Your browser does not fully support modern features. Please upgrade for a smoother experience.

Submitted Successfully!
Thank you for your contribution! You can also upload a video entry or images related to this topic.
For video creation, please contact our Academic Video Service.
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | Iwona Bodys-Cupak | -- | 2217 | 2023-09-14 13:17:44 | | | |
| 2 | Sirius Huang | Meta information modification | 2217 | 2023-09-15 04:57:23 | | |
Video Upload Options
We provide professional Academic Video Service to translate complex research into visually appealing presentations. Would you like to try it?
Cite
If you have any further questions, please contact Encyclopedia Editorial Office.
Bednarek, A.; Klepacz, R.; Bodys-Cupak, I.E. Care of Patients with Rheumatic Diseases. Encyclopedia. Available online: https://encyclopedia.pub/entry/49172 (accessed on 08 February 2026).
Bednarek A, Klepacz R, Bodys-Cupak IE. Care of Patients with Rheumatic Diseases. Encyclopedia. Available at: https://encyclopedia.pub/entry/49172. Accessed February 08, 2026.
Bednarek, Anna, Robert Klepacz, Iwona Elżbieta Bodys-Cupak. "Care of Patients with Rheumatic Diseases" Encyclopedia, https://encyclopedia.pub/entry/49172 (accessed February 08, 2026).
Bednarek, A., Klepacz, R., & Bodys-Cupak, I.E. (2023, September 14). Care of Patients with Rheumatic Diseases. In Encyclopedia. https://encyclopedia.pub/entry/49172
Bednarek, Anna, et al. "Care of Patients with Rheumatic Diseases." Encyclopedia. Web. 14 September, 2023.
Copy Citation
In order to provide the highest quality of care to patients, nurses working at the advanced level are expected to develop knowledge and to initiate services and practices carried out in collaboration with other professionals. In 2018, the European League Against Rheumatism (EULAR) updated its recommendations for the role of the nurse in the management and care of patients with rheumatic conditions.
rheumatic diseases
nursing care
advanced practice nurse
EULAR recommendations for nurses
1. Introduction
The global prevalence of rheumatic diseases in adults ranges from 0.24% to 1% and is varied by genetic and environmental factors. Rheumatic diseases are also a significant cause of chronic illnesses in the pediatric population. Multiple organ complications, disability, and the inability to participate in social life are common consequences [1][2]. Public education programs, introduced in many countries, seek to increase public awareness of rheumatic diseases [3][4]. They have also contributed to early diagnosis and therapy. On the other hand, advances in the management of rheumatologic conditions and biomedical research in immunology and genetics in recent years have raised the prospect of optimal health functioning for patients affected by inflammatory joint disease.
Most people want to maintain a high quality of life despite chronic illness. This has resulted in a shift in the health needs of patients and their families, particularly in the need for professional support and preparation for self-care. Hence, new models of care, including innovative organizational and educational solutions for nurses, have also become necessary [5].
2. EULAR Recommendations for Nurses
A review of the literature indicates the effectiveness, safety, and accessibility of care provided by nurses from the patient’s perspective [6][7]; this is also reflected in the priority principles for the recommendations developed by the EULAR 2018 panel of experts. Rheumatology nurses work in close collaboration with patients and their families [8]. As members of an interdisciplinary healthcare team, they share a focus on effective care that addresses health needs, values, and patient preferences. In their professional practice, nurses use different sources of knowledge, i.e., scientific evidence, including protocols and guidelines, but also their own nursing experience, patients’ aspirations (needs), and territorial contexts [9][10].
Patient education by the nurse, including therapeutic aspects and health promotion, is strongly emphasized in the updated EULAR 2018 recommendations [11]. Several authors confirm the positive impact of nurse-led patient education programs in disease-related areas such as pain, illness perception, quality of life, and adherence to recommendations [10][11][12][13].
Guided by evidence from the research, patient satisfaction with nursing care was made a priority. It was demonstrated that consultations with nurses have a significant, positive, and long-term (two years) effect on patient satisfaction [14]. In addition, it was reported that patients appreciate maintaining a professional relationship with a nurse. Studies also emphasized nurses’ holistic and professional approach to care, and patients’ trust in nurses’ knowledge, as well as a supportive style of mutual relations [15][16][17].
The unpredictable nature of rheumatic conditions and new treatment options sometimes require prompt access to care. At the same time, we can take advantage of the new forms of communication, support, and follow-up of diseases that are provided by online consultations, which allow for remote care [16]. When making their recommendation for quick patient access to nursing care, the EULAR task force focused on the current scientific evidence from qualitative studies in which patients indicated that telehealth follow-up and online consultations by nurses gave them a sense of personalized support from a knowledgeable healthcare team. The quality of this kind of service was comparable to the quality of a conventional follow-up to control the disease activity performed by a physician [18][19].
Randomized clinical trials comparing nurse-led and physician-led follow-up of patients showed that the quality of control of disease activity resulting from nursing care was equivalent to the quality of control when the care was provided by physicians. There were no significant differences in the quality of health functioning between patients monitored by a nurse and a physician. In addition, nurses played an important role in the early detection of inflammatory changes in joints (by physical examination, including assessment of pain, swelling and skin warmth within the joint), interpretation of laboratory results, continuation of drug treatment, and adherence to vaccination schedules [20]. Nursing care was cost-neutral or slightly less costly than the care provided by physicians, but there was no evidence of savings in services provided. When developing this recommendation, the panel of experts recognized the need for involving nurses in the comprehensive management and monitoring of the disease (disease management) [21][22][23].
Further recommendations of the expert panel focused on the need for nurses to provide support to patients with psychosocial problems in order to reduce symptoms of anxiety and depression and to motivate them to function effectively despite their disease. Psychological stress experienced by patients with rheumatologic conditions has a documented negative impact on their somatic complaints and should be eliminated. In addition, depression is a well-known comorbid condition that requires proper treatment and careful handling of the patient [24].
In a study of rheumatology patients with symptoms of depression, the quality of nurse-led care was found to be equivalent to the care provided by a rheumatologist. It was noted that patients and their families appreciated the opportunity to have an in-depth conversation with a nurse, where they could tackle various issues affecting their mental state [12]. Hence, the identification of the psychosocial problems of patients with rheumatologic conditions and supporting them in this respect were found to be key components of nursing care. The simultaneous promotion of self-management gives patients and their families the opportunity to gain the necessary knowledge, skills, and confidence to cope with the physical and psychosocial consequences of living with a chronic disease and facilitates making lifestyle changes following their preferences [17]. Research has confirmed that nurse-led interventions can improve patients’ and/or families’ sense of self-efficacy to cope with fluctuations of the disease in daily life [25][26][27].
The final EULAR 2018 recommendations address the aspects of continuing education for nurses in the specialty of rheumatology in order to improve and maintain knowledge and skills, as well as the undertaking of extended/advanced roles following specialized training, in compliance with national regulations. The wording of these recommendations remained unchanged from previous recommendations [28]. However, the level of evidence for these recommendations has increased due to new insights from studies showing that educational programs for rheumatology nurses resulted in increased knowledge and skills, as well as improvements in practices. Some tasks traditionally performed by physicians and physiotherapists, such as joint examination, identification of signs and symptoms in rheumatic diseases, and the ability to distinguish abnormalities, can be performed by nurses who have completed specialized training. Rheumatology nursing is not, however, a formal specialty in every country. Yet the education of nurses in the specialty of rheumatology is crucial to the development of competent and holistic care for patients of all ages with rheumatological problems [29][30].
3. Summary of Recommendations—Tasks for Nurses in the Care of Patients with Rheumatic Diseases
The EULAR 2018 recommendations for rheumatology nurses and the review of the research highlight the need to improve nurses’ knowledge and practice of specialized clinical skills, pedagogical and psychological education, and work organization. Nurses, especially APNs, play an important role in the process of patient diagnosis and therapy (Table 1).
At the same time, the importance of their communication skills in identifying patients’ psychosocial problems and in supporting patients and their families in making therapeutic decisions is also increasingly recognized. Person-centered care and partnership with patients are also important areas in APNs’ activities that motivate patients to self-care. The proper organization of care by nurses is important to avoid the risk of excessive workload that may reduce the quality of services provided [31][32].
Table 1. Summary of selected items in terms of the overriding principles and detailed EULAR recommendations regarding the care of rheumatological patients by nurses.
| Author | Title | Journal, Year | Summary of Research Results |
|---|---|---|---|
| Perkin K. [6] | Nurse Practitioners and Interprofessional Collaboration | Journal of Interprofessional Care 2011, 25(4), 243–4. | In the opinion of the patient, care provided by nurses is effective, safe and easily accessible. Rheumatology nurses are important members of the medical team caring for the patient. |
| Riley L., et al. [33] | The Role of Nurse Practitioners in Delivering Rheumatology Care and Services: Results of a U.S. survey | Journal of the American Association of Nurse Practitioners 2017, 29(11),673–681. | Rheumatology nurses work in an interdisciplinary medical team, they constantly cooperate with the patient and his family in the field of care and treatment. |
| van Eijk-Hustings Y,. et al. [34] | Dissemination and Evaluation of the European League against Rheumatism Recommendations for the Role of the Nurse in the Management of Chronic Inflammatory Arthritis: Results of a Multinational Survey among Nurses, Rheumatologists and Patients | Rheumatology 2014, 53 (8), 1491–6. | In professional practice, nurses use various sources of knowledge, i.e., scientific evidence, including protocols and guidelines, as well as their own experience gained while working with patients and their families. |
| Fusama M., et al. [35] | Survey on Attitudes Regarding EULAR Recommendations for the Role of Nurses Involved in Medical Care of Patients with Chronic Inflammatory Arthritis in Japan | Modern Rheumatology 2017, 27(5), 886–93. | In patient care, nurses rely on a variety of sources of knowledge, including scientific evidence, protocols, and guidelines. They are also guided by their own nursing experience resulting from the territorial context and take into account the needs and aspirations of patients. |
| Barbosa L., et al. [9] | Applicability of the EULAR Recommendations on theRrole of the Nurse in the Management of Chronic Inflammatory Arthritis in Portugal | Acta Reumatologica Portuguesa 2013, 38,(3), 186–91. | |
| Solomon D.H., et al. [14] | Roles of Nurse Practitioners and Physician Assistants in Rheumatology Practices in the US | Arthritis Care & Research 2014, 66(7), 1108–13. | The care provided by rheumatology nurses is effective and takes into account the health needs, values and preferences of patients. Patient education by nurses covers areas related to the disease, such as pain, quality of life, and adherence. |
| Walker J.[32] | Rheumatoid Arthritis: Role of the Nurse and Multidisciplinary Team | British Journal of Nursing 2012, 21(6), 334, 336–9. | Patients are satisfied with the nursing care. They have a positive experience of maintaining a competent relationship with the nurse. |
| Morgan S. & Yoder L.H. [36] | A Concept Analysis of Person-Centered Care | Journal of Holistic Nursing 2012, 30(1), 6–15. | The holistic and professional approach of nurses to care inspires the trust of rheumatology patients in the knowledge of nurses, and also strengthens the supportive style of mutual relations. |
| Larsson I. [37] | Nurse-Led Care and Patients as Partners Are Essential Aspects of the Future of Rheumatology Care | The Journal of Rheumatology 2017, 44(6), 720–722. | In the patients’ opinion, teleconsultation by nurses provides them with a sense of individual support from a competent healthcare team. The quality of service provided by nurses is comparable to being observed by a physician in terms of disease control. |
| Frølund J.C. & Primdahl J. [26] | Patients’ Experiences of Nurse-Led Screening for Cardiovascular Risk in Rheumatoid Arthritis | Musculoskeletal Care 2015, 13(4), 236–47. | Rheumatology nurses have an important role in the early detection of inflammatory changes in the joints, the interpretation of laboratory test results, the follow-up of pharmacological treatment, and the monitoring of patients’ adherence to vaccination schedules. |
| Grønning K., et al. [16] | Patients’ Confidence in Coping with Arthritis after Nurse-Led Education; a Qualitative Study | BMC Nursing 2016, 15(28), 1–8. | Patients appreciate the opportunity to discuss various issues affecting their mental state with the nurse. Nurses provide support to patients with psychosocial problems in order to reduce the symptoms of anxiety and depression and motivate them to function effectively in the disease. |
| Robinson S., et al. [30] | A National Survey of Nurse Training: Confidence and Competence in Educating Patients Commencing Methotrexate Therapy | Musculoskeletal Care 2017, 15(3), 281–92. | Nurses play an important role in the early detection of inflammatory changes in the joints, the interpretation of laboratory test results and the continuation of pharmacological treatment. Nurse-delivered care can reduce hospital admissions and lower the cost of care. |
| Primdahl J., et al. [38] | The Impact on Self-Efficacy of Different Types of Follow-Up Care and Disease Status in Patients with Rheumatoid Arthritis–A Randomized Trial | Patient Education and Counseling 2012, 88(1), 121–128. | Identification of psychosocial problems of patients with rheumatological diseases by nurses and their support are important elements of nursing care for patients and their families. Nurse-led interventions can improve patients’ self-efficacy to cope with the disease in their daily lives. |
EULAR recommendations show that APNs are able to independently provide effective follow-up of patients with chronic rheumatoid disease, with control of the risk factors for relapse and the early detection of complications. According to patients, care provided by nurses can improve their quality of life and enhance satisfaction with medical services through longer and more detailed consultations [28]. From the perspective of a healthcare system, nurse-delivered care can reduce hospital admissions, and lower the cost of care and support team coordination [36]. Patients value the competence of nurses, especially APNs, and patient trust in the family physician is the most important factor influencing the perception of the importance of care provided by nurses. Patient perspectives provide important insights into the implementation of APNs into the healthcare system. It enhances nurses’ sense of self-efficacy, resulting in improved nursing services and higher quality of care [37][38].
In conclusion, it is important to bear in mind that all medical services are defined by particular healthcare systems. Regardless of the formal conditions, a precise definition of the roles and tasks of particular professional groups should optimize the healthcare provided. This is intended to result in prompt diagnosis, and in effective, safe therapy with a consideration of the impact of the chronic disease on the patient’s functioning and immediate environment (Figure 1).
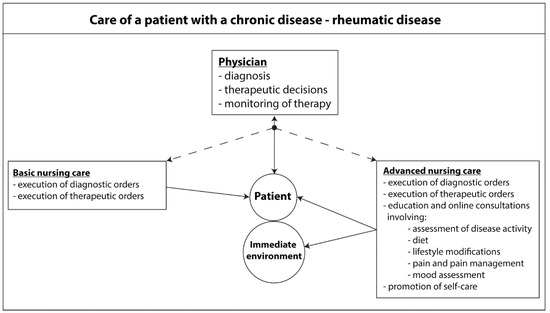
Figure 1. Care of a patient with a chronic rheumatic disease.
References
- Tobón, G.J.; Youinou, P.; Saraux, A. The environment, geo-epidemiology, and autoimmune disease: Rheumatoid arthritis. J. Autoimmun. 2010, 35, 10–14.
- Safiri, S.; Kolahi, A.A.; Hoy, D.; Smith, E.; Bettampadi, D.; Mansournia, M.A.; Almasi-Hashiani, A.; Ashrafi-Asgarabad, A.; Moradi-Lakeh, M.; Qorbani, M.; et al. Global, regional and national burden of rheumatoid arthritis 1990–2017: A systematic analysis of the global burden of disease study 2017. Ann. Rheum. Dis. 2019, 78, 1463–1471.
- Goma, S.H.; Razek, M.R.A.; Abdelbary, N.M. Impact of rheumatoid arthritis on the quality of life and its relation to disease activity. Egypt. Rheumatol. Rehabil. 2019, 46, 304–312.
- Symmons, D.; Mathers, C.; Pfleger, B. The Global Burden of Rheumatoid Arthritis in the Year 2000 Global Burden of Disease; World Health Organization: Geneva, Switzerland, 2015; Volume 18, pp. 1–30.
- Salmond, S.W.; Echevarria, M. Healthcare Transformation and Changing Roles for Nursing. Orthop. Nurs. 2017, 36, 12–25.
- Perkin, K. Nurse practitioners and interprofessional collaboration. J. Interprofessional Care 2011, 25, 243–244.
- Dowling, M.; Beauchesne, M.; Farrelly, F.; Murphy, K. Advanced practice nursing: A concept analysis. Int. J. Nurs. Pract. 2013, 19, 131–140.
- The Centre for Evidence-Based Medicine (CEBM). Oxford Centre for Evidence-Based Medicine—Levels of Evidence (March 2009) Web Page. Available online: http://www.cebm.net/oxford-centre-evidence-based-medicine-levels-evidence-march-2009/ (accessed on 1 May 2023).
- Barbosa, L.; Ramiro, S.; Santos, M.J.; Canas Da Silva, J. Applicability of the EULAR recommendations on the role of the nurse in the management of chronic inflammatory arthritis in Portugal. Acta Reumatol. Port. 2013, 38, 186–191.
- Minnock, P.; McKee, G.; Kelly, A.; Carter, C.C.; Menzies, W.; O’Sullivan, D.; Richards, P.; Ndosi, M.; van Eijk Hustings, Y. Nursing sensitive outcomes in patients with rheumatoid arthritis: A systematic literature review. Int. J. Nurs. Stud. 2018, 77, 115–129.
- Knittle, K.; De Gucht, V.; Hurkmans, E.; Peeters, A.; Ronday, K.; Maes, S.; Vlieland, T.V. Targeting motivation and self-regulation to increase physical activity among patients with rheumatoid arthritis: A randomised controlled trial. Clincal Rheumatol. 2015, 34, 231–238.
- Paek, S.I.; Jung, S.M.; Lee, L.; Kwok, S.K.; Kim, W.K.; Park, S.H.; Ju, J.H.; Sohng, K.Y. Effects of Individual Education Using a Treating-to-target Strategy in Patients with Rheumatoid Arthritis. Int. J. Rheum. Dis. 2018, 25, 255–262.
- Ndosi, M.; Vinall, K.; Hale, C.A.; Ptak, H.; Hill, J. The effectiveness of nurse-led care in people with rheumatoid arthritis: A systematic review. Int. J. Nurs. Stud. 2011, 48, 642–654.
- Solomon, D.H.; Bitton, A.; Fraenkel, L.; Brown, E.; Cao, P.; Katz, J.N. Roles of nurse practitioners and physician assistants in rheumatology practices in the US. Arthritis Care Res. 2014, 66, 1108–1113.
- Zangi, H.A.; Ndosi, M.; Adams, J.; Andersen, L.; Bode, C.; Boström, C.; van Eijk-Hustings, Y.; Gossec, L.; Korandová, J.; Mendes, G.; et al. EULAR recommendations for patient education for people with inflammatory arthritis. Ann. Rheum. Dis. 2015, 74, 954–962.
- Grønning, K.; Skomsvoll, J.F.; Rannestad, T.; Steinsbekk, A. The effect of an educational programme consisting of group and individual arthritis education for patients with polyarthritis-a randomised controlled trial. Patient Educ. Couns. 2012, 88, 113–120.
- Ndosi, M.; Johnson, D.; Young, T.; Hardware, B.; Hill, J.; Hale, C.; Maxwell, J.; Roussou, E.; Adebajo, A. Effects of needs-based patient education on self-efficacy and health outcomes in people with rheumatoid arthritis: A multicentre, single blind, randomised controlled trial. Ann. Rheum. Dis. 2016, 75, 1126–1132.
- Primdahl, J.; Sřrensen, J.; Horn, H.C.; Petersen, R.; Hørslev-Petersen, K. Shared care or nursing consultations as an alternative to rheumatologist follow-up for rheumatoid arthritis outpatients with low disease activity patient outcomes from a 2-year, randomised controlled trial. Ann. Rheum. Dis. 2014, 73, 357–364.
- de Thurah, A.; Stengaard-Pedersen, K.; Axelsen, M.; Fredberg, U.; Schougaard, L.M.V.; Hjollund, N.H.I.; Pfeiffer-Jensen, M.; Laurberg, T.B.; Tarp, U.; Lomborg, K.; et al. Tele-Health follow-up strategy for tight control of disease activity in rheumatoid arthritis: Results of a randomized controlled trial. Arthritis Care Res. 2018, 70, 353–360.
- Watts, R.A.; Mooney, J.; Barton, G.; MacGregor, A.J.; Shepstone, L.; Irvine, L.; Scott, D.G.I. The outcome and cost-effectiveness of nurse-led care in the community for people with rheumatoid arthritis: A non-randomized pragmatic study. BMJ Open 2015, 5, e007696.
- de Thurah, A.; Esbensen, B.A.; Roelsgaard, I.K.; Frandsen, T.F.; Primdahl, J. Efficacy of embedded nurse-led versus conventional physician-led follow-up in rheumatoid arthritis: A systematic review and meta-analysis. RMD (Reum. Musculoskelet. Dis.) Open 2017, 3, e000481.
- Smolen, J.S.; Breedveld, F.C.; Burmester, G.R.; Bykerk, V.; Dougados, M.; Emery, P.; Kvien, T.K.; Navarro-Compán, M.V.; Oliver, S.; Schoels, M.; et al. Treating rheumatoid arthritis to target: 2014 update of the recommendations of an international Task force. Ann. Rheumtic Dis. 2016, 75, 3–15.
- Smolen, J.S.; Landewé, R.; Bijlsma, J.; Burmester, G.; Chatzidionysiou, K.; Dougados, M.; Nam, J.; Ramiro, S.; Voshaar, M.; van Vollenhovena, R.; et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2016 update. Ann. Rheumtic Dis. 2017, 76, 960–977.
- Goulenok, T.; Serre, J.; François, C.; Van der Haegen, M.C.; Alexandra, J.F.; Papo, T.; Sacré, K. Nurse-led vaccination program dramatically improves pneumococcal vaccination coverage among patients with chronic inflammatory rheumatic diseases: A prospective pilot study . Ann. Rheum. Dis. 2017, 76 (Suppl. S2), 78–82.
- Craig, P.; Dieppe, P.; Macintyre, S.; Michie, S.; Nazareth, I.; Petticrew, M. Developing and evaluating complex interventions: The new medical Research Council guidance. Int. J. Nurs. Stud. 2013, 50, 587–592.
- Frølund, J.C.; Primdahl, J. Patients’ experiences of nurse-led screening for cardiovascular risk in rheumatoid arthritis. Musculoskelet. Care 2015, 13, 236–247.
- Hill, J.; Thorpe, R.; Bird, H. Outcomes for patients with RA: A rheumatology nurse practitioner clinic compared to standard outpatient care. Musculoskelet. Care 2003, 1, 5–20.
- Grønning, K.; Midttun, L.; Steinsbekk, A. Patients’ confidence in coping with arthritis after nurse-led education; a qualitative study. BMC Nurs. 2016, 15, 28.
- Garner, S.; Lopatina, E.; Rankin, J.A.; Marshall, D.A. Nurse-Led care for patients with rheumatoid arthritis: A systematic review of the effect on quality of care. J. Rheumatol. 2017, 44, 757–765.
- Robinson, S.; Hassell, A.; Ryan, S.; Adams, N.; Walker, D. A national survey of nurse training: Confidence and competence in educating patients commencing methotrexate therapy. Musculoskelet. Care 2017, 15, 281–292.
- British Society for Rheumatology. Specialist Nursing in Rheumatology. The State of Play. Available online: https://www.rheumatology.org.uk/Portals/0/Documents/Policy/Reports/Specialist_nursing_rheumatology_2019_State_of_Play.pdf?ver=2019-04-24-170948-180 (accessed on 1 June 2019).
- Walker, J. Rheumatoid arthritis: Role of the nurse and multidisciplinary team. Br. J. Nurs. 2012, 21, 334, 336–339.
- Riley, L.; Harris, C.; McKay, M.; Gondran, S.E.; DeCola, P.; Soonasra, A. The role of nurse practitioners in delivering rheumatology care and services: Results of a U.S. survey. J. Am. Assoc. Nurse Pract. 2017, 29, 673–681.
- van Eijk-Hustings, Y.; van Tubergen, A.; Boström, C.; Braychenko, E.; Buss, B.; Felix, J.; Firth, J.; Hammond, A.; Harston, B.; Hernandez, C.; et al. EULAR recommendations for the role of the nurse in the management of chronic inflammatory arthritis. Ann. Rheum. Dis. 2012, 71, 13–19.
- Fusama, M.; Nakahara, H.; van Eijk-Hustings, Y.; Oliver, S.; Takeuchi, T. Survey on attitudes regarding EULAR recommendations for the role of nurses involved in medical care of patients with chronic inflammatory arthritis in Japan. Mod. Rheumatol. 2017, 27, 886–893.
- Morgan, S.; Yoder, L.H. A concept analysis of person-centered care. J. Holist. Nurs. 2012, 30, 6–15.
- Larsson, I. Nurse-led Care and Patients as Partners Are Essential Aspects of the Future of Rheumatology Care. J. Rheumatol. 2017, 44, 720–722.
- Primdahl, J.; Wagner, L.; Holst, R.; Hørslev-Petersen, K. The impact on self-efficacy of different types of follow-up care and disease status in patients with rheumatoid arthritis–a randomized trial. Patient Educ. Couns. 2012, 88, 121–128.
More
Information
Subjects:
Nursing
Contributors
MDPI registered users' name will be linked to their SciProfiles pages. To register with us, please refer to https://encyclopedia.pub/register
:
View Times:
601
Revisions:
2 times
(View History)
Update Date:
15 Sep 2023
Notice
You are not a member of the advisory board for this topic. If you want to update advisory board member profile, please contact office@encyclopedia.pub.
OK
Confirm
Only members of the Encyclopedia advisory board for this topic are allowed to note entries. Would you like to become an advisory board member of the Encyclopedia?
Yes
No
${ textCharacter }/${ maxCharacter }
Submit
Cancel
Back
Comments
${ item }
|
More
No more~
There is no comment~
${ textCharacter }/${ maxCharacter }
Submit
Cancel
${ selectedItem.replyTextCharacter }/${ selectedItem.replyMaxCharacter }
Submit
Cancel
Confirm
Are you sure to Delete?
Yes
No




