Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Eurico Madureira | -- | 2601 | 2023-10-24 19:59:31 | | | |
| 2 | Catherine Yang | Meta information modification | 2601 | 2023-10-25 02:56:10 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Madureira, E.; Aboelezz, A.; Su, W.; Roghanchi, P. Respirable Coal Mine Dust Lung Deposition. Encyclopedia. Available online: https://encyclopedia.pub/entry/50758 (accessed on 08 February 2026).
Madureira E, Aboelezz A, Su W, Roghanchi P. Respirable Coal Mine Dust Lung Deposition. Encyclopedia. Available at: https://encyclopedia.pub/entry/50758. Accessed February 08, 2026.
Madureira, Eurico, Ahmed Aboelezz, Wei-Chung Su, Pedram Roghanchi. "Respirable Coal Mine Dust Lung Deposition" Encyclopedia, https://encyclopedia.pub/entry/50758 (accessed February 08, 2026).
Madureira, E., Aboelezz, A., Su, W., & Roghanchi, P. (2023, October 24). Respirable Coal Mine Dust Lung Deposition. In Encyclopedia. https://encyclopedia.pub/entry/50758
Madureira, Eurico, et al. "Respirable Coal Mine Dust Lung Deposition." Encyclopedia. Web. 24 October, 2023.
Copy Citation
Respirable Coal Mine Dust (RCMD), with a specific focus on examining particle deposition across different regions of the airway system and lungs. The interplay of several critical factors, including particle characteristics and an individual’s breathing patterns, plays a pivotal role in determining whether particles settle in the lungs or are exhaled.
respirable coal mine dust
lung deposition
coal dust
dust exposure
respiratory diseases
1. RCMD Inhalation and Lung Deposition
The journey of inhaled dust particles through the respiratory system is crucial to understanding RCMD inhalation and lung deposition. Beginning at the nostrils or mouth, dust particles enter the respiratory airways, encountering various clearance mechanisms. These mechanisms are found in distinct areas of the respiratory system. The nasal cavity (nasopharynx, larynx, and trachea) contains small hairs and mucus that filter out the largest particles (10 to 6 µm). Moving down the respiratory tract, the tracheobronchial (TB) tree (trachea, bronchi, and smaller bronchioles) is equipped with ciliated columnar and goblet cells, which trap particles in the size range of 6 to 3 µm. Finally, in the alveoli region (smaller bronchiole balloons), alveoli macrophage cells play a pivotal role. Upon contact with dust or harmful particles, the macrophage cells engulf and transport particles to the TB region, where expulsion from the respiratory system occurs through coughing or swallowing [1][2]. Lung fluid in this region aids in respiratory processes by moisturizing inhaled air and enhancing macrophage function [3].
Furthermore, research indicates that these clearance mechanisms, particularly in the alveoli region, can be impaired by prolonged dust exposure and macrophage overload. The retention or accumulation of particles in the lungs depends on the rate of dust particle deposition within the lungs and the efficiency of macrophage clearance. The duration of dust particle exposure directly affects the rate and quantity of particle deposition in the lungs. An increase in unidentified particle deposition in the alveoli prompts the recruitment of additional macrophages to enhance the clearance process, emphasizing the importance of understanding these mechanisms for assessing RCMD inhalation and lung deposition in mining environments [4][5].
1.1. Factors Influencing Deposition
Particle physicochemical characteristics (e.g., size, shape, charge), airway physiological parameters (e.g., breathing patterns), and airway geometry collectively influence the deposition of inhaled dust particles [6][7][8].
-
Particle Size: Particle size plays a pivotal role in determining where particles deposit in the respiratory system. Particles in the respirable range (10 nm to 10 µm) tend to deposit differently in three distinct regions: the head, TB, and alveoli regions. Smaller particles (<3 µm) and nano-sized particles (<300 nm) have a higher likelihood of depositing in the alveoli region as Illustrated in Figure 1 [9].
-
Particle Shape: Particle shape affects interactions with respiratory tissue. Angular particles are more likely to deposit in the airways or lungs [14].
-
Electric Charge: Coal dust particles carry electric charge after pulverization, with this property varying by particle type. Electric charge can influence the deposition of very small particles (<4 µm) by allowing them to reach deeper respiratory zones [15].
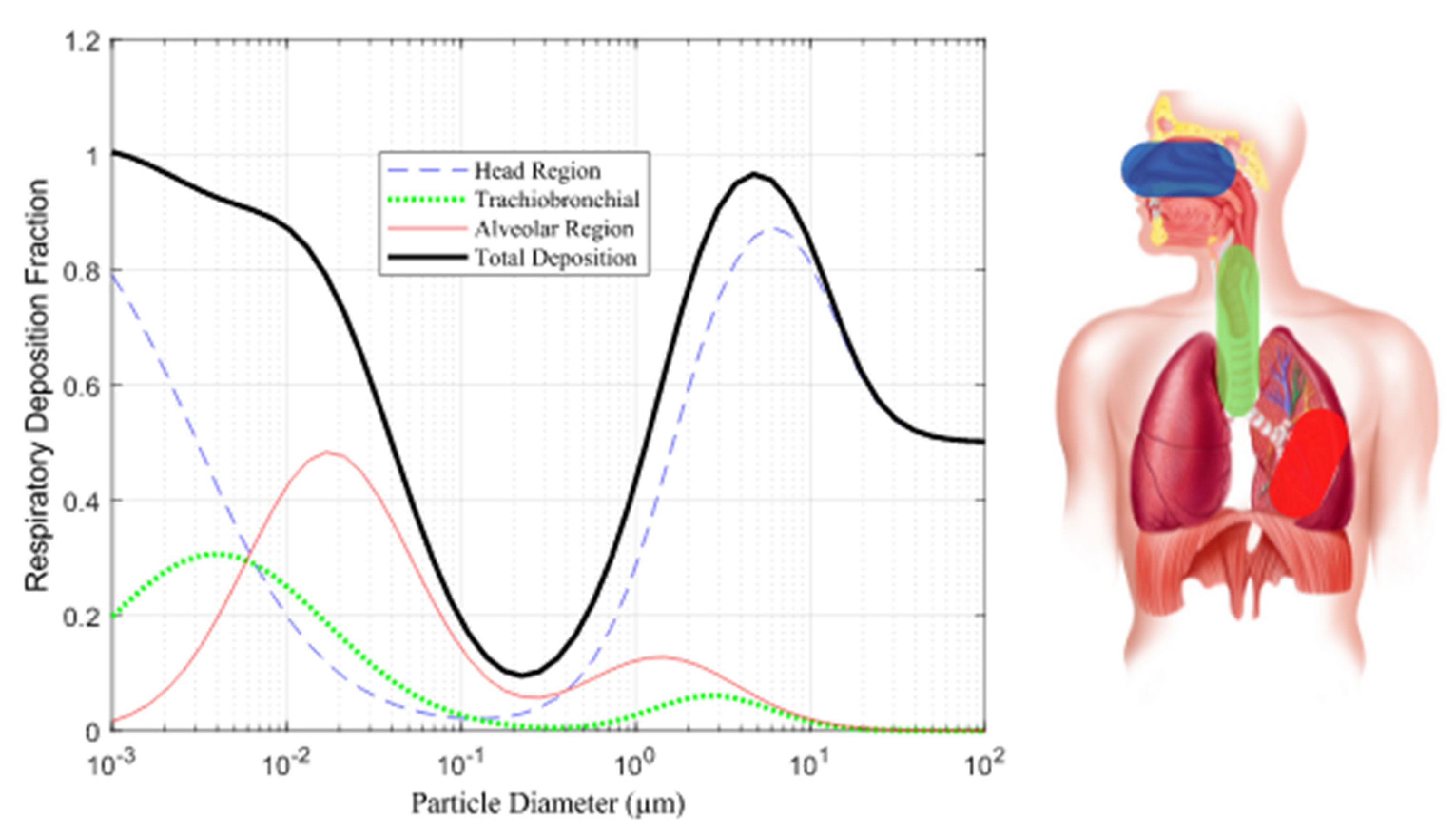
Figure 1. Prediction of deposition in the respiratory tract [15].
1.2. Deposition Mechanisms
Several mechanisms govern dust particle deposition, including inertial impaction, gravitational sedimentation, Brownian diffusion, interception, and turbulent diffusion [6][7].
This research focuses on the main mechanisms based on particle size:
-
Inertial Impaction: Particles travel at a speed that may cause them to collide with airway surfaces due to changes in airflow direction. Particle size, charge, airflow, and airway geometry influence impaction, particularly in the early respiratory system, where larger particles travel.
-
Gravitational Sedimentation: Particles gradually settle over time due to gravity, influenced by breath maneuvers, particle aerodynamic diameter, and density. Holding one’s breath increases the likelihood of sedimentation, with heavier particles settling faster.
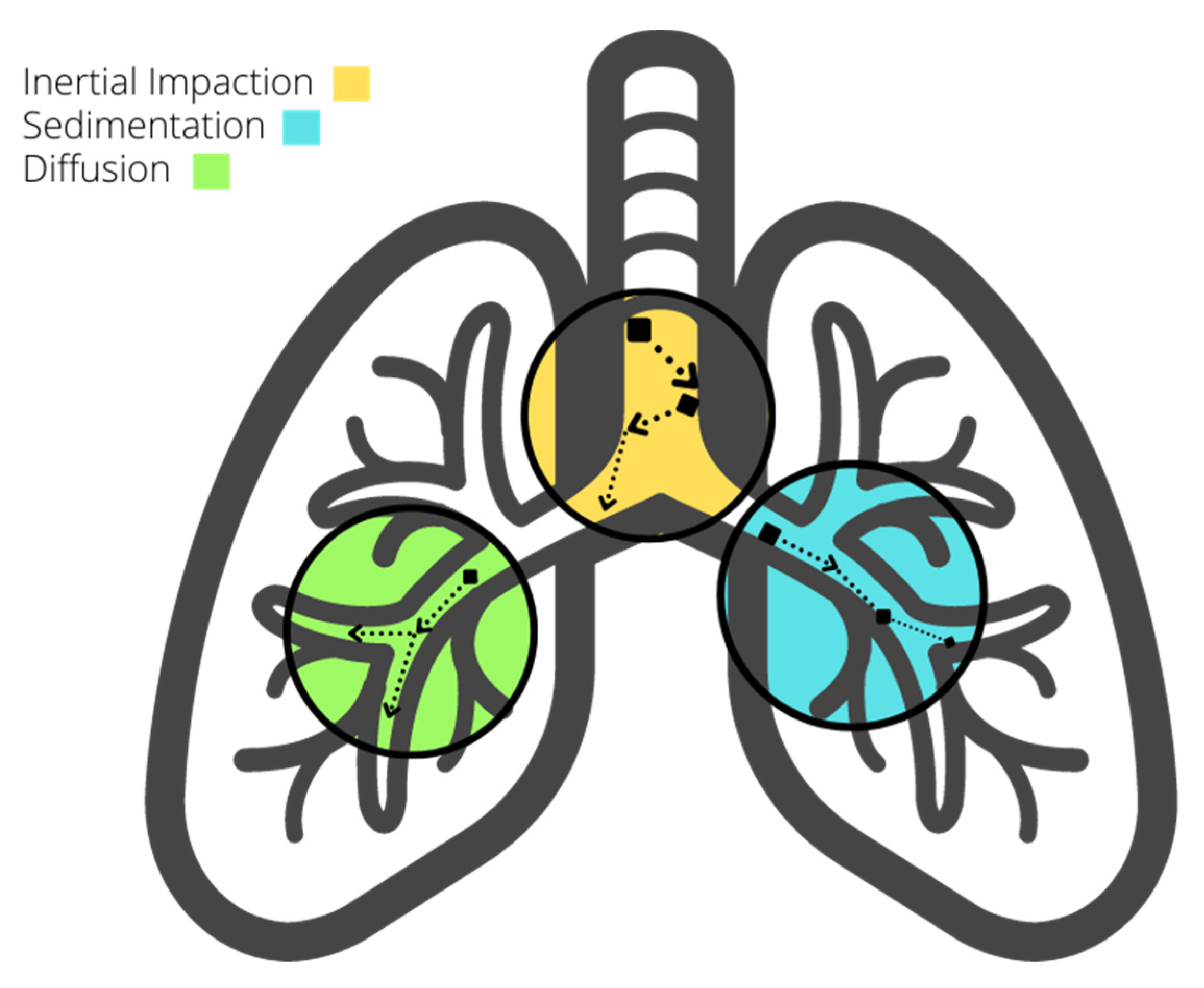
Figure 2. Deposition mechanisms in the respiratory system.
Comprehending these factors and mechanisms in conjunction with fluid dynamics enables us to discern the advantages of particle fragmentation into larger sizes, as such particles possess a greater likelihood of early settlement and extraction from the respiratory system, with the converse being true. In scenarios where fine fragmentation prevails, it necessitates the implementation of comprehensive protective measures.
2. RCMD Sources and Exposure in Coal Mines
Dust sources in mining activities stem from rock-related processes such as blasting, cutting, transportation, and rock dusting [17]. Underground coal miners face greater risks compared to surface and metal mine workers due to higher dust concentrations in confined underground environments [18]. About 3% of airborne mine dust originates from excavations [19]. From normal operation to wear and tear, mining machinery emits harmful particles with varying chemical compositions [20]. These particles can linger in the air and enter the deepest parts of the human lung or be removed by the body’s clearance mechanisms [21].
Approximately 1.7 million U.S. workers, spanning both mining and non-mining sectors, face potential exposure to hazardous dust containing crystalline silica on an annual basis [22]. Research indicates that miners may develop chronic simple silicosis after roughly 20 years of exposure, with some enduring exposure periods as long as 44 years [23][24]. Occupations characterized by high levels of risk encompass roles such as drill operators, roof bolters, and machine operators, among others. Conversely, positions like belt operators and shovel operators entail lower risks [25][26]. Notably, roof bolting alone can account for up to 50% of quartz particles in dust, with 20% falling within the respirable size range (<10 µm) [27][28]. Workers situated in intake and exhaust areas face heightened risks of inhaling fine particles compared to those stationed at the working face [29]. Nevertheless, a discernible distinction that provides enhanced protection to individuals in high-risk positions is currently lacking.
Methods for detecting coal and silica dust concentrations in mining operations encompass time-consuming laboratory techniques such as X-ray Diffraction (XRD) and Scanning Electron Microscopy with Energy Disperse X-ray (SEM-EDX). Meanwhile, field-portable devices such as the Fourier-Transform Infrared (FTIR) and Continuous Personal Dust Monitoring (CPDM) furnish essential data without necessitating laboratory assistance. In the context of both surface and underground coal mines, the responsibility for enforcing permissible exposure limits concerning coal dust and silica predominantly falls upon the mining operator, aided by contemporary monitoring devices such as the CPDM. This instrument yields estimations of dust concentrations at the conclusion of each work shift. Regrettably, it exhibits certain limitations, including bulkiness, noise emissions, and an inability to measure silica concentration [22][30][31]. This approach has demonstrated a relative inefficiency in enabling mine operators to make real-time decisions, as opposed to relying solely on end-of-shift data, while also incurring additional fatigue for the mine operator. Consequently, there is a discernible demand for more advanced equipment capable of enhancing precision. Notably, the aforementioned limitations of the CPDM have prompted research into alternative, more convenient solutions [32][33].
Continued inhalation of coal dust over time impairs respiratory tract clearance mechanisms, reducing their ability to expel particles and causing lung tissue lesions [34][35]. The International Labor Organization (ILO) classifies opacity caused by coal and silica dust inhalation into four categories (0, 1, 2, and 3) with twelve subcategories (0/1, 1/0, 1/1, etc.) [36]. Progression of pulmonary opacity is linked to higher exposure to silica dust, particularly in the mining of thin coal seams, where more host rock must be moved [23][37]. Opacity 1/0+ often advances more rapidly with exposure to quartz dust. Additionally, higher radiologic profusions are associated with ash content in low-rank coal and are influenced by both coal dust and ash content in high-rank coal [12].
3. RCMD Characterization Techniques
RCMD is typically characterized by mass concentration and mass fraction, but factors such as shape, size, and particle composition also influence its hazard potential [15]. SEM-EDX, a commonly employed laboratory technique for dust sample characterization, involves the examination of dust particle surfaces through X-ray spectra generated by the interaction between an electron beam and the particle’s surface. However, it is worth noting that, on certain occasions, there is a potential for underestimating coal particles, which may lead to an unnoticed increase in exposure to coal dust due to the mischaracterization of RCMD [38].
In a study analyzing samples collected from a low-seam mine in central Appalachia (collected at the roof bolter, belt drive, and intake location), the results indicated that particles in the roof bolter and belt drive samples were primarily composed of alumino-silicate, with a presence of carbonaceous content in the roof bolter samples. These particles can be associated with coal mineral micro-agglomerates, which, despite being coal, may not always be classified as such by SEM-EDX. This observation becomes evident when comparing SEM-EDX results with Thermographic Analysis (TGA) results, which often reveal reduced coal values and increased rock dust content. This discrepancy may occur when coal particles are coated with rock dust or Diesel Particulate Matter (DPM) [1][37].
4. Computational Fluid Dynamics in Investigating Particle Deposition
In the realm of computational fluid dynamics, numerous attempts have been made to simplify the intricate human respiratory system. These efforts involve focusing on specific respiratory system components or streamlining geometric representations. This section delves into various initiatives within this field.
Within this compiled dataset of references, spanning from 2010 to 2022, a total of 54 references were analyzed for the CFD section. Over the years, the distribution of references has been diverse, with the highest percentage (26.23%) found in 2021. The remaining years each have a percentage of references ranging from 3.28% to 9.84%, illustrating the sustained research interest in this field throughout the past decade. The following bar Chart 1 visually represents the variation in publication years and their corresponding percentages used in the article.
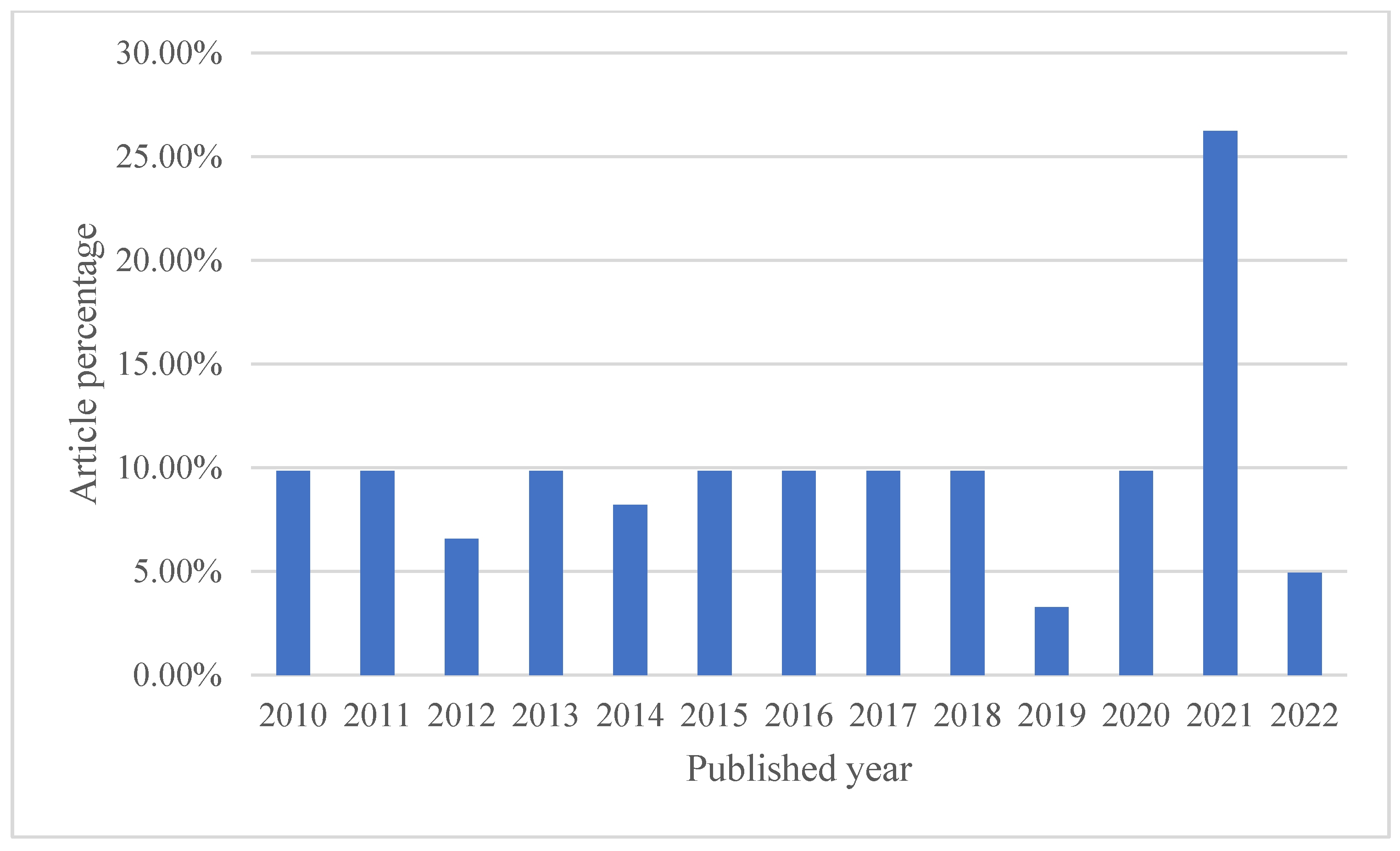
Chart 1. Articles distribution in the CFD section.
4.1. Model Geometry
The computational analysis of the complex geometry of the human lung presents considerable challenges and demands a substantial investment of time. Consequently, research in this field frequently employs varying degrees of simplification, influenced by the specific research objectives.
Basic Models: Some studies employ rudimentary models to explore the transport and deposition of microparticles and nanoparticles (1–50 nm) within the bronchial tree during inhalation [39].
Enhanced Models: In contrast, more sophisticated models, exemplified in Figure 3, are evident in various studies. These models incorporate additional airway generations and offer a more comprehensive representation of lung dynamics [40][41][42][43].
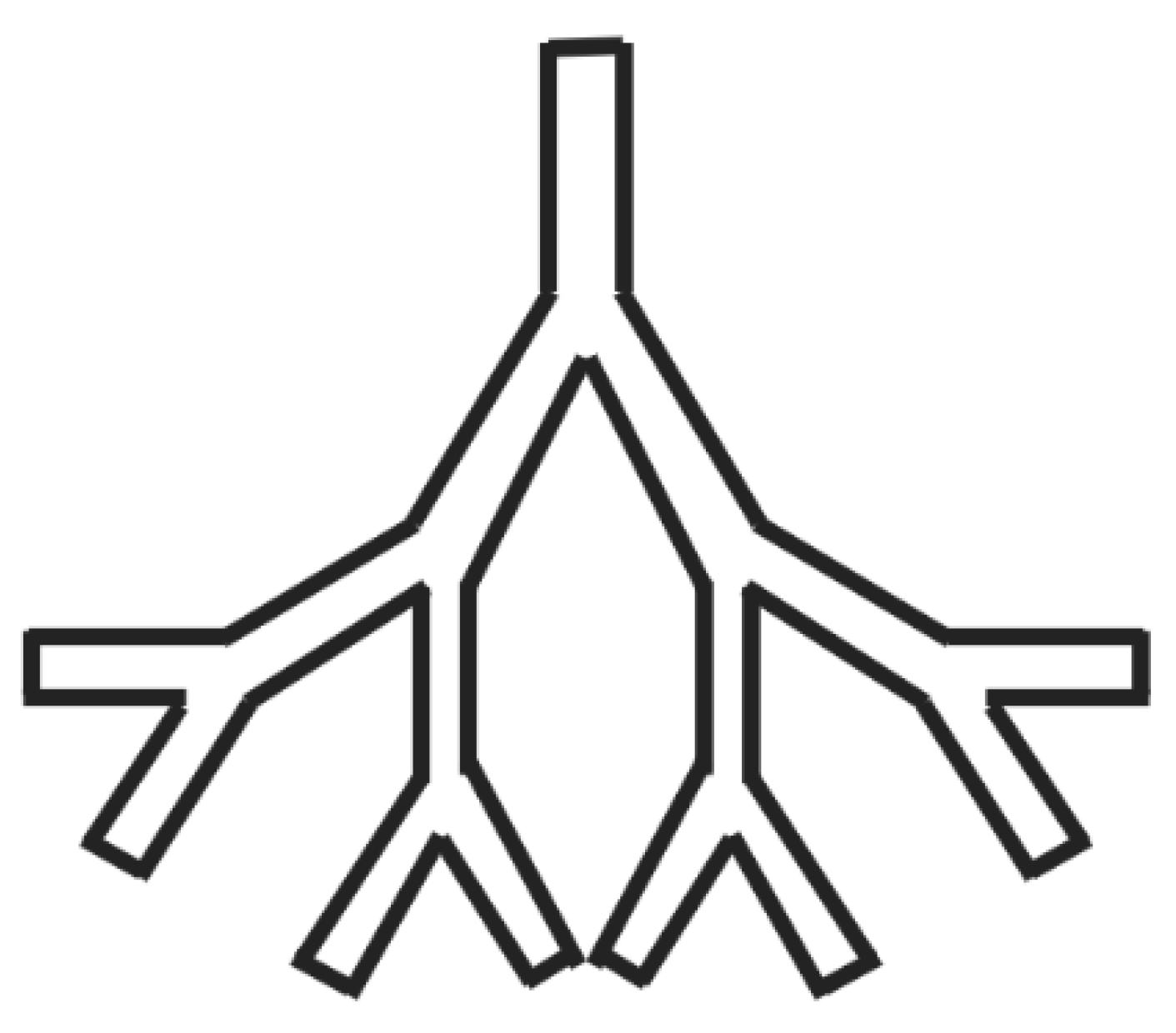
Figure 3. Schematics of an enhanced airway model.
The repercussions of these simplifications were explored and compared to actual lung models with their simplified counterparts, emphasizing the differences in material deposition [44].
Some research endeavors concentrate on specific regions within the respiratory system. For instance, certain studies examine particle deposition within the nasal airway [45][46]. Simultaneously, a distinct study delves into the ramifications of wall roughness on deposition rates within the nasal airway, as depicted in Figure 4 [47].
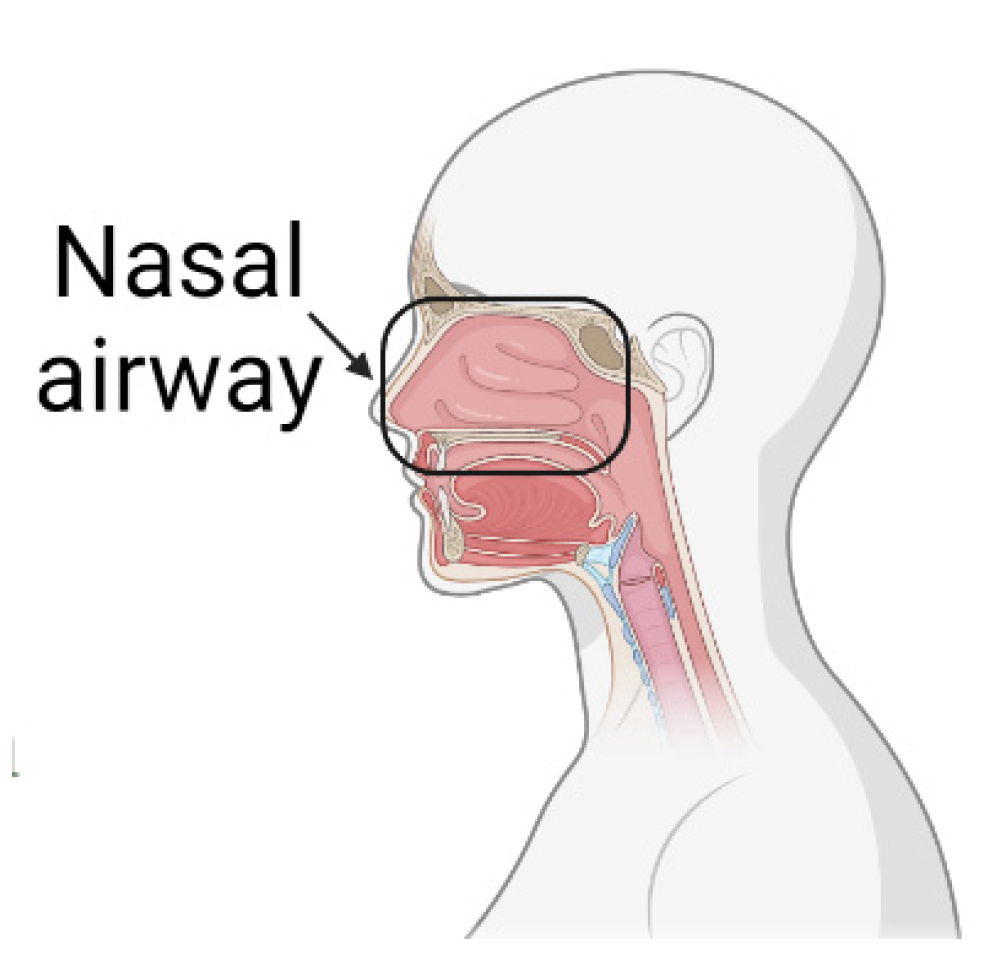
Figure 4. Nasal airway section under investigation.
To attain a comprehensive understanding of flow patterns and particle deposition, several studies expanded their modeling domain within the human upper airway system, as displayed in Figure 5 [48][49].
Mouth–Throat and Upper Tracheobronchial Models: Research focusing on regions critical for drug delivery, such as the mouth–throat (MT) and upper tracheobronchial (TB) models, is well-documented [50][51][52][53][54]. An innovative Stochastic Individual Path (SIP) modeling approach was introduced to streamline tracheobronchial research [55][56].
Patient-Specific Models: Some studies have opted for models reconstructed from actual patient scans to provide an authentic representation of the respiratory system, as illustrated in Figure 6 [57][58][59][60][61][62][63][64][65][66][67]. The complexity of these realistic models is often dictated by the requisite precision and the scope of the research. Naturally, as these models grow in detail, the computational demands and processing times correspondingly increase.
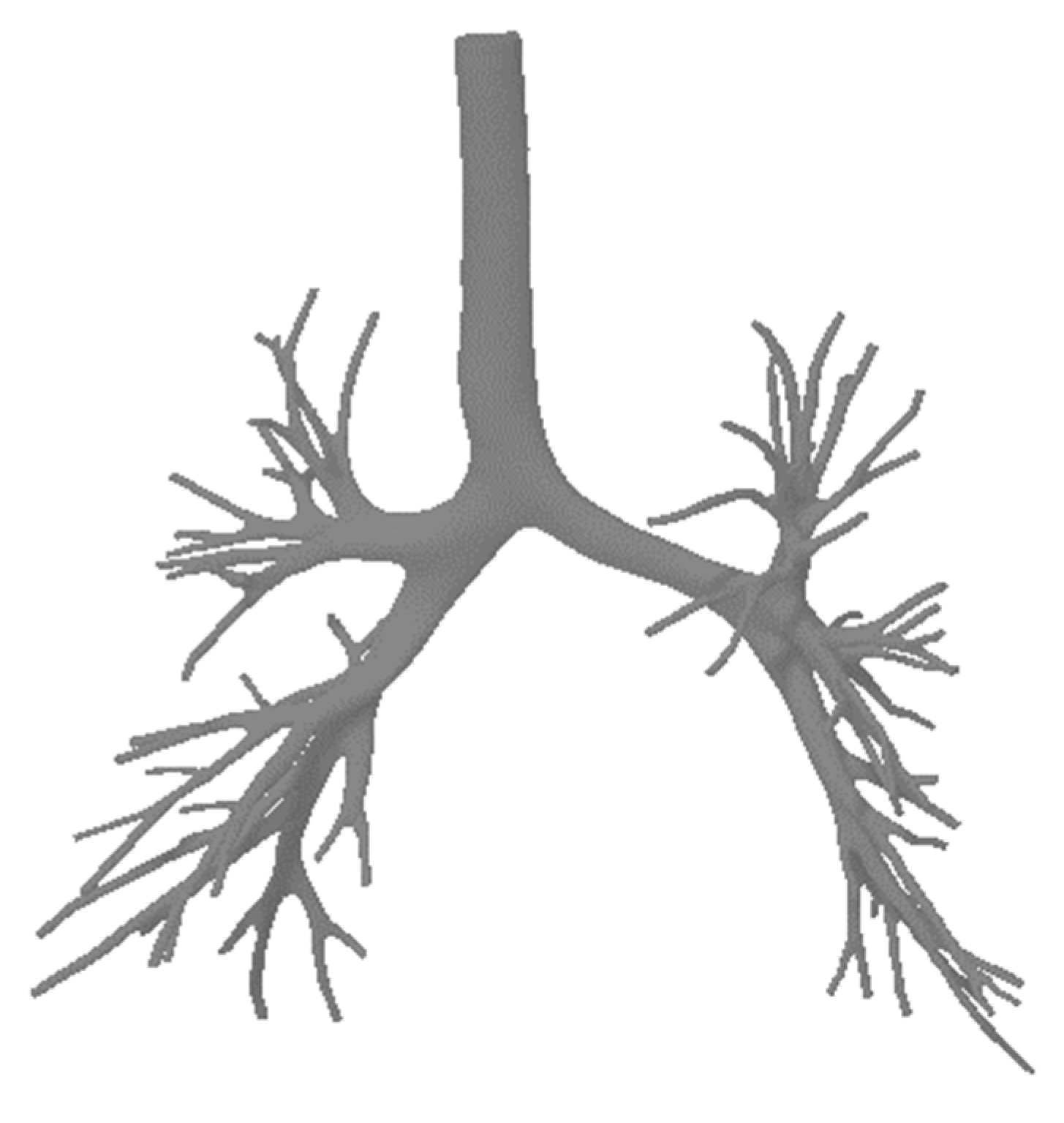
Figure 6. A realistic lung model.
4.2. Computational Analysis
When analyzing the breadth of computational methodologies utilized across different studies, the significant influence of the computational environment and boundary conditions on the accuracy of results becomes evident [40]. Delving into specifics, they harnessed fluent to solve the Navier–Stokes equations, factoring in key elements like drag and gravity that impact particle motion. Their assumptions of steady and incompressible flow resonate with the approaches taken by researchers who defined inlet conditions with a fully developed (parabolic) velocity [68]. In a similar vein, another study anchored their research on Fluent 6.3, focusing on the intricate human upper airway dynamics and incorporating the effects of Brownian motion alongside drag and gravity using the Lagrangian approach [66].
Moreover, the adoption of varied software platforms and techniques, such as Farhadi’s use of Fluent 14.0 and the Eulerian technique, contrasted with the use of ANSYS’ CFX, Version 15, by others, signifies the versatility researchers find necessary in modeling the intricate behaviors within the lungs [48][58]. Notably, one study introduced a distinctive perspective by integrating lung motion modeling into their OPENFOAM CFD simulations [69]. Concurrently, utilizing ANSYS FLUENT 15, another study cast a spotlight on particle-fluid interactions, ensuring that steady-state, incompressible Newtonian flow was aptly represented [70]. This spectrum of methodologies, culminating with the employment of the Low Reynolds Number (LRN) k turbulence model by another group, offers a profound reflection of the depth and diversity of approaches in the realm of computational analysis of the respiratory systems [71].
4.3. Difficulties of CFD Modeling
The realm of CFD modeling, especially when simulating intricate airflow patterns and pollutant dispersion in real environments, is fraught with challenges [70]. One of the primary hurdles arises from the quality and representativeness of input parameters. For instance, boundary conditions, turbulence models, and material properties play pivotal roles in ensuring the accuracy of the simulations. Yet, acquiring these with high precision remains a formidable task [40][41]. Compounding this issue, CFD simulations often resort to simplifications, either by assuming steady-state conditions or overlooking minute turbulence effects, which consequently sews seeds of uncertainty in the results [44][52][53][58][63][72]. The dynamic nature of airflow, characterized by transient behaviors like turbulent flows skirting obstacles or mutable ventilation conditions, adds another layer of complexity [42][45][48][53][62][65][66][73]. Even choices made at a technical level—such as the adoption of numerical schemes, meshing techniques, or CFD software—bear consequences on the accuracy and reliability of findings [43][46][50][51][58][60]. Nevertheless, a judicious approach to CFD modeling, which includes a meticulous evaluation of its inherent constraints and uncertainties, can act as a beacon to steer clear of biases, ultimately refining the validity of results [67].
4.4. Advantages of CFD for Particle Lung Deposition
While CFD modeling poses certain challenges, its benefits, especially in studying airflow patterns and particle dispersion within the lung, are indispensable [40]. A paramount advantage of CFD is its ability to accurately simulate intricate and evolving airflow patterns within the human respiratory system [43][56][59][69][70][72][73]. Conducting such detailed simulations through experimental methods could be either practically challenging or ethically questionable. This capability of CFD provides unparalleled insights into the trajectory and settling of pollutants within the lung’s airways [45][47][48][52][57][58].
Furthermore, CFD provides a versatile platform for researchers, allowing them to make modifications to design parameters and simulate varied scenarios, such as changes in ventilation or structural layouts [41][50][54]. This adaptability is pivotal in evaluating the efficiency of various respiratory interventions and understanding the effectiveness of diverse control measures. In a real-world context, CFD modeling is invaluable for decision-makers. It can pinpoint areas of high particle exposure, offer evaluations of different treatment strategies, and project their outcomes [5][49][53][60][62][64][65].
Collectively, these advantages underscore the immense potential of CFD in delivering a comprehensive, contextual, and practical understanding of particle deposition dynamics within the respiratory system [40][42][46][48][61][66][68].
4.5. CFD Model Validation
It is apparent that while the significance of CFD model validation is well acknowledged, the methods and metrics used for validation vary across studies [40][41][55][70].
Several papers have emphasized the importance of comparing CFD outcomes with experimental or real-world data to ascertain model accuracy [47][48][62][65][68]. For instance, some studies utilized empirical field observations to identify discrepancies in CFD predictions, ensuring rectification and refined results [49][50][59][64][71][73].
Furthermore, the implications of these validations are multifaceted. They not only enhance the credibility of research conclusions [43][44][56][61] but also solidify the basis for interpreting CFD-based findings in real-world scenarios [40][42][49][56]. The process of validation, as highlighted by several sources, aids in unmasking biases and uncertainties, ensuring a comprehensive understanding of the CFD model’s applicability and limitations [39][45][54][74].
References
- Shekarian, Y. An Investigation of the Effects of Mining Parameters on the Prevalence of Coal Worker’s Pneumoconiosis (CWP) Risks Among the US Coal Miners; New Mexico Institute of Mining and Technology: Socorro, NM, USA, 2020.
- Kuempel, E.D.; Attfield, M.D.; Vallyathan, V.; Lapp, N.L.; Hale, J.M.; Smith, R.J.; Castranova, V. Pulmonary inflammation and crystalline silica in respirable coal mine dust: Dose-response. J. Biosci. 2003, 28, 61–69.
- Carvalho, T.C.; Peters, J.I.; Williams, R.O., 3rd. Influence of particle size on regional lung deposition—What evidence is there? Int. J. Pharm. 2011, 406, 1–10.
- Kuempel, E.D.; Tran, C.L.; Smith, R.J.; Bailer, A.J. A biomathematical model of particle clearance and retention in the lungs of coal miners. II. Evaluation of variability and uncertainty. Regul. Toxicol. Pharmacol. 2001, 34, 88–101.
- Piglione, M.C.; Fontana, D.; Vanni, M. Simulation of particle deposition in human central airways. Eur. J. Mech.—B/Fluids 2012, 31, 91–101.
- Hofmann, W. Modelling inhaled particle deposition in the human lung—A review. J. Aerosol Sci. 2011, 42, 693–724.
- Rahimi, E.; Shekarian, Y.; Shekarian, N.; Roghanchi, P. Investigation of respirable coal mine dust (RCMD) and respirable crystalline silica (RCS) in the U.S. underground and surface coal mines. Sci. Rep. 2023, 13, 1767.
- Cheng, Y.S.; Su, W.-C. Deposition of Particles in Human Mouth–Throat Replicas and a USP Induction Port. J. Aerosol Med. Pulm. Drug Deliv. 2015, 28, 147–155.
- Schatzel, S.J. Identifying sources of respirable quartz and silica dust in underground coal mines in southern West Virginia, western Virginia, and eastern Kentucky. Int. J. Coal Geol. 2009, 78, 110–118.
- Sellaro, R.; Sarver, E.; Baxter, D. A Standard Characterization Methodology for Respirable Coal Mine Dust Using SEM-EDX. Resources 2015, 4, 939–957.
- Deng, Q.; Deng, L.; Miao, Y.; Guo, X.; Li, Y. Particle deposition in the human lung: Health implications of particulate matter from different sources. Environ. Res. 2019, 169, 237–245.
- Sarver, E.; Keles, C.; Rezaee, M. Beyond conventional metrics: Comprehensive characterization of respirable coal mine dust. Int. J. Coal Geol. 2019, 207, 84–95.
- Bui, V.K.H.; Moon, J.-Y.; Chae, M.; Park, D.; Lee, Y.-C. Prediction of Aerosol Deposition in the Human Respiratory Tract via Computational Models: A Review with Recent Updates. Atmosphere 2020, 11, 137.
- Xie, Y.-S.; Fan, G.-X.; Dai, J.-W.; Song, X.-B. New Respirable Dust Suppression Systems for Coal Mines. J. China Univ. Min. Technol. 2007, 17, 321–325.
- Shekarian, Y.; Rahimi, E.; Rezaee, M.; Su, W.-C.; Roghanchi, P. Respirable Coal Mine Dust: A Review of Respiratory Deposition, Regulations, and Characterization. Minerals 2021, 11, 696.
- Kodros, J.K.; Volckens, J.; Jathar, S.H.; Pierce, J.R. Ambient Particulate Matter Size Distributions Drive Regional and Global Variability in Particle Deposition in the Respiratory Tract. GeoHealth 2018, 2, 298–312.
- Stacey, P.; Thorpe, A.; Roberts, P.; Butler, O. Determination of respirable-sized crystalline silica in different ambient environments in the United Kingdom with a mobile high flow rate sampler utilising porous foams to achieve the required particle size selection. Atmos. Environ. 2018, 182, 51–57.
- Brodny, J.; Tutak, M. Exposure to Harmful Dusts on Fully Powered Longwall Coal Mines in Poland. Int. J. Environ. Res. Public Health 2018, 15, 1846.
- Trechera, P.; Querol, X.; Lah, R.; Johnson, D.; Wrana, A.; Williamson, B.; Moreno, T. Chemistry and particle size distribution of respirable coal dust in underground mines in Central Eastern Europe. Int. J. Coal Sci. Technol. 2022, 9, 3.
- Shekarian, Y.; Rahimi, E.; Shekarian, N.; Rezaee, M.; Roghanchi, P. An analysis of contributing mining factors in coal workers’ pneumoconiosis prevalence in the United States coal mines, 1986–2018. Int. J. Coal Sci. Technol. 2021, 8, 1227–1237.
- Baron, P.A.; Rice, F.L.; Key-Schwartz, R.; Bartley, D.; Schlecht, P. Health Effects of Occupational Exposure to Respirable Crystalline Silica; National Institute for Occupational Safety and Health: Cincinnati, OH, USA, 2002; Volume 145.
- Pollard, K.M. Silica, Silicosis, and Autoimmunity. Front. Immunol. 2016, 7, 97.
- Beer, C.; Kolstad, H.A.; Søndergaard, K.; Bendstrup, E.; Heederik, D.; Olsen, K.E.; Omland, Ø.; Petsonk, E.; Sigsgaard, T.; Sherson, D.L.; et al. A systematic review of occupational exposure to coal dust and the risk of interstitial lung diseases. Eur. Clin. Respir. J. 2017, 4, 1264711.
- Chekan, G.; Colinet, J.; Grau, R. Silica Dust Sources in Underground Metal/Nonmetal Mines—Two Case Studies. In Proceedings of the SME Annual Meeting, Phoenix, Arizona, 1 January 2002.
- Pandey, J.K.; Agarwal, D.; Gorain, S.; Dubey, R.K.; Vishwakarma, M.K.; Mishra, K.K.; Pal, A.K. Characterisation of respirable dust exposure of different category of workers in Jharia Coalfields. Arab. J. Geosci. 2017, 10, 183.
- Jiang, H.; Luo, Y. Development of a roof bolter drilling control process to reduce the generation of respirable dust. Int. J. Coal Sci. Technol. 2021, 8, 199–204.
- Jiang, H.; Luo, Y.; McQuerrey, J. Experimental study on effects of drilling parameters on respirable dust production during roof bolting operations. J. Occup. Environ. Hyg. 2018, 15, 143–151.
- Shangguan, Y.; Zhuang, X.; Querol, X.; Li, B.; Li, J.; Moreno, N.; Trechera, P.; Sola, P.C.; Uzu, G. Mineralogical and geochemical variations from coal to deposited dust and toxicity of size-segregated respirable dust in a blasting mining underground coal mine in Hunan Province, South China. Int. J. Coal Geol. 2021, 248, 103863.
- Ainsworth, S.M. Infrared Analysis of Respirable Coal Mine Dust for Quartz: Thirty-Five Years. J. ASTM Int. 2005, 2, 12231.
- Abbasi, B.; Wang, X.; Chow, J.C.; Watson, J.G.; Peik, B.; Nasiri, V.; Riemenschnitter, K.B.; Elahifard, M. Review of Respirable Coal Mine Dust Characterization for Mass Concentration, Size Distribution and Chemical Composition. Minerals 2021, 11, 426.
- Pan, L.; Golden, S.; Assemi, S.; Sime, M.F.; Wang, X.; Gao, Y.; Miller, J. Characterization of Particle Size and Composition of Respirable Coal Mine Dust. Minerals 2021, 11, 276.
- Miller, A.L.; Drake, P.L.; Murphy, N.C.; Cauda, E.G.; LeBouf, R.F.; Markevicius, G. Deposition Uniformity of Coal Dust on Filters and Its Effect on the Accuracy of FTIR Analyses for Silica. Aerosol Sci. Technol. 2013, 47, 724–733.
- Hajizadehmotlagh, M.; Paprotny, I. Miniaturized Wearable Respirable Dust Monitor (WEARDM) for Underground Coal Mines: Designs and Experimental Evaluation. In Proceedings of the 2019 IEEE SENSORS, Montreal, QC, Canada, 27–30 October 2019; pp. 1–4.
- Suarthana, E.; Laney, A.S.; Storey, E.; Hale, J.M.; Attfield, M.D. Coal workers’ pneumoconiosis in the United States: Regional differences 40 years after implementation of the 1969 Federal Coal Mine Health and Safety Act. Occup. Environ. Med. 2011, 68, 908–913.
- Gregoratto, D.; Bailey, M.R.; Marsh, J.W. Modelling particle retention in the alveolar-interstitial region of the human lungs. J. Radiol. Prot. 2010, 30, 491–512.
- Cohen, R.A.; Petsonk, E.L.; Rose, C.; Young, B.; Regier, M.; Najmuddin, A.; Abraham, J.L.; Churg, A.; Green, F.H.Y. Lung Pathology in U.S. Coal Workers with Rapidly Progressive Pneumoconiosis Implicates Silica and Silicates. Am. J. Respir. Crit. Care Med. 2016, 193, 673–680.
- Sarver, E.; Keleş, Ç.; Afrouz, S.G. Particle size and mineralogy distributions in respirable dust samples from 25 US underground coal mines. Int. J. Coal Geol. 2021, 247, 103851.
- Gonzalez, J.; Keles, C.; Sarver, E. On the Occurrence and Persistence of Coal-Mineral Microagglomerates in Respirable Coal Mine Dust. Min. Metall. Explor. 2022, 39, 271–282.
- Chen, X.; Zhong, W.; Zhou, X.; Jin, B.; Sun, B. CFD–DEM simulation of particle transport and deposition in pulmonary airway. Powder Technol. 2012, 228, 309–318.
- Feng, Y.; Kleinstreuer, C. Micron-particle transport, interactions and deposition in triple lung-airway bifurcations using a novel modeling approach. J. Aerosol Sci. 2014, 71, 1–15.
- Islam, M.S.; Saha, S.C.; Gemci, T.; Yang, I.A.; Sauret, E.; Ristovski, Z.; Gu, Y.T. Euler-Lagrange Prediction of Diesel-Exhaust Polydisperse Particle Transport and Deposition in Lung: Anatomy and Turbulence Effects. Sci. Rep. 2019, 9, 12423.
- Chen, X.; Feng, Y.; Zhong, W.; Sun, B.; Tao, F. Numerical investigation of particle deposition in a triple bifurcation airway due to gravitational sedimentation and inertial impaction. Powder Technol. 2018, 323, 284–293.
- Kim, Y.H.; Tong, Z.B.; Chan, H.K.; Yang, R.Y. CFD modelling of air and particle flows in different airway models. J. Aerosol Sci. 2019, 134, 14–28.
- Gao, N.; Niu, J.; He, Q.; Zhu, T.; Wu, J. Using RANS turbulence models and Lagrangian approach to predict particle deposition in turbulent channel flows. Build. Environ. 2012, 48, 206–214.
- Lambert, A.R.; O’Shaughnessy, P.; Tawhai, M.H.; Hoffman, E.A.; Lin, C.L. Regional deposition of particles in an image-based airway model: Large-eddy simulation and left-right lung ventilation asymmetry. Aerosol Sci. Technol. 2011, 45, 11–25.
- Schroeter, J.D.; Garcia, G.J.; Kimbell, J.S. Effects of Surface Smoothness on Inertial Particle Deposition in Human Nasal Models. J. Aerosol Sci. 2011, 42, 52–63.
- Xi, J.; Si, X.; Kim, J.W.; Berlinski, A. Simulation of airflow and aerosol deposition in the nasal cavity of a 5-year-old child. J. Aerosol Sci. 2011, 42, 156–173.
- Farhadi Ghalati, P.; Keshavarzian, E.; Abouali, O.; Faramarzi, A.; Tu, J.; Shakibafard, A. Numerical analysis of micro- and nano-particle deposition in a realistic human upper airway. Comput. Biol. Med. 2012, 42, 39–49.
- Hindle, M.; Longest, P.W. Evaluation of enhanced condensational growth (ECG) for controlled respiratory drug delivery in a mouth-throat and upper tracheobronchial model. Pharm. Res. 2010, 27, 1800–1811.
- Longest, P.W.; Tian, G.; Walenga, R.L.; Hindle, M. Comparing MDI and DPI aerosol deposition using in vitro experiments and a new stochastic individual path (SIP) model of the conducting airways. Pharm. Res. 2012, 29, 1670–1688.
- Zhang, Z.; Kleinstreuer, C. Laminar-to-turbulent fluid–nanoparticle dynamics simulations: Model comparisons and nanoparticle-deposition applications. Int. J. Numer. Methods Biomed. Eng. 2011, 27, 1930–1950.
- Awadalla, M.; Miyawaki, S.; Abou Alaiwa, M.H.; Adam, R.J.; Bouzek, D.C.; Michalski, A.S.; Fuld, M.K.; Reynolds, K.J.; Hoffman, E.A.; Lin, C.-L.; et al. Early Airway Structural Changes in Cystic Fibrosis Pigs as a Determinant of Particle Distribution and Deposition. Ann. Biomed. Eng. 2014, 42, 915–927.
- Koullapis, P.G.; Kassinos, S.C.; Bivolarova, M.P.; Melikov, A.K. Particle deposition in a realistic geometry of the human conducting airways: Effects of inlet velocity profile, inhalation flowrate and electrostatic charge. J. Biomech. 2016, 49, 2201–2212.
- Zhang, Z.; Kleinstreuer, C.; Hyun, S. Size-change and deposition of conventional and composite cigarette smoke particles during inhalation in a subject-specific airway model. J. Aerosol Sci. 2012, 46, 34–52.
- Longest, P.W.; Tian, G.; Khajeh-Hosseini-Dalasm, N.; Hindle, M. Validating Whole-Airway CFD Predictions of DPI Aerosol Deposition at Multiple Flow Rates. J. Aerosol Med. Pulm. Drug Deliv. 2016, 29, 461–481.
- Inthavong, K.; Choi, L.-T.; Tu, J.; Ding, S.; Thien, F. Micron particle deposition in a tracheobronchial airway model under different breathing conditions. Med. Eng. Phys. 2010, 32, 1198–1212.
- Sturm, R. Deposition and cellular interaction of cancer-inducing particles in the human respiratory tract: Theoretical approaches and experimental data. Thorac. Cancer 2010, 1, 141–152.
- Mead-Hunter, R.; King, A.J.C.; Larcombe, A.N.; Mullins, B.J. The influence of moving walls on respiratory aerosol deposition modelling. J. Aerosol Sci. 2013, 64, 48–59.
- Soni, B.; Aliabadi, S. Large-scale CFD simulations of airflow and particle deposition in lung airway. Comput. Fluids 2013, 88, 804–812.
- Kolanjiyil, A.V.; Kleinstreuer, C. Computationally efficient analysis of particle transport and deposition in a human whole-lung-airway model. Part I: Theory and model validation. Comput. Biol. Med. 2016, 79, 193–204.
- Kolanjiyil, A.V.; Kleinstreuer, C.; Sadikot, R.T. Computationally efficient analysis of particle transport and deposition in a human whole-lung-airway model. Part II: Dry powder inhaler application. Comput. Biol. Med. 2017, 84, 247–253.
- Islam, M.S.; Saha, S.C.; Sauret, E.; Gemci, T.; Yang, I.A.; Gu, Y.T. Ultrafine particle transport and deposition in a large scale 17-generation lung model. J. Biomech. 2017, 64, 16–25.
- Lintermann, A.; Schröder, W. Simulation of aerosol particle deposition in the upper human tracheobronchial tract. Eur. J. Mech.—B/Fluids 2017, 63, 73–89.
- Kadota, K.; Imanaka, A.; Shimazaki, M.; Takemiya, T.; Kubo, K.; Uchiyama, H.; Tozuka, Y. Effects of inhalation procedure on particle behavior and deposition in the airways analyzed by numerical simulation. J. Taiwan Inst. Chem. Eng. 2018, 90, 44–50.
- Poorbahrami, K.; Oakes, J.M. Regional flow and deposition variability in adult female lungs: A numerical simulation pilot study. Clin. Biomech. 2019, 66, 40–49.
- Koullapis, P.G.; Stylianou, F.S.; Sznitman, J.; Olsson, B.; Kassinos, S.C. Towards whole-lung simulations of aerosol deposition: A model of the deep lung. J. Aerosol Sci. 2020, 144, 105541.
- Chen, X.; Zhong, W.; Tom, J.; Kleinstreuer, C.; Feng, Y.; He, X. Experimental-computational study of fibrous particle transport and deposition in a bifurcating lung model. Particuology 2016, 28, 102–113.
- Garcia, G.J.; Schroeter, J.D.; Kimbell, J.S. Olfactory deposition of inhaled nanoparticles in humans. Inhal. Toxicol. 2015, 27, 394–403.
- Pourmehran, O.; Rahimi-Gorji, M.; Gorji-Bandpy, M.; Gorji, T.B. Simulation of magnetic drug targeting through tracheobronchial airways in the presence of an external non-uniform magnetic field using Lagrangian magnetic particle tracking. J. Magn. Magn. Mater. 2015, 393, 380–393.
- Tian, G.; Longest, P.W.; Su, G.; Walenga, R.L.; Hindle, M. Development of a stochastic individual path (SIP) model for predicting the tracheobronchial deposition of pharmaceutical aerosols: Effects of transient inhalation and sampling the airways. J. Aerosol Sci. 2011, 42, 781–799.
- Löndahl, J.; Möller, W.; Pagels, J.H.; Kreyling, W.G.; Swietlicki, E.; Schmid, O. Measurement techniques for respiratory tract deposition of airborne nanoparticles: A critical review. J. Aerosol Med. Pulm. Drug Deliv. 2014, 27, 229–254.
- Islam, M.S.; Saha, S.C.; Sauret, E.; Gemci, T.; Gu, Y.T. Pulmonary aerosol transport and deposition analysis in upper 17 generations of the human respiratory tract. J. Aerosol Sci. 2017, 108, 29–43.
- Kolanjiyil, A.V.; Kleinstreuer, C. Computational analysis of aerosol-dynamics in a human whole-lung airway model. J. Aerosol Sci. 2017, 114, 301–316.
- Rissler, J.; Swietlicki, E.; Bengtsson, A.; Boman, C.; Pagels, J.; Sandström, T.; Blomberg, A.; Löndahl, J. Experimental determination of deposition of diesel exhaust particles in the human respiratory tract. J. Aerosol Sci. 2012, 48, 18–33.
More
Information
Subjects:
Mineralogy
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
691
Revisions:
2 times
(View History)
Update Date:
25 Oct 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No





