
| Version | Summary | Created by | Modification | Content Size | Created at | Operation |
|---|---|---|---|---|---|---|
| 1 | János Nemcsik | -- | 1732 | 2023-09-06 08:06:48 | | | |
| 2 | Catherine Yang | Meta information modification | 1732 | 2023-09-06 08:27:08 | | |
Video Upload Options
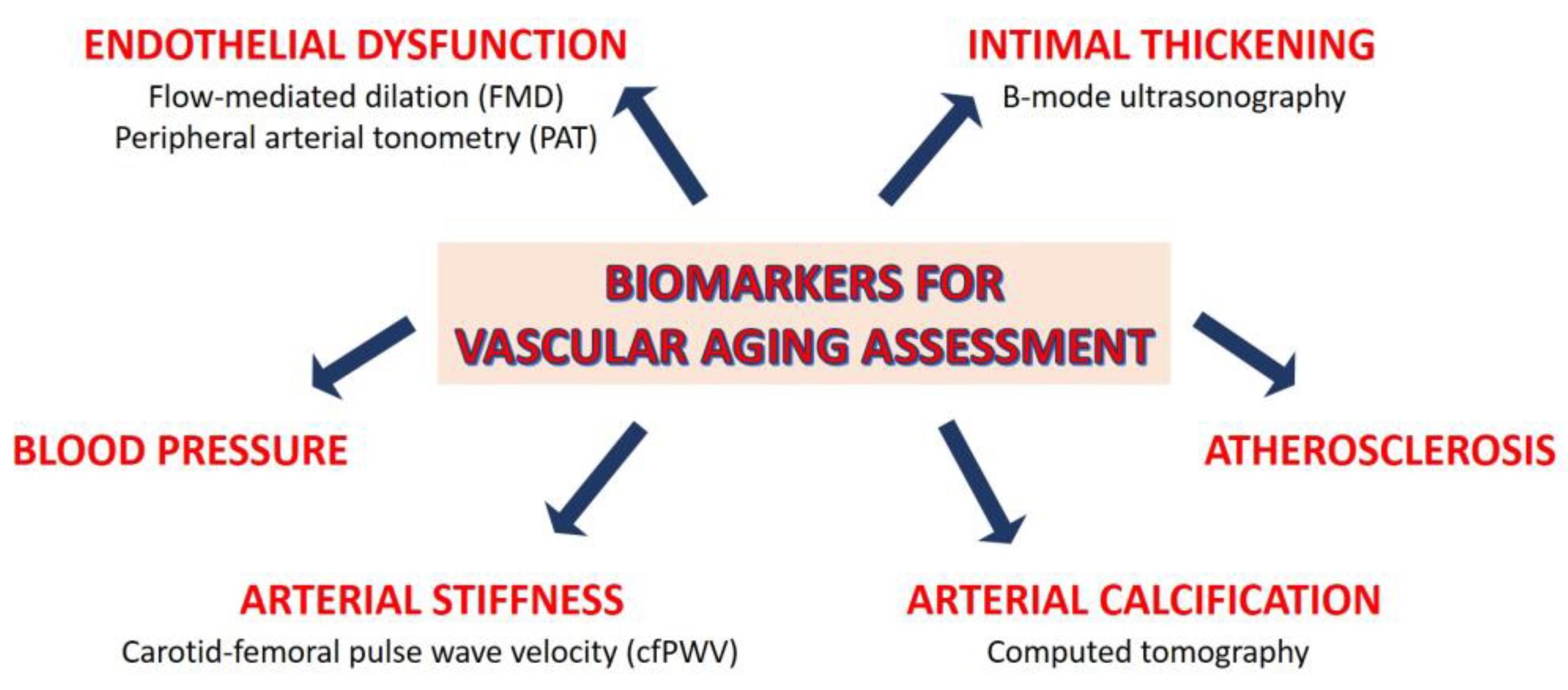
Vascular aging, i.e., the deterioration of the structure and function of the arteries over the life course, predicts cardiovascular events and mortality. Vascular degeneration can be recognized before becoming clinically symptomatic; therefore, its assessment allows the early identification of individuals at risk. This opens the possibility of minimizing disease progression. Vascular remodeling with advancing age is characterized by arterial stiffening and calcification. Arterial stiffening affects the macro- and micro-vasculature in unique ways. The main function of large arteries is to dampen the pulsatility of cardiac contraction by elastic recoiling after systolic expansion, so that constant, rather than pulsatile, blood flow is propelled to organs and tissues, including the coronary arteries.
1. Biological vs. Chronological Aging: Lessons from Progeria
2. Sex Differences in Cardiovascular Aging
3. Assessment of Vascular Aging
References
- Hamczyk, M.R.; Nevado, R.M.; Barettino, A.; Fuster, V.; Andrés, V. Biological Versus Chronological Aging: JACC Focus Seminar. J. Am. Coll. Cardiol. 2020, 75, 919–930.
- Hamczyk, M.R.; del Campo, L.; Andrés, V. Aging in the Cardiovascular System: Lessons from Hutchinson-Gilford Progeria Syndrome. Annu. Rev. Physiol. 2018, 80, 27–48.
- Benedicto, I.; Dorado, B.; Andrés, V. Molecular and Cellular Mechanisms Driving Cardiovascular Disease in Hutchinson-Gilford Progeria Syndrome: Lessons Learned from Animal Models. Cells 2021, 10, 1157.
- St Hilaire, C. Medial Arterial Calcification: A Significant and Independent Contributor of Peripheral Artery Disease. Arterioscler. Thromb. Vasc. Biol. 2022, 42, 253–260.
- Villa-Bellosta, R.; Rivera-Torres, J.; Osorio, F.G.; Acín-Pérez, R.; Enriquez, J.A.; López-Otín, C.; Andrés, V. Defective extracellular pyrophosphate metabolism promotes vascular calcification in a mouse model of Hutchinson-Gilford progeria syndrome that is ameliorated on pyrophosphate treatment. Circulation 2013, 127, 2442–2451.
- Dela Justina, V.; Miguez, J.S.G.; Priviero, F.; Sullivan, J.C.; Giachini, F.R.; Webb, R.C. Sex Differences in Molecular Mechanisms of Cardiovascular Aging. Front. Aging 2021, 2, 725884.
- Ji, H.; Kwan, A.C.; Chen, M.T.; Ouyang, D.; Ebinger, J.E.; Bell, S.P.; Niiranen, T.J.; Bello, N.A.; Cheng, S. Sex Differences in Myocardial and Vascular Aging. Circ. Res. 2022, 130, 566–577.
- Karikkineth, A.C.; AlGhatrif, M.; Oberdier, M.T.; Morrell, C.; Palchamy, E.; Strait, J.B.; Ferrucci, L.; Lakatta, E.G. Sex Differences in Longitudinal Determinants of Carotid Intima Medial Thickening with Aging in a Community-Dwelling Population: The Baltimore Longitudinal Study on Aging. J. Am. Heart Assoc. 2020, 9, e015396.
- Skaug, E.-A.; Aspenes, S.T.; Oldervoll, L.; Mørkedal, B.; Vatten, L.; Wisløff, U.; Ellingsen, O. Age and gender differences of endothelial function in 4739 healthy adults: The HUNT3 Fitness Study. Eur. J. Prev. Cardiol. 2013, 20, 531–540.
- Cheng, S.; Xanthakis, V.; Sullivan, L.M.; Vasan, R.S. Blood pressure tracking over the adult life course: Patterns and correlates in the Framingham heart study. Hypertension 2012, 60, 1393–1399.
- Ji, H.; Kim, A.; Ebinger, J.E.; Niiranen, T.J.; Claggett, B.L.; Bairey Merz, C.N.; Cheng, S. Sex Differences in Blood Pressure Trajectories Over the Life Course. JAMA Cardiol. 2020, 5, 19–26.
- López-Otín, C.; Blasco, M.A.; Partridge, L.; Serrano, M.; Kroemer, G. Hallmarks of aging: An expanding universe. Cell 2023, 186, 243–278.
- Climie, R.E.; Alastruey, J.; Mayer, C.C.; Schwarz, A.; Laucyte-Cibulskiene, A.; Voicehovska, J.; Bianchini, E.; Bruno, R.M.; Charlton, P.; Grillo, A.; et al. Vascular Ageing—Moving from Bench towards Bedside. Eur. J. Prev. Cardiol. 2023, 30, zwad028.
- Poredoš, P.; Cífková, R.; Marie Maier, J.A.; Nemcsik, J.; Šabovič, M.; Jug, B.; Ježovnik, M.K.; Schernthaner, G.H.; Antignani, P.L.; Catalano, M.; et al. Preclinical atherosclerosis and cardiovascular events: Do we have a consensus about the role of preclinical atherosclerosis in the prediction of cardiovascular events? Atherosclerosis 2022, 348, 25–35.
- Holder, S.M.; Bruno, R.M.; Shkredova, D.A.; Dawson, E.A.; Jones, H.; Hopkins, N.D.; Hopman, M.T.E.; Bailey, T.G.; Coombes, J.S.; Askew, C.D.; et al. Reference Intervals for Brachial Artery Flow-Mediated Dilation and the Relation with Cardiovascular Risk Factors. Hypertension 2021, 77, 1469–1480.
- Schnall, R.P.; Sheffy, J.K.; Penzel, T. Peripheral arterial tonometry-PAT technology. Sleep Med. Rev. 2022, 61, 101566.
- Nohria, A.; Gerhard-Herman, M.; Creager, M.A.; Hurley, S.; Mitra, D.; Ganz, P. Role of nitric oxide in the regulation of digital pulse volume amplitude in humans. J. Appl. Physiol. 2006, 101, 545–548.
- Sena, C.M.; Gonçalves, L.; Seiça, R. Methods to evaluate vascular function: A crucial approach towards predictive, preventive, and personalised medicine. EPMA J. 2022, 13, 209–235.
- Babcock, M.C.; DuBose, L.E.; Witten, T.L.; Brubaker, A.; Stauffer, B.L.; Hildreth, K.L.; Moreau, K.L. Assessment of macrovascular and microvascular function in aging males. J. Appl. Physiol. 2021, 130, 96–103.
- Alberro, A.; Iribarren-Lopez, A.; Sáenz-Cuesta, M.; Matheu, A.; Vergara, I.; Otaegui, D. Inflammaging markers characteristic of advanced age show similar levels with frailty and dependency. Sci. Rep. 2021, 11, 4358.
- Machin, D.R.; Bloom, S.I.; Campbell, R.A.; Phuong, T.T.T.; Gates, P.E.; Lesniewski, L.A.; Rondina, M.T.; Donato, A.J. Advanced age results in a diminished endothelial glycocalyx. Am. J. Physiol. Heart Circ. Physiol. 2018, 315, H531–H539.
- Patterson, E.K.; Cepinskas, G.; Fraser, D.D. Endothelial Glycocalyx Degradation in Critical Illness and Injury. Front. Med. 2022, 9, 898592.
- Gaarder, M.; Seierstad, T. Measurements of carotid intima media thickness in non-invasive high-frequency ultrasound images: The effect of dynamic range setting. Cardiovasc. Ultrasound 2015, 13, 5.
- Willeit, P.; Tschiderer, L.; Allara, E.; Reuber, K.; Seekircher, L.; Gao, L.; Liao, X.; Lonn, E.; Gerstein, H.C.; Yusuf, S.; et al. Carotid Intima-Media Thickness Progression as Surrogate Marker for Cardiovascular Risk: Meta-Analysis of 119 Clinical Trials Involving 100 667 Patients. Circulation 2020, 142, 621–642.
- Sarkola, T.; Manlhiot, C.; Slorach, C.; Bradley, T.J.; Hui, W.; Mertens, L.; Redington, A.; Jaeggi, E. Evolution of the arterial structure and function from infancy to adolescence is related to anthropometric and blood pressure changes. Arterioscler. Thromb. Vasc. Biol. 2012, 32, 2516–2524.
- van den Munckhof, I.C.L.; Jones, H.; Hopman, M.T.E.; de Graaf, J.; Nyakayiru, J.; van Dijk, B.; Eijsvogels, T.M.H.; Thijssen, D.H.J. Relation between age and carotid artery intima-medial thickness: A systematic review. Clin. Cardiol. 2018, 41, 698–704.
- O’Brien, M.W.; Kimmerly, D.S.; Theou, O. Sex-specific frailty and chronological age normative carotid artery intima-media thickness values using the Canadian longitudinal study of aging. Vascular 2023, 31, 17085381231157124.
- Nilsson, P.M.; Boutouyrie, P.; Laurent, S. Vascular aging: A tale of EVA and ADAM in cardiovascular risk assessment and prevention. Hypertension 2009, 54, 3–10.
- Laurent, S.; Chatellier, G.; Azizi, M.; Calvet, D.; Choukroun, G.; Danchin, N.; Delsart, P.; Girerd, X.; Gosse, P.; Khettab, H.; et al. SPARTE Study: Normalization of Arterial Stiffness and Cardiovascular Events in Patients with Hypertension at Medium to Very High Risk. Hypertension 2021, 78, 983–995.
- Bruno, R.M.; Nilsson, P.M.; Engström, G.; Wadström, B.N.; Empana, J.-P.; Boutouyrie, P.; Laurent, S. Early and Supernormal Vascular Aging: Clinical Characteristics and Association with Incident Cardiovascular Events. Hypertension 2020, 76, 1616–1624.
- McClelland, R.L.; Nasir, K.; Budoff, M.; Blumenthal, R.S.; Kronmal, R.A. Arterial age as a function of coronary artery calcium (from the Multi-Ethnic Study of Atherosclerosis ). Am. J. Cardiol. 2009, 103, 59–63.
- D’Agostino, R.B.S.; Vasan, R.S.; Pencina, M.J.; Wolf, P.A.; Cobain, M.; Massaro, J.M.; Kannel, W.B. General cardiovascular risk profile for use in primary care: The Framingham Heart Study. Circulation 2008, 117, 743–753.
- Conroy, R.M.; Pyörälä, K.; Fitzgerald, A.P.; Sans, S.; Menotti, A.; De Backer, G.; De Bacquer, D.; Ducimetière, P.; Jousilahti, P.; Keil, U.; et al. Estimation of ten-year risk of fatal cardiovascular disease in Europe: The SCORE project. Eur. Heart J. 2003, 24, 987–1003.
- Cuende, J.I.; Cuende, N.; Calaveras-Lagartos, J. How to calculate vascular age with the SCORE project scales: A new method of cardiovascular risk evaluation. Eur. Heart J. 2010, 31, 2351–2358.
- Gyöngyösi, H.; Kőrösi, B.; Batta, D.; Nemcsik-Bencze, Z.; László, A.; Tislér, A.; Cseprekál, O.; Torzsa, P.; Eörsi, D.; Nemcsik, J. Comparison of Different Cardiovascular Risk Score and Pulse Wave Velocity-Based Methods for Vascular Age Calculation. Heart Lung Circ. 2021, 30, 1744–1751.
- Vecsey-Nagy, M.; Szilveszter, B.; Kolossváry, M.; Boussoussou, M.; Vattay, B.; Merkely, B.; Maurovich-Horvat, P.; Radovits, T.; Nemcsik, J. Correlation between Coronary Artery Calcium- and Different Cardiovascular Risk Score-Based Methods for the Estimation of Vascular Age in Caucasian Patients. J. Clin. Med. 2022, 11, 1111.




