Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Efterpi Michailidou | -- | 1378 | 2023-10-19 11:14:30 | | | |
| 2 | Jason Zhu | Meta information modification | 1378 | 2023-10-20 03:15:10 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Michailidou, E.; Rüegg, P.O.; Karrer, T.; Korda, A.; Weder, S.; Kompis, M.; Caversaccio, M.; Mantokoudis, G. Transmastoid Superior Semicircular Canal Plugging for SSCD. Encyclopedia. Available online: https://encyclopedia.pub/entry/50532 (accessed on 07 February 2026).
Michailidou E, Rüegg PO, Karrer T, Korda A, Weder S, Kompis M, et al. Transmastoid Superior Semicircular Canal Plugging for SSCD. Encyclopedia. Available at: https://encyclopedia.pub/entry/50532. Accessed February 07, 2026.
Michailidou, Efterpi, Pascal Oliver Rüegg, Tanya Karrer, Athanasia Korda, Stefan Weder, Martin Kompis, Marco Caversaccio, Georgios Mantokoudis. "Transmastoid Superior Semicircular Canal Plugging for SSCD" Encyclopedia, https://encyclopedia.pub/entry/50532 (accessed February 07, 2026).
Michailidou, E., Rüegg, P.O., Karrer, T., Korda, A., Weder, S., Kompis, M., Caversaccio, M., & Mantokoudis, G. (2023, October 19). Transmastoid Superior Semicircular Canal Plugging for SSCD. In Encyclopedia. https://encyclopedia.pub/entry/50532
Michailidou, Efterpi, et al. "Transmastoid Superior Semicircular Canal Plugging for SSCD." Encyclopedia. Web. 19 October, 2023.
Copy Citation
The transmastoid plugging of a superior semicircular canal is considered a safe and effective technique for the management of superior semicircular canal dehiscence (SSCD).
superior canal dehiscence syndrome
transmastoid
plugging
hearing loss
1. Introduction
Superior semicircular canal dehiscence (SSCD) was initially described in 1998 by Lloyd Minor [1][2][3]. Various techniques have been described for the treatment of this condition [4]. However, vestibular surgery always bears the risk of peri- or postoperative hearing loss due to the loss of perilymph fluid or inflammation. In addition, the traditional surgical access (middle fossa approach) requires a craniotomy and involves some retraction of the temporal lobe [5][6]. Surgery is recommended in patients experiencing disabling vestibular symptoms typically triggered by sound (Tulio phenomenon) and pressure stimuli (Hennebert sign), known as the superior canal dehiscence syndrome (SCDS).
Patients with SCDS often suffer from hearing symptoms such as conductive hyperacusis, phonophobia, autophony, audible eye movements, and pulsatile tinnitus (perceiving rhythmic noises in the ears resembling a heartbeat) [7][8][9].
The surgical repair of the dehiscence involves either plugging, resurfacing, or capping the canal using the middle cranial fossa approach [10][11]. The transmastoid approach, which is a less invasive technique than the middle cranial fossa approach, was first reported by Agrawal and Parnes in 2008 [12]. This approach can be used with both canal plugging and modified resurfacing techniques. The transmastoid approach was modified via assisted endoscopic surgery or underwater plugging techniques [13][14][15]. A balanced salt solution (BSS) might be filled up in the mastoid cavity before a canal repair. BSS has an osmolality similar to periphymph and might prevent the accidental loss of perilymph fluid due to surgical trauma of the membranous labyrinth or due to unintentional suction. The transmastoid access does not provide a direct visualization of the dehiscence over the semicircular canal [12]. Plugging the canal at the ampulated and the non-ampulated end allows for an efficient occlusion of the canal, avoiding any uncontrolled exposure of the dehiscence and manipulations on the middle fossa dura.
The assessment of a surgical complication rate is difficult considering the low prevalence of SCDS in the population (0.4 to 0.5%) and the high rate of patients being asymptomatic.
2. Search Results and Study Selection
The PRISMA flow chart in Figure 1 illustrates the search and review process. The search identified 643 unique citations, and researchers sought to examine 358 full abstracts, of which 270 were excluded at the abstract level. After initial screening, there were a total of 23 disagreements about study inclusion from the two reviewers (ME and RP, inter-rater reliability κ = 0.814). Overall disagreement on the reason for exclusion was 18%. These differences were resolved via discussion and adjudication by a third reviewer (MG).
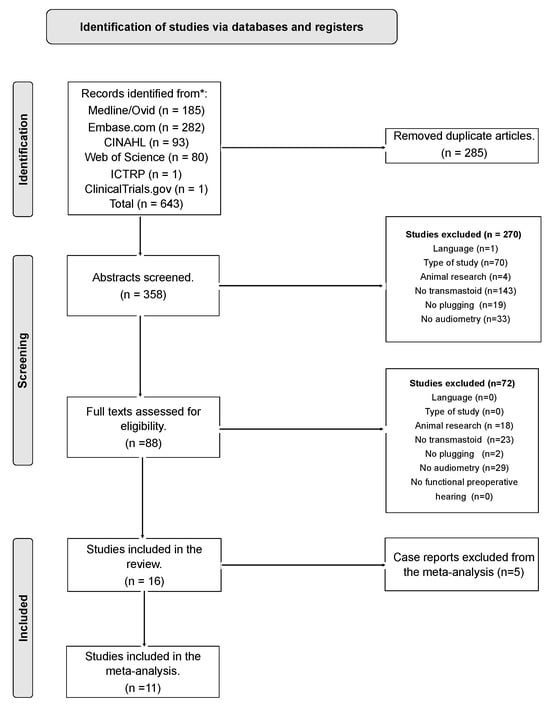
Figure 1. Prisma flow chart.
researchers performed a full-text screening on 88 manuscripts (disagreement 1.4%, inter-rater reliability κ = 0.885). researchers included 16 eligible articles (9 retrospective studies, 1 prospective study, and 6 case reports, as shown in Table 1), representing 2.3% of the total (n = 643).
Table 1. Studies included in the meta-analysis: Study type, patients’ characteristics, and hearing outcomes pre- and postoperative. Mean age is calculated in years, time of postoperative audiometry in months, frequency of thresholds in Hz, pre- and postoperative air and bone conduction thresholds in dB.
| Author, Year | Type of Study | Ears | Patients | Mean Age (SD) | Male/ Female |
Mean Follow-Up Time | Frequency (kHz) | Mean AC pre-OP (SD) |
Mean AC post-OP (SD) | Mean BC pre-OP (SD) | Mean BC post-OP (SD) | Mean ABG pre-OP (SD) | Mean ABG post-OP (SD) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ellsperman S.E. et al., 2021 [16] | Retrospective | 26 | 26 | 55 (10.2) | 8/18 | 20 | 0.5, 1, 2, 4 | 28.1 (19.6) | 26.9 (13.3) | 17.9 (16.5) | 17.4 (12.9) | 22.8 (11.1) | 18.7 (9.6) |
| Kawamura Y. et al., 2022 [15] | Retrospective | 7 | 7 | 53.3 (13.7) | 2/5 | 12.3 | 0.5, 1, 2, 4 | 20.5 (10.6) | 20.4 (7.7) | 15 (9.1) | 18.8 (9.9) | 8 (6.4) | 3 (5.3) |
| Gersdorff G. et al., 2022 [17] | Retrospective | 30 * | 27 | 52 (10.6) | 11/16 | 19 | 0.25, 0.5, 1, 2, 3, 4 | 31.85 (33.3) | 29.2 (37.1) | 14.5 (23.88) | 21.5 (25.5) | 15.6 (15.5) | 10 (11.8) |
| Lin K.F. et al., 2021 [18] | Retrospective | 29 | 29 | 51.2 (NA) | NA | 16.4 | 0.5, 1, 2, 3 | 25.6 (18.9) | 29.5 (20) | 17.5 (16) | 22.3 (18.4) | 8.1 (6.4) | 7.2 (7) |
| Nieto P. et al., 2021 [19] | Retrospective | 9 | 9 | 52.7 (10) | 3/6 | 9 | 0.5, 1, 2, 4 | 23.6 (15.7) | 26.4 (14) | 15 (13.4) | 16.9 (12.6) | NA | NA |
| Stultiens J.J.A. et al., 2022 [20] | Prospective | 4 | 4 | 51.5 (6.4) | 3/1 | 2 | 1, 2, 4 | 35 (21.8) | 38 (20.3) | 31.75 (19.6) | 33.25 (20.5) | 3.25 (2.8) | 4.75 (1.9) |
| Somers T. et al., 2014 [21] | Retrospective | 11 * | 10 | 51.5 (14.1) | 5/6 | 7.5 | 0.5, 1, 2, 4 | 31.6 (26.7) | 40.3 (25.5) | 14.8 (19.1) | 19.6 (20.6) | 23.4 (14.9) | 20 (14.9) |
| Van Haesendonck G. et al., 2016 [22] | Retrospective | 13 * | 12 | 51.5 (5.7) | 6/7 | 5.6 | 0.5, 1, 2, 4 | 24.3 (12.8) | 19.8 (9.5) | 13 (9.4) | 15.1 (7.1) | 12.9 (9.1) | 5 (4.7) |
| Deschenes G.R. et al., 2009 [23] | Retrospective | 3 * | 2 | 44.5 (5.5) | 2/1 | 3.5 | 0.5, 1, 2, 4 | 18.3 (1.1) | 10 (4.6) | 10 (0.6) | 10.4 (5.2) | 9.1 (0.6) | 13.85 (8.83) |
| Morrison M. et al., 2022 + 2 Insel cases [24] | Retrospektive | 3 | 3 | 53 | 2/1 | 2.8 | 0.5, 1, 2, 4 | 42 (7.6) | 39.1 (2.1) | 20 (3) | 27.4 (4) | 15.8 (10.9) | 12.5 (6.7) |
| Shaul C. et al., 2023 [25] | Retrospective | 24 * | 23 | 54 | 8/15 | 12 | 0.5, 1, 2 | 26.4 (16) | 26.5 (19) | 13.7 (17) | 20.5 (18) | 12.7 (8) | 5.9 (6) |
| Cocca S. et al., 2022 ** [26] | Case report | 1 | 1 | 34 | 0/1 | 2 | 0.5, 1, 2, 4 | 50 | 27.5 | 23.75 | 22.5 | 21.3 | 5 |
| Dang, P.T. et al., 2014 ** [27] | Case report | 1 | 1 | 52 | 1/0 | 9 | 0.5, 1, 2, 4 | 41.25 | 27.5 | 33.75 | 23.75 | 7.5 | 3.75 |
| Kirtane M.V. et al., 2009 ** [28] | Case report | 1 | 1 | 37 | 1/0 | 2 | 0.5, 1, 2, 4 | 31.25 | 38.75 | 6.25 | 22.5 | 12.5 | 11.3 |
| Wijaya C. et al., 2012 ** [29] | Case report | 1 | 1 | 48 | 1/0 | 6 | 0.5, 1, 2, 4 | 63.75 | 73.75 | 45 | 67.5 | 17.5 | 7.5 |
| McCall A.A. et al., 2011 ** [30] | Case report | 1 | 1 | 15 | 0/1 | 12 | 0.5, 1, 2, 4 | 5 | 2.5 | −1.25 | 0 | 6.3 | 2.5 |
| Total *** | 11 studies | 159 | 152 | 52.6 (10.2) | 50/76 | 14.1 | 25.1 (11) | 22.2 (10.5) | 15.3 (11.2) | 18.8 (12.1) | 11.5 (10.2) | 8.4 (8.6) |
researchers included 11 out of 16 publications in the meta-analysis. Five case reports were excluded from the meta-analysis due to selection bias. researchers included The own case report from Morrison et al. [24] which was part of an unbiased consecutive case series (n = 3) conducted from August 2020 to September 2022. For included studies, two independent raters (ME/RP) assessed the risk of bias or applicability concerns using QUADAS-2 tailored study criteria [31], resolving disagreements via discussion. Two studies were rated as having a high risk of bias/applicability concerns in the domain of “flow and timing”, as the postoperative audiogram was performed more than 18 months after surgery.
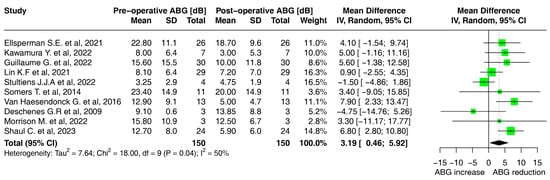
The I2 statistic, indicating the degree of heterogeneity among the included studies, was 2% for AC and 0% for BC. On the other hand, the I2 statistic for the air–bone gap was 50%, representing substantial heterogeneity in the studies [32].
3. Characteristics of Patients
Overall, 159 ears (152 patients) received a transmastoid canal plugging and were included in the study. Six patients underwent bilateral surgery, and one patient was operated on twice. The calculated mean age was 52.6 years (SD 10.2). The male/female ratio was around 0.7 (Table 1). In one study the exact male/female ratio was not available.
The mean follow-up time was 52.6 years. The average monitoring period was approximately 14 months. Out of the total, 56 patients were followed for a duration exceeding 18 months, whereas only seven ears were reported to have been within a brief time frame of just 2 months.
4. Hearing Outcomes
No cases of total hearing loss were reported after transmastoid canal plugging. However, one patient in the study of Ellsperman et al. [16] exhibited a significant sensorineural hearing loss of 30 dB eight months after the surgery.
researchers found a mean air conduction (AC) threshold at 25.1 dB PTA (SD 11) preoperatively and 22.2 dB (SD 10.5) postoperatively (Table 2). AC hearing thresholds did not significantly change after surgery (2.89 dB; 95% CI −0.05, 5.84 dB; I2 = 0%) (Figure 2A).
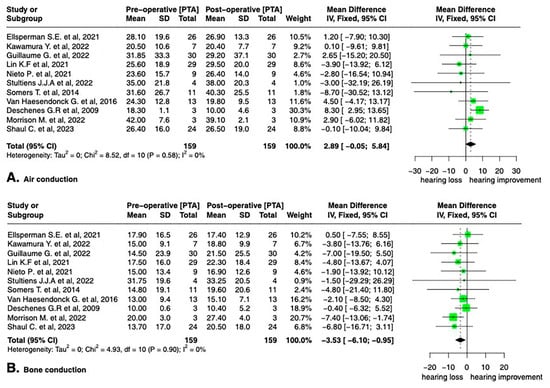
researchers found a mean bone conduction threshold at 15.3 dB PTA (SD 11.2) preoperatively and 18.8 dB (SD 12.1) postoperatively (Table 2). The mean preoperative BC threshold decreased significantly by −3.53 dB (95% CI, −6.10, −0.95 dB; I2 = 0%) from 15.8 dB (SD 17.1) to 19.9 dB (SD 17.7) (Figure 2B).
The air–bone gap before and after surgery was also studied in a subanalysis (Table 2); in one study, the air–bone gap data were not available. The mean preoperative air–bone gap was calculated to be 11.5 dB (SD 10.2) and decreased by 3.19 dB (SD 2.7) to 8.4 dB (8.6 SD) (Figure 3).
5. Clinical Symptoms before and after Surgery
Table 2 and Table 3 summarize information about the auditory and vestibular symptoms of the patients both before and after surgery. Data from the case reports were also included in these tables. Unfortunately, not all articles reported preoperative clinical symptoms and postoperative rates of symptom resolution. Autophony and tinnitus were the most reported hearing symptoms among the patients; aural fullness and hyperacusis were less frequently complained about. Following surgery, there was a significant improvement in all auditory symptoms, with an improvement rate exceeding 90% for most symptoms, except for tinnitus, which persisted in 30% of the cases. (Table 2).
Table 2. Auditory symptoms before and after surgery.
| Preoperative | Postoperative | |||||||
|---|---|---|---|---|---|---|---|---|
| Study | Aural Fullness | Autophony | Tinnitus | Hyperacusis | Aural Fullness | Autophony | Tinnitus | Hyperacusis |
| Ellsperman S.E. et al., 2021 [16] | NA | NA | NA | NA | NA | NA | NA | NA |
| Kawamura Y. et al., 2022 [15] | 4 | 6 | 2 | 5 | 0 | 0 | 0 | NA |
| Gersdorff G. et al., 2022 [17] | 19 | 29 | 18 | 9 | 1 | 1 | 7 | 0 |
| Lin K.F. et al., 2021 [18] | NA | NA | NA | NA | NA | NA | NA | NA |
| Nieto P. et al., 2021 [19] | 5 | 7 | 6 | NA | 1 | 0 | 1 | NA |
| Stultiens J.J.A. et al., 2022 [20] | NA | 4 | 4 | NA | NA | 0 | NA | NA |
| Somers T. et al., 2014 [21] | NA | 9 | 2 | 2 | NA | 0 | 2 | 0 |
| Van Haesendonck G. et al., 2016 [22] | NA | 1 | 9 | 8 | NA | 1 | 3 | 2 |
| Deschenes G.R. et al., 2009 [23] | NA | 1 | 1 | NA | NA | NA | NA | NA |
| Morrison M. et al., 2022 + 2 Insel cases [24] | 1 | 2 | 2 | 2 | 0 | 0 | 2 | 0 |
| Shaul C. et al., 2023 [25] | 9 | 18 | 16 | 4 | 1 | 1 | 3 | 1 |
| Cocca S. et al., 2022 [26] | 1 | 1 | NA | 1 | 1 | 0 | 1 | 1 |
| Dang, P.T. et al., 2014 [27] | NA | 1 | NA | NA | NA | 0 | NA | NA |
| Kirtane M.V. et al., 2009 [28] | 1 | NA | 1 | NA | 0 | NA | NA | NA |
| Wijaya C. et al., 2012 [29] | 0 | NA | 0 | NA | 0 | NA | 0 | NA |
| Total (rate of patients with remaining symptoms) | 41 | 79 | 62 | 31 | 4 (9.7%) |
3 (3.7%) |
19 (30%) |
4 (12.9%) |
Regarding vestibular symptoms and signs, the patients predominantly reported oscillopsia, and the Tullio phenomenon was frequently documented. Less frequently documented was a positive Hennebert’s sign. Postoperatively, there was a high recovery rate of symptoms, with a resolution of the Tulio sign in 90.3%, Hennebert sign in 100%, and oscillopsia in 87.5%.
References
- Ward, B.K.; van de Berg, R.; van Rompaey, V.; Bisdorff, A.; Hullar, T.E.; Welgampola, M.S.; Carey, J.P. Superior Semicircular Canal Dehiscence Syndrome: Diagnostic Criteria Consensus Document of the Committee for the Classification of Vestibular Disorders of the Bárány Society. J. Vestib. Res. Equilib. Orientat. 2021, 31, 131–141.
- Minor, L.B.; Solomon, D.; Zinreich, J.S.; Zee, D.S. Sound- and/or Pressure-Induced Vertigo Due to Bone Dehiscence of the Superior Semicircular Canal. Arch. Otolaryngol.—Head Neck Surg. 1998, 124, 249–258.
- Minor, L.B. Clinical Manifestations of Superior Semicircular Canal Dehiscence. Laryngoscope 2005, 115, 1717–1727.
- Ziylan, F.; Kinaci, A.; Beynon, A.J.; Kunst, H.P.M. A Comparison of Surgical Treatments for Superior Semicircular Canal Dehiscence: A Systematic Review. Otol. Neurotol. 2017, 38, 1–10.
- Ward, B.K.; Carey, J.P.; Minor, L.B. Superior Canal Dehiscence Syndrome: Lessons from the First 20 Years. Front. Neurol. 2017, 8, 177.
- Steenerson, K.K.; Crane, B.T.; Minor, L.B. Superior Semicircular Canal Dehiscence Syndrome. Semin. Neurol. 2020, 40, 151–159.
- Schmuziger, N.; Allum, J.; Buitrago-Téllez, C.; Probst, R. Incapacitating Hypersensitivity to One’s Own Body Sounds Due to a Dehiscence of Bone Overlying the Superior Semicircular Canal. A Case Report. Eur. Arch. Oto-Rhino-Laryngol. 2006, 263, 69–74.
- Minor, L.B.; Carey, J.P.; Cremer, P.D.; Lustig, L.R.; Streubel, S.-O.; Ruckenstein, M.J. Dehiscence of Bone Overlying the Superior Canal as a Cause of Apparent Conductive Hearing Loss. Otol. Neurotol. 2003, 24, 270–278.
- Watson, S.R.; Halmagyi, G.M.; Colebatch, J.G. Vestibular Hypersensitivity to Sound (Tullio Phenomenon). Neurology 2000, 54, 722–728.
- Vlastarakos, P.V.; Proikas, K.; Tavoulari, E.; Kikidis, D.; Maragoudakis, P.; Nikolopoulos, T.P. Efficacy Assessment and Complications of Surgical Management for Superior Semicircular Canal Dehiscence: A Meta-Analysis of Published Interventional Studies. Eur. Arch. Oto-Rhino-Laryngol. 2009, 266, 177–186.
- Mueller, S.A.; Vibert, D.; Haeusler, R.; Raabe, A.; Caversaccio, M. Surgical Capping of Superior Semicircular Canal Dehiscence. Eur. Arch. Oto-Rhino-Laryngol. 2013, 271, 1369–1374.
- Agrawal, S.K.; Parnes, L.S. Transmastoid Superior Semicircular Canal Occlusion. Otol. Neurotol. 2008, 29, 363–367.
- Yamauchi, D.; Yamazaki, M.; Ohta, J.; Kadowaki, S.; Nomura, K.; Hidaka, H.; Oshima, T.; Kawase, T.; Katori, Y. Closure Technique for Labyrinthine Fistula by ‘Underwater’ Endoscopic Ear Surgery. Laryngoscope 2014, 124, 2616–2618.
- Creighton, F.X.J.; Zhang, L.; Ward, B.; Carey, J.P. Hearing Outcomes for an Underwater Endoscopic Technique for Transmastoid Repair of Superior Semicircular Canal Dehiscence. Otol. Neurotol. 2021, 42, E1691–E1697.
- Kawamura, Y.; Yamauchi, D.; Kobayashi, T.; Ikeda, R.; Kawase, T.; Katori, Y. Hearing Outcomes of Transmastoid Plugging for Superior Canal Dehiscence Syndrome by Underwater Endoscopic Surgery: With Special Reference to Transient Bone Conduction Increase in Early Postoperative Period. Otol. Neurotol. 2022, 43, 368–375.
- Ellsperman, S.E.; Telian, S.A.; Kileny, P.R.; Welch, C.M. Auditory Outcomes Following Transmastoid and Middle Cranial Fossa Approaches for Superior Semicircular Canal Dehiscence Repair. Otol. Neurotol. 2021, 42, 1544–1552.
- Gersdorff, G.; Blaivie, C.; de Foer, B.; Deggouj, N.; Wyckmans, F.; Somers, T. Evaluation of the Transmastoid Plugging Approach for Superior Semicircular Canal Dehiscences: A Retrospective Series of 30 Ears. Eur. Arch. Oto-Rhino-Laryngol. 2022, 279, 4861–4869.
- Lin, K.F.; Bojrab, D.I.I.; Fritz, C.G.; Vandieren, A.; Babu, S.C. Hearing Outcomes After Surgical Manipulation of the Membranous Labyrinth During Superior Semicircular Canal Dehiscence Plugging or Posterior Semicircular Canal Occlusion. Otol. Neurotol. 2021, 42, 806–814.
- Nieto, P.; Gallois, Y.; Molinier, C.; Deguine, O.; Marx, M. Surgical Treatments of Superior Semicircular Canal Dehiscence: A Single-Centre Experience in 63 Cases. Laryngoscope Investig. Otolaryngol. 2021, 6, 1414–1420.
- Stultiens, J.J.A.; Guinand, N.; Van Rompaey, V.; Fornos, A.P.; Kunst, H.P.M.; Kingma, H.; van de Berg, R. The Resilience of the Inner Ear—Vestibular and Audiometric Impact of Transmastoid Semicircular Canal Plugging. J. Neurol. 2022, 269, 5229–5238.
- Zhao, Y.C.; Somers, T.; van Dinther, J.; Vanspauwen, R.; Husseman, J.; Briggs, R. Transmastoid Repair of Superior Semicircular Canal Dehiscence. J. Neurol. Surg. Part B Skull Base 2012, 73, 225–229.
- Van Haesendonck, G.; Van de Heyning, P.; Van Rompaey, V. Retrospective Cohort Study on Hearing Outcome after Transmastoid Plugging in Superior Semicircular Canal Dehiscence Syndrome: Our Experience. Clin. Otolaryngol. 2016, 41, 601–606.
- Deschenes, G.R.; Hsu, D.P.; Megerian, C.A. Outpatient Repair of Superior Semicircular Canal Dehiscence via the Transmastoid Approach. Laryngoscope 2009, 119, 1765–1769.
- Morrison, M.; Korda, A.; Wagner, F.; Caversaccio, M.D.; Mantokoudis, G. Case Report: Fremitus Nystagmus in Superior Canal Dehiscence Syndrome. Front. Neurol. 2022, 13, 844687.
- Shaul, C.; Weder, S.; Dragovic, A.; Gerard, J.-M.; Briggs, R.J.S. Trans-Mastoid Plugging of Superior Semicircular Canal Dehiscence: Long-Term Follow-Up. Eur. Arch. Oto-Rhino-Laryngol. 2023. Online ahead of print.
- Cocca, S.; Mignacco, G.; Mandalà, M.; Giannitto, C.; Esposito, A.A.; Porcino, S. A ‘Double’ Third Window Syndrome: The Case of Semicircular Canal Dehiscence in Twin Sisters. Rep. Med. Imaging 2022, 15, 1–7.
- Dang, P.T.; A Kennedy, T.; Gubbels, S.P. Simultaneous, Unilateral Plugging of Superior and Posterior Semicircular Canal Dehiscences to Treat Debilitating Hyperacusis. J. Laryngol. Otol. 2014, 128, 174–178.
- Kirtane, M.V.; Sharma, A.; Satwalekar, D. Transmastoid Repair of Superior Semicircular Canal Dehiscence. J. Laryngol. Otol. 2009, 123, 356–358.
- Wijaya, C.; Dias, A.; Conlon, B. Superior Semicircular Canal Occlusion-Transmastoid Approach. Int. J. Surg. Case Rep. 2012, 3, 42–44.
- McCall, A.A.; McKenna, M.J.; Merchant, S.N.; Curtin, H.D.; Lee, D.J. Superior Canal Dehiscence Syndrome Associated with the Superior Petrosal Sinus in Pediatric and Adult Patients. Otol. Neurotol. 2011, 32, 1312–1319.
- Whiting, P.F.; Rutjes, A.W.S.; Westwood, M.E.; Mallett, S.; Deeks, J.J.; Reitsma, J.B.; Leeflang, M.M.G.; Sterne, J.A.C.; Bossuyt, P.M.M.; QUADAS-2 Group. QUADAS-2: A Revised Tool for the Quality Assessment of Diagnostic Accuracy Studies. Ann. Intern. Med. 2011, 155, 529–536.
- Huedo-Medina, T.B.; Sánchez-Meca, J.; Marín-Martínez, F.; Botella, J. Assessing Heterogeneity in Meta-Analysis: Q Statistic or I 2 Index? Psychol. Methods 2006, 11, 193–206.
More
Information
Subjects:
Others
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
727
Revisions:
2 times
(View History)
Update Date:
20 Oct 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




