Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Birgitta Dresp | -- | 1755 | 2023-11-21 11:03:28 | | | |
| 2 | Rita Xu | Meta information modification | 1755 | 2023-11-21 11:09:59 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Dresp-Langley, B. COVID-19 Pandemic And Mental Health. Encyclopedia. Available online: https://encyclopedia.pub/entry/51839 (accessed on 07 February 2026).
Dresp-Langley B. COVID-19 Pandemic And Mental Health. Encyclopedia. Available at: https://encyclopedia.pub/entry/51839. Accessed February 07, 2026.
Dresp-Langley, Birgitta. "COVID-19 Pandemic And Mental Health" Encyclopedia, https://encyclopedia.pub/entry/51839 (accessed February 07, 2026).
Dresp-Langley, B. (2023, November 21). COVID-19 Pandemic And Mental Health. In Encyclopedia. https://encyclopedia.pub/entry/51839
Dresp-Langley, Birgitta. "COVID-19 Pandemic And Mental Health." Encyclopedia. Web. 21 November, 2023.
Copy Citation
When “hijacked” by compulsive behaviors that affect the reward and stress centers of the brain, functional changes in the dopamine circuitry occur as the consequence of pathological brain adaptation. As a brain correlate of mental health, dopamine has a central functional role in behavioral regulation from healthy reward-seeking to pathological adaptation to stress in response to adversity.
dopamine
brain
addiction
stress
anhedonia
1. Introduction
The neurotransmitter dopamine fulfills a critical function in regulating the responses of the mesolimbic system, also known as the reward system, in the neural circuits of the mammalian brain [1]. The reward system governs and regulates responses ranging from pleasure and cravings to disgust and anhedonia, triggered by chemicals and other stimuli and guiding a larger proportion of our behavior than we may be aware of or are ready to admit [2]. In ancient times, the function of the reward system made the difference between life and death, because it made us and other species deploy most of our or their attention and behavioral effort towards things that were important for the survival of the species, such as food, sleep, and sex. Our ancestors did not have a supermarket around the corner but had to hunt for food and often had to deploy a considerable amount of time and energy to find it. An individual who found sweet fruit in the environment, for example, had better consume it quickly, in as large of quantities as possible, before another did. Ripe fruits have the highest sugar content and provide higher amounts of instant energy compared with other foods. The human preference for sweet nutrients may, indeed, be due to the evolutionary advantage that craving and eating high-calorie foods has caused. Responding selectively to survival-relevant stimuli, in the course of evolution, has become hardwired into the brain’s reward system [3]. Food, sleep, physical contact, and sex are primary stimuli that reinforce the neural connections of the reward system, and a craving for these primary stimuli is inherent in humans [4], as well as most other mammals [5]. The reward system is composed of brain structures that mediate the physiological and cognitive aspects of a reward. This involves neurobiological processes driving the brain’s capapcity to associate stimuli such as substances or activities with a pleasant and positive outcome. Reward-associated mechanisms explain why individuals search for initially positive stimuli again and again and why this can ultimately lead to compulsive behaviors and addicions that pose a threat to mental health. Pandemic-related adversities and the stresses they engendered [6], with the long lockdown periods where people in social isolation had to rely on food for comfort or digital tools to get feedback rewards via the internet, can be seen as major triggers of changes in motivation and compulsive reward-seeking behaviors worldwide. These are linked here to the pathological adaptation of dopamine-mediated reward circuitry, triggered and consolidated through functional links with brain structures controlling the circadian rythm and/or the responses to chronic stress. This offersplausible insight into why environmental adversity pushed individuals of all nations, during and after the pandemic, into compulsive behaviors that couldlead to sleep disorders, anhedonia (from the Greek language: “inability to feel or experience pleasure”), depression, and in extreme cases, suicidal ideation.
2. COVID-19 Pandemic and Mental Health
In 2022, the World Health Organisation (WHO) issued a brief [7] with facts and figures showing that the COVID-19 pandemic has had a severe impact on the mental health and well-being of people around the world. While many individuals have adapted, others have experienced mental health problems that, only in some cases, are a consequence of COVID-19 infection. The brief stated further that the pandemic also continues to impede access to mental health services and raised concerns about increases in suicidal behavior, stressing the causal role of psychological and environmental factors producing ontological insecurity in individuals and populations. In the wake of the COVID-19 pandemic, experts havewitnessed a
- ➢
-
significant rise in addictions and related mental illnesses;
- ➢
-
significant rise in the corresponding anti-depressant prescription uptake;
- ➢
-
increased risk of suicidal ideation or suicide.
Any potential doubts about the impact of COVID-19 on mental health have been largely put to rest by the most recent papers on the topic [8][9][10][11][12]. Loneliness, physical exhaustion, sleep disturbances, and anhedonia linked to compulsive or addictive behaviors such as binge-eating [13][14], substance abuse [15], and digital reward craving [16] were identified asbeing linked to suicidal ideation [13][17][18]—in particular, in younger individuals—during and after the pandemic. These reflect some of the most negative effects of pandemic-related adversity on mental health worldwide.
2.1. Adversity and Vulnerability
Mental health issues arise from a specific context. Recently reported effects of the pandemic have shown, beyond all reasonable doubt, that adversity affects people’s capacity tocope with the stresses it produces. Conditions of extreme adversity challenge the stress and immune system responses needed for coping, and beyond a certain threshold, such conditions can trigger behavioral changes as listed and discussed here above; all of them have been functionally linked to the complex brain pathways involving dopamine release, reward mechanisms, and their interactions or regulations [19][20]. During the different waves of the pandemic, many individuals had an actual COVID-19 infection, with direct effects on the brain’s immune system, stress centers, and the dopamine system, affecting people’s mood beyond the actual duration of the illness. Cohort studies examining the psychopathological and cognitive status of COVID-19 pneumonia survivors [21], for example, have shown that three months after discharge from the hospital, close to 40% still self-rated their symptoms in the clinical range for at least one psychopathological dimension, with persistent depressive symptomatology, while anxiety and insomnia progressively decreased during follow-up. Studies on the impact of the COVID-19 pandemic on individuals with eating disorders have been performed all over the world, showing that the traumatic effects of COVID-19 have exacerbated specific eating disorder-related psychopathologies [22], pointing towards complex interactions between environmental and personal factors. Healthy siblings of patients with eating disorders have beenfound to present specific psychological vulnerabilities, i.e., specific associations between interpersonal sensitivity and posttraumatic symptoms, including anxiety, depression, and compulsive behaviors [22][23]. Moreover, having to cope with adversity during childhood increases the risk of mental health problems in adulthood, and it has been suggested that this effect may be mediated by increased striatal dopamine neurotransmission [24]. Also, while resilience may be viewed as an individual’s positive adaptation to experiences of adversity [25], it is also known that conditions of adversity reinforce the already exisiting vulnerability to mental illness and may create a new vulnerabilty duringspecific adverse contexts such as a pandemic [10] or armed conflict [26]. It has been confirmed that stress responses can cause functional changes in the amygdala and the dopaminergic circuits of the brain in relation to stress-induced cortisol release mechanisms [26][27][28]. Some of these studies have shown a cortisol-induced increase in serotonin in subjects with major depressive disorder, offering further insight into the functional links between stress, sleep disorders, and depression, where an increase in one brain correlate affects another, thereby creating or increasing the physiological vulnerability to mental illness in individuals under prolonged stress.
2.2. Bingeing
The COVID-19 pandemic creatednegative health consequences such as consuming high-fat and sugar foods, increasing body weight [29], anxiety and depression [30], anhedonia [30][31], or a combination thereof [32]. As a core characteristic of eating disorders and all forms of addiction [33], bingeing is associated with changes in the activity of the brain’s reward system in the process of pathological adaptation of the central nervous system through deregulation of the reward mechanisms generating positive reinforcement. As explained earlier, this deregulation progressively leads to the consolidation of the anti-reward brain state that produces anxiety, anhedonia, and depression. Most people during COVID-19 lockdown reportedly turned to substances or other “rewarding” activities to deal with the stress of isolation and the negative feelings it engendered [34][35]. A number of factors related to the COVID-19 pandemic may have contributed to the reportedly high incidence of food addictions during and after that period [35][36]. It has been suggested that people under the influence of the excessive and uncontrolled consumption of extremely palatable foods experience similar highreward sensations as recorded for addicts resorting to classic intoxicants, both at the behavioral and neurobiological levels [35][36][37]. As lives and daily routines were transformed by the pandemic and rapidly rising anxiety fueled by social isolation and, often, unemployment, the mental health of millions is at stake. In the United States alone [38], close to 60% of adults screened declared that the pandemic led them to abuse alcohol and other drugs, binge eating, and/or compulsive internet gambling.
2.3. The New Digital Drug
COVID-19 spread across the world ata rapid pace, and to further limit the spread of infection, lockdowns were declared in most parts of the world. People were forced to stay indoors, and the internet was the only source of entertainment. This context engendered addictive behavior with measurable negative effects on anxiety and sleep quality, especially among younger individuals [38][39][40][41]. Digital addiction involves theinternet as a channel through which individuals may access whatever content they want (games, social media, shopping, etc.) wherever and whenever they want. The development of the addictive response is digitally facilitated by such instant availability [40][41][42][43][44][45]. At an advanced stage, digital addiction [41] is associated with significant and permanent symptomatic psychological, cognitive, and physiological states, with a measurable dopamine deficiency and impaired mental health [44]. Psychological stress [44][45][46][47], anxiety and depression [48][49][50], eating disorders [51][52][53], sleeplessness [54][55], and mood changes, along with suicidal ideation [56][57], are the most frequently reported. A compilation of cross-national studies on more than 89,000 participants from 31 nations performed almost ten years ago, well before the COVID-19 pandemic, already suggested a global prevalence estimate for digital addiction of 6% worldwide [43]. Interdependent variables such as sociocultural factors, biological vulnerabilities (genetic predisposition and preexisting metabolic disorders), and psychological factors (personality characteristics and a negative affect) play a critical role [58][59][60][61][62][63]. Excessive seeking of the new digital drug and addiction to the internet have been identified as part of the consequences of the COVID-19 pandemic, with a major impact on the mental health of predominantly young people and teenagers [61][62][63][64][65][66][67][68][69]. This involves, like all compulsive behavior loops, the brain’s reward circuitry, with all the complex interactions between environmental, metabolic, and neurobiological changes in the brain discussed above. Dopamine, and the modulation thereof under conditions of adversity and stress (Figure 1), is the common functional denominator [70].
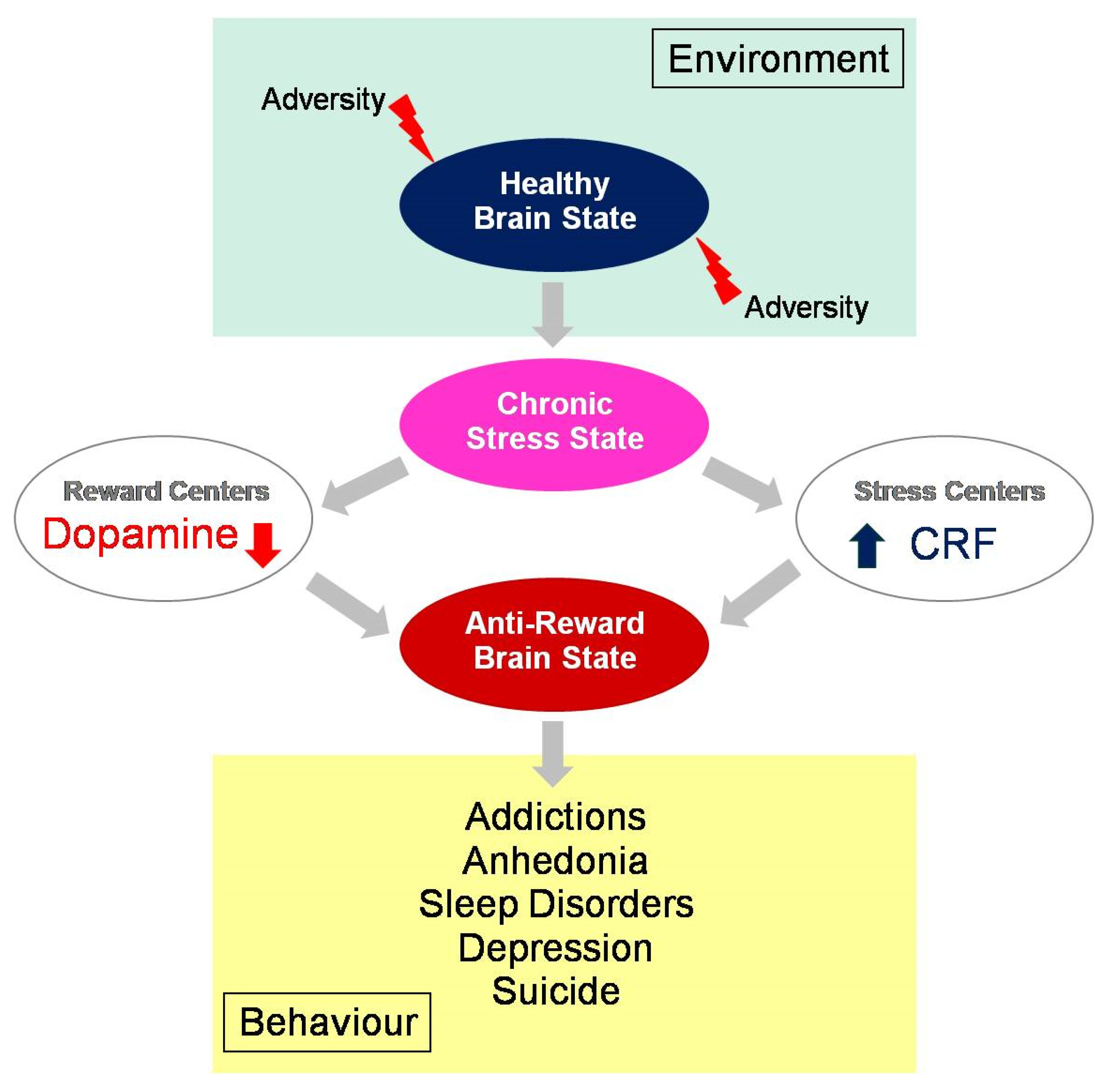
Figure 1. Behavioral consequences of an anti-reward brain state, with ultimately depleted dopamine levels in the reward centersand increased cortisol levels in the centers that regulate the brain’s response in pathological adaptation to chronic stress. Under adverse environmental conditions, such as those generated by the COVID-19 pandemic, healthy reward-seeking has progressively evolved into stress-related compulsory behaviors and/or addictions leading to anhedonia and related mental health issues worldwide.
References
- Lewis, R.G.; Florio, E.; Punzo, D.; Borrelli, E. The Brain’s Reward System in Health and Disease. Adv. Exp. Med. Biol. 2021, 1344, 57–69.
- Kringelbach, M.L.; Berridge, K.C. The Functional Neuroanatomy of Pleasure and Happiness. Discov. Med. 2010, 9, 579–587.
- Robbins, T.W.; Everitt, B.J. Neurobehavioural mechanisms of reward and motivation. Curr. Opin. Neurobiol. 1996, 6, 228–236.
- De Decker, A.; On behalf of the I. Family Consortium; Verbeken, S.; Sioen, I.; Van Lippevelde, W.; Braet, C.; Eiben, G.; Pala, V.; Reish, L.A.; De Henauw, S. Palatable food consumption in children: Interplay between (food) reward motivation and the home food environment. Eur. J. Pediatr. 2017, 176, 465–474.
- Everitt, B.J. Sexual motivation: A neural and behavioural analysis of the mechanisms underlying appetitive and copulatory responses of male rats. Neurosci. Biobehav. Rev. 1990, 14, 217–232.
- Manchia, M.; Gathier, A.W.; Yapici-Eser, H.; Schmidt, M.V.; de Quervain, D.; van Amelsvoort, T.; Bisson, J.I.; Cryan, J.F.; Howes, O.D.; Pinto, L.; et al. The impact of the prolonged COVID-19 pandemic on stress resilience and mental health: A critical review across waves. Eur. Neuropsychopharmacol. 2022, 55, 22–83.
- World Health Organization. Mental Health and COVID-19, Early Evidence of the Pandemics Impact. 2022. Available online: https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1 (accessed on 5 September 2023).
- Oakes, M.B. Ontological insecurity in the post-Covid-19 fallout: Using existentialism as a method to develop a psychosocial understanding to a mental health crisis. Med. Health Care Philos. 2023, 30, 425–432.
- Tomlinson, M.; Marlow, M. COVID-19 and mental health: Building back better or reimagining a new way forward? PLoS Med. 2023, 20, e1004216.
- Winkler, P.; Mohrova, Z.; Mlada, K.; Kuklova, M.; Kagstrom, A.; Mohr, P.; Formanek, T. Prevalence of current mental disorders before and during the second wave of COVID-19 pandemic: An analysis of repeated nationwide cross-sectional surveys. J. Psychiatr. Res. 2021, 139, 167–171.
- Pierce, M.; McManus, S.; Hope, H.; Hotopf, M.; Ford, T.; Hatch, S.L.; John, A.; Kontopantelis, E.; Webb, R.T.; Wessely, S.; et al. Mental health responses to the COVID-19 pandemic: A latent class trajectory analysis using longitudinal UK data. Lancet Psychiatry 2021, 8, 610–619.
- Knudsen, A.K.S.; Stene-Larsen, K.; Gustavson, K.; Hotopf, M.; Kessler, R.C.; Krokstad, S.; Skogen, J.C.; Øverland, S.; Reneflot, A. Prevalence of mental disorders, suicidal ideation and suicides in the general population before and during the COVID-19 pandemic in Norway: A population-based repeated cross-sectional analysis. Lancet Reg. Health Eur. 2021, 4, 100071.
- Davies, H.L.; Hübel, C.; Herle, M.; Kakar, S.; Mundy, J.; Peel, A.J.; Ter Kuile, A.R.; Zvrskovec, J.; Monssen, D.; Lim, K.X.; et al. Risk and protective factors for new-onset binge eating, low weight, and self-harm symptoms in >35,000 individuals in the UK during the COVID-19 pandemic. Int. J. Eat. Disord. 2023, 56, 91–107.
- Güzel, Â.; Mutlu, N.L.; Molendijk, M. COVID-19-related changes in eating disorder pathology, emotional and binge eating and need for care: A systematic review with frequentist and Bayesian meta-analyses. Eat. Weight Disord. 2023, 28, 19.
- Martinelli, T.F.; Nagelhout, G.E.; Best, D.; Vanderplasschen, W.; Van de Mheen, D. Factors associated with problematic substance use before and during the COVID-19 pandemic among a drug addiction recovery cohort: A prospective study in the Netherlands, Belgium, and UK. J. Subst. Use Addict. Treat. 2023, 148, 209025.
- Zhao, L.; Li, X.; Yang, Q.; Peng, Y.; Jiang, L.; Jia, P.; Shi, W. The longitudinal association between internet addiction and depressive and anxiety symptoms among Chinese adolescents before and during the COVID-19 pandemic. Front. Public Health 2023, 10, 1096660.
- Stanley, I.H.; Flarity, K.M.; April, M.D. Suicide Ideation, Plans, and Attempts Attributed to the COVID-19 Pandemic Among US Veterans. JAMA Netw. Open 2023, 6, e2320193.
- Tardeh, S.; Adibi, A.; Mozafari, A.A. Prevalence of Suicide Ideation and Attempt during COVID-19 Pandemic: A Systematic Review and Meta-Analysis. Int. J. Prev. Med. 2023, 14, 9.
- Baik, J.H. Stress and the dopaminergic reward system. Exp. Mol. Med. 2020, 52, 1879–1890.
- Correia, A.S.; Cardoso, A.; Vale, N. Oxidative Stress in Depression: The Link with the Stress Response, Neuroinflammation, Serotonin, Neurogenesis and Synaptic Plasticity. Antioxidants 2023, 12, 470.
- Mazza, M.G.; De Lorenzo, R.; Conte, C.; Poletti, S.; Vai, B.; Bollettini, I.; Melloni, E.M.T.; Furlan, R.; Ciceri, F.; Rovere-Querini, P.; et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav. Immun. 2020, 89, 594–600.
- Meneguzzo, P.; De Mico, A.; Gori, P.; Ajello, A.; Ceccato, E.; Consolati, M.D.; Vita, A.; Sala, A.; Santonastaso, P. A Multicenter Network Analysis Examining the Psychological Effects of the COVID-19 Pandemic on Patients with Eating Disorders versus Their Healthy Siblings. J. Clin. Med. 2022, 11, 7187.
- Meneguzzo, P.; Sala, A.; Merlino, L.; Ceccato, E.; Santonastaso, P. One year of COVID-19 pandemic on patients with eating disorders, healthy sisters, and community women: Evidence of psychological vulnerabilities. Eat. Weight Disord. 2022, 27, 3429–3438.
- Egerton, A.; Valmaggia, L.R.; Howes, O.D.; Day, F.; Chaddock, C.A.; Allen, P.; Winton-Brown, T.T.; Bloomfield, M.A.P.; Bhattacharyya, S.; Chilcott, J.; et al. Adversity in childhood linked to elevated striatal dopamine function in adulthood. Schizophr. Res. 2016, 176, 171–176.
- Chuang, S.P.; Wu, J.Y.W.; Wang, C.S. Resilience and Quality of Life in People with Mental Illness: A Systematic Review and Meta-Analysis. Neuropsychiatr. Dis. Treat 2023, 19, 507–514.
- Østergaard, M.L.D.; Aponte-Canencio, D.M.; Ortiz, Y.B.; Botero, H.J.V.; Modvig, J.S.; Brasholt, M. Vulnerability factors in conflict-related mental health. Med. Confl. Surviv. 2023, 39, 63–80.
- Oswald, L.M.; Wong, D.F.; McCaul, M.; Zhou, Y.; Kuwabara, H.; Choi, L.; Brasic, J.; Wand, G.S. Relationships among ventral striatal dopamine release, cortisol secretion, and subjective responses to amphetamine. Neuropsychopharmacology 2005, 30, 821–832.
- Wand, G.S.; Oswald, L.M.; McCaul, M.E.; Wong, D.F.; Johnson, E.; Zhou, Y.; Kuwabara, H.; Kumar, A. Association of amphetamine-induced striatal dopamine release and cortisol responses to psychological stress. Neuropsychopharmacology 2007, 32, 2310–2320.
- Yaribeygi, H.; Panahi, Y.; Sahraei, H.; Johnston, T.P.; Sahebkar, A. The impact of stress on body function: A review. EXCLI J. 2017, 16, 1057–1072.
- Fleischer, E.; Landaeta-Díaz, L.; González-Medina, G.; Horovitz, O. Anxiety, anhedonia, and related food consumption in Israelis populations: An online cross-sectional study two years since the outbreak of COVID-19. Heliyon 2023, 9, e17211.
- Vindegaard, N.; Benros, M.E. COVID-19 pandemic and mental health consequences: Systematic review of the current evidence. Brain Behav. Immun. 2020, 89, 531–542.
- Alloy, L.B.; Chat, I.K.; Grehl, M.M.; Stephenson, A.R.; Adogli, Z.V.; Olino, T.M.; Ellman, L.M.; Miller, G.E.; Nusslock, R. Reward and Immune Systems in Emotion (RISE) prospective longitudinal study: Protocol overview of an integrative reward-inflammation model of first onset of major depression in adolescence. Brain Behav. Immun. Health 2023, 30, 100643.
- Kronberg, G.; Goldstein, R.Z. An fMRI marker of drug and food craving. Nat. Neurosci. 2023, 26, 178–180.
- Costa, R.; Pinto, T.M.; Conde, A.; Mesquita, A.; Motrico, E.; Figueiredo, B. Women’s perinatal depression: Anhedonia-related symptoms have increased in the COVID-19 pandemic. Gen. Hosp. Psychiatry 2023, 84, 102–111.
- Zielińska, M.; Łuszczki, E.; Bartosiewicz, A.; Wyszyńska, J.; Dereń, K. The Prevalence of “Food Addiction” during the COVID-19 Pandemic Measured Using the Yale Food Addiction Scale 2.0 (YFAS 2.0) among the Adult Population of Poland. Nutrients 2021, 13, 4115.
- Flaudias, V.; Iceta, S.; Zerhouni, O.; Rodgers, R.F.; Billieux, J.; Llorca, P.M.; Boudesseul, J.; de Chazeron, I.; Romo, L.; Maurage, P.; et al. COVID-19 pandemic lockdown and problematic eating behaviors in a student population. J. Behav. Addict. 2020, 9, 826–835.
- Ellis, J.; Ferini-Strambi, L.; García-Borreguero, D.; Heidbreder, A.; O’Regan, D.; Parrino, L.; Selsick, H.; Penzel, T. Chronic Insomnia Disorder across Europe: Expert Opinion on Challenges and Opportunities to Improve Care. Healthcare 2023, 11, 716.
- Avena, N.M.; Simkus, J.; Lewandowski, A.; Gold, M.S.; Potenza, M.N. Substance Use Disorders and Behavioral Addictions during the COVID-19 Pandemic and COVID-19-Related Restrictions. Front. Psychiatry 2021, 12, 653674.
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 112954.
- Lin, M.-P. Prevalence of Internet Addiction during the COVID-19 Outbreak and Its Risk Factors among Junior High School Students in Taiwan. Int. J. Environ. Res. Public Health 2020, 17, 8547.
- Dresp-Langley, B.; Hutt, A. Digital Addiction and Sleep. Int. J. Environ. Res. Public Health 2022, 19, 6910.
- Griffiths, M.D.; Pontes, H.M. Internet Addiction Disorder and Internet Gaming Disorder are not the same. J. Addict. Res. Ther. 2014, 5, e1.
- Cheng, C.; Li, A.Y. Internet addiction prevalence and quality of (real) life: A meta-analysis of 31 nations across seven world regions. Cyberpsychol. Behav. Soc. Netw. 2014, 17, 755–760.
- Liu, M.; Luo, J. Relationship between peripheral blood dopamine level and internet addiction disorder in adolescents: A pilot study. Int. J. Clin. Exp. Med. 2015, 8, 9943–9948.
- Nalwa, K.; Anand, A.P. Internet addiction in students: A cause of concern. Cyberpsychol. Behav. 2003, 6, 653–656.
- Cao, F.; Su, L. Internet addiction among Chinese adolescents: Prevalence and psychological features. Child Care Health Dev. 2006, 33, 275–281.
- Fu, K.W.; Chan, W.S.; Wong, P.W.; Yip, P.S. Internet addiction: Prevalence, discriminant validity and correlates among adolescents in Hong Kong. Br. J. Psychiatry 2010, 196, 486–492.
- Saikia, A.M.; Das, J.; Barman, P.; Bharali, M.D. Internet Addiction and its Relationships with Depression, Anxiety, and Stress in Urban Adolescents of Kamrup District, Assam. J.Fam. Community Med. 2019, 26, 108–112.
- Dalbudak, E.; Evren, C.; Aldemir, S.; Coskun, K.S.; Ugurlu, H.; Yildirim, F.G. Relationship of internet addiction severity with depression, anxiety and alexithymia, temperament, and character in university students. Cyberpsychol. Behav. Soc. Netw. 2013, 16, 272–278.
- Shakya, H.B.; Christakis, N.A. Association of ‘Facebook’ use with compromised well-being: A longitudinal study. Am. J. Epidemiol. 2017, 185, 203–211.
- Lau, J.T.F.; Walden, D.L.; Wu, A.M.S.; Cheng, K.M.; Lau, M.C.M.; Mo, P.K.H. Bidirectional predictions between Internet addiction and probable depression among Chinese adolescents. J. Behav. Addict. 2018, 7, 633–643.
- Hinojo-Lucena, F.J.; Aznar-Díaz, I.; Cáceres-Reche, M.P.; Trujillo-Torres, J.M.; Romero-Rodríguez, J.M. Problematic Internet Use as a Predictor of Eating Disorders in Students: A Systematic Review and Meta-Analysis Study. Nutrients 2019, 11, 2151.
- Moreno, M.A.; Eickhoff, J.; Zhao, Q.; Suris, J.C. College Students and Problematic Internet Use: A Pilot Study Assessing Self-Appraisal and Independent Behavior Change. J. Adolesc. Health 2019, 64, 131–133.
- Krishnamurthy, S.; Chetlapalli, S.K. Internet addiction: Prevalence and risk factors: A cross-sectional study among college students in Bengaluru, the Silicon Valley of India. Indian J. Public Health 2015, 59, 115–121.
- Li, J.B.; Lau, J.T.F.; Mo, P.K.H.; Su, X.F.; Tang, J.; Qin, Z.G.; Gross, D.L. Insomnia partially mediates the association between problematic Internet use and depression among secondary school students in China. J. Behav. Addict. 2017, 6, 554–563.
- Chen, Y.L.; Gau, S.S. Sleep problems and internet addiction among children and adolescents: A longitudinal study. J. Sleep. Res. 2016, 25, 458–465.
- Kim, K.; Ryu, E.; Chon, M.-Y.; Yeun, E.-J.; Choi, S.-Y.; Seo, J.-S.; Nam, B.-W. Internet addiction in Korean adolescents and its relation to depression and suicidal ideation: A questionnaire survey. Int. J. Nurs. Stud. 2006, 43, 185–192.
- Keles, B.; McCrae, N.; Grealish, A. A systematic review: The influence of social media on depression, anxiety and psychological distress in adolescents. Int. J. Adolesc. Youth 2020, 25, 79–93.
- Yau, Y.H.; Potenza, M.N. Gambling disorder and other behavioral addictions: Recognition and treatment. Harv. Rev. Psychiatry 2015, 23, 134–146.
- Greenfield, D. Treatment Considerations in Internet and Video Game Addiction: A Qualitative Discussion. Child Adolesc. Clin. North Am. Rev. Youth Internet Habits Ment. Health 2018, 27, 327–344.
- Twenge, J.M. Have Smartphones Destroyed a Generation? Atlantic 2017. Available online: https://www.theatlantic.com/magazine/archive/2017/09/has-the-smartphone-destroyed-a-generation/534198/ (accessed on 5 September 2023).
- Dresp-Langley, B. Consciousness Beyond Neural Fields: Expanding the Possibilities of What Has Not Yet Happened. Front. Psychol. 2022, 12, 762349.
- Shaw, M.; Black, D.W. Internet addiction: Definition, assessment, epidemiology and clinical management. CNS Drugs 2008, 22, 353–365.
- Kuss, D.J.; Griffiths, M.D.; Karila, L.; Billieux, J. Internet addiction: A systematic review of epidemiological research for the last decade. Curr. Pharm. Des. 2014, 20, 4026–4052.
- Rumpf, H.-J.; Achab, S.; Billieux, J.; Bowden-Jones, H.; Carragher, N.; Demetrovics, Z.; Higuchi, S.; King, D.L.; Mann, K.; Potenza, M.; et al. Including gaming disorder in the ICD-11, the need to do so from a clinical and public health perspective. J. Behav. Addict. 2018, 7, 556–561.
- Onukwuli, V.O.; Onyinye, E.N.; Udigwe, I.B.; Umeh, U.M.; Enebe, J.T.; Umerah, A.T. Internet addiction during the COVID-19 pandemic among adolescents in southeast Nigeria and implications for adolescent care in the post-pandemic era: A cross-sectional study. SAGE Open Med. 2023, 11, 20503121231152763.
- Kumar, G.; Dash, P.; Jnaneswar, A.; Suresan, V.; Jha, K.; Ghosal, S. Impact of internet addiction during COVID-19 on anxiety and sleep quality among college students of Bhubaneswar city. J. Educ. Health Promot. 2022, 11, 156.
- Melca, I.A.; Teixeira, E.K.; Nardi, A.E.; Spear, A.L. Association of Internet Addiction and Mental Disorders in Medical Students: A Systematic Review. Prim. Care Companion CNS Disord. 2023, 25, 22r03384.
- Dresp-Langley, B. Children’s Health in the Digital Age. Int. J. Environ. Res. Public Health 2020, 17, 3240.
- Oster, H. The interplay between stress, circadian clocks, and energy metabolism. J. Endocrinol. 2020, 247, R13–R25.
More
Information
Contributor
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
615
Revisions:
2 times
(View History)
Update Date:
21 Nov 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




