poly(glycolic acid) (PGA), poly(vinyl alcohol) (PVA), and polyurethane (PU), are also being explored for their potential in BTE and have been discussed in great detail elsewhere [2][16][17]. When crafted into nanoscale forms, such as fibers or particles, these polymers show promising potential in promoting cell attachment, proliferation, differentiation, and delivering therapeutic agents, thereby boosting bone regeneration [8][9][18][19][20].
2.2. Natural Polymers
Chitosan (CS) is another example of a biopolymer exhibiting a multitude of favorable properties, including non-toxicity, biodegradability, biocompatibility [21][22], antifungal, antibacterial [23][24], and wound healing abilities. Therefore, CS is widely utilized in the biomedical, biotechnology, and pharmaceutical fields [25][26]. CS is a prime candidate for crafting potential bone scaffolds, particularly when paired with osteoconductive substances, such as HA [21][27] and poly(acrylic acid) (PAA) [28]. Studies have shown that CS-based bone scaffolds foster cell adhesion and osteoblast cell proliferation, creating mineralized bone matrices in vitro [29]. An enhancement in osteoblast cell proliferation was observed for CS composites that incorporated nanoHA, ultimately triggering bone regeneration within eight weeks as validated by micro-computed tomography [30]. The mechanical characteristics of CS scaffolds can be enhanced by crosslinking with substances possessing a minimum of two reactive functional groups, such as calcium phosphates, composites (nanozirconia and nanocalcium zirconate), and bioglass, leading to a superior performance compared to constructs consisting of only CS [31].
Cellulose is another widespread linear biopolymer that contributes significant tensile strength to trees and is present in various organisms, including marine species, bacteria, fungi, and even amoebas [32]. It is usually characterized by long fibrils that comprise various crystalline and amorphous regions. By subjecting the cellulose pulp to mechanical or chemical alterations, it is feasible to extract tiny crystalline cellulose components. These diminutive cellulose polymers, referred to as cellulose nanocrystals (CNCs), typically exhibit diameters of 2–20 nm and a length distribution of 100–600 nm [33]. The functionalization of CNCs with sulphate or phosphate ester groups can be achieved through sulfuric or phosphoric acid hydrolyses [34]. These modified scaffolds reveal superior crosslinking and, subsequently, enhanced mechanical properties compared to those that are unmodified.
Furthermore, compared with phosphate ester-modified aerogels, aerogels crafted from sulphate ester-treated CNCs display greater compressive strength, porosity, and crosslinking [35]. These sulphate ester-modified CNCs (S–CNCs) possess in vivo osteoconductive properties, enabling bone growth at the defect location. After three weeks, S–CNC aerogels can create a bone volume percentage that exceeds controls by 33% and can see a size increase of 50% after twelve weeks. Comprehensive research into cell–interface interactions and in vivo scaffold degradation is crucial. Scaffolds constructed using modified CNCs with bone tissue-enhancing properties are emerging as promising solutions for BTE applications [36]. Various methods, like electrospinning or 3D printing, may be applied to fabricate polymeric scaffolds and the recent advances in these applications have been outlined elsewhere [37][38].
3. Mineral-Based and Metallic Nanoscale Materials Used for BTE
NPs obtained from minerals, such as zinc, silica, or calcium phosphate particles, are classified as nanoscale materials where their primary role is to provide vital ions for tissue generation. They do so by enhancing the mechanical properties of 3D-printed scaffolds. Mineral-derived nanomaterials can be produced by several techniques, such as plasma spraying, milling, and precipitation from solution [39]. Similarly, metallic nanoscale formulations of gold (Au), silver (Ag), and titanium (Ti) have been explored at length for their enhanced functionalities.
3.1. Mineral Nanoparticles
Calcium Phosphate
Adding mineral-based nanomaterials to both the surface and bulk of 3D-printed scaffolds has been shown to improve the overall functionality of the scaffolds. Nanomaterials derived from calcium phosphate (CaP) are often added to the 3D-printed scaffolds since bone is inherently composed of CaP crystals (70%) and 30% of organic collagen fibrils [40]. In 2017, Chen et al. generated a biomimetic composite scaffold of collagen and biphasic calcium phosphate nanoparticles (BCP NPs). They engineered these scaffolds to release dexamethasone (DEX) during preparation and hybridized this with collagen scaffolds. The subcutaneous implantation of the composite scaffolds at the dorsal side of athymic nude mice demonstrated the regeneration of the ectopic bone tissue. When used for the 3D culture of human BM-derived MSCs, these scaffolds demonstrated enhanced biocompatibility and promoted the osteogenic differentiation of hMSCs [41]. Another study by Sokolova et al. in 2020 used scaffolds of PLGA and nanohydroxyapatite (nHAP) (85:15) combined with DNA-loaded CaP NPs. The results suggested increased cytocompatibility and rate of gene transfection into cells indicating their favorable application as a scaffold for BTE or a bone substitution material [42].
Silicon Dioxide (SiO2)
Silica NPs are an example of inorganic NPs. Silica particles have been shown to promote osteoblast differentiation while inhibiting osteoclast differentiation [43]. A recent study by Echazú et al. in 2022 [44] combined soluble silica particles and a CS polymer to engineer a potential bone substitute. This was implanted into the medullary compartment of both tibiae in Wistar rats and investigated for cytotoxicity and biocompatibility. The results indicated successful new bone formation at the tissue–biocomposite interface (osseointegration) [44]. Another study conducted in 2023 by Shuai et al. used poly(L-lactic acid) (PLLA)-based bone scaffolds and combined SiO2 NPs with graphene oxide (GO) NS to promote the dispersion of GO on the biopolymer bone scaffold. The optimization of the adequate dispersion of GO with SiO2 enhanced the mechanical properties and cytocompatibility of the scaffold, making it a potential candidate for BTE applications [45].
Zinc Oxide (ZnO)
Zinc is one of the minerals present in bone in the form of trace elements. It promotes bone density and the prevention of bone loss [46]. It also activates proteins involved in bone homeostasis as a part of inorganic minerals. ZnO NPs exhibit low toxicity, act as antibacterial agents, and exhibit optimal biological compatibility and chemical stability. They stimulate osteogenesis and hence have the potential to accelerate bone growth and mineralization [47][48]. In 2020, Cho et al. investigated the cell proliferation and antibacterial activities of a PCL/nanoHA scaffold doped with ZnO. Their results indicated that the scaffolds with 100 nm-thick ZnO coatings showed enhanced antibacterial cell proliferation activities and mechanical properties [49]. In 2017, Forero et al. studied the effect of CS/gelatin/nanoHA scaffolds containing a nano-copper–zinc alloy for BTE. These scaffolds increased the proliferation and adhesion of mouse embryonic fibroblasts and induced osteogenic differentiation. After an in vivo subcutaneous implant, they induced the growth of surrounding tissues and promoted granulation tissue formation [50]. The use of ZnO NPs in the field of BTE is very limited, but promising, with novel advancements being made using hybrid mix of compatible biopolymers.
3.2. Metallic NPs
A high penetrating ability and surface area coupled with improved cell adhesion, differentiation, and growth suggests that metal NPs are one of the ideal candidates for scaffold fabrication in BTE. Ag and Au are the most common osteogenic agents used in this category. They exhibit a high surface area, enhanced antibacterial properties, biocompatibility, and surface reactive features in order to identify pathogenic viruses [51] and intracellular targets [52].
Silver (Ag)
Silver (metal or salt) has been used as an antibacterial agent in implants [53][54]. Ag ions can penetrate the bacterial cell wall and cause growth inhibition. Ag-based scaffolds are highly potent with enhanced cell adhesion and cytocompatibility, improved osteogenesis and osteo-conductivity, acceptable mechanical strength, an ability to bridge oxygen molecules, and low toxicity [55][56][57]. Akturk et al. optimized the protocol to generate an antibacterial gelatin nanocomposite membrane for BTE applications. They used soluble starch-coated Ag NPs and bioactive glass particles incorporated into gelatin to fabricate a nanohybrid nanocomposite fiber [58]. Another study investigated the use of CS-silver polymeric scaffolds in BTE. These scaffolds demonstrated enhanced matrix mineralization and osteogenic differentiation (marked by the upregulation of marker genes Runt-related transcription factor 2 (Runx2), type-1 collagen (Col-I), alkaline phosphatase (ALP) activity, and secreted osteocalcin (OCN)) [59].
Gold (Au)
Gold NPs exhibit low toxicity, high antibacterial effects, and biocompatibility in the scaffold environment [60]. While some studies indicate dose-dependent cytotoxicity in human cell lines marked by membrane damage and reactive oxidative species (ROS) generation [61][62], this property of Au NPs has often been useful to destroy cancer cells [63]. Thus, ensuring the appropriate size and dosing of Au NP plays a crucial role in BTE applications. Nekounam et al. demonstrated an optimized protocol for the fabrication of a carbon NF/Au NP-based scaffold that supported cell proliferation and indicated low toxicity in bone cells [64]. Au NPs that are smaller in size (<10 nm) have been used for miRNA delivery to the nucleus. Yu et al. in 2017 created nanohybrids using polyethylenimine, liposomes coated on the surface of Au NPs. After the release from endosomes inside the cells, miR-5106 was able to facilitate BM stem cell osteoblastic differentiation, which further aided in mineralization [65].
Titanium Dioxide (TiO2)
TiO2 NPs are bioinert cell carrier materials with improved permeability and high biocompatibility. They are available in the form of nanocrystals and exhibit antibacterial and antiseptic properties making them a promising scaffolding material for bone tissue repair [66]. A study published in 2018 described the methodology to fabricate a lightweight and economical TiO2/CS scaffold by freeze-drying [67]. An in vitro study conducted by Pattanashetti et al. in 2020 determined the ideal weight percentages of TiO2 NPs that needed to be crosslinked in a PVA matrix. These nanofibrous scaffolds were developed using electrospinning and the results indicated that 0.1 g of TiO2 exhibited enhanced mechanical stability and a subsequent slow rate of degradation in the scaffolds. These scaffolds were found to be viable and non-toxic to the cells, as observed by the MTT assay using MG-63 osteosarcoma cell lines [68].
References
- Simchi, A.; Mazaheri, M.; Eslahi, N.; Ordikhani, F.; Tamjid, E. Nanomedicine applications in orthopedic medicine: State of the art. Int. J. Nanomed. 2023, 10, 6039–6054.
- Scott, T.G.; Blackburn, G.; Ashley, M.; Bayer, I.S.; Ghosh, A.; Biris, A.S.; Biswas, A. Advances in bionanomaterials for bone tissue engineering. J. Nanosci. Nanotechnol. 2013, 13, 1–22.
- Qiao, K.; Xu, L.; Tang, J.; Wang, Q.; Lim, K.S.; Hooper, G.; Woodfield, T.B.F.; Liu, G.; Tian, K.; Zhang, W.; et al. The advances in nanomedicine for bone and cartilage repair. J. Nanobiotechnol. 2022, 20, 141.
- Babuska, V.; Kasi, P.B.; Chocholata, P.; Wiesnerova, L.; Dvorakova, J.; Vrzakova, R.; Nekleionova, A.; Landsmann, L.; Kulda, V. Nanomaterials in Bone Regeneration. Appl. Sci. 2022, 12, 6793.
- Vieira, S.; Vial, S.; Reis, R.L.; Oliveira, J.M. Nanoparticles for bone tissue engineering. Biotechnol. Prog. 2017, 33, 590–611.
- Guillén-Carvajal, K.; Valdez-Salas, B.; Beltrán-Partida, E.; Salomón-Carlos, J.; Cheng, N. Chitosan, Gelatin, and Collagen Hydrogels for Bone Regeneration. Polymers 2023, 15, 2762.
- Begines, B.; Ortiz, T.; Pérez-Aranda, M.; Martínez, G.; Merinero, M.; Argüelles-Arias, F.; Alcudia, A. Polymeric Nanoparticles for Drug Delivery: Recent Developments and Future Prospects. Nanomaterials 2020, 10, 1403.
- Khan, M.U.A.; Al-Arjan, W.S.; Binkadem, M.S.; Mehboob, H.; Haider, A.; Raza, M.A.; Razak, S.I.A.; Hasan, A.; Amin, R. Development of Biopolymeric Hybrid Scaffold-Based on AAc/GO/nHAp/TiO2 Nanocomposite for Bone Tissue Engineering: In-Vitro Analysis. Nanomaterials 2021, 11, 1319.
- Matos, R.J.R.; Silva, J.C.; Soares, P.I.P.; Borges, J.P. Polyvinylpyrrolidone Nanofibers Incorporating Mesoporous Bioactive Glass for Bone Tissue Engineering. Biomimetics 2023, 8, 206.
- Dwivedi, R.; Kumar, S.; Pandey, R.; Mahajan, A.; Nandana, D.; Katti, D.S.; Mehrotra, D. Polycaprolactone as biomaterial for bone scaffolds: Review of literature. J. Oral Biol. Craniofacial Res. 2020, 10, 381–388.
- Al-Maawi, S.; Dohle, E.; Lim, J.; Weigl, P.; Teoh, S.H.; Sader, R.; Ghanaati, S. Biologization of Pcl-Mesh Using Platelet Rich Fibrin (Prf) Enhances Its Regenerative Potential In Vitro. Int. J. Mol. Sci. 2021, 22, 2159.
- Jin, S.; Xia, X.; Huang, J.; Yuan, C.; Zuo, Y.; Li, Y.; Li, J. Recent advances in PLGA-based biomaterials for bone tissue regeneration. Acta Biomater. 2021, 127, 56–79.
- Hassan, M.; Sulaiman, M.; Yuvaraju, P.D.; Galiwango, E.; Rehman, I.u.; Al-Marzouqi, A.H.; Khaleel, A.; Mohsin, S. Biomimetic PLGA/Strontium-Zinc Nano Hydroxyapatite Composite Scaffolds for Bone Regeneration. J. Funct. Biomater. 2022, 13, 13.
- Chen, L.; Zhu, W.-M.; Fei, Z.-Q.; Chen, J.-L.; Xiong, J.-Y.; Zhang, J.-F.; Duan, L.; Huang, J.; Liu, Z.; Wang, D.; et al. The study on biocompatibility of porous nHA/PLGA composite scaffolds for tissue engineering with rabbit chondrocytes in vitro. BioMed Res. Int. 2013, 2013, 412745.
- Wang, H.; Zou, Q.; Boerman, O.C.; Nijhuis, A.W.; Jansen, J.A.; Li, Y.; Leeuwenburgh, S.C. Combined delivery of BMP-2 and bFGF from nanostructured colloidal gelatin gels and its effect on bone regeneration in vivo. J. Control. Release Off. J. Control. Release Soc. 2013, 166, 172–181.
- Zhu, L.; Luo, D.; Liu, Y. Effect of the nano/microscale structure of biomaterial scaffolds on bone regeneration. Int. J. Oral Sci. 2020, 12, 6.
- Abbas, M.; Alqahtani, M.S.; Alhifzi, R. Recent Developments in Polymer Nanocomposites for Bone Regeneration. Int. J. Mol. Sci. 2023, 24, 3312.
- Castro, J.I.; Llano, C.H.V.; Tenorio, D.L.; Saavedra, M.; Zapata, P.; Navia-Porras, D.P.; Delgado-Ospina, J.; Chaur, M.N.; Hernández, J.H.M.; Grande-Tovar, C.D. Biocompatibility Assessment of Polylactic Acid (PLA) and Nanobioglass (n-BG) Nanocomposites for Biomedical Applications. Molecules 2022, 27, 3640.
- Suaza, M.L.M.; Rivera, J.C.L.; Padilla, M.C.R.; Acevedo, M.E.M.; Orozco, C.P.O.; Triviño, D.G.Z. Poly(vinyl alcohol)/Silk Fibroin/Ag-NPs Composite Nanofibers as a Substrate for MG-63 Cells’ Growth. Polymers 2023, 15, 1838.
- Wang, Y.-J.; Jeng, U.-S.; Hsu, S.-H. Biodegradable Water-Based Polyurethane Shape Memory Elastomers for Bone Tissue Engineering. ACS Biomater. Sci. Eng. 2018, 4, 1397–1406.
- Anitha, A.; Sowmya, S.; Kumar, P.S.; Deepthi, S.; Chennazhi, K.; Ehrlich, H.; Tsurkan, M.; Jayakumar, R. Chitin and chitosan in selected biomedical applications. Prog. Polym. Sci. 2014, 399, 1644–1667.
- Aljawish, A.; Chevalot, I.; Jasniewski, J.; Scher, J.; Muniglia, L. Enzymatic synthesis of chitosan derivatives and their potential applications. J. Mol. Catal. B Enzym. 2015, 112, 25–39.
- Yildizbakan, L.; Iqbal, N.; Ganguly, P.; Kumi-Barimah, E.; Do, T.; Jones, E.; Giannoudis, P.V.; Jha, A. Fabrication and Characterisation of the Cytotoxic and Antibacterial Properties of Chitosan-Cerium Oxide Porous Scaffolds. Antibiotics 2023, 12, 1004.
- Iqbal, N.; Braxton, T.M.; Anastasiou, A.; Raif, E.M.; Chung, C.K.Y.; Kumar, S.; Giannoudis, P.V.; Jha, A. Dicalcium Phosphate Dihydrate Mineral Loaded Freeze-Dried Scaffolds for Potential Synthetic Bone Applications. Materials 2022, 15, 6245.
- Younes, I.; Rinaudo, M. Chitin and chitosan preparation from marine sources. Structure, properties and applications. Mar. Drugs 2015, 13, 1133–1174.
- Garg, U.; Chauhan, S.; Nagaich, U.; Jain, N. Current Advances in Chitosan Nanoparticles Based Drug Delivery and Targeting. Adv. Pharm. Bull. 2019, 9, 195–204.
- Rodríguez-Vázquez, M.; Vega-Ruiz, B.; Ramos-Zúñiga, R.; Saldaña-Koppel, D.A.; Quiñones-Olvera, L.F. Chitosan and Its Potential Use as a Scaffold for Tissue Engineering in Regenerative Medicine. BioMed Res. Int. 2015, 2015, 821279.
- Ibrahim, H.M.; Zairy, E.M.R.E. Chitosan as a Biomaterial—Structure, Properties, and Electrospun Nanofibers. In Concepts, Compounds and the Alternatives of Antibacterials; IntechOpen: London, UK, 2015.
- Levengood, S.K.L.; Zhang, M. Chitosan-based scaffolds for bone tissue engineering. J. Mater. Chem. B 2014, 2, 3161–3184.
- Lee, J.S.; Baek, S.D.; Venkatesan, J.; Bhatnagar, I.; Chang, H.K.; Kim, H.T.; Kim, S.-K. In vivo study of chitosan-natural nano hydroxyapatite scaffolds for bone tissue regeneration. Int. J. Biol. Macromol. 2014, 67, 360–366.
- Sultankulov, B.; Berillo, D.; Sultankulova, K.; Tokay, T.; Saparov, A. Progress in the Development of Chitosan-Based Biomaterials for Tissue Engineering and Regenerative Medicine. Biomolecules 2019, 9, 470.
- Mehdi Jorfi, E.J.F. Recent advances in nanocellulose for biomedical applications. J. Appl. Polym. Sci. 2014, 132, 41719.
- Md Nazrul Islam, F.R. Chapter 6—Production and modification of nanofibrillated cellulose composites and potential applications. In Green Composites for Automotive Applications; Woodhead Publishing Series in Composites Science and Engineering; Elsevier: Amsterdam, The Netherlands, 2019; pp. 115–141.
- Osorio, D.A.; Lee, B.E.J.; Kwiecien, J.M.; Wang, X.; Shahid, I.; Hurley, A.L.; Cranston, E.D.; Grandfield, K. Cross-linked cellulose nanocrystal aerogels as viable bone tissue scaffolds. Acta Biomater. 2019, 87, 152–165.
- Baldwin, P.; Li, D.J.; Auston, D.A.; Mir, H.S.; Yoon, R.S.; Koval, K.J. Autograft, Allograft, and Bone Graft Substitutes: Clinical Evidence and Indications for Use in the Setting of Orthopaedic Trauma Surgery. J. Orthop. Trauma 2019, 33, 203–213.
- Sagadevan, S.; Schirhagl, R.; Rahman, Z.; Bin Ismail, M.F.; Lett, J.A.; Fatimah, I.; Kaus, N.H.M.; Oh, W.-C. Recent advancements in polymer matrix nanocomposites for bone tissue engineering applications. J. Drug Deliv. Sci. Technol. 2023, 82, 104313.
- Ganguly, P.; Jones, E.; Panagiotopoulou, V.; Jha, A.; Blanchy, M.; Antimisiaris, S.; Anton, M.; Dhuiège, B.; Marotta, M.; Marjanovic, N.; et al. Electrospun and 3D printed polymeric materials for one-stage critical-size long bone defect regeneration inspired by the Masquelet technique: Recent Advances. Injury 2022, 53 (Suppl. S2), s2–s12.
- Di Marzio, N.; Eglin, D.; Serra, T.; Moroni, L. Bio-Fabrication: Convergence of 3D Bioprinting and Nano-Biomaterials in Tissue Engineering and Regenerative Medicine. Front. Bioeng. Biotechnol. 2020, 8, 326.
- Shin, K.; Acri, T.; Geary, S.; Salem, A.K. Biomimetic Mineralization of Biomaterials Using Simulated Body Fluids for Bone Tissue Engineering and Regenerative Medicine. Tissue Eng. Part A 2017, 23, 1169–1180.
- Hindy, O.A.; Goker, M.; Yilgor Huri, P. Nanoscale agents within 3D-printed constructs: Intersection of nanotechnology and personalized bone tissue engineering. Emergent Mater. 2022, 5, 195–205.
- Chen, Y.; Kawazoe, N.; Chen, G. Preparation of dexamethasone-loaded biphasic calcium phosphate nanoparticles/collagen porous composite scaffolds for bone tissue engineering. Acta Biomater. 2018, 67, 341–353.
- Sokolova, V.; Kostka, K.; Shalumon, K.T.; Prymak, O.; Chen, J.-P.; Epple, M. Synthesis and characterization of PLGA/HAP scaffolds with DNA-functionalised calcium phosphate nanoparticles for bone tissue engineering. J. Mater. Sci. Mater. Med. 2020, 31, 102.
- Ha, S.-W.; Viggeswarapu, M.; Habib, M.M.; Beck, G.R. Bioactive effects of silica nanoparticles on bone cells are size, surface, and composition dependent. Acta Biomater. 2018, 82, 184–196.
- Echazú, M.I.A.; Renou, S.J.; Alvarez, G.S.; Desimone, M.F.; Olmedo, D.G. Synthesis and Evaluation of a Chitosan–Silica-Based Bone Substitute for Tissue Engineering. Int. J. Mol. Sci. 2022, 23, 13379.
- Shuai, C.; Yang, F.; Shuai, Y.; Peng, S.; Chen, S.; Deng, Y.; Feng, P. Silicon dioxide nanoparticles decorated on graphene oxide nanosheets and their application in poly(l-lactic acid) scaffold. J. Adv. Res. 2023, 48, 175–190.
- Li, Y.; Yang, Y.; Qing, Y.; Li, R.; Tang, X.; Guo, D.; Qin, Y. Enhancing ZnO-NP Antibacterial and Osteogenesis Properties in Orthopedic Applications: A Review. Int. J. Nanomed. 2020, 15, 6247–6262.
- Kandasamy, S.; Narayanan, V.; Sumathi, S. Zinc and manganese substituted hydroxyapatite/CMC/PVP electrospun composite for bone repair applications. Int. J. Biol. Macromol. 2020, 145, 1018–1030.
- Singh, T.A.; Sharma, A.; Tejwan, N.; Ghosh, N.; Das, J.; Sil, P.C. A state of the art review on the synthesis, antibacterial, antioxidant, antidiabetic and tissue regeneration activities of zinc oxide nanoparticles. Adv. Colloid Interface Sci. 2021, 295, 102495.
- Cho, Y.S.; Kim, H.-K.; Ghim, M.-S.; Hong, M.W.; Kim, Y.Y.; Cho, Y.-S. Evaluation of the Antibacterial Activity and Cell Response for 3D-Printed Polycaprolactone/Nanohydroxyapatite Scaffold with Zinc Oxide Coating. Polymers 2020, 12, 2193.
- Forero, J.C.; Roa, E.; Reyes, J.G.; Acevedo, C.; Osses, N. Development of Useful Biomaterial for Bone Tissue Engineering by Incorporating Nano-Copper-Zinc Alloy (nCuZn) in Chitosan/Gelatin/Nano-Hydroxyapatite (Ch/G/nHAp) Scaffold. Materials 2017, 10, 1177.
- Mokhtarzadeh, A.; Eivazzadeh-Keihan, R.; Pashazadeh, P.; Hejazi, M.; Gharaatifar, N.; Hasanzadeh, M.; Baradaran, B.; de la Guardia, M. Nanomaterial-based biosensors for detection of pathogenic virus. Trends Anal. Chem. TRAC 2017, 97, 445–457.
- Chenab, K.K.; Eivazzadeh-Keihan, R.; Maleki, A.; Pashazadeh-Panahi, P.; Hamblin, M.R.; Mokhtarzadeh, A. Biomedical applications of nanoflares: Targeted intracellular fluorescence probes. Nanomed. Nanotechnol. Biol. Med. 2019, 17, 342–358.
- Qing, Y.; Cheng, L.; Li, R.; Liu, G.; Zhang, Y.; Tang, X.; Wang, J.; Liu, H.; Qin, Y. Potential antibacterial mechanism of silver nanoparticles and the optimization of orthopedic implants by advanced modification technologies. Int. J. Nanomed. 2018, 13, 3311–3327.
- Wang, Y.-C.; Lin, S.-H.; Chien, C.-S.; Kung, J.-C.; Shih, C.-J. In Vitro Bioactivity and Antibacterial Effects of a Silver-Containing Mesoporous Bioactive Glass Film on the Surface of Titanium Implants. Int. J. Mol. Sci. 2022, 23, 9291.
- Eivazzadeh-Keihan, R.; Noruzi, E.B.; Chenab, K.K.; Jafari, A.; Radinekiyan, F.; Hashemi, S.M.; Ahmadpour, F.; Behboudi, A.; Mosafer, J.; Mokhtarzadeh, A.; et al. Metal-based nanoparticles for bone tissue engineering. J. Tissue Eng. Regen. Med. 2020, 14, 1687–1714.
- Xu, L.; Wang, Y.-Y.; Huang, J.; Chen, C.-Y.; Wang, Z.-X.; Xie, H. Silver nanoparticles: Synthesis, medical applications and biosafety. Theranostics 2020, 10, 8996–9031.
- Padmanabhan, V.P.; Sivashanmugam, P.; Kulandaivelu, R.; Sagadevan, S.; Sridevi, B.; Govindasamy, R.; Thiruvengadam, M. Biosynthesised Silver Nanoparticles Loading onto Biphasic Calcium Phosphate for Antibacterial and Bone Tissue Engineering Applications. Antibiotics 2022, 11, 1780.
- Akturk, A.; Taygun, M.E.; Goller, G. Optimization of the electrospinning process variables for gelatin/silver nanoparticles/bioactive glass nanocomposites for bone tissue engineering—Akturk—2020—Polymer Composites—Wiley Online Library. Polym. Compos. 2020, 41, 2411–2425.
- Vaidhyanathan, B.; Vincent, P.; Vadivel, S.; Karuppiah, P.; Al-Dhabi, N.A.; Sadhasivam, D.R.; Vimalraj, S.; Saravanan, S. Fabrication and Investigation of the Suitability of Chitosan-Silver Composite Scaffolds for Bone Tissue Engineering Applications. Process Biochem. 2021, 100, 178–187.
- Lopes, J.; Ferreira-Gonçalves, T.; Ascensão, L.; Viana, A.S.; Carvalho, L.; Catarino, J.; Faísca, P.; Oliva, A.; Barros, D.P.C.d.; Rodrigues, C.M.P.; et al. Safety of Gold Nanoparticles: From In Vitro to In Vivo Testing Array Checklist. Pharmaceutics 2023, 15, 1120.
- Tang, Y.; Shen, Y.; Huang, L.; Lv, G.; Lei, C.; Fan, X.; Lin, F.; Zhang, Y.; Wu, L.; Yang, Y. In vitro cytotoxicity of gold nanorods in A549 cells. Environ. Toxicol. Pharmacol. 2015, 39, 871–878.
- Pooja, D.; Panyaram, S.; Kulhari, H.; Rachamalla, S.S.; Sistla, R. Xanthan gum stabilized gold nanoparticles: Characterization, biocompatibility, stability and cytotoxicity. Carbohydr. Polym. 2014, 110, 1–9.
- Ko, W.-C.; Wang, S.-J.; Hsiao, C.-Y.; Hung, C.-T.; Hsu, Y.-J.; Chang, D.-C.; Hung, C.-F. Pharmacological Role of Functionalized Gold Nanoparticles in Disease Applications. Molecules 2022, 27, 1551.
- Nekounam, H.; Allahyari, Z.; Gholizadeh, S.; Mirzaei, E.; Shokrgozar, M.A.; Faridi-Majidi, R. Simple and robust fabrication and characterization of conductive carbonized nanofibers loaded with gold nanoparticles for bone tissue engineering applications. Mater. Sci. Eng. C Mater. Biol. Appl. 2020, 117, 111226.
- Yu, M.; Lei, B.; Gao, C.; Yan, J.; Ma, P.X. Optimizing surface-engineered ultra-small gold nanoparticles for highly efficient miRNA delivery to enhance osteogenic differentiation of bone mesenchymal stromal cells. Nano Res. 2016, 10, 49–63.
- Hou, Y.; Cai, K.; Li, J.; Chen, X.; Lai, M.; Hu, Y.; Luo, Z.; Ding, X.; Xu, D. Effects of titanium nanoparticles on adhesion, migration, proliferation, and differentiation of mesenchymal stem cells. Int. J. Nanomed. 2013, 8, 3619–3630.
- Kumar, P. Nano-TiO2 Doped Chitosan Scaffold for the Bone Tissue Engineering Applications. Int. J. Biomater. 2018, 2018, 6576157.
- Pattanashetti, N.A.; Hiremath, C.; Naik, S.R.; Heggannavar, G.B.; Kariduraganavar, M.Y. Development of nanofibrous scaffolds by varying the TiO2 content in crosslinked PVA for bone tissue engineering. New J. Chem. 2020, 44, 2111–2121.
More
Information
Subjects:
Cell & Tissue Engineering
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
534
Revisions:
2 times
(View History)
Update Date:
22 Nov 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





