
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Vito Annese | -- | 1609 | 2023-10-26 20:47:45 | | | |
| 2 | Lindsay Dong | + 3 word(s) | 1612 | 2023-10-27 10:59:11 | | |
Video Upload Options
Ulcerative colitis and Crohn’s disease are traditionally defined as the two main subtypes of inflammatory bowel disease. However, a more recent view considers inflammatory bowel diseases (IBDs) as a spectrum of heterogeneous phenotypes with consistent differences in clinical presentation and behaviors, likely explained by differences in underlying pathogenetic mechanisms. The etiology is still elusive, and the suggested pathogenesis is a complex interplay among genetic predisposition and abnormal immune response at the mucosal intestinal level, activated by only partially identified environmental triggers leading to altered intestinal permeability and impaired handling of gut microbiota. The undeniable continuous progress of medical therapy with more frequent shifts from traditional to more advanced modalities also underlines the actual unmet needs.
1. Introduction
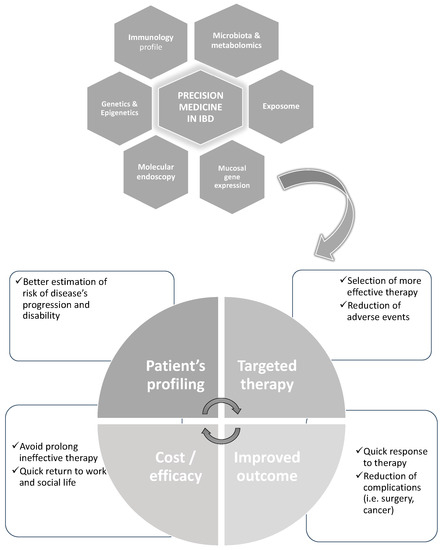
2. The Potential of Precision Medicine IBD
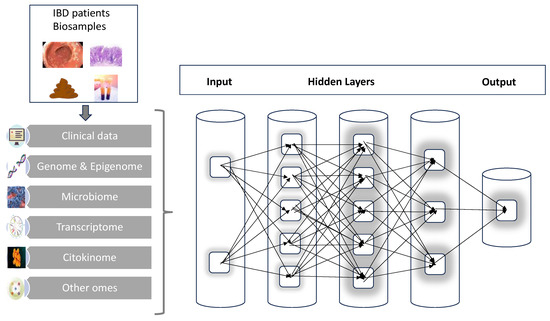
3. The Potential of Artificial Intelligence in IBD
4. Initial Applications in IBD
4.1. Prediction of Disease Course
Given the great heterogeneity, it is very likely that understanding the disease course and evolution is one of the cornerstones for developing a precision medicine approach to IBD.
An emerging area is the comprehensive evaluation of intestinal involvement in CD not only with endoscopy but utilizing imaging-based biomarkers. More specifically, one potential tool is the so-called Lemann Index (LI) which is a scoring system that combines the utilization of clinical and endoscopic figures with imaging obtained with magnetic resonance enterography (MRE). The evaluation of bowel damage already at the diagnosis might help decision making in favor of more aggressive therapy, and periodic re-evaluation might estimate the increase or reduced disease burden [9].
Another important contribution has been achieved by the pediatric cohort of the RISK study [10] which has demonstrated that combining the clinical information (age, race, disease location), antimicrobial serologies and gene signature from ileal biopsies (more specifically, an extracellular matrix signature) with a system biology methodology has been able to predict the more aggressive course of the disease such as the development of stricturing disease in 3 years of disease course.
Because of the invasiveness of the endoscopic procedure and the restriction for more frequent re-evaluation, the focus has been shifted to the utilization of blood-based biomarkers. Unfortunately, neither the investigation of DNA methylation [11] nor the genomewide association studies (GWAs) [12] have demonstrated adequate power to identify variants with an elevated odds ratio (OR) which is useful to direct patient stratification.
4.2. Prediction of Complication of Therapy
4.3. Prediction of Response to Therapy
References
- Ng, S.C.; Shi, H.Y.; Hamidi, N.; Underwood, F.E.; Tang, W.; Benchimol, E.I.; Panaccione, R.; Ghosh, S.; Wu, J.C.Y.; Chan, F.K.L.; et al. Worldwide incidence and prevalence of inflammatory bowel disease in the 21st century: A systematic review of population-based study. Lancet 2018, 390, 2769–2778.
- Torres, J.; Mehandru, S.; Colombel, J.F.; Peyrin-Biroulet, L. Crohn’s disease. Lancet 2017, 389, 1741–1755.
- Ungaro, R.; Mehandru, S.; Allen, P.B.; Peyrin-Biroulet, L.; Colombel, J.F. Ulcerative colitis. Lancet 2017, 389, 1756–1770.
- Hoff, H.E. Weir Mitchell address on instrumental precision in medicine in the perspective of 70 years. Conn. Med. 1971, 35, 640–644.
- National Research Council. Toward Precision Medicine: Building a Knowledge Network for Biomedical Research and a Next Taxonomy of Disease; National Research Council: Washington, DC, USA, 2011.
- Schleidgen, S.; Klimgler, C.; Bertram, T.; Rogowski, W.H.; Marckmann, G. What is personalized medicine: Sharpening a vague term based on a systematic literature review. BMC Med. Ethics 2013, 14, 55.
- Ideker, T.; Galitski, T.; Hood, L. A new approach to decoding life: Systems biology. Annu. Rev. Genom. Hum. Genet. 2001, 2, 343–372.
- Handelman, G.S.; Kok, H.K.; Chandra, R.V.; Razavi, A.H.; Lee, M.J.; Asadi, H. eDoctor: Machine learning and the future of the medicine. J. Intern. Med. 2018, 284, 603–619.
- Pariente, B.; Mary, J.Y.; Danese, S.; Chowers, Y.; De Cruz, P.; D’Haens, G.; Loftus, E.V., Jr.; Louis, E.; Panés, J.; Schölmerich, J.; et al. Development of Lemman score to assess digestive tract damage in patients with Crohn’s disease. Gastroenterology 2015, 148, 52–63.
- Kuhatasan, S.; Denson, L.A.; Walters, T.D.; Kim, M.O.; Marigorta, U.M.; Schirmer, M.; Mondal, K.; Liu, C.; Griffiths, A.; Noe, J.D.; et al. Prediction of complicated disease course for children newly diagnosed with Crohn’s disease: A multicenter inception cohort study. Lancet 2017, 389, 1710–1718.
- Sominemi, H.K.; Venkateswaran, S.; Kilaru, V.; Marigorta, U.M.; Mo, A.; Okou, D.T.; Kellermayer, R.; Mondal, K.; Cobb, D.; Walters, T.D.; et al. Blood-derived DNA methylation signatures of Crohn’s disease and severity of intestinal inflammation. Gastroenterology 2019, 156, 2254–2265.
- Lee, J.C.; Biasci, D.; Roberts, R.; Gearry, R.B.; Mansfield, J.C.; Ahmad, T.; Prescott, N.J.; Satsangi, J.; Wilson, D.C.; Jostins, L.; et al. UK IBD Genetic Consortium Genome wide association study identifies distinct genetic contributions to prognosis and susceptibility of Crohn’s disease. Nat. Genet. 2021, 49, 262–268.
- Coenen, M.J.; de Jong, D.J.; van Marrewijk, C.J.; Derijks, L.J.; Vermeulen, S.H.; Wong, D.R.; Klungel, O.H.; Verbeek, A.L.; Hooymans, P.M.; Peters, W.H.; et al. TOPIC recruitment team. Identification of patients with variants in TPMT and dose reduction reduces hematologic events during thiopurine treatment of inflammatory bowel disease. Gastroenterology 2015, 149, 907–917.
- Yang, S.K.; Hong, M.; Baek, J.; Choi, H.; Zhao, W.; Jung, Y.; Haritunians, T.; Ye, B.D.; Kim, K.J.; Park, S.H.; et al. A common nonsense variant in NUDT15 confers susceptibility to thiopurine-induced leukopenia. Nat. Genet. 2014, 46, 1017–1020.
- Heap, G.A.; Weedon, M.N.; Bewshea, C.M.; Singh, A.; Chen, M.; Satchwell, J.B.; Vivian, J.P.; So, K.; Dubois, P.C.; Andrews, J.M.; et al. International Serious adverse event consortium: IBD pharmacogenetics study group. GLA-DQA1-DRB1 variants confer susceptibility to pancreatitis induced by thiopurines immunosuppressants. Nat. Genet. 2014, 46, 1131–1134.
- Atreya, R.; Neumann, H.; Neufert, C.; Waldner, M.J.; Billmeier, U.; Zopf, Y.; Willma, M.; App, C.; Münster, T.; Kessler, H.; et al. In vivo imaging using fluorescent antibodies for tumor necrosis factor predict therapeutic response in Crohn’s disease. Nat. Med. 2014, 20, 33–38.
- Sokol, H.; Pigneur, B.; Watterlot, L.; Lakhdari, O.; Bermúdez-Humarán, L.G.; Gratadoux, J.J.; Blugeon, S.; Bridonneau, C.; Furet, J.P.; Corthier, G.; et al. Fecalibacterium prausnutzii is an anti-inflammatory commensal bacterium identified by the gut microbiota analysis of Crohn’s disease patients. Proc. Nat. Acad. Sci. USA 2008, 105, 16731–16736.
- Caenepeel, C.; Sadat Seyed Tabib, N.; Vieira-Silva, S.; Vermeire, S. Review article: How the intestinal microbiota may reflect disease activity and influence therapeutic outcome in inflammatory bowel disease. Aliment. Pharmacol. Ther. 2020, 52, 1453–1468.
- Barber, G.E.; Yajmir, V.; Khalili, H.; Giallourakis, C.; Garber, J.; Xavier, R.; Ananthakrishnan, A.N. Genetic marker predict primary non-response and durable response to anti-TNF biologic therapy in Crohn’s disease. Am. J. Gastroenterol. 2016, 111, 1816–1822.
- Parkes, M.; Noor, N.M.; Dowling, F.; Leung, H.; Bond, S.; Whitehead, L.; Upponi, S.; Kinnon, P.; Sandham, A.P.; Lyons, P.A.; et al. Predicting outcomes pf Crohn’s disease using a molecular biomarker : Protocol for a multicenter, randomized, biomarker-stratified trial. BMJ Open 2018, 8, e026767.
- ISRCTN Registry. The PREdiCCt Study: The prognostic effect of environmental factors in Crohn’s and colitis. BMC 2022.




