Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Leon Cong Zhi Chan | -- | 1753 | 2023-10-17 14:59:56 | | | |
| 2 | Wendy Huang | Meta information modification | 1753 | 2023-10-18 08:52:40 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Movendane, Y.; Sipalo, M.G.; Chan, L.C.Z. Folic Acid in Maternal, Perinatal, and Paediatric Health. Encyclopedia. Available online: https://encyclopedia.pub/entry/50397 (accessed on 07 February 2026).
Movendane Y, Sipalo MG, Chan LCZ. Folic Acid in Maternal, Perinatal, and Paediatric Health. Encyclopedia. Available at: https://encyclopedia.pub/entry/50397. Accessed February 07, 2026.
Movendane, Yogesh, Mbozu G. Sipalo, Leon C. Z. Chan. "Folic Acid in Maternal, Perinatal, and Paediatric Health" Encyclopedia, https://encyclopedia.pub/entry/50397 (accessed February 07, 2026).
Movendane, Y., Sipalo, M.G., & Chan, L.C.Z. (2023, October 17). Folic Acid in Maternal, Perinatal, and Paediatric Health. In Encyclopedia. https://encyclopedia.pub/entry/50397
Movendane, Yogesh, et al. "Folic Acid in Maternal, Perinatal, and Paediatric Health." Encyclopedia. Web. 17 October, 2023.
Copy Citation
Folates refer to a class of B9 vitamers with a basic structure composed of heterocyclic pteridine moiety covalently linked via a C9-N10 methylene bridge to p-aminobenzoylglutamate. Auxotrophic primates like human beings rely on exogenous dietary vitamin B9 supplementation to meet their metabolic demands. Folates play a crucial role in nucleotide synthesis and DNA methylation. Maternal folate deficiency causes several pregnancy-related complications, perinatal defects, and early childhood cognitive impairments.
folic acid
NTDs
hypertension
pre-term birth
stillbirth
spontaneous abortion
cognition
GDM
1. Introduction
Deoxyribonucleic acid (DNA), the genetic biopolymer repository synthesised and conserved within eukaryotic cells, is composed of deoxynucleotide triphosphate (dNTP) monomers. Deoxythymidine triphosphate (dTTP), a key dNTP, is synthesised by thymidylate synthase in the presence of folate derivative as cofactor. During pregnancy, the exponential increase in nucleotide biosynthesis supports rapid cell proliferation and tissue formation in the developing foetus. It creates a high metabolic demand for essential nutrients, usually quenched through maternal dietary intake or supplementation. Vitamin B9 or M (IUPAC name: (2S)-2-[[4-[(2-amino-4-oxo-3H-pteridin-6-yl)methylamino]benzoyl]amino]pentanedioic acid) is essential for nucleotide biosynthesis, DNA methylation, and amino acid homeostasis in cells [1]. Folates refer to a class of B9 vitamers with a basic structure composed of heterocyclic pteridine moiety covalently linked via a C9-N10 methylene bridge to p-aminobenzoylglutamate (Figure 1) [2]. The biological activity and bioavailability of B9 vitamers vary with oxidation state, substitutions, and the number of glutamate chains. Since humans lack the molecular machinery for de novo folate cofactor synthesis, the exogenous ingestion of natural folate polyglutamates and synthetic folic acid (FA) vitamer supplements support the nutritional demand. The ingested folate polyglutamates hydrolysed to monoglutamates, are converted to 5-methyltetrahydrofolate in the intestinal mucosa prior to entering circulation [3]. This circulated folate is then converted to 7,8-dihydrofolate (DHF) and 5,6,7,8-tetrahydrofolate (THF) by the cells to meet the metabolic demand [4][5].
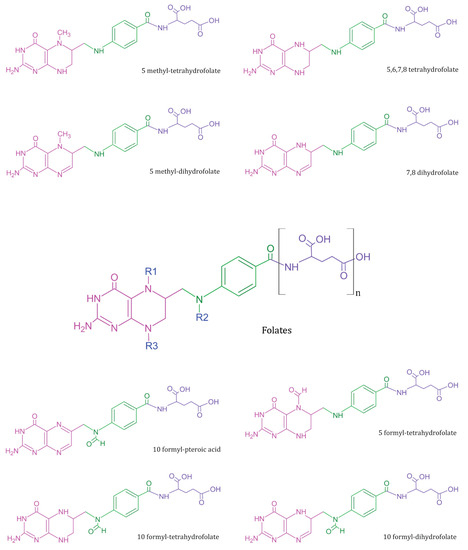
Figure 1. Summary of common folate vitamers—Folates (in centre) represent a general template structure, composed of a pteridine ring (in pink), p-aminobenzoic acid (in green), and glutamic acid moiety (in purple). Most metabolically active B9 vitamers exist in monoglutamate form and vary in structure based on R1, R2, and R3 substitutions.
The stability of B9 vitamers is reviewed elsewhere [6]. The normal range of folates is about 5–15 ng/mL in serum, 16–21 ng/mL in cerebrospinal fluid, and 175–316 ng/mL in erythrocytes [7]. To maintain the normal folate range, the daily recommended folate intake is 400 µg folate per day for adults [8]. Serum folate levels below the normal range indicate a deficiency condition. Multiple lines of evidence implicate folate deficiency in a variety of conditions during pregnancy that severely impact maternal and child health. Among such conditions, neural tube defects, pre-eclampsia, pre-term birth, stillbirth, spontaneous abortion, cognitive impairment, childhood cancers, polycystic ovary syndrome, and postpartum maternal mental health contribute substantially to the global health burden [9][10][11][12].
Among pregnant women who received at least 400 µg FA daily through fortified food and vitamin supplementations, complications such as neural tube defects dropped nearly by 50%. In women with a history of neural tube defects (high risk pregnancies), the daily dose of FA is recommended 1–3 months prior to conception [13]. Based on such well-substantiated evidence, strong folic acid fortification frameworks and policies are taking shape to tackle folate deficiency globally [14][15][16]. On the other hand, recent evidence suggests excess FA intake could also be detrimental to health [17].
Together, the danger of folate deficiency and excess highlights the need to monitor appropriate FA intake, especially during preconception and perinatal periods. At present, maternal folate levels are measured in clinical or laboratory settings. Intriguingly, an increase in stillbirth and neonatal mortality rates was observed across different countries during the COVID-19 pandemic [18][19]. This observation highlights the impact of dependency on clinical infrastructure for perinatal healthcare. Although unexpected, the need for point-of-care devices to bring quality perinatal healthcare to communities was evident during the pandemic.
Folates have been implicated in maternal and perinatal health for at least three decades. The role of various folates in metabolic homeostasis are summarised elsewhere [20][21][22]. In the following section, the focus is on the associations between maternal folate deficiency and different perinatal complications.
2. Neural Tube Defects
The World Health Organization (WHO) reports an annual global estimate of 240,000 neonatal deaths within the first 28 days due to congenital disorders as of 2023. Neural tube defects (NTDs) occurring in weeks 3 or 4 of pregnancy are among the most common and extremely severe but preventable congenital disorders [23]. Anencephaly, the most fatal of NTDs, is a congenital brain malformation, where the anterior (cranial) neural arch fails to close during embryo development. This condition invariably results in stillbirth or neonatal mortality [11][24].
While anencephaly occurs early in embryogenesis, the same malformation occurring late in embryogenesis results in encephalocele. Typical brain-tissue protrusion through the skull, mostly in the occipital region, is a characteristic of encephalocele. It is relatively rare compared to anencephaly, yet presents a high mortality risk [25]. Another common NTD, spina bifida (SB), is a congenital spinal cord malformation, wherein the posterior (caudal) vertebral arch fails to close, resulting in meningocele, myelomeningocele, and/or hydrocephalus [11][26]. In the case of SB, though the mortality rate is relatively lower than anencephaly, the patients are likely to experience neurological disabilities.
Within the proposed multifactorial aetiology of NTDs, nutritional deficiency arguably is the most easily preventable factor [27][28]. FA supplements and fortification were reported to reduce NTDs related to neonatal mortality [11][28][29][30]. In particular, two exemplary large-population, data-based analyses concluded periconceptual maternal FA intake prevents NTD occurrences [31][32]. Another meta-analysis of NTDs in eastern Africa also suggests that mandatory FA supplements could reduce the risk of NTDs [33]. Fascinatingly, an 11-year follow-up study by Caffrey et al. shows that continued FA supplementation post the timeframe recommended to prevent NTDs supports neurocognitive development in the baby [34].
3. Hypertensive Disorders
Pregnancy-induced hypertension (PIH) reduces nutrition and oxygen supply to the foetus. PIH includes chronic hypertension, pre-eclampsia (PE), superimposed pre-eclampsia, and gestational hypertension [35]. PE clinically manifests as hypertension and proteinuria occurring post-week 20 of gestation [36]. The aetiology of PE remains largely unknown. Moreover, unlike other pregnancy-related complications, PE is detrimental to both maternal and foetal health [37]. Strikingly, a key observation in PE and gestational hypertension is elevated levels of homocysteine in blood [12]. It is well-established that FA supplements mitigate the risk posed by elevated homocysteine levels [38].
Not surprisingly, controversial evidence for nutritional supplementation in reducing PE risk does exist [39][40]. Yet, the overwhelming amount of evidence highlights FA supplementation as a protective factor against PE [12][36][41][42][43][44].
4. Pre-Term Birth
The WHO estimated around 13.4 million pre-term births (PTB) in 2020, which is a leading cause of neonatal mortality. For human beings, 40 weeks marks the normal gestation period. Any spontaneous pre-term labour between the 28th and 37th week of gestation is termed PTB [45]. The complications associated with PTB are diverse and include cerebral palsy, hypothermia, hypoglycaemia, brain injury, and cognitive impairment [46]. Tackling PTB is unquestionably a global priority. In May 2023, the United Nations International Children’s Emergency Fund (UNICEF) published an updated report on PTB, titled “Born Too Soon: Decade of action on preterm birth”. This report found that preterm births have not changed significantly in any region of the world in the past decade. Southern Asia and Sub-Saharan Africa account for more than 65% of preterm births recorded globally. In Singapore, nearly 9% of pregnancies end in PTB, and the trend is expected to increase in the near future [47].
Furthermore, this report proposes an action plan and identifies intersectoral risk factors influencing PTB, among which maternal nutrition is of high significance. Notably, a retrospective cohort study including 200,000 women observed a reduced PTB risk with FA supplementation [46]. Another case-controlled study reported low maternal serum folate levels in PTB cases [45].
A recent meta-analysis of epidemiological studies correlating PTB risk and maternal folate levels also conclusively states that PTB risk reduces with higher maternal folate levels [48]. Lastly, an observational study observing the high maternal folate level association with low PTB risk even proposed possible maternal folate level optimisation in the post-fortification era [49].
5. Stillbirth and Spontaneous Abortion
In 2014, 194 countries endorsed the “Every Newborn Action Plan (ENAP)” developed by the WHO. The ENAP sets a global target to achieve less than 12 stillbirths per 1000 total births in all 194 countries by 2030. Stillbirth is the loss of the foetus post week 20 of gestation. Approximately 1.9 million babies, or one every 16 s were born stillborn in 2021. The major causes of stillbirths include placental malperfusion, foetal asphyxia, congenital malformations, infection, PTB, PE, and umbilical cord complications [50][51][52]. Spontaneous abortion (SA) refers to the loss of a foetus prior to week 20 of gestation [53]. Several factors such as chromosomal abnormalities, nutritional deficiency, immunogenic factors, DNA fragmentations, lifestyle choices, and other factors could result in SA [53][54]. In accordance with such findings, studies suggest periconceptional FA supplementation reduces the risk of SA and stillbirths [55][56][57][58][59].
6. Early Childhood Cognition
Cognition, occasionally dubbed the ultimate brain function, develops extensively during early childhood. Based on accumulating evidence highlighting the role of periconceptional FA supplementation in foetal neurodevelopment, studies hypothesised its influence on cognition and motor abilities. Fascinatingly, a study of children aged 4–5 years reported that low maternal FA levels resulted in attentional dysfunction preferentially among boys [60]. A longitudinal study of children aged 7–9 years, from the same group, reported that low maternal FA results in low alertness irrespective of gender.
Interestingly, they also observed comparatively better cognitive and working memory among girls [61]. Another study conducted in Japan reports a higher cognitive, language, and social development quotient among 4-years-olds whose mothers began FA supplementation before week 12 of gestation [8]. Although such strong correlations are well-substantiated, certain previous studies providing insignificant correlations do exist [62]. This might be due to several postnatal factors influencing infant development through early childhood.
7. Genomic and Epigenomic Instability
Most intriguingly, the latest sets of evidence hint at the need to study the optimal threshold for FA intake. As summarised above, low FA intake results in adverse pregnancy outcomes. On the other hand, excess FA supplement consumption could induce genomic and epigenomic instability [63][64]. Although further studies on the human population is essential to estimate the true impact of high and low FA intake, it is highly likely that excess FA intake could also result in unfavourable outcomes.
8. Gestational Diabetes Mellitus
Among different pregnancy-related complications, the most common metabolomic disorder is gestational diabetes mellitus (GDM) [65]. GDM refers to glucose intolerance occurring in early pregnancy and is estimated to affect 30% of pregnancies globally [66]. In Singapore, GDM is the most prevalent metabolomic pregnancy-related disorder, observed in roughly 25% of pregnancies. Several studies have reported a strong association between GDM and high FA with vitamin B12 insufficiency [67][68][69]. Although the aetiology of GDM remains elusive, current observations consistently report the imbalance in FA and vitamin B12 concentrations, postulating a potential role for surplus FA in GDM.
References
- Barua, S.; Kuizon, S.; Junaid, M.A. Folic acid supplementation in pregnancy and implications in health and disease. J. Biomed. Sci. 2014, 21, 77.
- Ducker, G.S.; Rabinowitz, J.D. One-Carbon Metabolism in Health and Disease. Cell Metab. 2017, 25, 27–42.
- Agata, S.M. Methods for assessment of folate (vitamin B9). In Laboratory Assessment of Vitamin Status; Elsevier: Amsterdam, The Netherlands, 2018; pp. 219–264.
- Matherly, L.H. Molecular and cellular biology of the human reduced folate carrier. Prog. Nucleic Acid. Res. Mol. Biol. 2001, 67, 131–162.
- Zhao, R.; Matherly, L.H.; Goldman, I.D. Membrane transporters and folate homeostasis: Intestinal absorption and transport into systemic compartments and tissues. Expert Rev. Mol. Med. 2009, 11, e4.
- Gazzali, A.M.; Lobry, M.; Colombeau, L.; Acherar, S.; Azaïs, H.; Mordon, S.; Arnoux, P.; Baros, F.; Vanderesse, R.; Frochot, C. Stability of folic acid under several parameters. Eur. J. Pharm. Sci. 2016, 93, 419–430.
- Batra, B.; Narwal, V.; Kalra, V.; Sharma, M.; Rana, J.S. Folic acid biosensors: A review. Process Biochem. 2020, 92, 343–354.
- Nishigori, H.; Nishigori, T.; Obara, T.; Suzuki, T.; Mori, M.; Imaizumi, K.; Murata, T.; Kyozuka, H.; Ogata, Y.; Sato, A.; et al. Prenatal folic acid supplement/dietary folate and cognitive development in 4-year-old offspring from the Japan Environment and Children’s Study. Sci. Rep. 2023, 13, 9541.
- Nguyen, P.H.; DiGirolamo, A.M.; Gonzalez-Casanova, I.; Pham, H.; Hao, W.; Nguyen, H.; Truong, T.V.; Nguyen, S.; Harding, K.B.; Reinhart, G.A.; et al. Impact of preconceptional micronutrient supplementation on maternal mental health during pregnancy and postpartum: Results from a randomized controlled trial in Vietnam. BMC Womens Health 2017, 17, 44.
- Mortensen, J.H.S.; Øyen, N.; Fomina, T.; Melbye, M.; Tretli, S.; Vollset, S.E.; Bjørge, T. Supplemental folic acid in pregnancy and childhood cancer risk. Br. J. Cancer 2016, 114, 71–75.
- Blencowe, H.; Cousens, S.; Modell, B.; Lawn, J. Folic acid to reduce neonatal mortality from neural tube disorders. Int. J. Epidemiol. 2010, 39, i110–i121.
- Liu, C.; Liu, C.; Wang, Q.; Zhang, Z. Supplementation of folic acid in pregnancy and the risk of preeclampsia and gestational hypertension: A meta-analysis. Arch. Gynecol. Obstet. 2018, 298, 697–704.
- Argyridis, S. Folic acid in pregnancy. Obstet. Gynaecol. Reprod. Med. 2019, 29, 118–120.
- Wald, N.J.; Morris, J.K.; Blakemore, C. Public health failure in the prevention of neural tube defects: Time to abandon the tolerable upper intake level of folate. Public Health Rev. 2018, 39, 2.
- Kancherla, V.; Botto, L.D.; Rowe, L.A.; Shlobin, N.A.; Caceres, A.; Arynchyna-Smith, A.; Zimmerman, K.; Blount, J.; Kibruyisfaw, Z.; Ghotme, K.A.; et al. Preventing birth defects, saving lives, and promoting health equity: An urgent call to action for universal mandatory food fortification with folic acid. Lancet Glob. Health 2022, 10, e1053–e1057.
- Smith, A.D.; Sobczyńska-Malefora, A.; Green, R.; Reynolds, E.H.; Refsum, H. Mandatory food fortification with folic acid. Lancet Glob. Health 2022, 10, e1389.
- Patel, K.R.; Sobczyńska-Malefora, A. The adverse effects of an excessive folic acid intake. Eur. J. Clin. Nutr. 2017, 71, 159–163.
- Calvert, C.; Brockway, M.; Zoega, H.; Miller, J.E.; Been, J.V.; Amegah, A.K.; Racine-Poon, A.; Oskoui, S.E.; Abok, I.I.; Aghaeepour, N.; et al. Changes in preterm birth and stillbirth during COVID-19 lockdowns in 26 countries. Nat. Hum. Behav. 2023, 7, 529–544.
- Vaccaro, C.; Mahmoud, F.; Aboulatta, L.; Aloud, B.; Eltonsy, S. The impact of COVID-19 first wave national lockdowns on perinatal outcomes: A rapid review and meta-analysis. BMC Pregnancy Childbirth 2021, 21, 676.
- Zheng, Y.; Cantley, L.C. Toward a better understanding of folate metabolism in health and disease. J. Exp. Med. 2019, 216, 253–266.
- Franco, C.N.; Seabrook, L.J.; Nguyen, S.T.; Leonard, J.T.; Albrecht, L.V. Simplifying the B Complex: How Vitamins B6 and B9 Modulate One Carbon Metabolism in Cancer and Beyond. Metabolites 2022, 12, 961.
- Virdi, S.; Jadavji, N.M. The Impact of Maternal Folates on Brain Development and Function after Birth. Metabolites 2022, 12, 876.
- Blencowe, H.; Kancherla, V.; Moorthie, S.; Darlison, M.W.; Modell, B. Estimates of global and regional prevalence of neural tube defects for 2015: A systematic analysis. Ann. N. Y. Acad. Sci. 2018, 1414, 31–46.
- Salari, N.; Fatahi, B.; Fatahian, R.; Mohammadi, P.; Rahmani, A.; Darvishi, N.; Keivan, M.; Shohaimi, S.; Mohammadi, M. Global prevalence of congenital anencephaly: A comprehensive systematic review and meta-analysis. Reprod. Health 2022, 19, 201.
- Toriello, H.V. Policy statement on folic acid and neural tube defects. Genet. Med. 2011, 13, 593–596.
- Pattisapu, J.V.; Veerappan, V.R.; White, C.; Vijayasekhar, M.V.; Tesfaye, N.; Rao, B.H.; Park, K.B. Spina bifida management in low- and middle-income countries—A comprehensive policy approach. Child’s Nerv. Syst. 2023, 39, 1821–1829.
- Lacasañ, M.; Blanco-Muñoz, J.; Borja-Aburto, V.H.; Aguilar-Garduño, C.; Rodríaguez-Barranco, M.; Sierra-Ramirez, J.A.; Galaviz-Hernandez, C.; Gonzalez-Alzaga, B.; Garcia-Cavazos, R. Effect on risk of anencephaly of gene-nutrient interactions between methylenetetrahydrofolate reductase C677T polymorphism and maternal folate, vitamin B12 and homocysteine profile. Public Health Nutr. 2012, 15, 1419–1428.
- Ho, P.; Quigley, M.A.; Tatwavedi, D.; Britto, C.; Kurinczuk, J.J. Neonatal and infant mortality associated with spina bifida: A systematic review and meta-analysis. PLoS ONE 2021, 16, e0250098.
- Viswanathan, M.; Treiman, K.A.; Kish-Doto, J.; Middleton, J.C.; Coker-Schwimmer, E.J.L.; Nicholson, W.K. Folic acid supplementation for the prevention of neural tube defects an updated evidence report and systematic review for the US preventive services task force. JAMA—J. Am. Med. Assoc. 2017, 317, 190–203.
- Atta, C.A.M.; Fiest, K.M.; Frolkis, A.D.; Jette, N.; Pringsheim, T.; St Germaine-Smith, C.; Rajapakse, T.; Kaplan, G.G.; Metcalfe, A. Global birth prevalence of spina bifida by folic acid fortification status: A systematic review and meta-analysis. Am. J. Public Health 2016, 106, e24–e34.
- Madrid, L.; Vyas, K.J.; Kancherla, V.; Leulseged, H.; Suchdev, P.S.; Bassat, Q.; Sow, S.O.; El Arifeen, S.; Madhi, S.A.; Onyango, D.; et al. Neural tube defects as a cause of death among stillbirths, infants, and children younger than 5 years in sub-Saharan Africa and southeast Asia: An analysis of the CHAMPS network. Lancet Glob. Health 2023, 11, e1041–e1052.
- Liu, J.; Li, Z.; Ye, R.; Liu, J.; Ren, A. Periconceptional folic acid supplementation and sex difference in prevention of neural tube defects and their subtypes in China: Results from a large prospective cohort study. Nutr. J. 2018, 17, 115.
- Ssentongo, P.; Heilbrunn, E.S.; Ssentongo, A.E.; Ssenyonga, L.V.N.; Lekoubou, A. Birth prevalence of neural tube defects in eastern Africa: A systematic review and meta-analysis. BMC Neurol. 2022, 22, 115.
- Caffrey, A.; McNulty, H.; Rollins, M.; Prasad, G.; Gaur, P.; Talcott, J.B.; Witton, C.; Cassidy, T.; Marshall, B.; Dornan, J.; et al. Effects of maternal folic acid supplementation during the second and third trimesters of pregnancy on neurocognitive development in the child: An 11-year follow-up from a randomised controlled trial. BMC Med. 2021, 19, 73.
- Metoki, H.; Iwama, N.; Hamada, H.; Satoh, M.; Murakami, T.; Ishikuro, M.; Obara, T. Hypertensive disorders of pregnancy: Definition, management, and out-of-office blood pressure measurement. Hypertens. Res. 2022, 45, 1298–1309.
- Serrano, N.C.; Quintero-Lesmes, D.C.; Becerra-Bayona, S.; Guio, E.; Beltran, M.; Paez, M.C.; Ortiz, R.; Saldarriaga, W.; Diaz, L.A.; Monterrosa, Á.; et al. Association of pre-eclampsia risk with maternal levels of folate, homocysteine and vitamin B12 in Colombia: A case-control study. PLoS ONE 2018, 13, e0208137.
- Wen, S.W.; White, R.R.; Rybak, N.; Gaudet, L.M.; Robson, S.; Hague, W.; Simms-Stewart, D.; Carroli, G.; Smith, G.; Fraser, W.D.; et al. Effect of high dose folic acid supplementation in pregnancy on pre-eclampsia (FACT): Double blind, phase III, randomised controlled, international, multicentre trial. BMJ 2018, 362, k3478.
- Kaye, A.D.; Jeha, G.M.; Pham, A.D.; Fuller, M.C.; Lerner, Z.I.; Sibley, G.T.; Cornett, E.M.; Urits, I.; Viswanath, O.; Kevil, C.G. Folic Acid Supplementation in Patients with Elevated Homocysteine Levels. Adv. Ther. 2020, 37, 4149–4164.
- Slomski, A. High-Dose Folic Acid Does Not Prevent Preeclampsia. JAMA 2018, 320, 2068.
- Asres, A.W.; Samuel, S.; Daga, W.B.; Tena, A.; Alemu, A.; Workie, S.B.; Alemayehu, M.; Messel, H. Association between iron-folic acid supplementation and pregnancy-induced hypertension among pregnant women in public hospitals, Wolaita Sodo, Ethiopia 2021: A case-control study. BMC Public Health 2023, 23, 843.
- Rahat, B.; Hamid, A.; Bagga, R.; Kaur, J. Folic Acid Levels During Pregnancy Regulate Trophoblast Invasive Behavior and the Possible Development of Preeclampsia. Front. Nutr. 2022, 9, 847136.
- De Ocampo, M.P.G.; Araneta, M.R.G.; Macera, C.A.; Alcaraz, J.E.; Moore, T.R.; Chambers, C.D. Folic acid supplement use and the risk of gestational hypertension and preeclampsia. Women Birth 2018, 31, e77–e83.
- Agrawal, S.; Fledderjohann, J.; Vellakkal, S.; Stuckler, D. Adequately diversified dietary intake and iron and folic acid supplementation during pregnancy is associated with reduced occurrence of symptoms suggestive of pre-eclampsia or eclampsia in indian women. PLoS ONE 2015, 10, e0119120.
- Kaldygulova, L.; Ukybassova, T.; Aimagambetova, G.; Gaiday, A.; Tussupkaliyev, A. Biological Role of Folic Acid in Pregnancy and Possible Therapeutic Application for the Prevention of Preeclampsia. Biomedicines 2023, 11, 272.
- Sharif, M.E.; Mohamedain, A.; Ahmed, A.A.; Nasr, A.M.; Adam, I. Folic acid level and preterm birth among Sudanese women. Matern. Health Neonatol. Perinatol. 2017, 3, 25.
- Wu, Y.; Yuan, Y.; Kong, C.; Ma, Q.; Ye, H.; Jing, W.; Liu, J.; Liu, M. The association between periconceptional folic acid supplementation and the risk of preterm birth: A population-based retrospective cohort study of 200,000 women in China. Eur. J. Nutr. 2021, 60, 2181–2192.
- Gosavi, A.; Amin, Z.; David Carter, S.; Choolani, M.; Fee, E.; Milad, M.; Jobe, A. Antenatal corticosteroids in Singapore: A clinical and scientific assessment. Singap. Med. J. 2023.
- Li, B.; Zhang, X.; Peng, X.; Zhang, S.; Wang, X.; Zhu, C. Folic Acid and Risk of Preterm Birth: A Meta-Analysis. Front. Neurosci. 2019, 13, 1284.
- Olapeju, B.; Saifuddin, A.; Wang, G.; Ji, Y.; Hong, X.; Raghavan, R.; Summers, A.; Keiser, A.; Ji, H.; Zuckerman, B.; et al. Maternal postpartum plasma folate status and preterm birth in a high-risk US population. Public Health Nutr. 2019, 22, 1281–1291.
- McClure, E.M.; Saleem, S.; Goudar, S.S.; Tikmani, S.S.; Dhaded, S.M.; Hwang, K.; Guruprasad, G.; Shobha, D.; Sarvamangala, B.; Yogeshkumar, S.; et al. The causes of stillbirths in south Asia: Results from a prospective study in India and Pakistan (PURPOSe). Lancet Glob. Health 2022, 10, e970–e977.
- Aminu, M.; Bar-Zeev, S.; White, S.; Mathai, M.; Van Den Broek, N. Understanding cause of stillbirth: A prospective observational multi-country study from sub-Saharan Africa. BMC Pregnancy Childbirth 2019, 19, 470.
- Goldenberg, R.L.; Muhe, L.; Saleem, S.; Dhaded, S.; Goudar, S.S.; Patterson, J.; Nigussie, A.; McClure, E.M. Criteria for assigning cause of death for stillbirths and neonatal deaths in research studies in low-middle income countries. J. Matern. Neonatal Med. 2019, 32, 1915–1923.
- Ng, K.Y.B.; Cherian, G.; Kermack, A.J.; Bailey, S.; Macklon, N.; Sunkara, S.K.; Cheong, Y. Systematic review and meta-analysis of female lifestyle factors and risk of recurrent pregnancy loss. Sci. Rep. 2021, 11, 7081.
- Nonyane, B.A.S.; Norton, M.; Begum, N.; Shah, R.M.; Mitra, D.K.; Darmstadt, G.L.; Baqui, A.H. Pregnancy intervals after stillbirth, neonatal death and spontaneous abortion and the risk of an adverse outcome in the next pregnancy in rural Bangladesh. BMC Pregnancy Childbirth 2019, 19, 62.
- Mao, Y.Y.; Yang, L.; Li, M.; Liu, J.; Zhu, Q.X.; He, Y.; Zhou, W.-J. Periconceptional folic acid supplementation and the risk of spontaneous abortion among women who prepared to conceive: Impact of supplementation initiation timing. Nutrients 2020, 12, 2264.
- Yakoob, M.Y.; Menezes, E.V.; Soomro, T.; Haws, R.A.; Darmstadt, G.L.; Bhutta, Z.A. Reducing stillbirths: Behavioural and nutritional interventions before and during pregnancy. BMC Pregnancy Childbirth 2009, 9, S3.
- Caniglia, E.C.; Zash, R.; Swanson, S.A.; Smith, E.; Sudfeld, C.; Finkelstein, J.L.; Diseko, M.; Mayondi, G.; Mmalane, M.; Makhema, J.; et al. Iron, folic acid, and multiple micronutrient supplementation strategies during pregnancy and adverse birth outcomes in Botswana. Lancet Glob Health 2022, 10, e850–e861.
- He, Y.; Pan, A.; Hu, F.B.; Ma, X. Folic acid supplementation, birth defects, and adverse pregnancy outcomes in Chinese women: A population-based mega-cohort study. Lancet 2016, 388, S91.
- Silva, C.; Keating, E.; Pinto, E. The impact of folic acid supplementation on gestational and long term health: Critical temporal windows, benefits and risks. Porto Biomed. J. 2017, 2, 315–332.
- Compañ Gabucio, L.M.; García de la Hera, M.; Torres Collado, L.; Fernández-Somoano, A.; Tardón, A.; Guxens, M.; Vrijheid, M.; Rebagliato, M.; Murcia, M.; Ibarluzea, J.; et al. The use of lower or higher than recommended doses of folic acid supplements during pregnancy is associated with child attentional dysfunction at 4–5 years of age in the inma project. Nutrients 2021, 13, 327.
- Compañ-Gabucio, L.M.; Torres-Collado, L.; Garcia-de la Hera, M.; Fernández-Somoano, A.; Tardón, A.; Julvez, J.; Sunyer, J.; Rebagliato, M.; Murcia, M.; Ibarluzea, J.; et al. Association between the Use of Folic Acid Supplements during Pregnancy and Children’s Cognitive Function at 7–9 Years of Age in the INMA Cohort Study. Int. J. Environ. Res. Public Health 2022, 19, 12123.
- Caffrey, A.; McNulty, H.; Irwin, R.E.; Walsh, C.P.; Pentieva, K. Maternal folate nutrition and offspring health: Evidence and current controversies. Proc. Nutr. Soc. 2019, 78, 208–220.
- Cao, X.; Xu, J.; Lin, Y.L.; Cabrera, R.M.; Chen, Q.; Zhang, C.; Steele, J.W.; Han, X.; Gross, S.S.; Wlodarczyk, B.J.; et al. Excess folic acid intake increases DNA de novo point mutations. Cell Discov. 2023, 9, 22.
- Alnabbat, K.I.; Fardous, A.M.; Shahab, A.; James, A.A.; Bahry, M.R.; Heydari, A.R. High Dietary Folic Acid Intake Is Associated with Genomic Instability in Peripheral Lymphocytes of Healthy Adults. Nutrients 2022, 14, 3944.
- Hinkle, S.N.; Buck Louis, G.M.; Rawal, S.; Zhu, Y.; Albert, P.S.; Zhang, C. A longitudinal study of depression and gestational diabetes in pregnancy and the postpartum period. Diabetologia 2016, 59, 2594–2602.
- Li, L.J.; Wang, X.; Chong, Y.S.; Chan, J.K.Y.; Tan, K.H.; Eriksson, J.G.; Huang, Z.; Rahman, M.L.; Cui, L.; Zhang, C. Exploring preconception signatures of metabolites in mothers with gestational diabetes mellitus using a non-targeted approach. BMC Med. 2023, 21, 99.
- He, J.; Jiang, D.; Cui, X.; Ji, C. Vitamin B12 status and folic acid/vitamin B12 related to the risk of gestational diabetes mellitus in pregnancy: A systematic review and meta-analysis of observational studies. BMC Pregnancy Childbirth 2022, 22, 587.
- Yang, Y.; Cai, Z.; Zhang, J. Association between maternal folate status and gestational diabetes mellitus. Food Sci. Nutr. 2021, 9, 2042–2052.
- Lai, J.S.; Pang, W.W.; Cai, S.; Lee, Y.S.; Chan, J.K.Y.; Shek, L.P.C.; Yap, F.K.; Tan, K.H.; Godfrey, K.M.; van Dam, R.M.; et al. High folate and low vitamin B12 status during pregnancy is associated with gestational diabetes mellitus. Clin. Nutr. 2018, 37, 940–947.
More
Information
Subjects:
Pediatrics
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
545
Revisions:
2 times
(View History)
Update Date:
18 Oct 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




