
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Marco Daperno | -- | 1655 | 2023-11-14 09:23:25 | | | |
| 2 | Jessie Wu | Meta information modification | 1655 | 2023-11-15 03:05:33 | | |
Video Upload Options
Endoscopy is an essential tool supporting inflammatory bowel disease diagnosis, and ileocolonoscopy is essential to the diagnostic process because it allows for histological sampling. A decent description of endoscopic lesions may lead to a correct final diagnosis up to 89% of the time. Moreover, endoscopy is key to evaluating endoscopic severity, which in both Crohn’s disease and ulcerative colitis is associated with worse disease outcomes (e.g., more frequent advanced therapy requirements or more frequent hospitalizations and surgeries). Endoscopic severity should be reported according to validated endoscopic scores, such as the Mayo endoscopic subscore (MES) or the ulcerative colitis endoscopic index of severity (UCEIS) for ulcerative colitis, the Rutgeerts score for postoperative Crohn’s recurrence, and the Crohn’s disease endoscopic index of severity (CDEIS) or the simplified endoscopic score for Crohn’s disease (SES-CD) for luminal Crohn’s disease activity.
1. Introduction
2. Diagnosis
3. Severity Assessment
-
Deep and extensive ulcerations, bounded by swollen mucosa;
-
Mucosal detachment, which can be demonstrated by inserting the biopsy forceps under the edge of the ulceration;
-
Well-like ulcerations, visible as very deep ulcerations with a small diameter;
-
Large mucosal abrasions, formed by the junction of several deep ulcerations.
-
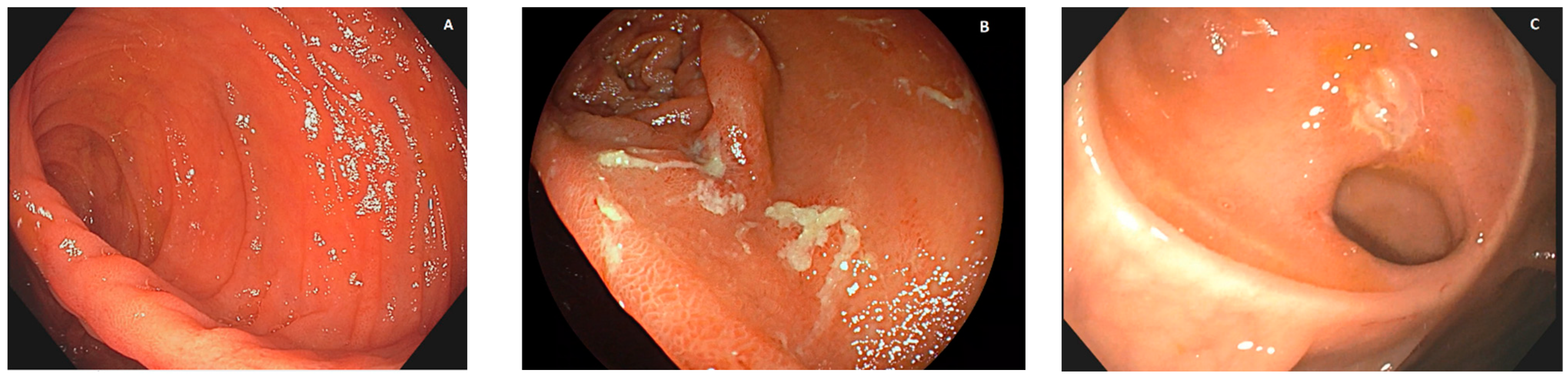
Patients with no recurrent lesions in the neoterminal ileum (i0; see Figure 1A) and those with up to five aphthous lesions in the neoterminal ileum (i1) had a clinical recurrence risk of 10% at 8 years;
-
Patients with more than five aphthous lesions in the neoterminal ileum with a normal mucosa between them, or with ulcers isolated from the anastomotic line (<1 cm), classified as i2, had a clinical recurrence risk of 40% at 5 years;
-
Patients with diffuse aphthous ileitis, with diffusely inflamed mucosa in between aphthae (classified as i3; see Figure 1B), had a clinical recurrence risk of 80% at 6 years;
-
Finally, patients with diffuse inflammation with already larger ulcers, nodules, and/or lumen narrowing (classified as i4; see Figure 1C) had a clinical recurrence risk of 100% at 4 years.
References
- Pera, A.; Bellando, P.; Caldera, D.; Ponti, V.; Astegiano, M.; Barletti, C.; David, E.; Arrigoni, A.; Rocca, G.; Verme, G. Colonoscopy in inflammatory bowel disease. Diagnostic accuracy and proposal of an endoscopic score. Gastroenterology 1987, 92, 181–185.
- Gomollon, F.; Dignass, A.; Annese, V.; Tilg, H.; Van Assche, G.; Lindsay, J.O.; Peyrin-Biroulet, L.; Cullen, G.J.; Daperno, M.; Kucharzik, T.; et al. 3rd European Evidence-based Consensus on the Diagnosis and Management of Crohn’s Disease 2016: Part 1: Diagnosis and Medical Management. J. Crohns Colitis 2017, 11, 3–25.
- Maaser, C.; Sturm, A.; Vavricka, S.R.; Kucharzik, T.; Fiorino, G.; Annese, V.; Calabrese, E.; Baumgart, D.C.; Bettenworth, D.; Borralho Nunes, P.; et al. ECCO-ESGAR Guideline for Diagnostic Assessment in IBD Part 1: Initial diagnosis, monitoring of known IBD, detection of complications. J. Crohns Colitis 2019, 13, 144–164.
- Satsangi, J.; Silverberg, M.S.; Vermeire, S.; Colombel, J.F. The Montreal classification of inflammatory bowel disease: Controversies, consensus, and implications. Gut 2006, 55, 749–753.
- Annese, V.; Daperno, M.; Rutter, M.D.; Amiot, A.; Bossuyt, P.; East, J.; Ferrante, M.; Gotz, M.; Katsanos, K.H.; Kiesslich, R.; et al. European evidence based consensus for endoscopy in inflammatory bowel disease. J. Crohns Colitis 2013, 7, 982–1018.
- Bourreille, A.; Ignjatovic, A.; Aabakken, L.; Loftus, E.V., Jr.; Eliakim, R.; Pennazio, M.; Bouhnik, Y.; Seidman, E.; Keuchel, M.; Albert, J.G.; et al. Role of small-bowel endoscopy in the management of patients with inflammatory bowel disease: An international OMED-ECCO consensus. Endoscopy 2009, 41, 618–637.
- Wolters, F.L.; Russel, M.G.; Sijbrandij, J.; Ambergen, T.; Odes, S.; Riis, L.; Langholz, E.; Politi, P.; Qasim, A.; Koutroubakis, I.; et al. Phenotype at diagnosis predicts recurrence rates in Crohn’s disease. Gut 2006, 55, 1124–1130.
- Cheifetz, A.S.; Kornbluth, A.A.; Legnani, P.; Schmelkin, I.; Brown, A.; Lichtiger, S.; Lewis, B.S. The risk of retention of the capsule endoscope in patients with known or suspected Crohn’s disease. Am. J. Gastroenterol. 2006, 101, 2218–2222.
- Allez, M.; Lemann, M.; Bonnet, J.; Cattan, P.; Jian, R.; Modigliani, R. Long term outcome of patients with active Crohn’s disease exhibiting extensive and deep ulcerations at colonoscopy. Am. J. Gastroenterol. 2002, 97, 947–953.
- Carbonnel, F.; Lavergne, A.; Lemann, M.; Bitoun, A.; Valleur, P.; Hautefeuille, P.; Galian, A.; Modigliani, R.; Rambaud, J.C. Colonoscopy of acute colitis. A safe and reliable tool for assessment of severity. Dig. Dis. Sci. 1994, 39, 1550–1557.
- Rutgeerts, P.; Geboes, K.; Vantrappen, G.; Beyls, J.; Kerremans, R.; Hiele, M. Predictability of the postoperative course of Crohn’s disease. Gastroenterology 1990, 99, 956–963.
- Ardizzone, S.; Cassinotti, A.; Duca, P.; Mazzali, C.; Penati, C.; Manes, G.; Marmo, R.; Massari, A.; Molteni, P.; Maconi, G.; et al. Mucosal healing predicts late outcomes after the first course of corticosteroids for newly diagnosed ulcerative colitis. Clin. Gastroenterol. Hepatol. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2011, 9, 483–489.e483.
- Baert, F.; Moortgat, L.; Van Assche, G.; Caenepeel, P.; Vergauwe, P.; De Vos, M.; Stokkers, P.; Hommes, D.; Rutgeerts, P.; Vermeire, S.; et al. Mucosal healing predicts sustained clinical remission in patients with early-stage Crohn’s disease. Gastroenterology 2010, 138, 463–468; quiz e410–461.
- Colombel, J.F.; Rutgeerts, P.; Reinisch, W.; Esser, D.; Wang, Y.; Lang, Y.; Marano, C.W.; Strauss, R.; Oddens, B.J.; Feagan, B.G.; et al. Early mucosal healing with infliximab is associated with improved long-term clinical outcomes in ulcerative colitis. Gastroenterology 2011, 141, 1194–1201.
- Louis, E.; Mary, J.Y.; Vernier-Massouille, G.; Grimaud, J.C.; Bouhnik, Y.; Laharie, D.; Dupas, J.L.; Pillant, H.; Picon, L.; Veyrac, M.; et al. Maintenance of remission among patients with Crohn’s disease on antimetabolite therapy after infliximab therapy is stopped. Gastroenterology 2012, 142, 63–70.e65; quiz e31.
- Schnitzler, F.; Fidder, H.; Ferrante, M.; Noman, M.; Arijs, I.; Van Assche, G.; Hoffman, I.; Van Steen, K.; Vermeire, S.; Rutgeerts, P. Mucosal healing predicts long-term outcome of maintenance therapy with infliximab in Crohn’s disease. Inflamm. Bowel Dis. 2009, 15, 1295–1301.
- Solberg, I.C.; Lygren, I.; Jahnsen, J.; Aadland, E.; Hoie, O.; Cvancarova, M.; Bernklev, T.; Henriksen, M.; Sauar, J.; Vatn, M.H.; et al. Clinical course during the first 10 years of ulcerative colitis: Results from a population-based inception cohort (IBSEN Study). Scand. J. Gastroenterol. 2009, 44, 431–440.
- Truelove, S.C.; Witts, L.J. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br. Med. J. 1955, 2, 1041–1048.
- Dal Piaz, G.; Mendolaro, M.; Mineccia, M.; Randazzo, C.; Massucco, P.; Cosimato, M.; Rigazio, C.; Guiotto, C.; Morello, E.; Ercole, E.; et al. Predictivity of early and late assessment for post-surgical recurrence of Crohn’s disease: Data from a single-center retrospective series. Dig. Liver Dis. Off. J. Ital. Soc. Gastroenterol. Ital. Assoc. Study Liver 2021, 53, 987–995.




