Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Beatrice Anghel | -- | 1543 | 2023-10-13 13:28:48 | | | |
| 2 | Jason Zhu | Meta information modification | 1543 | 2023-10-17 03:22:07 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Anghel, B.; Serboiu, C.; Marinescu, A.; Taciuc, I.; Bobirca, F.; Stanescu, A.D. External Beam Radiotherapy for Cervical Cancer. Encyclopedia. Available online: https://encyclopedia.pub/entry/50273 (accessed on 12 January 2026).
Anghel B, Serboiu C, Marinescu A, Taciuc I, Bobirca F, Stanescu AD. External Beam Radiotherapy for Cervical Cancer. Encyclopedia. Available at: https://encyclopedia.pub/entry/50273. Accessed January 12, 2026.
Anghel, Beatrice, Crenguta Serboiu, Andreea Marinescu, Iulian-Alexandru Taciuc, Florin Bobirca, Anca Daniela Stanescu. "External Beam Radiotherapy for Cervical Cancer" Encyclopedia, https://encyclopedia.pub/entry/50273 (accessed January 12, 2026).
Anghel, B., Serboiu, C., Marinescu, A., Taciuc, I., Bobirca, F., & Stanescu, A.D. (2023, October 13). External Beam Radiotherapy for Cervical Cancer. In Encyclopedia. https://encyclopedia.pub/entry/50273
Anghel, Beatrice, et al. "External Beam Radiotherapy for Cervical Cancer." Encyclopedia. Web. 13 October, 2023.
Copy Citation
The standard of care for locally advanced cervical cancer is external beam radiotherapy (EBRT) with simultaneous chemotherapy followed by an internal radiation boost. New imaging methods such as positron-emission tomography and magnetic resonance imaging have been implemented into daily practice for better tumor delineation in radiotherapy planning. The method of delivering radiation has changed with technical advances in qualitative imaging and treatment delivery. Image-guided radiotherapy (IGRT) plays an important role in minimizing treatment toxicity of pelvic radiation and provides a superior conformality for sparing the organs at risk (OARs) such as bone marrow, bowel, rectum, and bladder.
cervix cancer
image-guided brachytherapy
ART
1. Introduction
Cervical cancer is one of the most common malignancies in women worldwide and one of the deadliest forms of cancer with a high burden of disease in developing nations [1][2]. Infection with high-risk subtypes of the human papillomavirus is one of the most important risk factors involved in carcinogenesis [3][4]. Programs and health policies have influenced access to different levels of prevention. The research and development of a vaccine has been proven to significantly reduce the risk of developing cervical cancer in young women [5] but, when diagnosed in advanced stages, the outcomes for cervical cancer remain concerning. The 5-year OS for patients with regional disease is approximately 55% [6][7].
Chemoradiation (CRT) followed by brachytherapy (BT) is the main treatment for locally advanced cervical cancer (LACC) [8]. The addition of concurrent chemotherapy to external beam radiotherapy (EBRT) has improved the prognosis but treatment-related toxicity and distant recurrence remain a challenge [9]. Since 1999, CRT has been recognized as the standard of care in LACC with the results of five randomized controlled phase III trials showing a benefit of 30% to 50% survival advantage by using cisplatin-based chemotherapy to radiation (GOG 85, GOG 120, SWOG 8797/ Intergroup 0107, RTOG 9001) [10][11][12][13][14]. Conventional radiotherapy for cervical cancer is based on cervical examination, 3D conformal radiotherapy, and 2D intracavitary brachytherapy. Definitive CRT for early-stage cervical cancer has shown excellent local control. Compared with 2D or 3D EBRT, intensity-modulated radiation therapy (IMRT) refers to delivering clinical targeted doses using multiple beam angles and field shapes while protecting normal organs such as marrow-containing pelvic bones, bowel, rectum, and bladder [15][16][17][18]. With advances in imaging modalities, 3D-IGABT with CT or MRI has been frequently used to refine target coverage and decrease the dose to normal structures [19].
2. From 2D to 3D Conformal Radiotherapy
In the past, the treatment of LACC with RT has been implemented with 2D EBRT using anatomical landmarks on X-rays to be able to encompass the primary disease and the potential spread. Two parallel opposed fields (AP–PA) were the basic techniques of EBRT. Later, the “four-field box” technique was introduced to achieve better conformality with four large treatment fields, with the upper border at the level of the aortic bifurcation (L3–L5 vertebral body levels; T12 level in case of extended field in case of paraaortic nodes being involved), the anterior border placed anteriorly to the pubic symphysis, and another border posteriorly outlining the sacrum at the S3/S4 level.
The lateral borders are 1.5–2cm lateral to the pelvic brim and the inferior border is the bottom of the obturator foramen. Although easy to implement in practice, geographical misses have led to reduced LC [20]. CT invention was brought into RT planning after the 1990s, marking the evolution from 2D to 3D conformal RT. Based on the information obtained from a CT scan of the patient imaged in the same position for treatment and in a reproducible way has helped clinicians, physicists, and radiation therapists to understand concepts related to target delineation—gross tumor volume (GTV), clinical target volume (CTV), and planning target volume (PTV)—published in ICRU Report 50 and ICRU Report 62 [21][22]. This technique utilizes anatomical landmarks to better shape the dose distribution of the PTV with the protection of OARs with multileaf collimators (MLCs) [23]. Three-dimensional conformal RT provides volumetric dosimetry and has the advantage of quantifying and correlating treatment outcomes and toxicities.
3. Intensity-Modulated Radiotherapy (IMRT) Volumetric Intensity-Modulated Arcs (VMAT)
IMRT is a radiotherapy technique that warrants rigorous conformation of the radiation dose to the target volume. Through IMRT, there is potential to significantly reduce long-term morbidity and improve local control. Compared with conventional EBRT, IMRT uses small beamlets with variable intensity and better conformality to 3D target volumes while minimizing the dose to critical adjacent structures. In 2002, excellent results have been reported with the initial implementation of IMRT for women with gynecological cancers.
TIME-C, Uterus-11, PARCER, INTERTECC-2, Huang et al., and Ghandi et al. are numerous major studies involving advances in radiation therapy techniques with significant lower bowel and bladder toxicity [24][25][26][27]. Emerging evidence has shifted the balance increasingly in favor of the ordinary use of IMRT. IMRT can be given via multiple static fields or in arcs, a newer radiation technique known as volumetric intensity-modulated arc radiation therapy (VMAT). Conformality, faster treatment time, and fewer monitor units are some of the main advantages offered by VMAT.
IGRT can deliver a higher dose to the primary tumor and areas at high risk for recurrence with the SIB technique without exposing adjacent normal organs to radiation.
IMRT on a routine basis faces issues such as organ movement during RT (intrafraction) and during treatment (interfraction). Jadon et al. [28] reported that organ motion in EBRT for cervical cancer is present and the degree of movement during radiation therapy should be considered. Bladder and rectal filling influence uterine and cervical motion [29].
As pelvic organ motion seems to be patient-specific, personalized PTV margins and adaptive image-guided radiotherapy (IGRT) have been proposed to cover accurately the target volume while enlarging the normal tissues’ protection. As IMRT planning can spare normal OARs, IMRT plans and SIB of LNs are a great strategy to reduce radiation-induced normal tissue complication probability while improving outcomes in a shorter overall treatment time.
4. Adaptive External Beam Radiotherapy
IGRT is a dynamic complex process of performing imaging before daily radiotherapy with the intent of achieving target accuracy and precision by correcting geometric and anatomic variations. IGRT techniques consist of planar or volumetric imaging to obtain tighter treatment margins. Highly conformal techniques such as IMRT and stereotactic body radiotherapy (SBRT) demand a high level of setup reproducibility to ensure that the planned dose is delivered to the interest area. Planar IGRT techniques compare 2D radiographs in the same treatment position with digitally reconstructed radiographs (DRR), images obtained from simulation. This allows accurate matching of the radiograph from simulation on bony anatomy with the radiograph from treatment. Volumetric IGRT techniques provide 3D imaging comparable with the initial simulation imaging to check position. This allows for soft tissue and bony anatomy as well (volumetric IGRT: cone-beam CT, CT on rails, and megavoltage CT imaging) [30].
IGRT plays a central role in modern radiotherapy, especially for hypofractionation and stereotactic treatments. It can boost confidence that radiotherapy treatment is in the desired size and margins can be tailored when appropriate. Many factors can determine anatomic deformations to the tumor and OARs throughout a course of treatment:
Firstly, anatomic motion is caused by the system (e.g., musculoskeletal, gastrointestinal, genito-urinary, cardiac, and respiratory).
Secondly, the treatment-induced changes such as tumor reduction, regrowth resulting from accelerated repopulation, weight gain or loss, concomitant chemotherapy, and fibrosis of normal structures.
It can happen at three levels: offline between sessions, online immediately prior to treatment, and real-time during radiotherapy. Based on a predetermined set of scenarios, simple forms of adaptive radiotherapy apply correct measures and will define the concept of a multiadaptive image-guided radiation therapy (IGRT) plan.
In LACC, the uterus and cervix change position during treatment delivery due to variations in rectal and bladder filling and tumor shrinkage during RT [30]. Deformable image registration for transferring anatomic contours and dose between images are described in recent practice advances for forms of adaptive radiotherapy and software tools to analyze automatic treatment planning and deformable dose summation [31].
Adaptive radiotherapy is defined as a temporal adjustment of the treatment plan delivery to a patient, according to objective anatomic changes caused by weight loss, tumor shrinkage, or internal motion (Figure 1 and Figure 2).
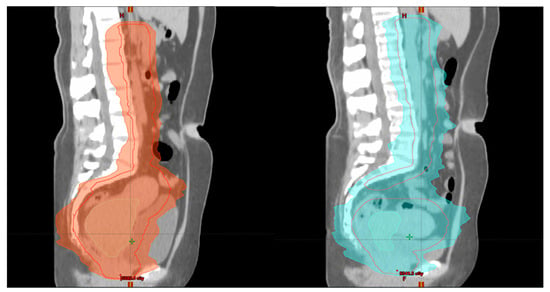
Figure 1. Patient 1 with FIGO stage IIIC2 LACC: left image (week 1)—initial plan of EBRT and right image (week 3) during EBRT—adaptive planning (sagittal view) for tumor shrinkage.
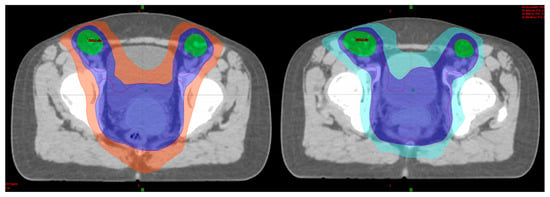
Figure 2. Patient 1 with FIGO stage IIIC2 LACC: left image (week 1)—initial plan of EBRT and right image (week 3) during EBRT—adaptive planning (axial view) for tumor shrinkage.
A new concept of internal target volume (ITV) is generated to account for various treatment positions for LACC by performing a simulation with a full and an empty bladder and then combining the CTV to be taken into consideration for every move between these two bladder filling extremes [32]. A margin between 3 and 7 mm (PTV) is added to the ITV to fully encompass setup and position errors. Then, volumetric IGRT is applied with cone beam CT (CBCT) to verify the position of the CTV and PTV daily prior to RT delivery. More advanced adaptive strategies have made space for a highly advanced work for treatment delivery called “plan of the day” or “online adaptive RT”. These approaches include same-day replanning and recently published review articles are available in the literature [33].
In special scenarios, after paraaortic exploration or hernia repairs, open or laparoscopic, it is vital to use IGRT techniques to protect the wound and prevent complications or even delays in starting radiotherapy for LACC [34].
References
- Arbyn, M.; Weiderpass, E.; Bruni, L.; de Sanjosé, S.; Saraiya, M.; Ferlay, J.; Bray, F. Estimates of incidence and mortality of cervical cancer in 2018: A worldwide analysis. Lancet Glob. Health 2020, 8, E191–E203.
- Brenner, D.R.; Weir, H.K.; Demers, A.A.; Ellison, L.F.; Louzado, C.; Shaw, A.; Turner, D.; Woods, R.R.; Smith, L.M. Canadian Cancer Statistics Advisory Committee. CMAJ 2020, 192, E199–E205.
- Otter, S.; Whitaker, S.; Chatterjee, J.; Stewart, A. The human papillomavirus as a common pathogen in oropharyngeal, anal, and cervical cancers. Clin. Oncol. 2019, 31, 81–90.
- Walboomers, J.M.M.; Jacobs, M.V.; Manos, M.M.; Bosch, F.X.; Kummer, J.A.; Shah, K.V.; Snijders, P.J.; Peto, J.; Meijer, C.J.; Muñoz, N. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. J. Pathol. 1999, 189, 12–19.
- Lei, J.; Ploner, A.; Elfström, K.M.; Wang, J.; Roth, A.; Fang, F.; Sundström, K.; Dillner, J.; Sparén, P. HPV Vaccination and the Risk of Invasive Cervical Cancer. N. Engl. J. Med. 2020, 383, 1340–1348.
- Benard, V.B.; Watson, M.; Saraiya, M.; Harewood, R.; Townsend, J.S.; Stroup, A.M.; Weir, H.K.; Allemani, C. Cervical cancer survival in the United States by race and stage (2001–2009): Findings from the CONCORD-2 study. Cancer 2017, 123 (Suppl. 24), 5119–5137.
- Han, K.; Milosevic, M.; Fyles, A.; Pintilie, M.; Viswanathan, A.N. Trends in the utilization of brachytherapy in cervical cancer in the United States. Int. J. Radiat. Oncol. Biol. Phys. 2013, 87, 111–119.
- Cervical Cancer Version 1.2024. Available online: https://www.nccn.org/professionals/physician_gls/pdf/cervical.pdf (accessed on 22 August 2023).
- Vale, C.; Tierney, J.F.; Stewart, L.A.; Brady, M.; Dinshaw, K.; Jakobsen, A. Chemoradiotherapy for Cervical Cancer Meta-Analysis Collaboration. Reducing uncertainties about the effects of chemoradiotherapy for cervical cancer: A systematic review and meta-analysis of individual patient data from 18 randomized trials. J. Clin. Oncol. 2008, 26, 5802–5812.
- Morris, M.; Eifel, P.J.; Lu, J.; Grigsby, P.W.; Levenback, C.; Stevens, R.E.; Rotman, M.; Gershenson, D.M.; Mutch, D.G. Pelvic radiation with concurrent chemotherapy compared with pelvic and para-aortic radiation for high-risk cervical cancer. N. Engl. J. Med. 1999, 340, 1137–1143.
- Keys, H.M.; Bundy, B.N.; Stehman, F.B.; Muderspach, L.I.; Chafe, W.E.; Suggs, C.L.; Walker, J.L.; Gersell, D. Cisplatin, radiation, and adjuvant hysterectomy compared with radiation and adjuvant hysterectomy for bulky stage IB cervical carcinoma. N. Engl. J. Med. 1999, 340, 1154–1161.
- Whitney, C.W.; Sause, W.; Bundy, B.N.; Malfetano, J.H.; Hannigan, E.V.; Fowler, W.C.; Clarke-Pearson, D.L.; Liao, S.Y. Randomized comparison of fluorouracil plus cisplatin versus hydroxyurea as an adjunct to radiation therapy in stage IIB-IVA carcinoma of the cervix with negative para-aortic lymph nodes: A Gynecologic Oncology Group and Southwest Oncology Group study. J. Clin. Oncol. 1999, 17, 1339–1348.
- Peters, W.A., III; Liu, P.Y.; Barrett, R.J.; Stock, R.J.; Monk, B.J.; Berek, J.S.; Souhami, L.; Grigsby, P.; Gordon, W., Jr.; Alberts, D.S. Concurrent chemotherapy and pelvic radiation therapy compared with pelvic radiation therapy alone as adjuvant therapy after radical surgery in high-risk early-stage cancer of the cervix. J. Clin. Oncol. 2000, 18, 1606–1613.
- Rose, P.G.; Bundy, B.N.; Watkins, E.B.; Thigpen, J.T.; Deppe, G.; Maiman, M.A.; Clarke-Pearson, D.L.; Insalaco, S. Concurrent cisplatin-based radiotherapy and chemotherapy for locally advanced cervical cancer. N. Engl. J. Med. 1999, 340, 1144–1153.
- Mundt, A.J.; Lujan, A.E.; Rotmensch, J.; Waggoner, S.E.; Yamada, S.D.; Fleming, G.; Roeske, J.C. Intensity-modulated whole pelvic radiotherapy in women with gynecologic malignancies. Int. J. Radiat. Oncol. Biol. Phys. 2002, 52, 1330–1337.
- Mundt, A.J.; Mell, L.K.; Roeske, J.C. Preliminary analysis of chronic gastrointestinal toxicity in gynecology patients treated with intensity-modulated whole pelvic radiation therapy. Int. J. Radiat. Oncol. Biol. Phys. 2003, 56, 1354–1360.
- Chen, M.F.; Tseng, C.J.; Tseng, C.C.; Kuo, Y.C.; Yu, C.Y.; Chen, W.C. Clinical outcome in posthysterectomy cervical cancer patients treated with concurrent cisplatin and intensity-modulated pelvic radiotherapy: Comparison with conventional radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2007, 67, 1438–1444.
- Beriwal, S.; Gan, G.N.; Heron, D.E.; Selvaraj, R.N.; Kim, H.; Lalonde, R.; Kelley, J.L.; Edwards, R.P. Early clinical outcome with concurrent chemotherapy and extended-field, intensity-modulated radiotherapy for cervical cancer. Int. J. Radiat. Oncol. Biol. Phys. 2007, 68, 166–171.
- Pötter, R.; Tanderup, K.; Kirisits, C.; de Leeuw, A.; Kirchheiner, K.; Nout, R.; Tan, L.T.; Haie-Meder, C.; Mahantshetty, U.; Segedin, B.; et al. The EMBRACE II study: The outcome and prospect of two decades of evolution within the GEC—ESTRO GYN working group and the EMBRACE studies. Clin. Transl. Radiat. Oncol. 2018, 9, 48–60.
- Bonin, S.R.; Lanciano, R.M.; Corn, B.W.; Hogan, W.M.; Hartz, W.H.; Hanks, G.E. Bony landmarks are not an adequate substitute for lymphangiography in defining pelvic lymph node location for the treatment of cervical cancer with radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 1996, 34, 167–172.
- International Commission on Radiation Units and Measurements. ICRU Report 50 Prescribing, Recording, and Reporting Photon Beam Therapy; International Commission on Radiation Units and Measurements: Bethesda, MD, USA, 1993; Volume 21.
- International Commission on Radiation Units and Measurements. ICRU Report 62 Prescribing, Recording, and Reporting Photon Beam Therapy; Supplement to ICRU Report 50; International Commission on Radiation Units and Measurements: Bethesda, MD, USA, 1999; Volume 21.
- Gerstner, N.; Wachter, S.; Knocke, T.H.; Fellner, C.; Wambersie, A.; Pötter, R. The benefit of Beam’s eye view-based 3D treatment planning for cervical cancer. Radiother. Oncol. 1999, 51, 71–78.
- Klopp, A.H.; Yeung, A.R.; Deshmukh, S.; Gil, K.M.; Wenzel, L.; Westin, S.N.; Gifford, K.; Gaffney, D.K.; Small Jr, W.; Thompson, S.; et al. Patient-reported toxicity during pelvic intensity-modulated radiation therapy: NRG oncology-RTOG 1203. J. Clin. Oncol. 2018, 36, 2538–2544.
- Marnitz, S.; Tsunoda, A.T.; Martus, P.; Vieira, M.; Affonso Junior, R.J.; Nunes, J.; Budach, V.; Hatel, H.; Mustea, A.; Sehouli, J.; et al. Surgical versus clinical staging prior to primary chemoradiation in patients with cervical cancer FIGO stages IIB-IVA: Oncologic results of a prospective randomized international multicenter (Uterus-11) intergroup study. Int. J. Gynecol. Cancer. 2020, 30, 1855–1861.
- Chopra, S.; Dora, T.; Gupta, S.; Kannan, S.; Engineer, R.; Mangaj, A.; Maheshwari, A.; Shylasree, T.S.; Ghosh, J.; Paul, S.N.; et al. Phase III randomized trial of postoperative adjuvant conventional radiation (3DCRT) versus image-guided intensity-modulated radiotherapy (IG-IMRT) in cervical cancer (PARCER): Final analysis. Int. J. Radiat. Oncol. Biol. Phys. 2020, 108, S1–S2.
- Mell, L.K.; Sirák, I.; Wei, L.; Tarnawski, R.; Mahantshetty, U.; Yashar, C.M.; McHale, M.T.; Xu, R.; Honerkamp-Smith, G.; Carmona, R.; et al. Bone marrow-sparing intensity modulated radiation therapy with concurrent cisplatin for stage IB-IVA cervical cancer: An international multicenter phase II clinical trial (INTERTECC-2). Int. J. Radiat. Oncol. Biol. Phys. 2017, 97, 536–545.
- Jadon, R.; Pembroke, C.A.; Hanna, C.L.; Palaniappan, N.; Evans, M.; Cleves, A.E.; Staffurth, J. A systematic review of organ motion and image-guided strategies in external beam radiotherapy for cervical cancer. Clin. Oncol. R. Coll. Radiol. 2014, 26, 185–196.
- Hoppe, R.T.; Phillips, T.L.; Roach, M. Chapter 12: Image-guided Adaptive Radiotherapy. In Textbook of Radiation Oncology, 3rd ed.; Keall, P.J., Hsu, A., Xing, L., Eds.; Saunders: Philadelphia, PA, USA, 2004.
- Verellen, D.; De Ridder, M.; Storme, G. A (short) history of image-guided radiotherapy. Radiother. Oncol. 2008, 86, 4–13.
- Chan, P.; Dinniwell, R.; Haider, M.A.; Cho, Y.B.; Jaffray, D.; Lockwood, G.; Levin, W.; Manchul, L.; Fyles, A.; Milosevic, M. Inter- and intrafractional tumor and organ movement in patients with cervical cancer undergoing radiotherapy: A cinematic-MRI point-of-interest study. Int. J. Radiat. Oncol. Biol. Phys. 2008, 70, 1507–1515.
- Bondar, L.; Hoogeman, M.; Mens, J.W.; Dhawtal, G.; de Pree, I.; Ahmad, R.; Quint, S.; Heijmen, B. Toward an individualized target motion management for IMRT of cervical cancer based on model-predicted cervix-uterus shape and position. Radiother. Oncol. 2011, 99, 240–245.
- Shelley, C.E.; Barraclough, L.H.; Nelder, C.L.; Otter, S.J.; Stewart, A.J. Adaptive Radiotherapy in the Management of Cervical Cancer: Review of Strategies and Clinical Implementation. Clin. Oncol. R. Coll. Radiol. 2021, 33, 579–590.
- Dumitrescu, V.; Serban, D.; Costea, D.; Dumitrescu, D.; Bobirca, F.; Geavlete, B.; Bratu, D.G.; Tribus, L.; Serboiu, C.; Alius, C.; et al. Transabdominal Preperitoneal Versus Lichtenstein Procedure for Inguinal Hernia Repair in Adults: A Comparative Evaluation of the Early Postoperative Pain and Outcomes. Cureus 2023, 15, e41886.
More
Information
Subjects:
Oncology
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
803
Revisions:
2 times
(View History)
Update Date:
17 Oct 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




